Abstract
Importance
The effect of large-scale disasters on bystander cardiopulmonary resuscitation (BCPR) performance is unknown.
Objective
To investigate whether and how large-scale earthquake and tsunami as well as subsequent nuclear pollution influenced BCPR performance for out-of-hospital cardiac arrest (OHCA) witnessed by family and friends/colleagues.
Design and setting
Retrospective analysis of prospectively collected, nationwide, population-based data for OHCA cases.
Participants
From the nationwide OHCA registry recorded between 11 March 2010 and 1 March 2013, we extracted 74 684 family-witnessed and friend/colleague-witnessed OHCA cases without prehospital physician involvement.
Exposure
Earthquake and tsunamis that were followed by nuclear pollution and largely affected the social life of citizens for at least 24 weeks.
Main outcome and measure
Neurologically favourable outcome after 1 month, 1-month survival and BCPR.
Methods
We analysed the 4-week average trend of BCPR rates in the years affected and before and after the disaster. We used univariate and multivariate logistic regression analyses to investigate whether these disasters affected BCPR and OHCA results.
Results
Multivariable logistic regression for tsunami-affected prefectures revealed that the BCPR rate during the impact phase in 2011 was significantly lower than that in 2010/2012 (42.5% vs 48.2%; adjusted OR; 95% CI 0.82; 0.68 to 0.99). A lower level of bystander compliance with dispatcher-assisted CPR instructions (62.1% vs 69.5%, 0.72; 95% CI 0.57 to 0.92) in the presence of a preserved level of voluntary BCPR performance (23.6% vs 23.8%) was also observed. Both 1-month survival and neurologically favourable outcome rates during the impact phase in 2011 were significantly poorer than those in 2010/2012 (8.5% vs 10.7%, 0.72; 95% CI 0.52 to 0.99, 4.0% vs 5.2%, 0.62; 95% CI 0.38 to 0.98, respectively).
Conclusion and relevance
A large-scale disaster with nuclear pollution influences BCPR performance and clinical outcomes of OHCA witnessed by family and friends/colleagues. Basic life-support training leading to voluntary-initiated BCPR might serve as preparedness for disaster and major accidents.
Keywords: accident & emergency medicine, education & training (see medical education & training), medical education & training, public health
Strengths and limitations of this study.
We studied the effects of large-scale disasters such as the Great East Japan Earthquake on the performance of bystander cardiopulmonary resuscitation (BCPR).
Analysis was performed using the 381 581 national out-of-hospital cardiac arrest cases in the All-Japan Utstein Registry of the Fire and Disaster Management Agency of Japan recorded between 11 March 2010 and 10 March 2013.
The primary outcome was the provision of BCPR by family or friends/colleagues, and the secondary outcomes were 1-month survival and neurologically favourable outcome after 1 month.
Introduction
The Great East Japan Earthquake swept the North-East Pacific coast of the Japanese mainland on 11 March 2011, and an earthquake-generated tsunami destroyed cities, towns and villages located at the North-East Pacific coast, resulting in the Fukushima Dai-ichi nuclear accident. This disaster forced citizens in afflicted areas to spend a long period as evacuees.1 2 A considerable number of major aftershocks with and without a tsunami warning (moment magnitude ≥6.0) occurred for 24 weeks after the main disaster (online supplemental figure, upper panel).3 After evacuation of survivors living in tsunami-affected areas, more than 15 000 people lived temporarily in ‘shelters’ and eventually moved into temporary housing areas, leaving their hometowns. The search for missing people continued for 24 weeks after the disaster. Based on a survey conducted on 10 June 2020, the final number of victims was 22 167, comprising 19 638 fatalities, which included 3739 disaster-related deaths and 2529 missing people (online supplemental figure, middle panel).2 Several emergency fire response teams and volunteers provided disaster services in the tsunami-affected prefectures (online supplemental figure, lower panel). Reconstruction of the destroyed towns and cities with resumption of farming and fishery industries began only around 24 weeks after the disaster.4 Several aspects of this disaster have been reviewed over the past 10 years following the disaster.2
bmjopen-2021-055640supp001.pdf (70.1KB, pdf)
Large-scale disasters or catastrophes may psychologically affect the social behaviour of citizens.5 6 Disasters are known to temporally increase the incidence of cardiovascular events and other acute illnesses that may lead to out-of-hospital cardiac arrest (OHCA).7–9 The outcomes of OHCA depend on dispatcher-assisted and bystander-initiated resuscitation efforts and on initial basic life-support (BLS) actions by bystanders who witness OHCA.10 The Fukushima nuclear pollution disaster and the large-scale pandemic such as COVID-19 may augment the level of general fear of pollution and infection in the population, which might discourage bystander cardiopulmonary resuscitation (BCPR).11 12 However, the impact of large-scale disasters on BCPR actions of laypersons is unknown. This study aimed to investigate whether and how the 2011 earthquake influenced the BCPR and outcomes in OHCA cases witnessed by family, friends, and colleagues in the prefectures that were most affected by the earthquake.
Methods
Data selection and grouping
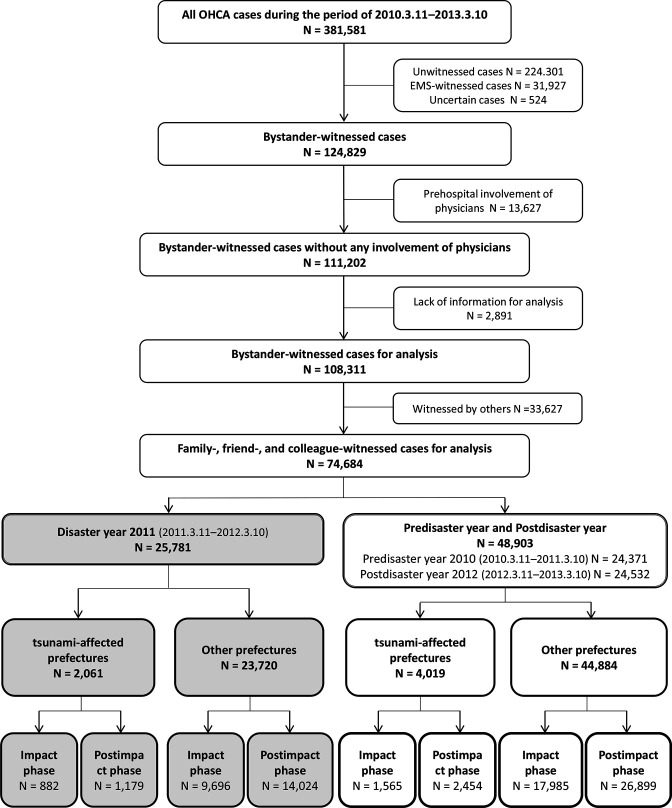
From the 381 581 nationwide OHCA cases in the All-Japan Utstein-style13 Registry of the Japanese Fire and Disaster Management Agency, recorded between 11 March 2010 and 10 March 2013, we extracted 108 311 bystander-witnessed cases that did not involve any physician and excluded 2891 cases that lacked information for analysis. After the disaster, many healthcare providers visited the site. Also, there were many healthcare providers in evacuation shelters and temporary housing. Therefore, we extracted 74 684 family-witnessed and friend/colleague-witnessed OHCA cases, excluding cases witnessed by others, to minimise the effect of healthcare providers volunteering for and/or being involved in disaster medical support (figure 1). The study period included the predisaster year 2010 (11 March 2010–10 March 2011), disaster year 2011 (11 March 2011–10 March 2012) and postdisaster year 2012 (11 March 2012–10 March 2013). Tsunami-affected prefectures, defined as prefectures in which a tsunami with a maximum height of >4 m was observed, included five prefectures located in the North-East Pacific coast of the Japanese mainland: Aomori, Iwate, Miyagi, Fukushima and Ibaraki prefectures.1 The prefectures other than these five tsunami-affected prefectures were designated as other prefectures.
Figure 1.
Data selection and subgroup extraction. EMS, emergency medical service; OHCA, out-of-hospital cardiac arrest.
On the basis of the occurrence of aftershocks, number of evacuees in evacuation centres, and resumption of social activities, we determined that 0–23 weeks from 11 March 2011 was the period affected by the disaster. We defined the same period from 2010 to 2012 as the impact phase.
Outcome measures
The primary outcome of this study was provision of BCPR by a family member or a friend/colleague. The secondary outcomes were a neurologically favourable outcome after 1 month, defined as a cerebral performance category score of 1 (good recovery) or 2 (moderate disability)14 and 1-month survival.
Data analysis
To investigate the validity of the impact phase definition, we analysed the 4-week average trends in the BCPR rate after the day of disaster in the year 2011 and on the same day (11 March) in the predisaster year of 2010 and postdisaster year of 2012 in the tsunami-affected and other prefectures.
The influence of disaster on BCPR and OHCA outcomes in the tsunami-affected prefectures were investigated using univariate and multivariable logistic regression analyses. The BCPR rates, 1-month survival rates, and neurologically favourable 1-month outcomes were compared between the disaster year (2011) and the predisaster/postdisaster years (2010/2012) during the impact and the postimpact phases in tsunami-affected and other prefectures.
Bystanders exhibit four patterns of behaviour against OHCA: BCPR following dispatcher-assisted CPR (DA-CPR) instruction, bystander-initiated BCPR without DA-CPR, no BCPR despite DA-CPR and no BCPR without DA-CPR. Furthermore, to clarify the association of the impact phase with dispatcher-assisted and bystander-initiated resuscitation efforts, we calculated the following three indices related to DA-CPR and BCPR in accordance with a previous report15: (1) sensitivity of DA-CPR for OHCA (=the number of cases for which DA-CPR was attempted divided by the number of cases that did not receive bystander-initiated BCPR without DA-CPR); (2) proportion of bystanders to follow DA-CPR (=the number of cases that received BCPR following DA-CPR divided by the number of cases for which DA-CPR was attempted) and (3) bystander’s own performance of BCPR for OHCA (=the number of cases that received bystander-initiated BCPR without DA-CPR divided by the number of cases for which DA-CPR was not attempted).10 16
Univariate analyses were performed using the χ2 test or Fisher’s exact probability test for nominal variables. Because the continuous variables analysed in this study did not show a normal distribution, the Mann-Whiney U test was applied for continuous variables. Multivariable logistic regression analysis for BCPR provision included the factors, which were well known to be associated with BCPR provision: daytime, weekend, patient sex and age, aetiology of OHCA (presumed cardiac or not, exogenous origin), family bystander and DA-CPR instruction. Factors included in multivariable logistic regression analysis for outcomes were daytime, patient sex and age, presumed cardiac aetiology, initial rhythm (shockable or not), BCPR provision, family bystander, tracheal intubation and epinephrine administration by paramedics, time interval between witness and emergency call, and time interval between emergency call and emergency medical service (EMS) arrival at patients (EMS response time). All tests were two tailed, and we considered a probability (p)<0.05 to be statistically significant. All statistical analyses were performed using the JMP Pro V.15 software (SAS Institute).
Patient and public involvement
Patients or the public were not involved in the design, conduct, reporting or dissemination plans of our study.
Results
Number of family-witnessed and friends/colleague-witnessed OHCA cases in the tsunami-affected prefectures and other prefectures
A total of 74 684 family-witnessed and friends/colleague-witnessed OHCA cases were extracted and analysed. Among these, the number of family-witnessed and friends/colleague-witnessed OHCA cases in the tsunami-affected prefectures was 2061 for the disaster year 2011 and 4019 for 2010/2012. The number of family-witnessed and friends/colleague-witnessed OHCA cases in other prefectures was 23 720 for 2011 and 44 884 for 2010/2012 (figure 1, lower part). The number of family-witnessed and friends/colleague-witnessed OHCA cases during the impact phase was 882 for the disaster year 2011and 1565 for 2010/2012 in the tsunami-affected prefectures, whereas it was 9696 for 2011 and 17 985 for 2010/2012 in other prefectures.
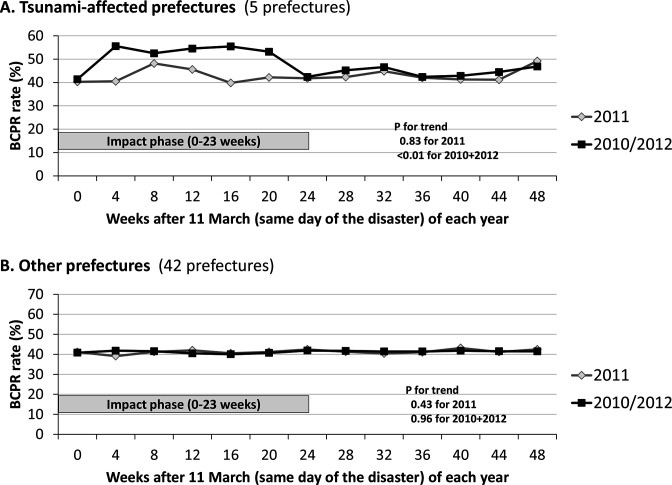
Validity of the impact phase definition (4-week average trends in BCPR provision after the day of disaster)
The trends in the BCPR rate in 2011 (disaster year) differed from those in 2010/2012 (predisaster and postdisaster years) in the tsunami-affected prefectures (figure 2, upper panel). In 2010/2012, the BCPR rate remained high (>50%) during weeks 4–23 (corresponding to the spring and summer seasons) whereas it was low (nearly 40%) during weeks 36–43 (winter season) (p for trend: <0.01). However, the BCPR rate remained low except for weeks 8–15 after the disaster, and no seasonal variations were observed in 2011 (p for trend: 0.83). The impact phase coincided with the period during which the differences in the 4-week averages of BCPR between 2011 and 2010/2012 were recognised in the tsunami-affected prefectures.
Figure 2.
Four-week average trends of bystander cardiopulmonary resuscitation in tsunami-affected prefectures and other prefectures BCPR impact phase, 0–23 weeks from 11 March. BCPR, bystander cardiopulmonary resuscitation.
On the other hand, in other prefectures (the tsunami-not-affected prefectures), the trend of BCPR rate was the same in 2011 (year of disaster) and 2010/2012. The BCPR rate remained at nearly 40% throughout the 3 years, regardless of the impact phase of the disaster (before and after the disaster; figure 2, lower panel). Furthermore, there were no obvious seasonal variations (p for trend: 0.43 in 2011 and 0.96 in 2010/2012).
The average rates of BCPR during the impact phase were 42.5% (375/882) for the disaster year 2011 and 48.2% (754/1,565) for 2010/2012 in tsunami-affected prefectures and 40.3% (3907/9696) for 2011 and 40.2% (7263/17 985) for 2010/2012 in other prefectures.
Differences in the backgrounds and characteristics of OHCA between the disaster year and the predisaster/postdisaster years
In the tsunami-affected prefectures, during the impact phase, the incidence of OHCA during weekends and the proportion of cases of presumed cardiac aetiology in 2011 were higher than those in 2010/2012, whereas the rate of DA-CPR was lower. As expected, transportation time from the scene to the hospital was prolonged in 2011. During the postimpact phase, there was no significant difference in backgrounds between 2011 and 2010/2012 (table 1).
Table 1.
Background, characteristics and time factors of family-witnessed and friend/colleague-witnessed out-of-hospital cardiac arrest cases in tsunami-affected prefectures
| Background, characteristics and time factors | Impact phase | Unadjusted OR (95% CI)* or P value |
Postimpact phase | Unadjusted OR (95% CI)* or P value |
||
| 2011 (N=882) |
2010/2012 (N=1565) |
2011 (N=1179) |
2010/2012 (N=2454) |
|||
| Family-witnessed patients, no (%) | 783 (88.8) | 1404 (89.7) | 0.91 (0.70 to 1.18) | 1074 (91.1) | 2219 (90.4) | 1.08 (0.85 to 1.38) |
| Daytime (7:00–19:00 hours), no (%) | 520 (59.0) | 950 (60.7) | 0.93 (0.79 to 1.10) | 682 (57.9) | 1485 (60.5) | 0.90 (0.79 to 1.03) |
| Weekend, no (%) | 141 (16.0) | 192 (12.3) | 1.36 (1.08 to 1.72) | 146 (12.4) | 338 (13.8) | 0.89 (0.72 to 1.09) |
| Age, median (IQR), year | 78 (65–84) | 76 (63–84) | 0.12 | 77 (66–84) | 78 (67–85) | 0.17 |
| Male patient, no (%) | 598 (67.8) | 1002 (64.0) | 1.18 (1.00 to 1.41) | 734 (62.3) | 1525 (62.1) | 1.01 (0.87 to 1.16) |
| Presumed cardiac aetiology, no (%) | 554 (62.8) | 877 (56.0) | 1.33 (1.12 to 1.57) | 725 (61.5) | 1443 (58.8) | 1.12 (0.97 to 1.29) |
| Exogenous origin†, no (%) | 102 (11.6) | 206 (13.2) | 0.86 (0.67 to 1.11) | 118 (10.0) | 259 (10.6) | 0.94 (0.75 to 1.19) |
| Shockable initial rhythm, no (%) | 162 (18.4) | 271 (17.3) | 1.07 (0.87 to 1.33) | 185 (15.7) | 345 (14.1) | 1.14 (0.94 to 1.38) |
| Dispatcher-assisted CPR, no (%) | 433 (49.1) | 835 (53.4) | 0.84 (0.72 to 0.99) | 598 (50.7) | 1240 (50.5) | 1.01 (0.88 to 1.16) |
| Defibrillation by bystanders with an AED, no (%) | 4 (0.5) | 9 (0.6) | 0.79 (0.24 to 2.58) | 11 (0.9) | 12 (0.6) | 1.65 (0.73 to 3.75) |
| Epinephrine administration by paramedics, no (%) | 153 (17.4) | 256 (16.4) | 1.07 (0.86 to 1.34) | 231 (19.6) | 448 (19.7) | 1.00 (0.84 to 1.19) |
| Tracheal intubation by paramedics, no (%) | 78 (8.8) | 161 (10.3) | 0.85 (0.64 to 1.12) | 103 (8.7) | 251 (10.2) | 0.84 (0.66 to 1.07) |
| Time intervals, median (IQR), min | ||||||
| Witness-to-emergency call | 2 (0–5) | 2 (0–5) | 0.71 | 2 (0–5) | 2 (0–5) | 0.49 |
| EMS response time‡ | 8 (7–11) | 9 (7–11) | 0.45 | 9 (7–11) | 9 (7–12) | 0.11 |
| EMS arrival at patient-to-arrival at the hospital | 21 (16–28) | 20 (15–27) | <0.05 | 22 (16–29) | 22 (16–29) | 0.74 |
Bold figures indicate significant results.
*2010/2012 as a reference.
†Asphyxia, submersion, hypothermia, poisoning and trauma.
‡Time interval between emergency call and EMS arrival at patient.
AED, automated external defibrillator; CPR, cardiopulmonary resuscitation; EMS, emergency medical service.
In other prefectures, significant differences in some prehospital confounders were observed between 2011 and 2010/2012 during the impact and postimpact phases. However, the differences in these parameters were very small (online supplemental table 1).
bmjopen-2021-055640supp002.pdf (75.8KB, pdf)
Multivariable regression analyses of the differences in BCPR provision and outcomes between the disaster year and the predisaster/postdisaster years
In the tsunami-affected prefectures, the rates of BCPR, 1-month survival and 1-month neurologically favourable outcome in 2011 were significantly lower than those in 2010/2012 during the impact phase. During the postimpact phase, no significant difference in any of these parameters was observed between 2011 and 2010/2012 (table 2). In other prefectures, significant differences were observed neither during the impact phase nor during the postimpact phase (online supplemental table 2).
Table 2.
Phasic comparisons of BCPR and outcomes between 2011 and 2010/2012 in tsunami-affected prefectures
| BCPR and outcomes | Impact phase | Adjusted OR (95% CI) with 2010/2012 as a reference |
Postimpact phase | Adjusted OR (95% CI) with 2010/2012 as a reference |
||
| 2011 (N=882) |
2010/2012 (N=1565) |
2011 (N=1179) |
2010/2012 (N=2454) |
|||
| BCPR rate, no (%) | 375 (42.5) | 754 (48.2) | 0.82 (0.68 to 0.99)* | 510 (43.3) | 1068 (43.5) | 0.99 (0.84 to 1.16)† |
| 1 month survival, no (%) | 75 (8.5) | 168 (10.7) | 0.72 (0.52 to 0.99)‡ | 103 (8.7) | 200 (8.2) | 1.02 (0.78 to 1.33)§ |
| Neurologically favourable outcome, no (%) | 35 (4.0) | 82 (5.2) | 0.62 (0.38 to 0.98)¶ | 48 (4.1) | 107 (4.4) | 0.89 (0.61 to 1.29)** |
Bold figures indicate significant results.
*Among the other factors including in the logistic regression model, age (adjusted OR; 95% CI, 0.93; 0.88 to 0.99/10 years), family bystander (0.52: 0.38 to 0.71), and DA-CPR provision (7.07; 5.89 to 8.5) were significantly associated with BCPR rate.
†Among the other factors including in the logistic regression model, age (0.92; 0.87 to 0.97/10 years), family bystander (0.49: 0.37 to 0.64) and DA-CPR provision (9.27; 7.92 to 10.9) were significantly associated with BCPR rate.
‡Among the other factors including in the logistic regression model, age (0.81; 0.75 to 0.88/10 years), EMS response time (0.38; 0.31 to 0.48/10 min), time interval of witness-to-emergency call (0.71; 0.59 to 0.91/10 min), male patients (1.43; 1.01 to 2.03), daytime (7:00–19:00 hours) OHCA (1.54; 1.13 to 2.11), shockable initial rhythm (6.93; 4.92 to 9.76) and epinephrine administration (0.64; 0.41 to 0.99) were significantly associated with 1-month survival.
§Among the other factors including in the logistic regression model, age (0.86; 0.80 to 0.92/10 years), EMS response time (0.46; 0.39 to 0.56/10 min), time interval of witness-to-emergency call (0.66; 0.57 to 0.80/10 min), cardiac aetiology (0.67; 0.50 to 0.89), and shockable initial rhythm (6.93; 4.92 to 9.76) were significantly associated with 1-month survival.
¶Among the other factors including in the logistic regression model, age (0.76; 0.69 to 0.85/10 years), EMS response time (0.29; 0.23 to 0.39/10 min), time interval of witness-to-emergency call (0.54; 0.41 to 0.79/10 min), shockable initial rhythm (12.4; 7.34 to 20.9), and epinephrine administration (0.18; 0.07 to 0.44) were significantly associated with neurologically favourable outcome.
**Among the other factors including in the logistic regression model, age (0.87; 0.79 to 0.97/10 years), EMS response time (0.39; 0.31 to 0.51/10 min), time interval of witness-to-emergency call (0.53; 0.43 to 0.69/10 min), shockable initial rhythm (12.4; 7.34 to 20.9) and cardiac aetiology (1.53; 1.07 to 2.2) were significantly associated with neurologically favourable outcome.
BCPR, bystander cardiopulmonary resuscitation; DA-CPR, dispatcher-assisted CPR; EMS, emergency medical service.
As shown in the footnotes, the multivariable regression analysis disclosed that DA-CPR (with adjusted ORs ranging from 7.07 to 9.27) was a common and major factor associated with BCPR provision, regardless of the phase and prefecture. The major factors associated with a neurologically favourable outcome included shockable initial rhythm and EMS response time. Notably, the adjusted OR (95% CI) of shockable initial rhythms for neurologically favourable outcome was much higher during the impact phase than during the postimpact phase in tsunami-affected prefectures (12.4 (7.3 to 20.9) vs 7.1 (4.7 to 10.8), interaction test, p<0.01).
Analysis of indices for dispatcher-assisted and bystander-initiated resuscitation efforts
In tsunami-affected prefectures, DA-CPR sensitivity and bystander’s compliance to DA-CPR appeared to be suppressed during the impact phase in 2011, being 55.8% and 62.1%, respectively in 2011, and 60.0% and 69.5%, respectively in 2010/2012. However, the difference between 2011 and However, 2010/2012 was significant only for bystander’s compliance to DA-CPR (adjusted OR; 95% CI 0.72; 0.57 to 0.92). During the postimpact phase, there were no significant differences in these indices between 2011 and 2010/2012. Difference in the performance of BCPR was detected neither during the impact phase nor during the postimpact phase (table 3).
Table 3.
Phasic comparisons of indices for dispatcher-assisted and bystander-initiated resuscitation efforts between 2011 and 2010/2012 in tsunami-affected prefectures
| Indices related to DA-CPR and BCPR | Impact phase | Unadjusted OR (95% CI) with 2010/2012 as a reference | Postimpact phase | Unadjusted OR (95% CI) with 2010/2012 as a reference | ||
| 2011 | 2010/2012 | 2011 | 2010/2012 | |||
| DA-CPR sensitivity, no/total (%) | 433/776 (55.8) | 835/1391 (60.0) | 0.84 (0.70 to 1.00) | 598/1062 (56.3) | 1,240/2224 (55.8) | 1.02 (0.88 to 1.19) |
| Bystander’s compliance to DA-CPR, no/total (%) | 269/433 (62.1) | 255/835 (69.5) | 0.72 (0.57 to 0.92) | 393/598 (65.7) | 838/1240 (67.6) | 0.92 (0.75 to 1.13) |
| Bystander’s own performance of BCPR, no/total (%) | 106/449 (23.6) | 174/730 (23.8) | 0.99 (0.72 to 1.07) | 117/581 (20.1) | 230/1214 (19.0) | 1.08 (0.84 to 1.39) |
Bold figures indicate significant results.
BCPR, bystander cardiopulmonary resuscitation; DA-CPR, dispatcher-assisted cardiopulmonary resuscitation.;
In other prefectures, none of the three indices differed between 2011 and 2010/2012; neither during the impact phase nor during the postimpact phase (online supplemental table 3).
Discussion
In disaster mental health, the reactions of the community and the individual are usually divided to four phases (heroic phase, honeymoon phase, disillusionment phase and restoration phase),17 although the duration of these phases may vary depending on the scale and type of disaster. The impact phase in this study covers the period from heroic phase to disillusionment phase. This relatively long impact phase and the wide area affected by the disaster may contribute to the detection of a significant impact of the disaster in this study.
Loss of family members and friends, lack of employment stability, or extensive damage to property, resulting in loss of or a decrease in income are reported as risk factors for the development of disaster-related mental health problems.18–20 In this study, the BCPR rate in tsunami-affected prefectures temporally increased during the 8–11 weeks after the disaster but remained low thereafter, reflecting a temporal relief in anxiety due to increased provision of supplies and accommodation during the ‘honeymoon phase’ and recognition of depressed economic resilience, repeated aftershocks, and escape or avoidance behaviour21 during disillusionment phase.
The BCPR rate varies between countries, but the BCPR rate in Japan in the 3 years from 2010 to 2012 was as high as or higher than that in the European Union and USA.22 23 In comparison with other prefectures, a higher BCPR rate in tsunami-affected prefectures might be due to the higher proportion of citizens having attended BLS training courses every year.24–26 People with CPR training are known to perform BCPR more than those without an experience of CPR training.27 Compared with the patients with OHCA in the other (nonaffected) prefectures, those in the tsunami-affected prefectures were subject to relatively higher BCPR rates in the predisaster and postdisaster years, particularly during the spring and summer seasons, which is identical to that in the impact phase that we determined. Major industries in the affected areas included fishery, agriculture and food processing managed by corporative unions. The population, particularly the elderly, typically endures a rugged winter at home, and their social activities diminish at the end of autumn and over the winter. Meanwhile, during spring and summer, citizens including the elderly cooperate in agricultural work and preparation of social events, including festivals and outdoor events.28 Increased collaborative activities of citizens, including the elderly, in these seasons and accommodativeness as a general personality trait of the citizens might be one of the reasons for this seasonal variation in BCPR rate because OHCA cases in these seasons are frequently managed by many bystanders, including those with training experience.
Surveys on citizens and EMS personnel who survived the disaster in tsunami-affected prefectures reported that more than half of them lost their family and friends/colleagues.29 People who died during the disaster were mostly the elderly (54.4%), suggesting that the proportion of trained bystanders was not affected by the disaster.30 Thus, decreased rates of BCPR and DA-CPR may be attributed to the decreased collaborative social activities and psychological reactions of dispatchers and bystanders, which may interfere with communication between bystanders and dispatchers.
The 2011 earthquake and the earthquake-associated tsunami were followed by a nuclear accident in the Fukushima prefecture. People who had a false understanding of radiation were afraid to interact with evacuees and avoided contact. For these reasons, it is highly possible that nuclear pollution may interfere with bystander-initiated CPR provision due to augmented fear of nuclear pollution during CPR, particularly of refugees from the polluted area.31 Recent studies on the COVID-19 pandemic on BCPR support this assumption.12
It might be difficult to prevent the BCPR and certain outcomes from deteriorating during the impact phase. The analysis of the three indices related to DA-CPR and BCPR showed that only the level of voluntary performance of BCPR was preserved during the impact phase in tsunami-affected prefectures. Because BLS training is known to augment the willingness to provide voluntary BCPR without DA-CPR,32 systematic BLS training to citizens may be effective for preservation of voluntary performance of BCPR in the event of a disaster. Furthermore, this study showed that the dependence of outcome on initial shockable rhythm was augmented during the impact phase in Tsunami-affected prefecture. However, incidences of public access to defibrillation (defibrillation by bystanders with an automated external defibrillator, AED) during the study period was extremely low (<1%), particularly during the impact phase in Tsunami-affected prefecture (0.6%). Public-access defibrillation has definitive impact on the outcome of OHCA.33 Therefore, BLS training including AED use and its supply might function as preparedness for disaster.
Limitation
This study has several strengths. First, this study focused on alterations in bystander-initiated and dispatcher-instructed BCPR after a large-scale disaster. Second, not only before-and-after comparisons but also differences in trends were analysed between tsunami-affected and tsunami-unaffected prefectures using a large nationwide dataset. However, this study also has several limitations. First, although the catastrophe occurred in the coastal areas of some of the prefectures, the analyses were performed after dividing the prefectures. In tsunami-affected prefectures, no major urban areas were located in the coastal area, and differences in BCPR intervention between urban and rural areas34 were excluded in this study. Second, bystander-specific data, such as age, sex, and training experience were not included in the database and therefore not available for study. Third, it was not possible to study whether the bystanders were actually psychologically affected. Therefore, these factors potentially associated with BCPR quality might affect the quality of the study results.35 Fourth, no comparative analysis was performed with the results of other disasters. Fifth, since this study is based on one disaster that occurred in Japan, it is unclear whether the results will apply to other disasters as well. Sixth, as with other observational studies, the validity of data is another potential limitation.
Conclusions
A large-scale disaster may influence bystander-initiated CPR and outcomes of OHCA witnessed by family/friends/colleagues. BLS training might serve as preparedness for disaster and major accidents.
Supplementary Material
Acknowledgments
We thank the EMS personnel and FDMA in Japan for their cooperation in collecting and managing the All-Japan Utstein Registry data. TU and KT equally contributed to this article as first authors.
Footnotes
Contributors: TU and KT had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. TU and KT equally contributed to this article as first authors. Guarantor: TU. Study concept and design: TU, KT and HI. Acquisition, analysis and interpretation of data: All authors. Drafting of the manuscript: AY, HM, HI, KT and TU. Clinical revision of the manuscript for important intellectual content: TU, HI, KT and YW. Statistical analysis: TU, KT and HI. Administrative, technical, or material support: HI and YW. Study supervision: HI and YW.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data sharing not applicable as no datasets generated and/or analysed for this study. No additional data available.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study was approved by the institutional review board of the Ishikawa Medical Control Council and conducted by the study group comprising of members of the Ishikawa Medical Control Council and their collaborators. Patient consent was not required for use of the secondary data.
References
- 1.Department of International Affairs, Japan Science and Technology Agency . The great East Japan earthquake information from official websites, 2011. Available: https://www.jst.go.jp/pr/pdf/great_east_japan_earthquake.pdf [Accessed 08 Dec 2021].
- 2.Fire and Disaster Management Agency (Japan) . Great East Japan Earthquake (in Japanese). Available: https://www.fdma.go.jp/disaster/higashinihon/ [Accessed 08 Dec 2021].
- 3.Japan Meteorological Agency . The 2011 great East Japan earthquake: number of aftershock (in Japanese). Available: http://www.data.jma.go.jp/svd/eqev/data/2011_03_11_tohoku/aftershock/ [Accessed 08 Dec 2021].
- 4.Reconstruction Agency (Japan) . Recovery and reconstruction from the great East Japan earthquake, 2012 (in Japanese). Available: https://www.reconstruction.go.jp/topics/20130104_higashinippondaishinsai_fukkoh.pdf [Accessed 08 Dec 2021].
- 5.Ozdemir O, Boysan M, Guzel Ozdemir P, et al. Relationships between posttraumatic stress disorder (PTSD), dissociation, quality of life, hopelessness, and suicidal ideation among earthquake survivors. Psychiatry Res 2015;228:598–605. 10.1016/j.psychres.2015.05.045 [DOI] [PubMed] [Google Scholar]
- 6.Makwana N. Disaster and its impact on mental health: a narrative review. J Family Med Prim Care 2019;8:3090–5. 10.4103/jfmpc.jfmpc_893_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leor J, Poole WK, Kloner RA. Sudden cardiac death triggered by an earthquake. N Engl J Med 1996;334:413–9. 10.1056/NEJM199602153340701 [DOI] [PubMed] [Google Scholar]
- 8.Ogawa K, Tsuji I, Shiono K, et al. Increased acute myocardial infarction mortality following the 1995 great Hanshin-Awaji earthquake in Japan. Int J Epidemiol 2000;29:449–55. 10.1093/ije/29.3.449 [DOI] [PubMed] [Google Scholar]
- 9.Sokejima S, Nakatani Y, Kario K, et al. Seismic intensity and risk of cerebrovascular stroke: 1995 Hanshin-Awaji earthquake. Prehosp Disaster Med 2004;19:297–306. 10.1017/S1049023X00001928 [DOI] [PubMed] [Google Scholar]
- 10.Yamashita A, Maeda T, Myojo Y, et al. Temporal variations in dispatcher-assisted and bystander-initiated resuscitation efforts. Am J Emerg Med 2018;36:2203–10. 10.1016/j.ajem.2018.03.080 [DOI] [PubMed] [Google Scholar]
- 11.Savastano S, Vanni V. Cardiopulmonary resuscitation in real life: the most frequent fears of lay rescuers. Resuscitation 2011;82:568–71. 10.1016/j.resuscitation.2010.12.010 [DOI] [PubMed] [Google Scholar]
- 12.Pranata R, Lim MA, Yonas E, et al. Out-Of-Hospital cardiac arrest prognosis during the COVID-19 pandemic. Intern Emerg Med 2020;15:875–7. 10.1007/s11739-020-02428-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jacobs I, Nadkarni V, Bahr J, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International liaison Committee on resuscitation (American heart association, European resuscitation Council, Australian resuscitation Council, New Zealand resuscitation Council, heart and stroke Foundation of Canada, InterAmerican heart Foundation, resuscitation councils of southern Africa). Circulation 2004;110:3385–97. 10.1161/01.CIR.0000147236.85306.15 [DOI] [PubMed] [Google Scholar]
- 14.Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet 1975;1:480–4. 10.1016/s0140-6736(75)92830-5 [DOI] [PubMed] [Google Scholar]
- 15.Maeda T, Yamashita A, Myojo Y, et al. Augmented survival of out-of-hospital cardiac arrest victims with the use of mobile phones for emergency communication under the DA-CPR protocol getting information from callers beside the victim. Resuscitation 2016;107:80–7. 10.1016/j.resuscitation.2016.08.010 [DOI] [PubMed] [Google Scholar]
- 16.Nishi T, Kamikura T, Funada A, et al. Are regional variations in activity of dispatcher-assisted cardiopulmonary resuscitation associated with out-of-hospital cardiac arrests outcomes? A nation-wide population-based cohort study. Resuscitation 2016;98:27–34. 10.1016/j.resuscitation.2015.10.004 [DOI] [PubMed] [Google Scholar]
- 17.Math SB, Nirmala MC, Moirangthem S, et al. Disaster management: mental health perspective. Indian J Psychol Med 2015;37:261–71. 10.4103/0253-7176.162915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Norris FH, Friedman MJ, Watson PJ, et al. 60,000 disaster victims speak: Part I. An empirical review of the empirical literature, 1981-2001. Psychiatry 2002;65:207–39. 10.1521/psyc.65.3.207.20173 [DOI] [PubMed] [Google Scholar]
- 19.Başoğlu M, Kiliç C, Salcioğlu E, et al. Prevalence of posttraumatic stress disorder and comorbid depression in earthquake survivors in turkey: an epidemiological study. J Trauma Stress 2004;17:133–41. 10.1023/B:JOTS.0000022619.31615.e8 [DOI] [PubMed] [Google Scholar]
- 20.van Griensven F, Chakkraband MLS, Thienkrua W, et al. Mental health problems among adults in tsunami-affected areas in southern Thailand. JAMA 2006;296:537–48. 10.1001/jama.296.5.537 [DOI] [PubMed] [Google Scholar]
- 21.Avoidance behavior. (n.d.) Miller-Keane encyclopedia and dictionary of medicine, nursing, and allied health, seventh edition, 2003. Available: https://medical-dictionary.thefreedictionary.com/Avoidance+behavior [Accessed 08 Dec 2021].
- 22.Gräsner J-T, Lefering R, Koster RW, et al. EuReCa ONE-27 nations, one Europe, one registry: a prospective one month analysis of out-of-hospital cardiac arrest outcomes in 27 countries in Europe. Resuscitation 2016;105:188–95. 10.1016/j.resuscitation.2016.06.004 [DOI] [PubMed] [Google Scholar]
- 23.Gabriel R, Mattias R, Martin J. Survival in out-of-hospital cardiac arrest after standard cardiopulmonary resuscitation or chest compressions only before arrival of emergency medical services: nationwide study during three guideline periods. Circulation 2019;139:2600–9. [DOI] [PubMed] [Google Scholar]
- 24.Fire and Disaster Management Agency (Japan) . Rescue operations and first-aid, 2010. Available: https://www.fdma.go.jp/pressrelease/houdou/items/h23/2312/231216_1houdou/02_1.pdf [Accessed 08 Dec 2021].
- 25.Fire and Disaster Management Agency (Japan) . Rescue operations and first-aid, 2011. Available: https://www.fdma.go.jp/publication/rescue/items/kkkg_h24_01_kyukyu.pdf [Accessed 08 Dec 2021].
- 26.Fire and Disaster Management Agency (Japan) . Rescue operations and first-aid, 2012. Available: https://www.fdma.go.jp/publication/rescue/items/kkkg_h25_01_kyukyu.pdf [Accessed 08 Dec 2021].
- 27.Greif R, Lockey AS, Conaghan P, et al. European resuscitation Council guidelines for resuscitation 2015: section 10. education and implementation of resuscitation. Resuscitation 2015;95:288–301. 10.1016/j.resuscitation.2015.07.032 [DOI] [PubMed] [Google Scholar]
- 28.Portal Site of Official Statistics of Japan website . Population census, 2010. Available: http://www.stat.go.jp/english/data/kokusei/2010/summary.html [Accessed 08 Dec 2021].
- 29.Fire and Disaster Management Agency (Japan) . Report, 2013. Available: https://www.fdma.go.jp/singi_kento/kento/kento098.html [Accessed 08 Dec 2021].
- 30.Ministry of Health, Labor and Welfare (Japan) . Overview of 2011 vital statistics, death situation due to the great East Japan earthquake from the viewpoint of vital statistics. (in Japanese. Available: https://www.mhlw.go.jp/toukei/saikin/hw/jinkou/kakutei11/dl/14_x34.pdf [Accessed 08 Dec 2021].
- 31.Maeda M, Oe M. Mental health consequences and social issues after the Fukushima disaster. Asia Pac J Public Health 2017;29:36S–46. 10.1177/1010539516689695 [DOI] [PubMed] [Google Scholar]
- 32.Tanigawa K, Iwami T, Nishiyama C, et al. Are trained individuals more likely to perform bystander CPR? an observational study. Resuscitation 2011;82:523–8. 10.1016/j.resuscitation.2011.01.027 [DOI] [PubMed] [Google Scholar]
- 33.Kitamura T, Kiyohara K, Sakai T, et al. Public-Access defibrillation and out-of-hospital cardiac arrest in Japan. N Engl J Med 2016;375:1649–59. 10.1056/NEJMsa1600011 [DOI] [PubMed] [Google Scholar]
- 34.Mathiesen WT, Bjørshol CA, Kvaløy JT, et al. Effects of modifiable prehospital factors on survival after out-of-hospital cardiac arrest in rural versus urban areas. Crit Care 2018;22:99. 10.1186/s13054-018-2017-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Takei Y, Nishi T, Matsubara H, et al. Factors associated with quality of bystander CPR: the presence of multiple rescuers and bystander-initiated CPR without instruction. Resuscitation 2014;85:492–8. 10.1016/j.resuscitation.2013.12.019 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-055640supp001.pdf (70.1KB, pdf)
bmjopen-2021-055640supp002.pdf (75.8KB, pdf)
Data Availability Statement
Data sharing not applicable as no datasets generated and/or analysed for this study. No additional data available.