Abstract
Background
Even though realignment procedures have gained popularity as concomitant techniques in cartilage repair approaches with underlying malalignment, the clinical efficacy has not been proven to full extent.
Methods
Out of 5474 patients from the German Cartilage Registry, 788 patients with focal cartilage defects on the medial femoral condyle having received either no accompanying surgery or high tibial osteotomy (HTO) were identified. After a 1:1 propensity score matching, outcome of 440 patients was evaluated using KOOS (Knee Injury and Osteoarthritis Outcome Score), VAS (visual analogue scale), and satisfaction during the 3-year follow-up.
Results
Patients having received a concomitant HTO had significantly higher postoperative KOOS values (12 months: 67.26 ± 15.69 vs.75.10 ± 16.12, P = 0.001; 24 months: 67.14 ± 23.85 vs. 77.11 ± 16.50, P = 0.010; 36 months: 74.40 ± 16.57 vs. 81.75 ± 14.22, P = 0.023) and lower pain levels (6 months: 3.43 ± 2.18 vs. 2.89 ± 2.15, P = 0.009; 12 months: 3.64 ± 2.20 vs. 2.17 ± 1.96, P < 0.001; 24 months: 4.20 ± 3.12 vs. 2.94 ± 2.45, P = 0.005; 36 months: 3.20 ± 2.18 vs. 2.02 ± 1.98, P = 0.003). One and 3 years postoperatively, concomitant HTO led to significantly higher satisfaction in patients. These advantages of accompanying HTO were also seen in the group of patients with a varus deformity of 5° or more, in which pain levels without concomitant HTO even increased during the 3-year follow-up.
Conclusion
The results of the present study underline the importance and safety of concomitant HTO in patients with cartilage defects and varus deformity. HTO should therefore be considered and recommended generously in patients with focal cartilage defects of the medial femoral condyle and varus deformity.
Keywords: cartilage repair, repair, osteotomy, procedures, microfracture, procedures, cartilage transplantation, grafts
Introduction
Ever since the introduction of innovative techniques for repair and regeneration of articular cartilage such as bone marrow stimulation (BMS) 1 and cell transplantation techniques, 2 the relevance of identifying underlying pathologies causing the cartilage defects and their concomitant treatment has been recognized with increasing interest.3-5
For cartilage defects located on the medial femoral condyle (MFC) varus deformity is one of the major underlying pathologies leading to a significant increase of forces in the medial compartment.4,6 Biomechanical studies proved potential of high tibial osteotomy (HTO) in terms of load reduction in the medial compartment 7 and further on the efficiency in peak pressure reduction in focal cartilage defects associated with varus deformity. 4
Furthermore, in an analysis of more than 1,700 patients suffering from cartilage defects of the knee, Spahn et al. 8 were able to describe a significant correlation between malalignment and defect location; varus deformity was the most common underlying pathology for defects of the medial compartment.
In order to address both cartilage defect and underlying pathology, valgization osteotomies such as HTOs come into focus. An earlier study could demonstrate that there was significant improvement in terms of “survival” of the cartilage procedure even in deformities less than 5°. 3 Furthermore, in a recent analysis of patients included in the German Cartilage Registry (KnorpelRegister DGOU), it could be shown that in German-speaking countries contributing their data to this registry, there is a clear trend toward conducting additional HTO even in smaller deformities. 9
Nevertheless, this study could not provide any data on clinical outcome and therefore on efficacy of combined osteotomy and cartilage repair procedures. Outcome analysis was part of the present study, which reports a large patient cohort based on data from the German Cartilage Registry and focuses on a direct comparison of isolated cartilage repair versus combined realignment and cartilage repair in a matched cohort setting.
Methods
Data Collection
Data from the KnorpelRegister DGOU were used for the present analysis. The KnorpelRegister DGOU is an observational, nation-wide, and longitudinal multicenter registry of patients assigned for surgical treatment of cartilage defects of the knee and aims to determine real-life treatment patterns and clinical outcomes. The registry was initiated by the Working Group Clinical Tissue Regeneration of the German Society for Orthopedics and Trauma (DGOU) in 2013. Since then, the number of sites has increased to 120. The registry is conducted in accordance with the Declaration of Helsinki and registered at germanctr.de (DRKS00005617). The current study was approved by the Ethics Commission of the Medical Center–University of Freiburg: EK-FR 105/13_130795).
All patients aged 18 years and older who meet the following criteria are eligible to take part in the German Cartilage Registry: surgical treatment of cartilage defects of the knee, ankle or hip joint at a participating site, signed written informed consent, and possession of a personal email address.
Until February 2020, 5474 patients assigned for surgical treatment of cartilage defects of the knee had been included in the registry.
Data collection is performed using a web-based RDE System “RDE-Light,” which was developed by the Clinical Trials Unit (Freiburg) as an electronic data entry interface and data management system for clinical studies and other projects in clinical research. Data are collected paperless and directly on site via an internet browser. Forms are based on HTML- and PDF-format. RDE-Light is available in various languages and validated according to GAMP 5. Furthermore, it fulfills all requirements of Good Clinical Practice (GCP). Established security standards like cryptographic security protocols (SSL/TLS), user authentication protocols and authorization concepts are applied.
After the patient signs the written informed consent the investigator is allowed to register the patient to the database. Patient- and defect-specific parameters are reported by the treating physician at the time of surgery.
Patient satisfaction is evaluated by a 4-item score (not satisfied, partially satisfied, satisfied, very satisfied) at every follow-up point (6, 12, 24, and 36 months postoperatively).
Functional outcome was assessed by visual analogue scale (VAS) and Knee Injury and Osteoarthritis Outcome Score (KOOS) score at 0 months (preoperatively) and after 6, 12, 24, and 36 months postoperatively.
The German Cartilage Registry is supported by a grant from the “Oscar-Helene-Stiftung” and the “Deutsche Arthrosehilfe e.V.”
Data Selection
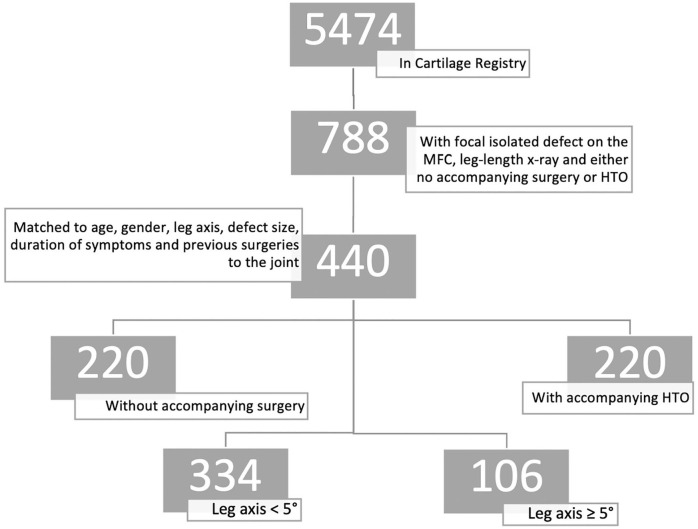
For the present study, only cases with isolated focal defects of the MFC in patients with existing leg-length x-rays having received either no accompanying surgery (group cartilage repair [CR]) or an accompanying HTO (group CR/HTO) were analyzed (n = 788) ( Fig. 1 ).
Figure 1.
Selection process of patients included in the underlying analysis.
Propensity Score Matching and Statistical Analysis
To reduce the bias resulting from the nonrandomized nature of the present analysis and to enhance comparability between the 2 treatment groups (without accompanying HTO [group CR] vs. accompanying surgery [group CR/HTO]), a 1:1 propensity score matching with replacement was performed with the built-in Propensity-Score plug-in of the SPSS V.26 software. Patients were matched by propensity score based on age, gender, leg axis (based on the hip-knee-angle), size of defect, duration of symptoms and previous operations on the joint. After matching with a tolerance of 0.006, a total of 220 patients with accompanying HTO were matched to 220 patients without accompanying surgery with similar patient characteristics.
Chi-square test was used to compare categorial variables and unpaired t test to compare continuous variables. Normal distribution was assessed visually by using Q-Q-plots. P values <0.05 were considered statistically significant. SPSS statistics version 26 was used to analyze the data.
Results
Patient Characteristics
The preoperative patient characteristics of the cohort of patients with isolated focal chondral defects of the MFC and preoperative leg-length x-ray are shown in Table 1 . A total of 788 patients fulfilling the aforementioned criteria could be identified. Group CR/HTO consisted of 250 patients (31.7%) while 538 (68.3%) patients were included in group CR. The patients in the CR/HTO group were older, had larger cartilage defects, longer symptom duration, more previous surgeries to the joint, were more often male, had a worse meniscus status and a more severely injured corresponding joint surface in accordance with higher degrees of malalignment in terms of varus deformity. Since these preoperative baseline characteristics could affect the postoperative outcome a 1:1 nearest neighbor propensity score matching was conducted to reduce the bias in evaluating the best practice in patients with varus deformity and chondral defects of the MFC.
Table 1.
Baseline Patient Characteristics of All Patients Fulfilling the Inclusion Criteria (see Fig. 1 ) before Matching. a
| CR |
CR/HTO |
P | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | Standard Deviation | Mean | Standard Deviation | ||||||||
| Degree varus, deg | 1.76 | 2.38 | 5.65 | 2.79 | <0.01 | ||||||
| Defect size, mm | 384.7 | 204.74 | 437.71 | 221.93 | 0.01 | ||||||
| Age, y | 37.88 | 12.59 | 41.37 | 11.03 | <0.01 | ||||||
| Symptom duration, mo | 21.04 | 33.34 | 28.56 | 43.33 | 0.016 | ||||||
| Previous surgeries, n | 0.74 | 0.98 | 1.02 | 1.05 | <0.01 | ||||||
| Previous surgeries on the cartilage, n | 0.41 | 0.712 | 0.43 | 0.732 | 0.725 | ||||||
| Gender | Male | Female | Male | Female | <0.01 | ||||||
| 53.90% | 46.10% | 79.6% | 20.40% | ||||||||
| Defect stadium | NA | I | II | IIIa/IIIb | IVa/IVb | NA | I | II | IIIa/IIIb | IVa/IVb | 0.254 |
| 0.90% | 0.70% | 0.90% | 39.20% | 58.20% | 0.40% | 0.00% | 0.00% | 37.60% | 62.00% | ||
| Corresponding joint surface | Intact | I°-II° | III-IV | Intact | I°-II° | III-IV | <0.01 | ||||
| 71.90% | 27.80% | 0.30% | 46.00% | 44.00% | 10.00% | ||||||
| Smoking status | Smoker | Nonsmoker | Ex-smoker | Smoker | Nonsmoker | Ex-smoker | 0.125 | ||||
| 25.30% | 71.50% | 3.20% | 22.00% | 72.00% | 6% | ||||||
| Meniscus status | Intact | <1/3 resected | >1/3 resected | Other | Intact | <1/3 resected | >1/3 resected | Other | <0.01 | ||
| 68.60% | 26.00% | 4.40% | 1.00% | 51.60% | 28.70% | 16.80% | 2.90% | ||||
CR = cartilage repair; HTO = high tibial osteotomy; NA = not applicable.
Significantly differing values are in boldface.
After matching, 220 couples (440 patients) were identified. The baseline characteristics of the matched cohort without any significant characteristics beyond the matched variables are shown in Table 2 . Since the categoric variables could not be matched, the corresponding joint surface and the defect stadium remained higher in the group of patients who received an accompanying HTO.
Table 2.
Baseline Patient Characteristics after Matching. a
| CR |
CR/HTO |
P | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | Standard Deviation | Mean | Standard Deviation | ||||||||
| Degree varus, deg | 5,80 | 3.52 | 5.64 | 2.8 | 0.59 | ||||||
| Defect Size, mm | 421.67 | 242.75 | 427.59 | 214.09 | 0.78 | ||||||
| Age, y | 42.80 | 11.89 | 41.95 | 11.01 | 0.44 | ||||||
| Symptom duration, mo | 22.63 | 42.88 | 28.85 | 44.7 | 0.13 | ||||||
| Previous surgeries, n | 0.98 | 1.01 | 1.01 | 1.06 | 0.78 | ||||||
| Previous surgeries on the cartilage, n | 0.37 | 0.57 | 0.41 | 0.71 | 0.46 | ||||||
| Gender | Male | Female | Male | Female | 0.123 | ||||||
| 71.80% | 28.20% | 78.20% | 21.80% | ||||||||
| Unmatched factors | |||||||||||
| Defect stadium | NA | I | II | IIIa/IIIb | IVa/IVb | NA | I | II | IIIa/IIIb | IVa/IVb | 0.025 |
| 0.00% | 0.00% | 2.30% | 45.00% | 52.70% | 0.50% | 0.00% | 0.00% | 37.30% | 62.30% | ||
| Corresponding joint surface | Intact | I°-II° | III-IV | Intact | I°-II° | III-IV | <0.01 | ||||
| 52.13% | 47.87% | 0% | 44.00% | 45.50% | 10.50% | ||||||
| Smoking status | Smoker | Nonsmoker | Ex-smoker | Smoker | Nonsmoker | Ex-smoker | 0.783 | ||||
| 20.40% | 72.70% | 6.90% | 22.70% | 71.40% | 5.90% | ||||||
| Meniscus status | Intact | <1/3 resected | >1/3 resected | Other | Intact | <1/3 resected | >1/3 resected | Other | 0.058 | ||
| 47.20% | 40.00% | 11.40% | 1.40% | 51.60% | 28.80% | 17.30% | 2.30% | ||||
CR = cartilage repair; HTO = high tibial osteotomy; NA = not applicable.
Categorial variables remained unmatched. Significantly differing values are in boldface.
Type of Cartilage Treatment
While the majority of patients received autologous chondrocyte implantation (ACI) as cartilage regenerative therapy, most patients with accompanying HTO were treated by BMS (5.1% vs. 19.4%) ( Table 3 ).
Table 3.
Type of Cartilage Treatment in Groups with and without Accompanying HTO.
| CR |
CR/HTO |
|||
|---|---|---|---|---|
| Number | Percentage | Number | Percentage | |
| Drilling | 0 | 0.0 | 0 | 0.0 |
| BMS | 11 | 5.1 | 42 | 19.4 |
| OCT | 9 | 4.1 | 4 | 1.8 |
| ACI | 76 | 35.0 | 82 | 37.8 |
| ACI and Spongiosa | 30 | 13.8 | 38 | 17.5 |
| Matrix-BMS | 8 | 3.7 | 10 | 4.6 |
| Debridement | 11 | 5.1 | 10 | 4.6 |
| Other | 58 | 26.7 | 24 | 11.1 |
| Multiple therapies | 14 | 6.5 | 7 | 3.2 |
CR = cartilage repair; HTO = high tibial osteotomy; ACI = autologous chondrocyte implantation; BMS = bone marrow stimulation; OCT = osteochondral transplantation.
Overall Outcome
KOOS
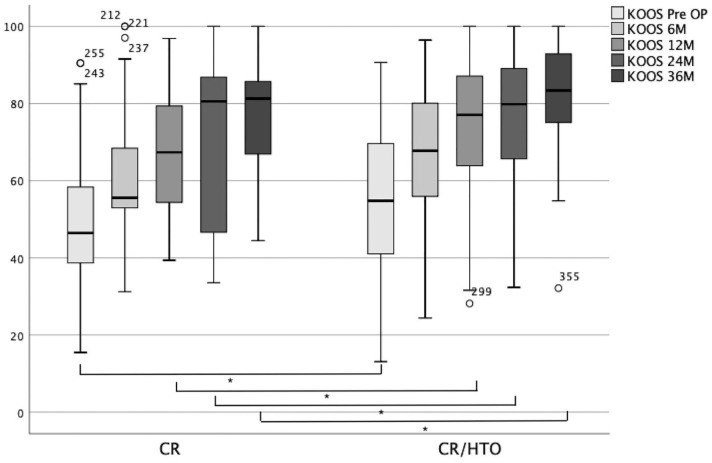
Patients in the CR/HTO group had significantly higher postoperative KOOS values from 12 to 36 months postoperatively (12 months: 67.26 ± 15.69 vs. 75.10 ± 16.12, P = 0.001; 24 months: 67.14 ± 23.85 vs. 77.11 ± 16.50, P = 0.010; 36 months: 74.40 ± 16.57 vs. 81.75 ± 14.22, P = 0.023) (see Table 4 and Fig. 2 ). The preoperative KOOS was also significantly higher in the CR/HTO group (49.62 ± 15.38 vs. 54.97 ± 18.78, P = 0.010). Values from patients without accompanying HTO are always mentioned first according to the provided tables.
Table 4.
Outcome Measures (KOOS, VAS, and Satisfaction) of Patients With Isolated CR Compared to Those with CR and Accompanying HTO (CR/HTO). a
| CR |
CR/HTO |
P | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | Standard Deviation | Mean | Standard Deviation | ||||||
| KOOS—0M | 49.62 | 15.38 | 54.97 | 18.78 | 0.010 | ||||
| KOOS—6M | 60.06 | 16.74 | 66.28 | 17.40 | 0.080 | ||||
| KOOS—12M | 67.26 | 15.69 | 75.10 | 16.13 | 0.001 | ||||
| KOOS—24M | 67.14 | 23.85 | 77.11 | 16.50 | 0.010 | ||||
| KOOS—36M | 74.40 | 16.57 | 81.75 | 14.22 | 0.023 | ||||
| VAS—Preoperative | 3.76 | 2.38 | 3.99 | 2.38 | 0.078 | ||||
| VAS—FU6 | 3.43 | 2.18 | 2.89 | 2.15 | 0.009 | ||||
| VAS—FU12 | 3.64 | 2.20 | 2.17 | 1.95 | <0.001 | ||||
| VAS—FU24 | 4.20 | 3.12 | 2.94 | 2.45 | 0.005 | ||||
| VAS—FU36 | 3.20 | 2.18 | 2.02 | 1.98 | 0.003 | ||||
| Not Satisfied | Partially Satisfied | Satisfied | Very Satisfied | Not Satisfied | Partially Satisfied | Satisfied | Very Satisfied | P | |
| Satisfaction—FU6 | 0.0% | 20.2% | 51.0% | 28.8% | 6.8% | 28.8% | 42.4% | 22.0% | 0.013 |
| Satisfaction—FU12 | 2.7% | 42.7% | 34.7% | 20.0% | 3.7% | 23.1% | 46.3% | 26.9% | 0.049 |
| Satisfaction—FU24 | 11.8% | 43.1% | 19.6% | 25.5% | 14.6% | 23.2% | 35.4% | 26.8% | 0.074 |
| Satisfaction—FU36 | 0.0% | 19.6% | 63.0% | 17.4% | 6.7% | 8.9% | 44.4% | 40.0% | 0.015 |
CR = cartilage repair; HTO = high tibial osteotomy; KOOS = Knee Injury and Osteoarthritis Outcome Score; VAS = visual analogue scale; FU = follow-up.
Significantly differing values are in boldface.
Figure 2.
Outcome (Knee Injury and Osteoarthritis Outcome Score [KOOS]) of patients with cartilage repair (CR) alone compared to patients with concomitant HTO (CR/HTO) preoperative (light gray—left), as well as 6, 12, 24 and 36 (dark gray—right) months postoperatively.
Pain
Throughout the whole follow-up period, higher pain scores were reported by patients who received the cartilage treatment without concomitant surgery even though preoperative pain scores were equal in both groups (3.76 ± 2.38 vs. 3.99 ± 2.38, P = 0.078) (see Table 4 ). HTO reduced postoperative pain scores significantly (VAS at 6 months: 3.43 ± 2.18 vs. 2.89 ± 2.15, P = 0.009; VAS at 12 months: 3.64 ± 2.20 vs. 2.17 ± 19.6, P < 0.001; VAS at 24 months: 4.20 ± 3.12 vs. 2.94 ± 2.45, P = 0.005; VAS at 36 months: 3.20 ± 2.18 vs. 2.02 ± 1.98, P = 0.003).
Satisfaction
While patients in the CR group initially (6-month follow-up [FU6]) reported higher satisfaction rates (0.0% not satisfied, 20.2% partially satisfied, 51.0% satisfied, 28,8% very satisfied vs. 6.8% not satisfied, 28.8% partially satisfied 42.4% satisfied, 22.0% very satisfied, P = 0.013), these findings reversed at 1 year (2.7% not satisfied, 42.7% partially satisfied, 34.7% satisfied, 20.0% very satisfied vs. 3.7% not satisfied, 23.1% partially satisfied 46.3% satisfied, 26.9% very satisfied, P = 0.049) FU and persisted even after 3 years (0.0% not satisfied, 19.6% partially satisfied, 63.0% satisfied, 17.4% very satisfied vs. 6,7% not satisfied, 8.9% partially satisfied 44.4% satisfied, 40.0% very satisfied, P = 0.015), whereas patients in the CR/HTO group reported higher satisfaction scores 6, 12, and 36 months after the operation (see Table 4 ).
Outcome in Dependence of Amount of Varus Deformity
To compare outcome in patients with varus deformity <5° (group A) and those with ≥5° (group B) 2 separate groups were established out of our propensity score–matched cohort of 440 patients. Group A consisted of 106 patients and group B of 334. The patient characteristics of both groups vary regarding positive and negative outcome predicting factors (see Table 5 ).
Table 5.
Baseline Characteristics of Patients with <5° Varus and Patients with ≥5° Varus within the Cohort of 440 Patients.
| Leg Axis <5° (Group
A) |
Leg Axis ≥5° (Group B) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | Standard Deviation | Mean | Standard Deviation | |||||||
| Degree varus, deg | 2.08 | 1.01 | 6.88 | 2.73 | ||||||
| Defect size, mm | 472.57 | 245.83 | 409.42 | 221.12 | ||||||
| Age, y | 39.26 | 11.66 | 43.36 | 11.23 | ||||||
| Symptom duration, mo | 35.78 | 55.66 | 22.55 | 38.95 | ||||||
| Previous surgeries, n | 1.31 | 1.11 | 0.90 | 1.00 | ||||||
| Previous surgeries on the cartilage, n | 0.48 | 0.80 | 0.36 | 0.60 | ||||||
| Gender | Male | Female | Male | Female | ||||||
| 85.8% | 14.2% | 71.6% | 28.4% | |||||||
| Defect stadium | NA | I | II | IIIa/IIIb | IVa/IVb | NA | I | II | IIIa/IIIb | IVa/IVb |
| 0.0% | 0.0% | 0.0% | 27.4% | 72.6% | 2.1% | 0.0% | 1.5% | 45.5% | 52,7% | |
| Corresponding joint surface | Intact | I°-II° | III-IV | Intact | I°-II° | III-IV | ||||
| 57.5% | 41.5% | 0.9% | 44.9% | 48.3% | 6.8% | |||||
| Smoking status | Smoker | Nonsmoker | Ex-smoker | Smoker | Nonsmoker | Ex-smoker | ||||
| 20.6% | 71.6% | 7.8% | 21.9% | 72.2% | 6.0% | |||||
| Meniscus status | Intact | <1/3 resected | >1/3 resected | Other | Intact | <1/3 resected | >1/3 resected | Other | ||
| 61.9% | 32.4% | 5.7% | 1.0% | 45.8% | 35.2% | 17.0% | 2.1% | |||
NA = not applicable.
In group, A no significant difference in terms of improved KOOS, VAS, or satisfaction could be observed between patients having received a concomitant HTO and those who had not ( Table 6 ).
Table 6.
Outcome Values in Patients with leg axis under 5° vs. 5° and over with and without accompanying HTO.
| Leg Axis <5° (Group
A) |
P | Leg Axis ≥5° (Group B) |
P | |||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CR | CR/HTO | CR | CR/HTO | Mean | Standard Deviation | Mean | Standard Deviation | Mean | Standard Deviation | Mean | Standard Deviation | KOOS—0M | ||||||||||||||||||||||
| 51.87 | 18.19 | 56.94 | 19.11 | 0.268 | 48.70 | 14.08 | 54.47 | 18.74 | 0.012 | |||||||||||||||||||||||||
| KOOS—6M | 74.29 | 16.36 | 69.49 | 17.23 | 0.273 | 53.58 | 12.41 | 65.30 | 17.42 | <0.001 | ||||||||||||||||||||||||
| KOOS—12M | 74.46 | 16.68 | 75.50 | 15.68 | 0.807 | 62.55 | 13.17 | 74.96 | 16.36 | <0.001 | ||||||||||||||||||||||||
| KOOS—24M | 79.27 | 15.02 | 79.85 | 14.93 | 0.905 | 61.59 | 25.22 | 76.09 | 17.05 | 0.004 | ||||||||||||||||||||||||
| KOOS—36M | 80.43 | 16.05 | 80.87 | 14.37 | 0.948 | 72.51 | 16.50 | 81.98 | 14.37 | 0.011 | ||||||||||||||||||||||||
| VAS—Preoperative | 3.79 | 2.55 | 3.85 | 2.28 | 0.912 | 3.74 | 2.30 | 4.02 | 2.41 | 0.384 | ||||||||||||||||||||||||
| VAS—FU6 | 1.94 | 1.94 | 2.76 | 2.12 | 0.113 | 4.17 | 1.90 | 2.92 | 2.17 | <0.001 | ||||||||||||||||||||||||
| VAS—FU12 | 2.38 | 1.60 | 2.42 | 1.81 | 0.927 | 4.67 | 2.10 | 2.09 | 2.00 | <0.001 | ||||||||||||||||||||||||
| VAS—FU24 | 2.56 | 2.01 | 2.68 | 2.32 | 0.857 | 5.13 | 3.27 | 3.03 | 2.51 | 0.003 | ||||||||||||||||||||||||
| VAS—FU36 | 2.27 | 2.61 | 2.27 | 2.15 | 1.000 | 3.49 | 1.98 | 1.94 | 1.95 | 0.002 | ||||||||||||||||||||||||
| Not Satisfied | Partially Satisfied | Satisfied | Very Satisfied | Not Satisfied | Partially Satisfied | Satisfied | Very Satisfied | P | Not Satisfied | Partially Satisfied | Satisfied | Very Satisfied | Not Satisfied | Partially Satisfied | Satisfied | Very Satisfied | P | |||||||||||||||||
| Satisfaction—FU6 | 0.0% | 20.0% | 51.4% | 28.6% | 3.4% | 27.6% | 44.8% | 24.1% | 0.603 | 0.0% | 20.3% | 50.7% | 29.0% | 7.8% | 29.1% | 41.7% | 21.4% | 0.040 | ||||||||||||||||
| Satisfaction—FU12 | 0.0% | 25.0% | 41.7% | 33.3% | 7.7% | 15.4% | 57.7% | 19.2% | 0.149 | 5.1% | 59.0% | 28.2% | 7.7% | 2.4% | 25.6% | 42.7% | 29.3% | 0.001 | ||||||||||||||||
| Satisfaction—FU24 | 10.5% | 42.1% | 15.8% | 31.6% | 8.7% | 21.7% | 43.5% | 26.1% | 0.249 | 12.5% | 43.8% | 21.9% | 21.9% | 16.9% | 23.7% | 32.2% | 27.1% | 0.265 | ||||||||||||||||
| Satisfaction—FU36 | 0.0% | 18.2% | 45.5% | 36.4% | 0.0% | 0.0% | 63.6% | 36.4% | 0.311 | 0.0% | 20.0% | 68.6% | 11.4% | 8.8% | 11.8% | 38.2% | 41.2% | 0.006 | ||||||||||||||||
CR = cartilage repair; HTO = high tibial osteotomy; KOOS = Knee Injury and Osteoarthritis Outcome Score; VAS = visual analogue scale; FU = follow-up.
Significantly differing values are in boldface.
In group B, HTO led to a significantly improved KOOS score throughout the whole follow-up period ( Table 6 ). Average preoperative pain score was equal between patients with and without accompanying HTO in group B but postoperatively patients having received an accompanying HTO had significant less pain than those who had not ( Table 6 ). In group B patients who did now undergo concomitant HTO showed increased pain levels from preoperative up to 2 years postoperatively; at the 3-year FU, the average pain score sank below preoperative values for the first time. The pain score in patients with accompanying HTO was below preoperative levels throughout the whole follow-up period and was reduced by 51.7% compared with preoperative values 3 years after surgery.
Regarding subjective satisfaction rates, a high number of patients in all 4 groups were apparently unsatisfied after 2 years FU (group A: without HTO 10.5%, with HTO 8.7%; group B: without HTO 12.5%, with HTO 16.9%). Patients in group B without HTO were significantly more satisfied initially (FU 6 months, P = 0.040), while reversed results were seen at one and 3 years were HTO led to significantly higher subjective satisfaction rates (FU 12 months, P = 0.001; FU 36 months, P = 0.006).
Nonetheless, the absolute share of “not satisfied” patients with leg axis ≥5° is larger after receiving accompanying HTO, while the overall satisfaction rate is higher (36 months: 11.4% vs. 41.2% “very satisfied,” P = 0.006).
Discussion
This is the first study presenting large cohort data after HTO and cartilage versus cartilage repair alone in patients with cartilage defect of the medial compartment of the knee. In contrast to earlier studies,10,11 this study was initiated to not only compare event-free survival but also functional outcome after combined HTO and CR versus isolated CR in a large cohort of patients with focal cartilage defects of the medial compartment of the knee.
Despite the large number of patients involved in this study, patients with cartilage defects of the knee represent a heterogenous cohort in terms of concomitant pathologies and in many scientific reports there is no reliable discrimination between patients with focal cartilage defects and early or even progressed osteoarthritis.10-12 This is of extraordinary importance since osteoarthritis is still the most relevant contraindication for any type of cartilage repair. Moreover, various factors, including not only integrity of the corresponding joint surface, meniscus status, duration of symptoms, and gender but also defect size and several other parameters can influence clinical outcome following different types of cartilage repair. For this purpose, in the present study a 1:1 nearest neighbor propensity score matched cohort of 440 patients from the German Cartilage Registry was analyzed in order to evaluate the effect of concomitant HTO to the best possible degree.
In the unmatched cohort, patients who received the cartilage surgery alone were younger, had smaller defects, a shorter duration of symptoms, less previous surgeries to the joint, were more often female, had a better meniscus status and a less severely injured corresponding joint surface and a lower amount of leg axis malalignment ( Table 1 ). 8 As a consequence, it was necessary to even out those differences before conducting an elaborate analysis ( Table 1 ). After the matching process, mean values of age, defect size, symptom duration, number of previous surgeries to the joint and the cartilage defect, degree of leg axis malalignment, and sex distribution were equal in the groups of patients with and without concomitant HTO ( Table 2 ). Categorial variables (defect stadium and corresponding joint surface integrity) remained unmatched, since categorial variables with more than 2 values are not covered well by the propensity score. This leads to a more integer corresponding joint surface and a lower defect stadium in patients without accompanying HTO. These 2 factors need to be discussed when interpreting outcome parameters of the 2 analyzed patient groups (with vs. without HTO). 13 Nevertheless, the matching process led to a homogenous distribution of various parameters with potential effect on functional outcome.
Based on the analysis of the 440 propensity score matched patients involved in the present study, major findings were that concomitant HTO leads to significantly higher KOOS values and lower pain scores 1, 2, and 3 years postoperatively ( Table 4 ). In patients with a cartilage defect of the medial femoral condyle having undergone isolated cartilage procedure, the mean pain level 2 years after the intervention even increased compared to preoperative levels, whereas concomitant HTO led to consistently lower postoperative pain levels. Moreover, an accompanying HTO led to more satisfied patients 1 and 3 years after the intervention ( Table 4 ). The rate of reinterventions was equal in both groups. In the cohort with a leg axis of 5° varus and more similar results as in the overall cohort in terms of better KOOS, lower pain, and higher patient satisfaction in patients with concomitant HTO could be shown. Even in the cohort of patients with deformities of less than 5° improved functional outcome could be demonstrated, however not significantly better compared to patients without accompanying HTO ( Table 6 ). Interestingly, 2 years postoperatively in all groups (CR, CR/HTO, groups A and B) the worst results regarding pain and satisfaction could be shown, even though KOOS did not show poor results at 24 months ( Tables 4 and 6). This finding is difficult to put into context and lacks a well-founded explanation.
Although the effect and necessity of concomitant osteotomy in cartilage repair has been generally accepted, it has never been shown so clearly in terms of improved functional outcome. Nevertheless, these results are in line with earlier studies (in vitro and in vivo) that suggest positive effects of unloading on regeneration of cartilage and the opposite for malalignment resulting in an overload and asymmetric load of the joint. Progression of untreated cartilage defects could be also shown in vitro and in vivo,14,15 probably resulting from the fact that the contact pressure concentrates around the rims of cartilage defects, 4 Especially in patients with varus malalignment, which is a proven risk factor for cartilage lesions of the medial compartment, 8 the underlying pathology needs to be addressed when cartilage repair is carried out to prevent further degeneration. 16 High tibial osteotomy with at least 50% release of the medial collateral ligament leads to reduced pressure in the medial compartment and on the preexisting cartilage defect.4,7
Good results of HTO combined with cartilage repair have been shown in terms of pain and patient-reported outcome measures, and HTO has proven feasible and safe.17-21 The present analysis supports this data. A recent systematic review depicted almost 100% return to work rates after ACI plus HTO whereas a significantly less number of patients (51.78%) returned to their former work activity after osteochondral allograft transplantation. 22 HTO in combination with ACI also led to the shortest return to work time (3.15 months) compared to ACI alone (3.34 months) and osteochondral allograft (11.1 months). Multiple studies and even systematic reviews and meta-analyses on the effect of high tibial osteotomy with a concomitant “cartilage procedure” in osteoarthritic knees compared with HTO alone exist,11,23-27 but literature about cartilage procedures with versus without concomitant high tibial osteotomy in patients with focal cartilage defects is sparse. Here the difference between focal cartilage defects and osteoarthritis needs to be emphasized. Whereas the average age of the described patients in the studies comparing HTO to HTO with concomitant “cartilage procedures” is between 50 and 64 years, 11 the average age in the German Cartilage Registry is 37.26 ± 12.53 and in our matched cohort 42.38 ± 11.46 years. Multiple studies have dealt with the question of survivorship and revision free survival of high tibial osteotomies in the treatment of osteoarthritis of the knee.10,12,28 The mean patient age between 50 and 54 years needs to be considered here. To date, publications dealing with the question of functional outcome of concomitant HTO in a cohort of young patients with focal cartilage defects of the knee are lacking. Also, concerning what degree of deformity requires a correction of varus malalignment, a limit of 5° became common sense29-32 without any scientific evidence. In patients with cartilage defects of the medial femoral condyle and varus deformity of <5° who received concomitant HTO with ACI lower failure rates (2/19 vs. 10/24) were observed compared with patients who received ACI alone. 3 Even though this 5° limit seems to be outdated and the trend goes toward performing HTO even in less severe leg axis deformities, 9 there has neither been any supporting scientific evidence until now, nor have data concerning functional outcome of cartilage repair accompanying HTO in large cohorts been published.
In the overall cohort with a mean varus deformity of 5.80 ± 3.52 (CR) and 5.64 ± 2.80 (CR/HTO) degrees, respectively, the benefit of a concomitant HTO in terms of KOOS, pain, and patient satisfaction could be shown even though patients who received the cartilage procedure alone had a more integer corresponding joint surface and a less severe defect stadium. This benefit was also shown in patients with a varus deformity of 5° or more. In patients with a varus deformity of less than 5°, the superiority of concomitant HTO in terms of functional outcome could not be shown during a 3-year follow-up, confirming the results of Bode et al. 3 This advantage of a concomitant HTO was shown, even though patients in the CR/HTO group had a less integer corresponding joint surface, a higher defect size, and underwent more often microfracture compared to the group of patients who received the cartilage procedure alone. The type of cartilage treatment was not die primary aim the present study and therefore it has not been included in the propensity matching, nevertheless it might influence outcome. Interestingly. the CR/HTO group BMS was used more frequently (19.4% vs. 5.1%) ( Table 3 ). According to multiple studies,29,33,34 BMS seems inferior, even though the CR/HTO showed better outcomes. Therefore, the inferiority of quality of cartilage repair in the CR/HTO group and the better results respectively might even strengthen the results of the present study.
Even though this study was conducted on a large cohort of patients, it was not possible to carry out a reliable gradually outcome analysis. In further studies, an exact angle at which patient outcome improves significantly from an accompanying high tibial osteotomy should be determined.
Limitations
This study shows several limitations. First of all, due to the fact that this study was based on registry data, input errors from patient and doctor side cannot be ruled out. Second, there has been no information on the type of performed valgisating tibial osteotomy; whether opening or closing wedge osteotomy was performed. In the biggest centers entering data in the registry, opening wedge osteotomy is performed almost exclusively. As a third limitation it must be mentioned that no information about the amount of correction can be made, since this information is not part of the Cartilage Registry. Fourth, propensity score matching has some limitations; the covariates chosen for matching may not be all the confounders affecting the outcome significantly. Influencing covariates might be overseen or not even asked for. So hidden bias due to latent variables may remain after matching.
Conclusion
Concomitant HTO results in better postoperative KOOS values, lower pain levels, and a higher patient satisfaction compared with the cartilage procedure alone in a propensity score–matched cohort. Even greater data sets with longer follow-up durations are needed to carry out a gradually outcome analysis to distinguish a scientific limit of varus deformity where valgization osteotomies accompanying cartilage repair are indicated to improve patient outcome. From a clinical point of view, this article underlines the importance of concomitant HTO in patients with cartilage defects and varus deformity and based on the results of the study, HTO should be considered and recommended generously in these patients.
Footnotes
Acknowledgments and Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article. The German Cartilage registry is supported by a grant from the “Oscar-Helene-Stiftung” and the “Deutsche arthrosehilfe e.V.”
Ethical Approval: The current study was approved by the Ethics Commission of the Medical Center–University of Freiburg: EK-FR 105/13_130795).
Trial Registration: The registry is conducted in accordance with the Declaration of Helsinki and registered at germanctr.de (DRKS00005617).
ORCID iD: Svea Faber  https://orcid.org/0000-0001-6570-1308
https://orcid.org/0000-0001-6570-1308
References
- 1. Steadman JR, Rodkey WG, Singleton SB, Briggs KK. Microfracture technique for full-thickness chondral defects: technique and clinical results. Oper Tech Orthop. 1997;7:300-4. doi: 10.1016/S1048-6666(97)80033-X [DOI] [Google Scholar]
- 2. Brittberg M, Lindahl A, Nilsson A, Ohlsson C, Isaksson O, Peterson L. Treatment of deep cartilage defects in the knee with autologous chondrocyte transplantation. N Engl J Med. 1994;331:889-895. doi: 10.1056/NEJM199410063311401 [DOI] [PubMed] [Google Scholar]
- 3. Bode G, Schmal H, Pestka JM, Ogon P, Sudkamp NP, Niemeyer P. A non-randomized controlled clinical trial on autologous chondrocyte implantation (ACI) in cartilage defects of the medial femoral condyle with or without high tibial osteotomy in patients with varus deformity of less than 5. Arch Orthop Trauma Surg. 2013;133:43-9. doi: 10.1007/s00402-012-1637-x [DOI] [PubMed] [Google Scholar]
- 4. Mina C, Garrett WE, Jr, Pietrobon R, Glisson R, Higgins L. High tibial osteotomy for unloading osteochondral defects in the medial compartment of the knee. Am J Sports Med. 2008;36:949-55. 10.1177/0363546508315471 [DOI] [PubMed] [Google Scholar]
- 5. Mouzopoulos G, Borbon C, Siebold R. Patellar chondral defects: a review of a challenging entity. Knee Surg Sports Traumatol Arthrosc. 2011;19:1990-2001. doi: 10.1007/s00167-011-1546-5 [DOI] [PubMed] [Google Scholar]
- 6. Agneskirchner JD, Hurschler C, Stukenborg-Colsman C, Imhoff AB, Lobenhoffer P. Effect of high tibial flexion osteotomy on cartilage pressure and joint kinematics: a biomechanical study in human cadaveric knees. Winner of the AGA-DonJoy Award 2004. Arch Orthop Trauma Surg. 2004;124:575-84. doi: 10.1007/s00402-004-0728-8 [DOI] [PubMed] [Google Scholar]
- 7. Agneskirchner JD, Hurschler C, Wrann CD, Lobenhoffer P. The effects of valgus medial opening wedge high tibial osteotomy on articular cartilage pressure of the knee: a biomechanical study. Arthroscopy. 2007;23:852-61. doi: 10.1016/j.arthro.2007.05.018 [DOI] [PubMed] [Google Scholar]
- 8. Spahn G, Fritz J, Albrecht D, Angele P, Fickert S, Aurich M, et al. Coincidence and therapy of dysalignments and degenerative knee cartilage lesions. Results from the German Cartilage Registry DGOU. Z Orthop Unfall. 2017;155:457-67. doi: 10.1055/s-0043-108649 [DOI] [PubMed] [Google Scholar]
- 9. Faber S, Zellner J, Angele P, Spahn G, Loer P, Zinser W, et al. Decision making for concomitant high tibial osteotomy (HTO) in cartilage repair patients based on a nationwide cohort study of 4968 patients. Arch Orthop Trauma Surg. 2020;140(10):1437-44. doi: 10.1007/s00402-020-03476-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jin C, Song EK, Santoso A, Ingale PS, Choi IS, Seon JK. Survival and risk factor analysis of medial open wedge high tibial osteotomy for unicompartment knee osteoarthritis. Arthroscopy. 2020;36:535-43. doi: 10.1016/j.arthro.2019.08.040 [DOI] [PubMed] [Google Scholar]
- 11. Lee OS, Ahn S, Ahn JH, Teo SH, Lee YS. Effectiveness of concurrent procedures during high tibial osteotomy for medial compartment osteoarthritis: a systematic review and meta-analysis. Arch Orthop Trauma Surg. 2018;138:227-36. doi: 10.1007/s00402-017-2826-4 [DOI] [PubMed] [Google Scholar]
- 12. Niinimäki TT, Eskelinen A, Mann BS, Junnila M, Ohtoner P, Leppilahti J. Survivorship of high tibial osteotomy in the treatment of osteoarthritis of the knee: Finnish registry-based study of 3195 knees. J Bone Joint Surg Br. 2012;94:1517-21. doi: 10.1302/0301-620X.94B11.29601 [DOI] [PubMed] [Google Scholar]
- 13. Gudas R, Mačiulaitis J, Staškūnas M, Smailys A. Clinical outcome after treatment of single and multiple cartilage defects by autologous matrix-induced chondrogenesis. J Orthop Surg (Hong Kong). 2019;27:2309499019851011. doi: 10.1177/2309499019851011 [DOI] [PubMed] [Google Scholar]
- 14. Everhart JS, Abouljoud MM, Kirven JC, Flanigan DC. Full-thickness cartilage defects are important independent predictive factors for progression to total knee arthroplasty in older adults with minimal to moderate osteoarthritis: data from the osteoarthritis initiative. J Bone Joint Surg Am. 2019;101:56-63. doi: 10.2106/JBJS.17.01657 [DOI] [PubMed] [Google Scholar]
- 15. Schinhan M, Gruber M, Vavken P, Dorotka R, Samouh L, Chiari C, et al. Critical-size defect induces unicompartmental osteoarthritis in a stable ovine knee. J Orthop Res. 2012;30:214-20. doi: 10.1002/jor.21521 [DOI] [PubMed] [Google Scholar]
- 16. Jungmann PM, Gersing AS, Baumann F, Holwein C, Braun S, Neumann J, et al. Cartilage repair surgery prevents progression of knee degeneration. Knee Surg Sports Traumatol Arthrosc. 2019;27:3001-13. doi: 10.1007/s00167-018-5321-8 [DOI] [PubMed] [Google Scholar]
- 17. Bode G, Ogon P, Pestka J, Zwingmann J, Feucht M, Sudkamp N, et al. Clinical outcome and return to work following single-stage combined autologous chondrocyte implantation and high tibial osteotomy. Int Orthop. 2015;39:689-96. doi: 10.1007/s00264-014-2547-z [DOI] [PubMed] [Google Scholar]
- 18. Kahlenberg CA, Nwachukwu BU, Hamid KS, Steinhaus ME, Williams RJ, 3rd. Analysis of outcomes for high tibial osteotomies performed with cartilage restoration techniques. Arthroscopy. 2017;33:486-92. doi: 10.1016/j.arthro.2016.08.010 [DOI] [PubMed] [Google Scholar]
- 19. Kim MK, Ko BS, Park JH. The proper correction of the mechanical axis in high tibial osteotomy with concomitant cartilage procedures—a retrospective comparative study. J Orthop Surg Res. 2019;14(1_suppl):281. doi: 10.1186/s13018-019-1333-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Niemeyer P, Schmal H, Hauschild O, von Heyden J, Sudkamp NP, Kostler W. Open-wedge osteotomy using an internal plate fixator in patients with medial-compartment gonarthritis and varus malalignment: 3-year results with regard to preoperative arthroscopic and radiographic findings. Arthroscopy. 2010;26(12):1607-16. doi: 10.1016/j.arthro.2010.05.006 [DOI] [PubMed] [Google Scholar]
- 21. Zarkadis NJ, Belmont PJ, Jr, Zachilli MA, Hollard CA, Kinsler AR, Todd MS, et al. Autologous chondrocyte implantation and tibial tubercle osteotomy for patellofemoral chondral defects: improved pain relief and occupational outcomes among US army servicemembers. Am J Sports Med. 2018;46:3198-208. doi: 10.1177/0363546518800713 [DOI] [PubMed] [Google Scholar]
- 22. Nimkingratana P, Brittberg M. Returning to work after articular cartilage repair intervention: a systematic review. Orthop J Sport Med. 2020;8:2325967120905526. doi: 10.1177/2325967120905526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ferruzzi A, Buda R, Cavallo M, Timoncini A, Natali S, Giannini S. Cartilage repair procedures associated with high tibial osteotomy in varus knees: Clinical results at 11years’ follow-up. Knee. 2014;21:445-50. doi: 10.1016/j.knee.2013.11.013 [DOI] [PubMed] [Google Scholar]
- 24. Koh YG, Kwon OR, Kim YS, Choi YJ. Comparative outcomes of open-wedge high tibial osteotomy mesenchymal stem cell treatment : a prospective study. Anthroscopy. 2014;30:1453-60. [DOI] [PubMed] [Google Scholar]
- 25. Lee OS, Lee SH, Mok SJ, Lee YS. Comparison of the regeneration of cartilage and the clinical outcomes after the open wedge high tibial osteotomy with or without microfracture: a retrospective case control study. BMC Musculoskelet Disord. 2019;20(1_suppl):267. doi: 10.1186/s12891-019-2607-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Saw KY, Anz A, Jee CSY, Ng RCS, Mohtrraudin N, Ragavanaidu K. High tibial osteotomy in combination with chondrogenesis after stem cell therapy: a histologic report of 8 cases. Arthroscopy. 2015;31:1909-20. doi: 10.1016/j.arthro.2015.03.038 [DOI] [PubMed] [Google Scholar]
- 27. Yao RZ, Liu WQ, Sun LZ, Yu MD, Wang GL. Effectiveness of high tibial osteotomy with or without other procedures for medial compartment osteoarthritis of knee: an update meta-analysis. J Knee Surg. Published online January 17, 2020. doi: 10.1055/s-0039-1700978 [DOI] [PubMed] [Google Scholar]
- 28. van Wulfften Palthe AFY, Clement ND, Temmerman OPP, Burger BJ. Survival and functional outcome of high tibial osteotomy for medial knee osteoarthritis: a 10–20-year cohort study. Eur J Orthop Surg Traumatol. 2018;28:1381-9. doi: 10.1007/s00590-018-2199-6 [DOI] [PubMed] [Google Scholar]
- 29. Brittberg M, Recker D, Ilgenfritz J, Saris DBF. Matrix-applied characterized autologous cultured chondrocytes versus microfracture: five-year follow-up of a prospective randomized trial. Am J Sports Med. 2018;46:1343-51. doi: 10.1177/0363546518756976 [DOI] [PubMed] [Google Scholar]
- 30. Niemeyer P, Albrecht D, Andereya S, Angele P, Ateschrang A, Aurich M, et al. Autologous chondrocyte implantation (ACI) for cartilage defects of the knee: a guideline by the working group „Clinical Tissue Regeneration” of the German Society of Orthopaedics and Trauma (DGOU). Knee. 2016;23:426-35. doi: 10.1016/j.knee.2016.02.001 [DOI] [PubMed] [Google Scholar]
- 31. Niemeyer P, Laute V, Zinser W, Becher C, Kolombe T, Fay J, et al. A prospective, randomized, open-label, multicenter, phase iii noninferiority trial to compare the clinical efficacy of matrix-associated autologous chondrocyte implantation with spheroid technology versus arthroscopic microfracture for cartilage defects of the knee. Orthop J Sport Med. 2019;7:232596711985444. doi: 10.1177/2325967119854442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Saris D, Price A, Widuchowski W, Bertrand-Marchand M, Caron J, Drogset JO. Matrix-applied characterized autologous cultured chondrocytes versus microfracture: two-year follow-up of a prospective randomized trial. Am J Sports Med. 2014;42:1384-94. doi: 10.1177/0363546514528093 [DOI] [PubMed] [Google Scholar]
- 33. Hoburg A, Löer I, Körsmeier K, Siebold R, Niemeyer P, Fickert S, Ruhnau K. Matrix-associated autologous chondrocyte implantation is an effective treatment at midterm follow-up in adolescents and young adults. Orthop J Sport Med. 2019;7:232596711984107. doi: 10.1177/2325967119841077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Saris DBF, Vanlauwe J, Victor J, Almqvist KF, Verdonk R, Bellemans J, et al. Treatment of symptomatic cartilage defects of the knee: characterized chondrocyte implantation results in better clinical outcome at 36 months in a randomized trial compared to microfracture. Am J Sports Med. 2009;37(Suppl 1):10S-19S. doi: 10.1177/0363546509350694 [DOI] [PubMed] [Google Scholar]