Abstract
Objective
Knee joint distraction (KJD) is a joint-preserving osteoarthritis treatment that may postpone a total knee arthroplasty (TKA) in younger patients. This systematic review and meta-analysis evaluates short- and long-term clinical benefit and tissue structure changes after KJD.
Design
MEDLINE, EMBASE, and Web of Science were searched for eligible clinical studies evaluating at least one of the primary parameters: WOMAC, VAS-pain, KOOS, EQ5D, radiographic joint space width or MRI cartilage thickness after KJD. Random effects models were applied on all outcome parameters and outcomes were compared with control groups found in the included studies.
Results
Eleven articles reporting on 7 different KJD cohorts with in total 127 patients and 5 control groups with multiple follow-up moments were included, of which 2 were randomized controlled trials. Significant improvements in all primary parameters were found and benefit lasted up to at least 9 years. Overall, outcomes were comparable with control groups, including high tibial osteotomy, although TKA showed better clinical response.
Conclusions
Current, still limited, evidence shows KJD causes clear benefit in clinical and structural parameters, both short- and long-term. Longer follow-up with more patients is necessary, to validate outcome and to potentially improve patient selection for this intensive treatment. Thus far, for younger knee osteoarthritis patients, KJD may be an option to consider.
Keywords: joint-preserving treatment, osteoarthritis, review, meta-analysis, knee joint distraction
Introduction
Knee osteoarthritis (OA) is a high incident joint disease with total knee arthroplasty (TKA) as final surgical option. 1 While TKA is considered cost-effective, reduces pain, and improves function, the prostheses’ limited life span brings a greater risk of a future revision when TKA is performed in younger (<65 years) patients. 2 As such, joint-preserving treatment is desirable for younger knee OA patients, to postpone TKA and reduce the chance of costly and less successful revision surgery. 3 When OA is limited to one side of the joint because of varus or valgus deviation, high tibial osteotomy (HTO) or distal femur osteotomy (DFO) is an option. These treatments have been applied in regular care for a long time and have been evaluated extensively.4-7 Unicompartmental knee arthroplasty is an option in unilateral OA as well. A newer joint-preserving treatment for knee OA is knee joint distraction (KJD). Distraction is a surgical treatment where 2 bony ends of a joint are temporarily separated by an external frame, fixed to the bones with bone pins. 8 It has shown progressive and sustained pain reduction, function improvement, and an increased radiographic joint space width (JSW) in patients with ankle OA.9-11 Following these promising results, multiple studies have investigated distraction of the knee joint. Successful KJD treatment could improve patients’ benefit, with reduced health costs for hospitals and society. 3 KJD might fill a gap in the treatment options for young patients with severe knee OA. 12 Before further implementation in regular care is justified based on the limited number of small studies, a meta-analysis is of value to give a more comprehensive overview of the current evidence for KJD as a possible treatment option. The goal of this systematic review and meta-analysis is to evaluate short- and long-term clinical benefit and tissue structure changes after KJD treatment for knee OA.
Methods
The review protocol is based on a protocol of Goh et al. for performing a systematic review about knee joint distraction, registered in PROSPERO (CRD42018087032). The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines for systematic reviews and meta-analyses were followed.
Sources and Search Terms
On July 8, 2019, MEDLINE, EMBASE, and Web of Science were searched for relevant articles. Search terms were (osteoarthritis OR arthritis OR cartilage OR osteochondral OR degenerative joint disease) AND distraction AND (knee OR tibiofemoral OR tibiofibular), and were applied on title and abstract and, in Web of Science, Keywords+.
Study Selection
All clinical studies where surgical KJD was applied for treatment of knee OA were eligible. One author (MPJ) selected all titles and abstracts that met in- and exclusion criteria.
Inclusion criteria were (1) the population consisted of knee OA patients; (2) treatment with KJD; (3) reporting the change of at least 1 of Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), visual analogue scale–pain (VAS-pain), Knee Injury and Osteoarthritis Outcome Score (KOOS), EuroQoL 5D-3L (EQ5D), radiographic joint space width (JSW), or magnetic resonance imaging (MRI) cartilage thickness between before and after treatment; (4) published or accepted for publication in a peer-reviewed journal or conference abstract of the past 2 years; and (5) English or Dutch language.
Exclusion criteria were (1) animal studies, (2) experimental studies, (3) cadaver studies, (4) reviews, (5) editorials, (6) case reports, and (7) letters.
Analysis
A risk of bias analysis, including selective reporting bias, was performed by one author (MPJ) in agreement with a second author (SCM). Possible publication bias was assessed as well.
Primary outcome measures were the WOMAC (scale 0-100, 100 = best), VAS-pain (scale 0-100, 0 = best), KOOS (scale 0-100, 100 = best), EQ5D (scale 0-1, 1 = best), radiographic JSW (mm), and MRI cartilage thickness (mm). Other clinical and cartilage-related outcomes found in included articles were analyzed as well. One author (MPJ) extracted data from the articles; investigators were not contacted for confirmation.
Heterogeneity was determined with the I 2 test, where I 2 > 75% indicates considerable heterogeneity and no meta-analysis was performed for that parameter. Random-effects models were used for all outcome measures. For continuous data, the mean difference (MD) and 95% confidence interval (95% CI) were calculated with the inverse variance method. For dichotomous data, the risk difference and 95% CI were calculated with the Cochran-Mantel-Haenszel method. No sensitivity analyses were performed. All patient groups that were used as a comparator for KJD in included studies are presented as control groups.
Data analysis was performed according to the Cochrane Handbook for Systematic Reviews of Interventions, using Review Manager 5.3 (The Nordic Cochrane Centre, The Cochrane Collaboration, 2014).
Results
Study Selection
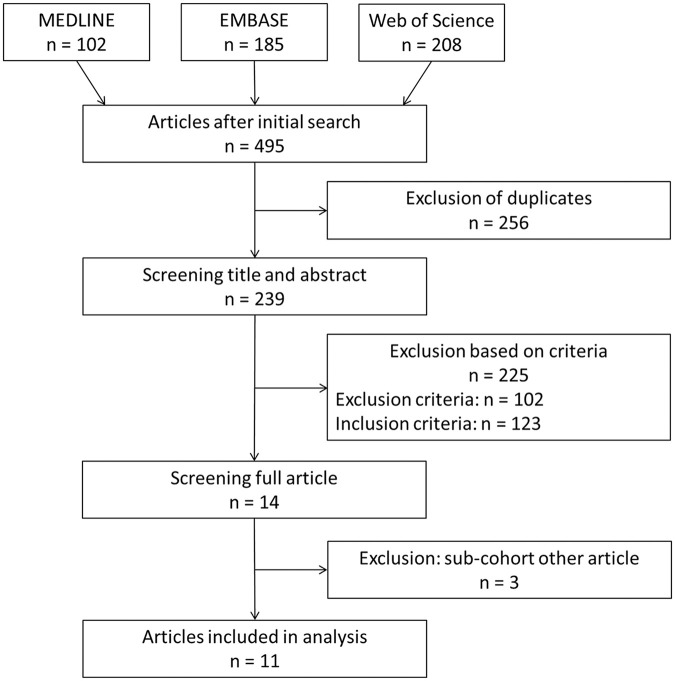
The selection process is shown in Figure 1 . After duplicate exclusion from the initially found 495 articles, 239 titles and abstracts were screened and, after applying inclusion and exclusion criteria, 14 complete articles were screened. Of these, 3 were excluded, since they reported on a subgroup from other included articles without reporting extra information on primary outcomes, leaving 11 articles included for analysis.12-22
Figure 1.
Flow diagram of article selection.
As multiple articles reported on different follow-up moments in the same patient cohorts, the overview of selected studies is separated per cohort of KJD-treated patients and control groups ( Table 1 ). 23
Table 1.
Included Studies.
| Study | Level of Evidence 23 | Treatment | No. of Patients | Follow-Up (Years) | Reference(s) | Outcome Measures |
|---|---|---|---|---|---|---|
| Knee joint distraction | ||||||
| Case series: Distraction and microfracture | IV | KJD and microfracture | 6 | Average 3 (1.2-4.3) | Deie et al., 2007 13 | VAS-pain, JSW |
| Case series: Distraction, microfracture and debridement | III-2 | KJD, microfracture and debridement | 19 | Average 5 (4.8-6.8) | Aly et al., 2011 15 | JSW |
| Open prospective study | IV | KJD | 20 | 1, 2, 5, 9 | Intema et al., 2011 16 ; Wiegant et al., 2013 17 ; Van der Woude et al., 2017 18 ; Jansen et al., 2018 19 | WOMAC, VAS-pain, JSW, MRI |
| RCT: KJD vs TKA | II | KJD | 20 | 1, 2 | Van der Woude et al., 2017 20 ; Jansen et al., 2019 21 | WOMAC, VAS-pain, KOOS, EQ5D, JSW |
| RCT: KJD vs HTO | II | KJD | 22 | 1, 2 | Van der Woude et al., 2017 22 ; Jansen et al., 2019 21 | WOMAC, VAS-pain, KOOS, EQ5D, JSW |
| Regular care (abstract) | III-2 | KJD | 40 | 1 | Jansen et al., 2019 12 | WOMAC |
| RCT MRI subcohort (abstract) | III-1 | KJD | 16 | 2 | Jansen et al., 2019 14 | MRI |
| Control groups | ||||||
| Case series: Microfracture and debridement | III-2 | Microfracture and debridement | 42 | Average 4 (3.6-6) | Aly et al., 2011 15 | JSW |
| Osteoarthritis Initiative (OAI) | III-1 | None | 138 | 5 | Van der Woude et al., 2017 18 | JSW, MRI |
| RCT: KJD vs TKA | II | TKA | 40 | 1, 2 | Van der Woude et al., 2017 20 ; Jansen et al., 2019 21 | WOMAC, VAS-pain, KOOS, EQ5D, JSW |
| RCT: KJD vs HTO | II | HTO | 46 | 1, 2 | Van der Woude et al., 2017 22 ; Jansen et al., 2019 21 | WOMAC, VAS-pain, KOOS, EQ5D, JSW |
| RCT MRI subcohort (abstract) | III-1 | HTO | 17 | 2 | Jansen et al., 2019 14 | MRI |
KJD = knee joint distraction; VAS-pain = visual analogue scale of pain; JSW = joint space width; WOMAC = Western Ontario and McMaster Universities Osteoarthritis Index; RCT = randomized controlled trial; TKA = total knee arthroplasty; KOOS = Knee injury and Osteoarthritis Outcome Score; EQ5D = EuroQol 5D-3L; HTO = high tibial osteotomy.
A total of 7 patient cohorts were treated with KJD, of which 2 in combination with another treatment: 1 cohort of 6 patients was treated with KJD and microfracture 13 and 1 cohort of 19 patients treated with KJD, microfracture, and debridement 15 that also had a control group of 42 patients treated with microfracture and debridement alone. In an open prospective study 20 patients were treated with KJD, without control group, and follow-up was reported after 1 year, 16 2 years, 17 5 years, 18 and 9 years. 19 At 5 years’ follow-up, this cohort was compared on structural outcome measures with 138 untreated patients from the Osteoarthritis Initiative (OAI), who were matched on patient characteristics with the KJD patients. In a randomized controlled trial (RCT) 20 KJD patients were compared with 40 TKA patients after 1 year 20 and 2 years. 21 In a different RCT, 22 KJD patients were compared with 46 HTO patients after 1 year 20 and 2 years. 21 In regular care, 40 patients were treated with KJD and evaluated after 1 year, without control group, reported in a conference abstract. 12 Last, a subgroup of 16 KJD patients and 17 HTO patients from the previously mentioned RCTs were evaluated and compared on an additional outcome measure (MRI cartilage thickness) after 2 years in a conference abstract. 14
The risk of bias for the included articles is shown in Figure 2 . As blinding of patients and personnel was not possible in any study and blinding of outcome measures only for structural parameters, none of the included articles had a completely low risk of bias. Only the RCTs20-22 had a low selection bias and only Jansen et al. (2018) 19 had a high bias for incomplete outcome data because of loss of patients during the long follow-up time. Aly et al. (2011) 15 had a high reporting bias because no precision/uncertainty of outcome measures is reported. Aly et al. (2011) 15 and Deie et al. (2007) 13 had an unclear risk of other bias because no clear study design was used. All other studies have an unclear risk of other bias because they all come from the same research group. Last, Jansen et al.12,14 had a lot of unclear bias since they are conference abstracts and as such did not report all information required to judge. No indication for publication bias was found.
Figure 2.
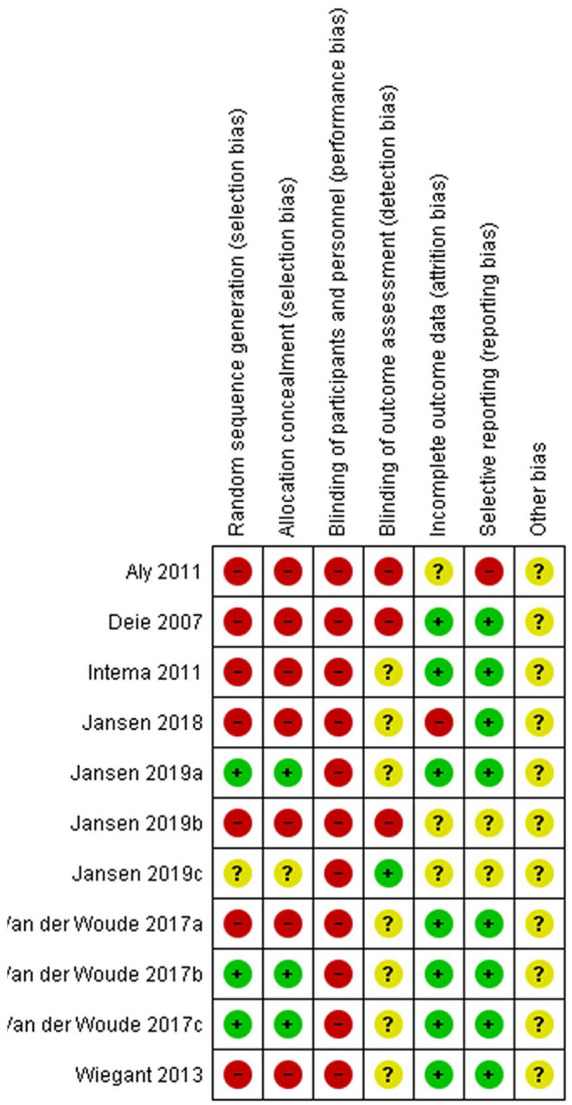
Risk of bias summary of included articles.
The pretreatment characteristics of the 7 included KJD cohorts are summarized in Table 2 , showing only minor differences between studies.
Table 2.
Patient Characteristics Before Treatment for Patients Treated With Knee Joint Distraction in Included Studies.
| First Author | Age (Years) | Female:Male Ratio | BMI (kg/m2) | Kellgren-Lawrence Grade 1:2:3:4 | Distraction Duration (Weeks) |
|---|---|---|---|---|---|
| Deie 2011 13 | 51.7 (SD 7.8) | 4:2 | 26.9 (SD 5.0) | 0:0:1:5 | 9.3 (SD 2.1) |
| Aly 2011 15 | Range 39-65 | 15:4 | 4 | ||
| Van der Woude 2017 18 | 48.5 (SEM 1.3) | 11:9 | 29.6 (SEM 0.8) | 3:4:11:2 | 8 |
| Van der Woude 2017 20 | 54.9 (SEM 1.8) | 11:9 | 27.4 (SEM 0.9) | 0:1:8:11 | 6 |
| Van der Woude 2017 22 | 51.2 (SEM 1.1) | 6:16 | 27.5 (SEM 0.7) | 6:4:11:1 | 6.1 (range 5.6-7.1) |
| Jansen 2019 12 | 54.3 (SD 6.8) | 17:23 | 27.7 (SD 3.9) | 0:7:23:10 | 6.5 (SD 0.6) |
| Jansen 2019 14 | Median 3 (IQR 1) |
BMI = body mass index; IQR = interquartile range; SD = standard deviation; SEM = standard error of the mean. Van der Woude 2017 18 is the open prospective study (also reported on by Intema 2011, 16 Wiegant 2013, 17 Jansen 2018 19 ); Van der Woude 2017 20 is the randomized controlled trial knee joint distraction versus total knee arthroplasty (also reported on by Jansen 2019 21 ); Van der Woude 2017 22 is the randomized controlled trial knee joint distraction versus high tibial osteotomy (also reported on by Jansen 2019 21 ).
Outcome after Knee Joint Distraction
Primary Outcome Measures
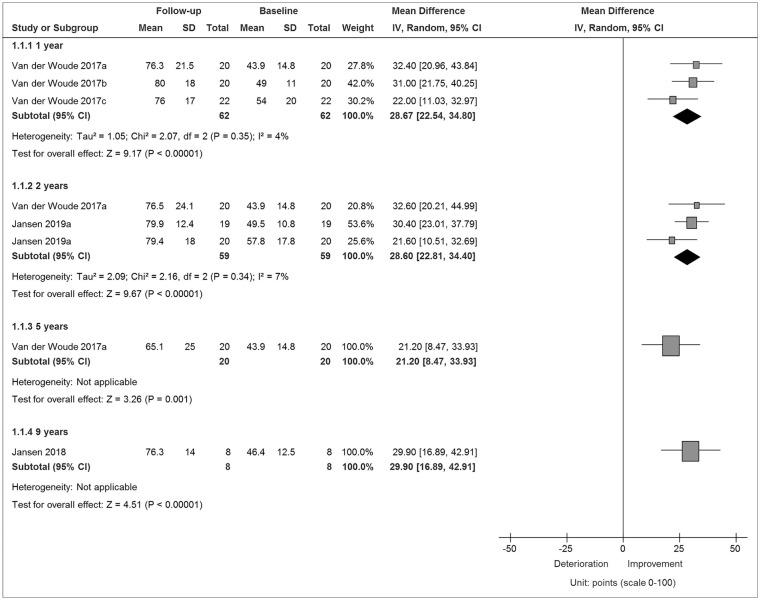
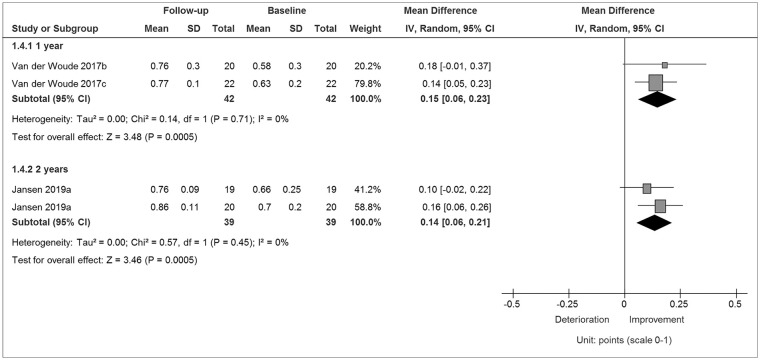
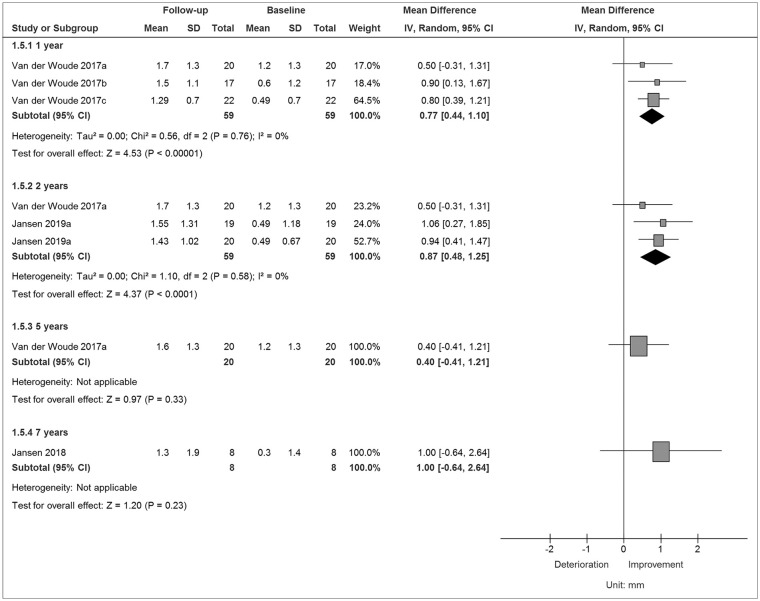
The results of the WOMAC, EQ5D, and minimum JSW after KJD are summarized in Figures 3–5, respectively. The outcomes for the VAS-pain, KOOS, mean JSW, and MRI cartilage thickness can be found in the supplementary data ( Supplementary Figures S1-S4). Patient cohorts treated with a combination of KJD and another therapy are not included in the figures. Neither are results from conference abstracts, as they did not report exact numbers.
Figure 3.
Change in total Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score 1, 2, 5, and 9 years after treatment with knee joint distraction.
References can be used multiple times because of division in patient cohort and years of follow-up. SD, standard deviation; CI, confidence interval.
Figure 4.
Change in total EuroQol 5D-3L (EQ5D) score 1 and 2 years after treatment with knee joint distraction.
References can be used multiple times because of division in patient cohort and years of follow-up. SD, standard deviation; CI, confidence interval.
Figure 5.
Change in minimum joint space width (JSW) 1, 2, 5, and 7 years after treatment with knee joint distraction.
References can be used multiple times because of division in patient cohort and years of follow-up. SD, standard deviation; CI, confidence interval.
The WOMAC and VAS-pain are evaluated in 3 cohorts after 1 year (patients n = 62) and 2 years (n = 59) and in 1 cohort after 5 years (n = 20) and 9 years (n = 8). The total WOMAC ( Fig. 3 ), VAS-pain (Supplementary Figure S1), and all WOMAC subscales were significantly increased compared with pretreatment at all time points, with an MD varying between 21.2 (5 years, P = 0.001) and 29.9 (9 years, P < 0.001) for the WOMAC and between 27.6 (5 years, P < 0.001) and 46.6 (9 years; P < 0.001) for the VAS.
The KOOS (Supplementary Figure S2) and EQ5D ( Fig. 4 ) were reported in 2 cohorts after 1 (n = 42) and 2 (n = 39) years, at both moments showing significant increases compared with pretreatment, as did all KOOS subscales. The KOOS had an MD of 23.2 (P < 0.001) and 24.9 (P < 0.001) and EQ5D of 0.15 (P < 0.001) and 0.14 (P < 0.001) after 1 and 2 years, respectively.
The minimum ( Figure 5 ) and mean (Supplementary Figure S3) JSW of the most affected compartment (MAC) are reported in 3 cohorts, after 1 (n = 59), 2 (n = 59), 5 (n = 20), and 7 (n = 8) years. Both JSW measures were statistically significantly increased after 1 and 2 years (MD between 0.68 and 0.87; all Ps < 0.01), but after 5 and 7 years, the JSW increase was no longer statistically significant (MD between 0.30 and 1.00; all Ps >0.2).
The MRI cartilage thickness is reported in 1 cohort after 1, 2, and 5 years (all n = 20; Supplementary Figure S4). After 1 year (MD = 0.70; P < 0.001) and 2 years (MD = 0.50; P = 0.002), there was a statistically significant increase compared to pretreatment, but after 5 years, the increase was no longer significant (MD = 0.20; P = 0.21).
For patients treated in regular care (n = 41) an increase in total WOMAC and subscales is shown, all with >20 points and P < 0.001. The MRI subgroup of RCT patients (n = 16) show a cartilage thickness increase of around 0.25 mm with P = 0.009.
Patients treated with KJD and microfracture (n = 6) showed a significant increase in VAS-pain (MD = 56.7; 95% CI 26.3-87.1; P < 0.001) and minimum JSW (MD = 1.09; 95% CI 0.19-1.99; P = 0.02) after an average of 3 years. Patients treated with KJD, microfracture, and debridement (n = 19) showed a significant increase in mean JSW from 2.5 to 4.3 mm with P < 0.001 after an average of 5 years.
Other Outcome Measures
Detailed results of additional outcome measures after KJD can be found in Table 3.
Table 3.
Changes in Nonprimary Outcome Parameters after Knee Joint Distraction.
| Knee joint distraction | Δ1 Year |
Δ2 Years |
Δ5 Years | ||||||
|---|---|---|---|---|---|---|---|---|---|
| No. of Cohorts (No. of Patients) | Change | P | No. of Cohorts (No. of Patients) | Change | P | No. of Cohorts (No. of Patients) | Change | P | |
| ICOAP | 2 (42) | −26.7 (−36.4 to −17.0) | <0.001 | 2 (39) | −29.4 (−36.6 to −22.2) | <0.001 | |||
| SF-36 PCS | 2 (42) | 7.8 (1.9-13.7) | 0.009 | 2 (39) | 6.1 (2.9-9.4) | <0.001 | |||
| SF-36 MCS | 2 (42) | −1.5 (−5.0 to 2.0) | 0.41 | 2 (39) | 0.5 (−2.8 to 3.8) | 0.76 | |||
| Knee flexion | 3 (62) | 2.4 (−1.0 to 5.7) | 0.16 | 2 (40) | 1.4 (−2.0 to 4.9) | 0.42 | |||
| MRI % denuded bone | 1 (20) | −17.3 (−26.5 to −8.1) | <0.001 | 1 (20) | −13.9 (−23.3 to −4.5) | 0.004 | 1 (20) | −5.7 (−15.6 to −5.2) | 0.30 |
| 1 (16) | ~5 | 0.010 | |||||||
| Knee joint distraction + microfracture | Δ ~3 Years | ||||||||
| No. of Cohorts (No. of Patients) | Change | P | |||||||
| Knee flexion | 1 (6) | 14.8 (2.7-26.9) | 0.04 | ||||||
| JOA score | 1 (6) | 28.7 (23.8-33.5) | <0.001 | ||||||
| Knee joint distraction, microfracture + debridement | Δ ~ 5 Years | ||||||||
| No. of cohorts (No. of Patients) | Change | P | |||||||
| Pain (0-4) | 1 (19) | Median 2 (IQR 1) to 0 (1) | <0.004 | ||||||
| Walking capacity | 1 (19) | Range 10-15 to 32-51 minutes | <0.001 | ||||||
| Difficulty stair climbing (yes/no) | 1 (19) | 100% to 36% yes | <0.002 | ||||||
| Knee flexion, deg | 1 (19) | Range 75-95 to 110-135 | <0.029 | ||||||
| Passive flexion, deg | 1 (19) | Range 85-120 to 150-170 | <0.193 | ||||||
| Tibiofemoral angle, deg | 1 (19) | Range 173-189 to 171-174 | <0.001 | ||||||
ICOAP = Intermittent and Constant OsteoArthritis Pain; SF-36 = Short Form 36; PCS = physical component scale; MCS = mental component scale; JOA = Japanese Orthopaedic Association; IQR = interquartile range. Bold p-values indicate statistical significance.
In 2 cohorts after 1 (n = 42) and 2 (n = 39) years, the ICOAP (Intermittent and Constant OsteoArthritis Pain; scale 0-100, 0 = best) and SF-36 (Short Form 36; scale 0-100, 100 = best) are reported. The ICOAP on 1 and 2 years and its subscales were significantly increased compared to pretreatment, as was the SF-36 PCS (physical component scale). The MCS (mental component scale) was not different from pretreatment values at 1 and 2 years.
Knee flexion (degrees) was measured before and 1 year after KJD in 3 cohorts (n = 62) and 2 years after KJD in 2 cohorts (n = 40). After both 1 and 2 years there was no significant difference from baseline.
The percentage subchondral bone without cartilage (denuded bone) is reported in 1 cohort (n = 20) and was significantly lower (better) than baseline at 1 and 2 years but not at 5 years. The MRI RCT subcohort (n = 16) graphically shows a significant decrease of this percentage of around 5.
After KJD and microfracture (n = 6) a significant increase in knee flexion and the Japanese Orthopaedic Association (JOA) score was reported. After KJD, microfracture and debridement (n = 19) a significant increase in active knee flexion, pain, walking capacity, stair climbing, and tibiofemoral angle was reported, but no difference in passive flexion.
Complications
Complications were reported in 5 studies with 87 patients, with 57 patients developing one or more pin tract skin infections, resulting in a risk of pin tract infections of 63% (95% CI 45-81). Only 3 studies (n = 62) reported treatment of complications. The majority of infections could be treated with oral antibiotics, resulting in a 57% (95% CI 33-82) risk of an infection requiring oral antibiotics and a 10% (95% CI 1-18) risk of an infection (including osteomyelitis, n = 1) requiring intravenous antibiotics. Also, 1 patient experienced postoperative foot drop, 3 patients a pulmonary embolism and 1 patient deep vein thrombosis, all successfully treated. One patient required knee manipulation under anesthesia 17 days after frame removal, 1 patient had a broken bone pin, and 1 patient experienced distraction frame failure, requiring refixation.
Comparison with Control Groups
Primary Outcome Measures
The comparisons with control groups for the VAS-pain, KOOS, mean JSW, and MRI cartilage thickness, as well as corresponding figures, can be found in the supplementary data; results were generally similar to those for the WOMAC, EQ5D, and minimum JSW as described below.
The WOMAC and EQ5D are compared between KJD and TKA and KJD and HTO in 2 different RCTs, 1 and 2 years after treatment. The change in total WOMAC (Supplementary Figure S5) was better for the control groups, with an MD varying between −12.0 (compared with TKA at 2 years) and −7.6 (HTO, 2 years), which was statistically significant for the 2-year difference between KJD and TKA (P = 0.011; rest P > 0.10). The EQ5D change (Supplementary Figure S6) was somewhat better for TKA than KJD after 1 year (MD = −0.17; P = 0.047) and 2 years (MD = −0.17; P = 0.051), with no significant difference between KJD and HTO at 1 year (MD = −0.01; P = 0.898) and 2 years (MD = 0.05; P = 0.559).
The change in minimum (Supplementary Figure S7) JSW of the MAC is compared between KJD and HTO after 1 and 2 years, showing a significantly better improvement for KJD after 1 year (MD = 0.40; P = 0.041) but no statistical difference after 2 years (MD = 0.32; P = 0.230). Compared with the OAI, the minimum JSW showed significantly better results 5 years after KJD (MD = 1.10; P < 0.001).
Other Outcome Measures
Other outcome measures compared between KJD and control groups were the SF-36, ICOAP, active and passive knee flexion, pain, walking capacity, stair climbing, tibiofemoral angle, and percentage denuded bone. Generally, there were no statistically significant differences in these measures between groups. Parameters that were statistically significantly different can be found in the supplementary data.
Complications
Only in the 2 RCTs the complications of the control groups, patients treated with TKA and with HTO, were described. Of 36 TKA patients, 5 required knee manipulation under anesthesia because of postoperative stiffness and 1 had a myocardial infarct 6 days postsurgery. Of 45 HTO patients, 2 experienced wound infection, 1 treated with oral and 1 with intravenous antibiotics. Furthermore, 1 patient received intravenous antibiotics for erysipelas and 1 patient had a partial medial meniscectomy <6 months after HTO.
Discussion
Overall, this review shows that KJD induces cartilaginous tissue regeneration and clinical improvement on short- and intermediate long-term. The effect sizes are large, so the small patient number is sufficient to demonstrate effects. The various clinical outcome measures showed similar results, as did the structural outcomes. The total number of patients is still limited, especially for long-term data, available in only 1 patient cohort. It is shown that prolonged treatment effect results in 75% of patients after 5 years and half of patients after 9 years still not undergoing TKA. 19 This implicates a clear reduction in survival over the long term. Longer follow-up is necessary to evaluate whether successfully postponing this first TKA over a sufficient period of time can indeed prevent a revision TKA as intended and reduce health care costs. 3
KJD provides cartilaginous tissue repair demonstrated by radiographs and MRI, results that are supported by biochemical marker studies that showed a net increase in systemic collagen type-II markers and by large animal in vivo studies.21,24 First-year posttreatment structural benefit, male gender, and more severe OA before treatment seem predictive for long-term benefit (survival).19,25 Also for ankle distraction male gender favored clinical outcome. 26 In contrast, young males perform less well after TKA compared with older females. 2 Young active males with severe damage might provide a more specific indication for KJD, although future cohorts and registries should confirm this.
Despite promising outcomes, KJD should not be perceived as an easy treatment for patients. The knee is immobilized for 6 weeks, and there is a high risk of pin tract skin infections. It is of importance that methods are found to decrease this risk as these can result in osteomyelitis, lead to significant use of oral antibiotics, and have a great impact on patients’ burden. However, these infections do not seem to cause problems for future TKA. Wiegant et al. 27 showed that TKA years after KJD did not result in extra complications whereas clinical benefit was not different from matched TKA patients without prior KJD. Future studies to reduce pin tract infection rates are needed, and preliminary results seem to make this feasible. 28 Apart from pin tract infections there were not many complications, but the few that did occur were relatively serious. While the number of complications after KJD besides pin tract infections was not that different than those in the control groups HTO and TKA, it is of importance to keep monitoring complications after KJD in larger studies and when introduced in regular care.
The included studies used different distraction periods (4-12 weeks). What effects this difference has and what period is ideal, is not known with certainty. No statistically significant difference between 6 and 8 weeks of distraction was observed, although at 6 weeks the benefit was slightly less. 29 This resulted in a 6-week distraction chosen for regular care. 12
Despite multiple studies showing cartilage regeneration after KJD, the mechanism enabling the regenerative process is not yet clear. Systemic biomarker analysis showed that KJD causes a decrease in collagen type-II degeneration marker CTX-II and an increase in collagen type-II synthesis marker PIIANP.17,21 Synovial fluid biomarkers showed changes in degenerative and regenerative pathways, and cartilage quality measurements (dGEMRIC) showed no changes over 2 years posttreatment, while cartilage volume increased and untreated patients might have shown a cartilage quality decrease.30,31 These results suggest that joint unloading by KJD stimulates intrinsic intra-articular conditions that promote cartilaginous tissue regeneration with an optimum between 1 and 2 years.
Patients treated with KJD show clearly better results than patients without KJD, while results were comparable between KJD and HTO. TKA patients often showed more clinical improvement but lost their native knee. Adding KJD to microfracture and debridement significantly improved results as well. Apart from pin tract infections, complications were not different in severity and number than those in other treatments. Knee contracture after 6-week fixation seemed no significant risk (on the contrary, flexion was regained quicker than after TKA). 20
Our study had several limitations. First, the number of patients was limited. Although the effect sizes were generally large, a larger number of patients would allow for stronger conclusions, especially for long-term results. Also, the treatment protocol (distraction duration) differed between studies. Furthermore, only two studies performed patient randomization, and none of the studies had a completely low risk of bias. Also, most studies were conducted by one research group, although in multi-center approach. Nevertheless, there were no indications for publication bias, and patient characteristics were generally very similar between the different studies. All studies seem to have included younger patients with severe knee OA, which is the target group for KJD treatment in regular care, increasing the likelihood that results found in this review may be expected in regular care as well.
In conclusion, this review analyzed data of available KJD studies for an extensive meta-analysis with multiple outcome measures, cohorts, and follow-up periods. Despite clear effects, it remains important that more patients are studied with longer follow-up, preferably in dedicated medical centers. This may also support treatment indication and patient selection. Better understanding of the underlying mechanisms of tissue structure repair and clinical benefit due to KJD might add to the above. Irrespectively, KJD provides for an additional option in joint-preserving treatments for osteoarthritis and a viable alternative to joint replacement, especially in younger patients.
Supplemental Material
Supplemental material, PRISMA_2009_flow_diagram for Knee Joint Distraction as Treatment for Osteoarthritis Results in Clinical and Structural Benefit: A Systematic Review and Meta-Analysis of the Limited Number of Studies and Patients Available by Mylène P. Jansen, Tim A.E.J. Boymans, Roel J.H. Custers, Rutger C.I. Van Geenen, Ronald J. Van Heerwaarden, Maarten R. Huizinga, Jorm M. Nellensteijn, Rob Sollie, Sander Spruijt and Simon C. Mastbergen in CARTILAGE
Supplemental material, Supplementary_Data for Knee Joint Distraction as Treatment for Osteoarthritis Results in Clinical and Structural Benefit: A Systematic Review and Meta-Analysis of the Limited Number of Studies and Patients Available by Mylène P. Jansen, Tim A.E.J. Boymans, Roel J.H. Custers, Rutger C.I. Van Geenen, Ronald J. Van Heerwaarden, Maarten R. Huizinga, Jorm M. Nellensteijn, Rob Sollie, Sander Spruijt and Simon C. Mastbergen in CARTILAGE
Supplemental material, Supplementary_Figure1 for Knee Joint Distraction as Treatment for Osteoarthritis Results in Clinical and Structural Benefit: A Systematic Review and Meta-Analysis of the Limited Number of Studies and Patients Available by Mylène P. Jansen, Tim A.E.J. Boymans, Roel J.H. Custers, Rutger C.I. Van Geenen, Ronald J. Van Heerwaarden, Maarten R. Huizinga, Jorm M. Nellensteijn, Rob Sollie, Sander Spruijt and Simon C. Mastbergen in CARTILAGE
Supplemental material, Supplementary_Figure10 for Knee Joint Distraction as Treatment for Osteoarthritis Results in Clinical and Structural Benefit: A Systematic Review and Meta-Analysis of the Limited Number of Studies and Patients Available by Mylène P. Jansen, Tim A.E.J. Boymans, Roel J.H. Custers, Rutger C.I. Van Geenen, Ronald J. Van Heerwaarden, Maarten R. Huizinga, Jorm M. Nellensteijn, Rob Sollie, Sander Spruijt and Simon C. Mastbergen in CARTILAGE
Supplemental material, Supplementary_Figure11 for Knee Joint Distraction as Treatment for Osteoarthritis Results in Clinical and Structural Benefit: A Systematic Review and Meta-Analysis of the Limited Number of Studies and Patients Available by Mylène P. Jansen, Tim A.E.J. Boymans, Roel J.H. Custers, Rutger C.I. Van Geenen, Ronald J. Van Heerwaarden, Maarten R. Huizinga, Jorm M. Nellensteijn, Rob Sollie, Sander Spruijt and Simon C. Mastbergen in CARTILAGE
Supplemental material, Supplementary_Figure2 for Knee Joint Distraction as Treatment for Osteoarthritis Results in Clinical and Structural Benefit: A Systematic Review and Meta-Analysis of the Limited Number of Studies and Patients Available by Mylène P. Jansen, Tim A.E.J. Boymans, Roel J.H. Custers, Rutger C.I. Van Geenen, Ronald J. Van Heerwaarden, Maarten R. Huizinga, Jorm M. Nellensteijn, Rob Sollie, Sander Spruijt and Simon C. Mastbergen in CARTILAGE
Supplemental material, Supplementary_Figure3 for Knee Joint Distraction as Treatment for Osteoarthritis Results in Clinical and Structural Benefit: A Systematic Review and Meta-Analysis of the Limited Number of Studies and Patients Available by Mylène P. Jansen, Tim A.E.J. Boymans, Roel J.H. Custers, Rutger C.I. Van Geenen, Ronald J. Van Heerwaarden, Maarten R. Huizinga, Jorm M. Nellensteijn, Rob Sollie, Sander Spruijt and Simon C. Mastbergen in CARTILAGE
Supplemental material, Supplementary_Figure4 for Knee Joint Distraction as Treatment for Osteoarthritis Results in Clinical and Structural Benefit: A Systematic Review and Meta-Analysis of the Limited Number of Studies and Patients Available by Mylène P. Jansen, Tim A.E.J. Boymans, Roel J.H. Custers, Rutger C.I. Van Geenen, Ronald J. Van Heerwaarden, Maarten R. Huizinga, Jorm M. Nellensteijn, Rob Sollie, Sander Spruijt and Simon C. Mastbergen in CARTILAGE
Supplemental material, Supplementary_Figure5 for Knee Joint Distraction as Treatment for Osteoarthritis Results in Clinical and Structural Benefit: A Systematic Review and Meta-Analysis of the Limited Number of Studies and Patients Available by Mylène P. Jansen, Tim A.E.J. Boymans, Roel J.H. Custers, Rutger C.I. Van Geenen, Ronald J. Van Heerwaarden, Maarten R. Huizinga, Jorm M. Nellensteijn, Rob Sollie, Sander Spruijt and Simon C. Mastbergen in CARTILAGE
Supplemental material, Supplementary_Figure6 for Knee Joint Distraction as Treatment for Osteoarthritis Results in Clinical and Structural Benefit: A Systematic Review and Meta-Analysis of the Limited Number of Studies and Patients Available by Mylène P. Jansen, Tim A.E.J. Boymans, Roel J.H. Custers, Rutger C.I. Van Geenen, Ronald J. Van Heerwaarden, Maarten R. Huizinga, Jorm M. Nellensteijn, Rob Sollie, Sander Spruijt and Simon C. Mastbergen in CARTILAGE
Supplemental material, Supplementary_Figure7 for Knee Joint Distraction as Treatment for Osteoarthritis Results in Clinical and Structural Benefit: A Systematic Review and Meta-Analysis of the Limited Number of Studies and Patients Available by Mylène P. Jansen, Tim A.E.J. Boymans, Roel J.H. Custers, Rutger C.I. Van Geenen, Ronald J. Van Heerwaarden, Maarten R. Huizinga, Jorm M. Nellensteijn, Rob Sollie, Sander Spruijt and Simon C. Mastbergen in CARTILAGE
Supplemental material, Supplementary_Figure8 for Knee Joint Distraction as Treatment for Osteoarthritis Results in Clinical and Structural Benefit: A Systematic Review and Meta-Analysis of the Limited Number of Studies and Patients Available by Mylène P. Jansen, Tim A.E.J. Boymans, Roel J.H. Custers, Rutger C.I. Van Geenen, Ronald J. Van Heerwaarden, Maarten R. Huizinga, Jorm M. Nellensteijn, Rob Sollie, Sander Spruijt and Simon C. Mastbergen in CARTILAGE
Supplemental material, Supplementary_Figure9 for Knee Joint Distraction as Treatment for Osteoarthritis Results in Clinical and Structural Benefit: A Systematic Review and Meta-Analysis of the Limited Number of Studies and Patients Available by Mylène P. Jansen, Tim A.E.J. Boymans, Roel J.H. Custers, Rutger C.I. Van Geenen, Ronald J. Van Heerwaarden, Maarten R. Huizinga, Jorm M. Nellensteijn, Rob Sollie, Sander Spruijt and Simon C. Mastbergen in CARTILAGE
Supplemental material, Supplementary_Figure_Legends for Knee Joint Distraction as Treatment for Osteoarthritis Results in Clinical and Structural Benefit: A Systematic Review and Meta-Analysis of the Limited Number of Studies and Patients Available by Mylène P. Jansen, Tim A.E.J. Boymans, Roel J.H. Custers, Rutger C.I. Van Geenen, Ronald J. Van Heerwaarden, Maarten R. Huizinga, Jorm M. Nellensteijn, Rob Sollie, Sander Spruijt and Simon C. Mastbergen in CARTILAGE
Footnotes
Authors’ Note: All work was performed at the department of Rheumatology & Clinical Immunology of the University Medical Center Utrecht.
Acknowledgments and Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Unrestricted funding by ZonMW and FOREUM supported this work; funders had no involvement with this article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
ORCID iD: Mylène P. Jansen  https://orcid.org/0000-0003-1929-6350
https://orcid.org/0000-0003-1929-6350
Supplementary material for this article is available on the Cartilage website at https://journals.sagepub.com/home/car.
References
- 1. Bijlsma JW, Berenbaum F, Lafeber FP. Osteoarthritis: an update with relevance for clinical practice. Lancet. 2011;377:2115-26. doi: 10.1016/S0140-6736(11)60243-2 [DOI] [PubMed] [Google Scholar]
- 2. Bayliss LE, Culliford D, Monk AP, Glyn-Jones S, Prieto-Alhambra D, Judge A, et al. The effect of patient age at intervention on risk of implant revision after total replacement of the hip or knee: a population-based cohort study. Lancet. 2017;389:1424-30. doi: 10.1016/S0140-6736(17)30059-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. van der Woude JAD, Nair SC, Custers RJH, van Laar JM, Kuchuck NO, Lafeber FPJG, et al. Knee joint distraction compared to total knee arthroplasty for treatment of end stage osteoarthritis: simulating long-term outcomes and cost-effectiveness. PLoS One. 2016;11:e0155524. doi: 10.1371/journal.pone.0155524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cao Z, Mai X, Wang J, Feng E, Huang Y. Unicompartmental knee arthroplasty vs high tibial osteotomy for knee osteoarthritis: a systematic review and meta-analysis. J Arthroplasty. 2018;33:952-9. doi: 10.1016/j.arth.2017.10.025 [DOI] [PubMed] [Google Scholar]
- 5. Lee OS, Ahn S, Ahn JH, Teo SH, Lee YS. Effectiveness of concurrent procedures during high tibial osteotomy for medial compartment osteoarthritis: a systematic review and meta-analysis. Arch Orthop Trauma Surg. 2018;138:227-36. doi: 10.1007/s00402-017-2826-4 [DOI] [PubMed] [Google Scholar]
- 6. Wylie JD, Jones DL, Hartley MK, Kapron AL, Krych AJ, Aoki SK, et al. Distal femoral osteotomy for the valgus knee: medial closing wedge versus lateral opening wedge: a systematic review. Arthroscopy. 2016;32(10):2141-7. doi: 10.1016/j.arthro.2016.04.010 [DOI] [PubMed] [Google Scholar]
- 7. Brouwer RW, Huizinga MR, Duivenvoorden T, van Raaij TM, Verhagen AP, Bierma-Zeinstra SMA, et al. Osteotomy for treating knee osteoarthritis. Cochrane Database Syst Rev. 2014;2014(12):CD004019. doi: 10.1002/14651858.CD004019.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lafeber FP, Intema F, Van Roermund PM, Marijnissen AC. Unloading joints to treat osteoarthritis, including joint distraction. Curr Opin Rheumatol. 2006;18:519-25. doi: 10.1097/01.bor.0000240366.54960.a1 [DOI] [PubMed] [Google Scholar]
- 9. Bernstein M, Reidler J, Fragomen A, Rozbruch SR. Ankle distraction arthroplasty. J Am Acad Orthop Surg. 2017;25:89-99. doi: 10.5435/JAAOS-D-14-00077 [DOI] [PubMed] [Google Scholar]
- 10. Marijnissen ACA, Van Roermund PM, Van Melkebeek J, Schenk W, Verbout AJ, Bijlsma JWJ, et al. Clinical benefit of joint distraction in the treatment of severe osteoarthritis of the ankle: proof of concept in an open prospective study and in a randomized controlled study. Arthritis Rheum. 2002;46:2893-902. doi: 10.1002/art.10612 [DOI] [PubMed] [Google Scholar]
- 11. Ploegmakers JJW, van Roermund PM, van Melkebeek J, Lammens J, Bijlsma JWJ, Lafeber FPJG, et al. Prolonged clinical benefit from joint distraction in the treatment of ankle osteoarthritis. Osteoarthritis Cartilage. 2005;13:582-8. doi: 10.1016/j.joca.2005.03.002 [DOI] [PubMed] [Google Scholar]
- 12. Jansen M, Mastbergen SC, Van Empelen MD, Kester EC, Lafeber FP, Custers RC. Knee joint distraction as standard of care treatment for knee osteoarthritis: a comparison with clinical trial patients. Osteoarthritis Cartilage. 2019;27:S515-S516. doi: 10.1016/j.joca.2019.02.589 [DOI] [Google Scholar]
- 13. Deie M, Ochi M, Adachi N, Kajiwara R, Kanaya A. A new articulated distraction arthroplasty device for treatment of the osteoarthritic knee joint: a preliminary report. Arthroscopy. 2007;23:833-8. [DOI] [PubMed] [Google Scholar]
- 14. Jansen MP, Maschek S, Van Heerwaarden RJ, Mastbergen SC, Wirth W, Lafeber FP, et al. Knee joint distraction is more efficient in rebuilding cartilage thickness in the more affected compartment than high tibial osteotomy in patients with knee osteoarthritis. Osteoarthritis Cartilage. 2019;27:S330-S331. doi: 10.1016/j.joca.2019.02.736 [DOI] [Google Scholar]
- 15. Aly TA, Hafez K, Amin O. Arthrodiatasis for management of knee osteoarthritis. Orthopedics. 2011;34:e338-e343. doi: 10.3928/01477447-20110627-17 [DOI] [PubMed] [Google Scholar]
- 16. Intema F, Van Roermund PM, Marijnissen ACA, Cotofana S, Eckstein F, Castelein RM, et al. Tissue structure modification in knee osteoarthritis by use of joint distraction: an open 1-year pilot study. Ann Rheum Dis. 2011;70:1441-6. doi: 10.1136/ard.2010.142364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wiegant K, van Roermund PM, Intema F, Cotofana S, Eckstein F, Mastbergen SC, et al. Sustained clinical and structural benefit after joint distraction in the treatment of severe knee osteoarthritis. Osteoarthr Cartil. 2013;21:1660-7. doi: 10.1016/j.joca.2013.08.006 [DOI] [PubMed] [Google Scholar]
- 18. van der Woude JTAD, Wiegant K, van Roermund PM, Intema F, Custers RJH, Eckstein F, et al. Five-year follow-up of knee joint distraction: clinical benefit and cartilaginous tissue repair in an open uncontrolled prospective study. Cartilage. 2017;8:263-71. doi: 10.1177/1947603516665442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jansen MP, van der Weiden GS, Van Roermund PM, Custers RJH, Mastbergen SC, Lafeber FPJG. Initial tissue repair predicts long-term clinical success of knee joint distraction as treatment for knee osteoarthritis. Osteoarthritis Cartilage. 2018;26:1604-8. doi: 10.1016/j.joca.2018.08.004 [DOI] [PubMed] [Google Scholar]
- 20. Van Der Woude JAD, Wiegant K, Van Heerwaarden RJ, Spruijt S, Emans PJ, Mastbergen SC, et al. Knee joint distraction compared with total knee arthroplasty a randomised controlled trial. Bone Joint J. 2017;99-B:51-8. doi: 10.1302/0301-620X.99B1.BJJ-2016-0099.R3 [DOI] [PubMed] [Google Scholar]
- 21. Jansen MP, Besselink NJ, van Heerwaarden RJ, Custers RJH, Emans PJ, Spruijt S, et al. Knee joint distraction compared with high tibial osteotomy and total knee arthroplasty: two-year clinical, radiographic, and biochemical marker outcomes of two randomized controlled trials. Cartilage. Epub 2019 Feb 13. doi: 10.1177/1947603519828432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. van der Woude JAD, Wiegant K, van Heerwaarden RJ, Spruijt S, van Roermund PM, Custers RJH, et al. Knee joint distraction compared with high tibial osteotomy: a randomized controlled trial. Knee Surg Sport Traumatol Arthrosc. 2017;25:876-86. doi: 10.1007/s00167-016-4131-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. McNair P, Lewis G. Levels of evidence in medicine. Int J Sports Phys Ther. 2012;7:474-81. [PMC free article] [PubMed] [Google Scholar]
- 24. Wiegant K, Intema F, Roermund PM, Barten-van Rijbroek AD, Doornebal A, Hazewinkel HAW, et al. Evidence of cartilage repair by joint distraction in a canine model of osteoarthritis. Arthritis Rheumatol. 2015;67:465-74. doi: 10.1002/art.38906 [DOI] [PubMed] [Google Scholar]
- 25. van der Woude JAD, Welsing PM, van Roermund PM, Custers RJH, Kuchuk NO, Lafeber FPJGG. Prediction of cartilaginous tissue repair after knee joint distraction. Knee. 2016;23:792-5. doi: 10.1016/j.knee.2016.02.015 [DOI] [PubMed] [Google Scholar]
- 26. Marijnissen ACA, Hoekstra MCL, Pré BCD, Van Roermund PM, Van Melkebeek J, Amendola A, et al. Patient characteristics as predictors of clinical outcome of distraction in treatment of severe ankle osteoarthritis. J Orthop Res. 2014;32:96-101. doi: 10.1002/jor.22475 [DOI] [PubMed] [Google Scholar]
- 27. Wiegant K, van Roermund PM, van Heerwaarden RJ, Spruijt S, Custers RJH, Kuchuck NO, et al. Total knee prosthesis after knee joint distraction treatment. J Surg Surg Res. 2015;1:066-071. doi: 10.17352/2455-2968.000016 [DOI] [Google Scholar]
- 28. Jansen MP, Van Egmond N, Kester EC, Custers RJH. Iodosorbzalf ter preventie van pengatinfecties bij kniedistractie. In: NOV-Jaarcongres; 2020. Jan 13. [Google Scholar]
- 29. van der Woude JAD, van Heerwaarden RJ, Spruijt S, Eckstein F, Maschek S, van Roermund PM, et al. Six weeks of continuous joint distraction appears sufficient for clinical benefit and cartilaginous tissue repair in the treatment of knee osteoarthritis. Knee. 2016;23:785-91. doi: 10.1016/j.knee.2016.05.001 [DOI] [PubMed] [Google Scholar]
- 30. Watt FE, Hamid B, Garriga C, Judge A, Hrusecka R, Custers R, et al. Analysis of proteins in the synovial fluid during joint distraction: unravelling mechano-sensitive pathways that drive intrinsic cartilage repair? Osteoarthritis Cartilage. 2018;26:S17-S18. doi: 10.1016/j.joca.2018.02.052 [DOI] [Google Scholar]
- 31. Besselink NJ, Vincken KL, Bartels LW, van Heerwaarden RJ, Concepcion AN, Marijnissen ACA, et al. Cartilage quality (dGEMRIC index) following knee joint distraction or high tibial osteotomy. Cartilage. 2020;11(1_suppl):19-31. doi: 10.1177/1947603518777578 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, PRISMA_2009_flow_diagram for Knee Joint Distraction as Treatment for Osteoarthritis Results in Clinical and Structural Benefit: A Systematic Review and Meta-Analysis of the Limited Number of Studies and Patients Available by Mylène P. Jansen, Tim A.E.J. Boymans, Roel J.H. Custers, Rutger C.I. Van Geenen, Ronald J. Van Heerwaarden, Maarten R. Huizinga, Jorm M. Nellensteijn, Rob Sollie, Sander Spruijt and Simon C. Mastbergen in CARTILAGE
Supplemental material, Supplementary_Data for Knee Joint Distraction as Treatment for Osteoarthritis Results in Clinical and Structural Benefit: A Systematic Review and Meta-Analysis of the Limited Number of Studies and Patients Available by Mylène P. Jansen, Tim A.E.J. Boymans, Roel J.H. Custers, Rutger C.I. Van Geenen, Ronald J. Van Heerwaarden, Maarten R. Huizinga, Jorm M. Nellensteijn, Rob Sollie, Sander Spruijt and Simon C. Mastbergen in CARTILAGE
Supplemental material, Supplementary_Figure1 for Knee Joint Distraction as Treatment for Osteoarthritis Results in Clinical and Structural Benefit: A Systematic Review and Meta-Analysis of the Limited Number of Studies and Patients Available by Mylène P. Jansen, Tim A.E.J. Boymans, Roel J.H. Custers, Rutger C.I. Van Geenen, Ronald J. Van Heerwaarden, Maarten R. Huizinga, Jorm M. Nellensteijn, Rob Sollie, Sander Spruijt and Simon C. Mastbergen in CARTILAGE
Supplemental material, Supplementary_Figure10 for Knee Joint Distraction as Treatment for Osteoarthritis Results in Clinical and Structural Benefit: A Systematic Review and Meta-Analysis of the Limited Number of Studies and Patients Available by Mylène P. Jansen, Tim A.E.J. Boymans, Roel J.H. Custers, Rutger C.I. Van Geenen, Ronald J. Van Heerwaarden, Maarten R. Huizinga, Jorm M. Nellensteijn, Rob Sollie, Sander Spruijt and Simon C. Mastbergen in CARTILAGE
Supplemental material, Supplementary_Figure11 for Knee Joint Distraction as Treatment for Osteoarthritis Results in Clinical and Structural Benefit: A Systematic Review and Meta-Analysis of the Limited Number of Studies and Patients Available by Mylène P. Jansen, Tim A.E.J. Boymans, Roel J.H. Custers, Rutger C.I. Van Geenen, Ronald J. Van Heerwaarden, Maarten R. Huizinga, Jorm M. Nellensteijn, Rob Sollie, Sander Spruijt and Simon C. Mastbergen in CARTILAGE
Supplemental material, Supplementary_Figure2 for Knee Joint Distraction as Treatment for Osteoarthritis Results in Clinical and Structural Benefit: A Systematic Review and Meta-Analysis of the Limited Number of Studies and Patients Available by Mylène P. Jansen, Tim A.E.J. Boymans, Roel J.H. Custers, Rutger C.I. Van Geenen, Ronald J. Van Heerwaarden, Maarten R. Huizinga, Jorm M. Nellensteijn, Rob Sollie, Sander Spruijt and Simon C. Mastbergen in CARTILAGE
Supplemental material, Supplementary_Figure3 for Knee Joint Distraction as Treatment for Osteoarthritis Results in Clinical and Structural Benefit: A Systematic Review and Meta-Analysis of the Limited Number of Studies and Patients Available by Mylène P. Jansen, Tim A.E.J. Boymans, Roel J.H. Custers, Rutger C.I. Van Geenen, Ronald J. Van Heerwaarden, Maarten R. Huizinga, Jorm M. Nellensteijn, Rob Sollie, Sander Spruijt and Simon C. Mastbergen in CARTILAGE
Supplemental material, Supplementary_Figure4 for Knee Joint Distraction as Treatment for Osteoarthritis Results in Clinical and Structural Benefit: A Systematic Review and Meta-Analysis of the Limited Number of Studies and Patients Available by Mylène P. Jansen, Tim A.E.J. Boymans, Roel J.H. Custers, Rutger C.I. Van Geenen, Ronald J. Van Heerwaarden, Maarten R. Huizinga, Jorm M. Nellensteijn, Rob Sollie, Sander Spruijt and Simon C. Mastbergen in CARTILAGE
Supplemental material, Supplementary_Figure5 for Knee Joint Distraction as Treatment for Osteoarthritis Results in Clinical and Structural Benefit: A Systematic Review and Meta-Analysis of the Limited Number of Studies and Patients Available by Mylène P. Jansen, Tim A.E.J. Boymans, Roel J.H. Custers, Rutger C.I. Van Geenen, Ronald J. Van Heerwaarden, Maarten R. Huizinga, Jorm M. Nellensteijn, Rob Sollie, Sander Spruijt and Simon C. Mastbergen in CARTILAGE
Supplemental material, Supplementary_Figure6 for Knee Joint Distraction as Treatment for Osteoarthritis Results in Clinical and Structural Benefit: A Systematic Review and Meta-Analysis of the Limited Number of Studies and Patients Available by Mylène P. Jansen, Tim A.E.J. Boymans, Roel J.H. Custers, Rutger C.I. Van Geenen, Ronald J. Van Heerwaarden, Maarten R. Huizinga, Jorm M. Nellensteijn, Rob Sollie, Sander Spruijt and Simon C. Mastbergen in CARTILAGE
Supplemental material, Supplementary_Figure7 for Knee Joint Distraction as Treatment for Osteoarthritis Results in Clinical and Structural Benefit: A Systematic Review and Meta-Analysis of the Limited Number of Studies and Patients Available by Mylène P. Jansen, Tim A.E.J. Boymans, Roel J.H. Custers, Rutger C.I. Van Geenen, Ronald J. Van Heerwaarden, Maarten R. Huizinga, Jorm M. Nellensteijn, Rob Sollie, Sander Spruijt and Simon C. Mastbergen in CARTILAGE
Supplemental material, Supplementary_Figure8 for Knee Joint Distraction as Treatment for Osteoarthritis Results in Clinical and Structural Benefit: A Systematic Review and Meta-Analysis of the Limited Number of Studies and Patients Available by Mylène P. Jansen, Tim A.E.J. Boymans, Roel J.H. Custers, Rutger C.I. Van Geenen, Ronald J. Van Heerwaarden, Maarten R. Huizinga, Jorm M. Nellensteijn, Rob Sollie, Sander Spruijt and Simon C. Mastbergen in CARTILAGE
Supplemental material, Supplementary_Figure9 for Knee Joint Distraction as Treatment for Osteoarthritis Results in Clinical and Structural Benefit: A Systematic Review and Meta-Analysis of the Limited Number of Studies and Patients Available by Mylène P. Jansen, Tim A.E.J. Boymans, Roel J.H. Custers, Rutger C.I. Van Geenen, Ronald J. Van Heerwaarden, Maarten R. Huizinga, Jorm M. Nellensteijn, Rob Sollie, Sander Spruijt and Simon C. Mastbergen in CARTILAGE
Supplemental material, Supplementary_Figure_Legends for Knee Joint Distraction as Treatment for Osteoarthritis Results in Clinical and Structural Benefit: A Systematic Review and Meta-Analysis of the Limited Number of Studies and Patients Available by Mylène P. Jansen, Tim A.E.J. Boymans, Roel J.H. Custers, Rutger C.I. Van Geenen, Ronald J. Van Heerwaarden, Maarten R. Huizinga, Jorm M. Nellensteijn, Rob Sollie, Sander Spruijt and Simon C. Mastbergen in CARTILAGE