Abstract
Objective
Fixation of unstable osteochondritis dissecans (OCD) lesions and displaced osteochondral fragments are frequently performed procedures in pediatric orthopedic surgery. Since 2018, CE-certified MAGNEZIX pins are used in our institution in these cases. The aim of this study was (1) to analyze safety, efficiency, and limitations of magnesium-pin-based fixation of unstable OCD lesions and displaced osteochondral fragments and (2) to report clinical and radiological outcomes at short-term follow-up (FU).
Design
In this prospective cohort study, 19 patients (10 girls and 9 boys) were included. Inclusion criteria were (1) magnetic resonance imaging–confirmed unstable OCD lesion or displaced osteochondral fragment, (2) fixation with magnesium-based pins, and (3) minimum FU of 6 months. X-rays were taken 6 weeks and 6 months after operation and magnetic resonance imaging scans every 4 to 6 months to assess the healing progress.
Results
In total 67 pins were used, with a mean of 3.6 ± 1.4 per patient. Average age at surgery was 13.7 years (11-17 years). Mean time of operation was 56 ± 31 minutes, including arthroscopy, fixation, and patellar realignment (n = 6). No intraoperative complications occurred. Average FU was 11.3 ± 4.2 months (6-20 months). No redislocation or new dislocation occurred. Until now a complete radiographic healing occurred in 12 cases. Due to an implant failure in one case 11 weeks after the index surgery a revision became necessary.
Conclusions
In short-term FU of 11 ± 4 months MAGNEZIX pins provide high stability after fixation of unstable OCDs and displaced osteochondral fragments leading to uncomplicated and timely healing.
Keywords: biodegradable implants, magnesium pins, osteochondritis dissecans, osteochondral lesion
Introduction
Surgical refixation is the gold standard for unstable osteochondritis dissecans (OCD) lesions or displaced osteochondral fragments, especially in younger patients. Good mid- and long-term outcomes are reported in the literature. 1 The design, material, and application of fixation devices differ, ranging from open reduction and internal fixation with metallic screws to arthroscopic assisted use of pins and bioresorbable implants. 2 The main advantage of bioresorbable implants is the avoidance of implant removal. Therefore, they are increasingly used in trauma and orthopedic surgery in recent years. Fixation of unstable osteochondral lesions with bioresorbable devices is commonly used and well documented in the literature. 3 However, besides good results there are failures reported after fixation of OCD and osteochondral lesions with biodegradable implants. 4 The quality of pin fixation is crucial to prevent failure, especially in fixation of osteochondral fragments or lesions. Accordingly, different devices consisting of various materials and composites have been used in recent years. Experimental data suggest that magnesium alloys exhibit superior bone-implant interface strength than copolymeric pins. 5 Furthermore, magnesium-based alloys offer good biocompatibility and degradation kinetics, have osteoconductive and anti-inflammatory properties, and cause reduced artifacts in magnetic resonance imaging (MRI). 6 The first magnesium devices (MAGNEZIX, Syntellix AG, Hannover, Germany) became commercially available in 2013 and were primarily used in adults for hallux valgus surgery and medial malleolar fractures.7,8 Since 2018, these implants (screws and pins) are used for fixation of fractures, osteotomies, and unstable osteochondral lesions in skeletally immature patients in our institution. The stability of the pins used in our study is supposed to be 80% of the initial stability after 75 days according to the statement of the manufacturer. In our study, none of the implants were completely resorbed after 11 months. In 2018, Plaass et al. could show through MRI that after 3 years magnesium-based implants were degraded but not fully remodeled. 9
The purpose of this study was to (1) analyze safety, efficiency, and limitations of the MAGNEZIX pin-based fixation of unstable OCD lesions and displaced osteochondral fragments and (2) to report short-term follow-up (FU) in children.
Methods
Study Design
In this prospective clinical case series, we analyzed all patient data after fixation of unstable OCD lesions and displaced osteochondral fragments using new biodegradable magnesium pins. Inclusion criteria were (1) age under 18 years, (2) MRI-confirmed unstable OCD lesions or displaced osteochondral fragments, (3) fixation with magnesium-based pins (MAGNEZIX), and (4) a minimum FU of 6 months. X-rays were performed 6 weeks and 6 months after operation and MRI scans every 4 to 6 months to assess the healing progress. Prior to surgery MRI films as well as radiographs (AP and lateral view) were taken to measure the size of the lesions and to assess the stability of fragments. The OCD lesions were classified according to the International Cartilage Repair Society (ICRS) criteria. 10 Postoperative radiographs were performed to analyze pin positioning and quality of reduction of displaced fragments. All patients had clinical and radiological FU 6 weeks (X-ray) and 6 months (X-ray and MRI) after the index surgery. In cases with longer FU an additional MRI was done 1 year postoperatively. Union, delayed, or nonunion complications, such as implant failure or infection, were documented. Duration of surgery and radiation exposure were also documented.
Implants
In all cases the osteochondral fragment or the unstable OCD lesions was reattached using biodegradable magnesium-based pins (MAGNEZIX Pins). These pins are magnesium-based implants made of an aluminum-free magnesium alloy that is classified as MgYREZr alloy according to DIN EN 1753 (i.e., magnesium, yttrium, zirconium, and other rare earth metals). The head of these pins is flattened to enable stable reduction of the fragment ( Fig. 1 ). These pins are available with different diameters (1.5, 2.0, 2.7, and 3.2 mm) and length (8-50 mm).
Figure 1.

Design of the magnesium-based pin (MAGNEZIX).
Surgical Technique and Postoperative Protocol
First, a standard arthroscopy (knee 16, tibiotalar joint 3) was performed. In proven cases of an unstable lesion or displaced fragment 4 patients had an arthroscopic refixation, whereas in 15 cases an open reduction was necessary. All pins were countersunk under the chondral surface to avoid prominence ( Fig. 2 ). For adequate intraarticular exposure of a talar OCD a medial malleolar osteotomy was used. These osteotomies were fixed with magnesium-based compression screws ( Fig. 3 ). To realign the patella we used the Goldthwait-procedure in 4 patients and the Elmslie-Trillat procedure in 2 patients ( Fig. 4 ). Postoperative management was identical for all patients including (1) joint immobilization with a simple brace (knee) or cast (ankle joint) and (2) no weight bearing of the operated leg for 6 weeks after surgery. Walking with full weight bearing and active exercises under physiotherapeutic guidance started 6 weeks after surgery. While presenting in our outpatient clinic 6 months postoperatively all patients had full range of motion.
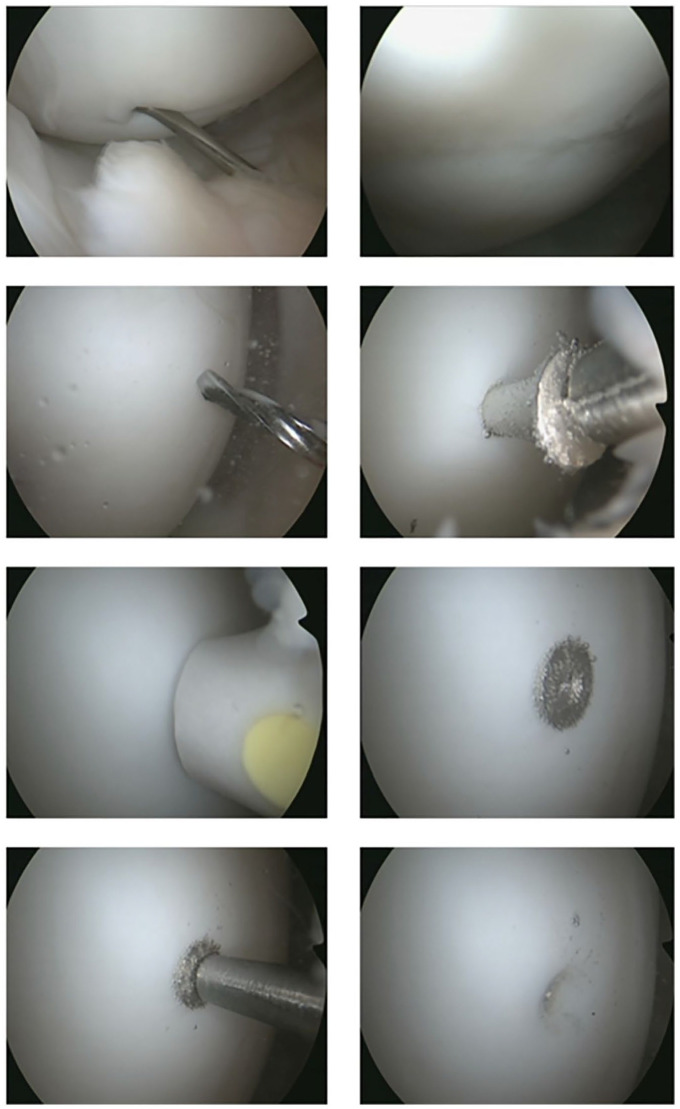
Figure 2.
Arthroscopic insertion of the pin.
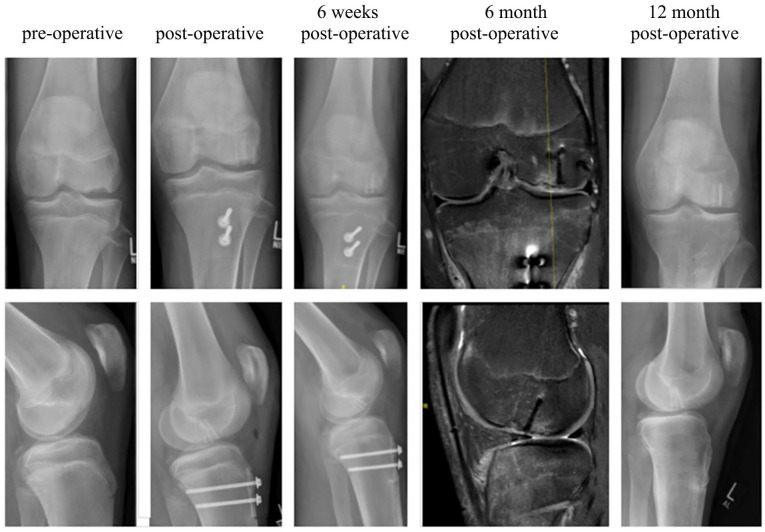
Figure 3.
Fixation of an unstable OCD lesion of the talus with 5 pins in a 16-year-old girl (patient 5).
Figure 4.
Fixation of a displaced osteochondral fragment of the lateral femur condyle after patella dislocation with 3 pins and realignment of the patella using the Elmslie-Trillat procedure in a 16-year-old boy (patient 8).
Results
Between April 2018 and March 2019, 19 patients (10 girls, 9 boys) fulfilled the inclusion criteria. Mean age at the time of surgery was 13.7 ± 1.9 years. In 9 patients an unstable OCD lesion (6 femoral, 3 talar), in 8 patients a displaced osteochondral fragment following dislocation of the patella, and in 2 patients a posttraumatic osteochondral fragment were treated by attending senior surgeons (3 different surgeons). All patients had a minimum FU of 6 months; the mean FU was 11.3 ± 4.2 months (range 6-20 months). In 4 cases the FU was longer than 12 months ( Table 1 ).
Table 1.
Patients’ Demographics, Lesion Characteristics, Surgical Procedure, and Follow-Up.
| Patient | Age (Years) | Gender | Diagnosis | Lesion Size (mm) |
ICRS | Operation | No. of Pins | FU (Months) | Union | |
|---|---|---|---|---|---|---|---|---|---|---|
| Coronal | Sagittal | |||||||||
| 1 | 12 | Female | DP, OPF | 14 | 21 | 4 | ASC knee, AT, GP | 3 | 10 | C |
| 2 | 16 | Female | OCD tali | 6 | 10 | 3 | ASC ankle joint, AT | 5 | 14 | T |
| 3 | 14 | Female | OCD MFC | 15 | 25 | 3 | ASC knee, AT | 3 | 20 | C |
| 4 | 15 | Male | OCD MFC | 7 | 45 | 3 | ASC knee | 2 | 13 | T |
| 5 | 12 | Female | OCD MFC | 19 | 28 | 3 | ASC knee | 4 | 17 | T |
| 6 | 13 | Female | OCD MFC | 14 | 23 | 3 | ASC knee | 6 | 6 | T |
| 7 | 12 | Male | OCD MFC | 17 | 24 | 3 | ASC knee, AT | 4 | 6 | C |
| 8 | 16 | Male | DP, OFLFC | 22 | 34 | 4 | ASC knee, AT, ETP | 3 | 12 | C |
| 9 | 13 | Male | TOD PFJ | 10 | 15 | 4 | ASC knee, AT | 2 | 12 | C |
| 10 | 12 | Female | DP, OFLFC | 17 | 38 | 4 | ASC knee, AT, GP | 7 | 13 | C |
| 11 | 16 | Female | OCD tali | 8 | 14 | 3 | ASC ankle joint, AT | 3 | 11 | T |
| 12 | 14 | Male | OCD MFC | 14 | 26 | 3 | ASC knee | 3 | 9 | C |
| 13 | 16 | Female | OCD tali | 9 | 16 | 3 | ASC ankle joint, AT | 3 | 7 | T |
| 14 | 15 | Female | DP, OPF | 5 | 10 | 4 | ASC knee, AT, ETP | 3 | 7 | C |
| 15 | 12 | Male | TOD PFJ | 18 | 38 | 4 | ASC knee, AT | 6 | 7 | T |
| 16 | 12 | Male | DP, OFLFC | 10 | 15 | 4 | ASC knee, AT, MPFLP | 3 | 17 | C |
| 17 | 13 | Male | DP, OPF | 20 | 14 | 4 | ASC knee, AT, GP | 2 | 13 | C |
| 18 | 11 | Female | DP, OFLFC | 14 | 19 | 4 | ASC knee, AT, GP | 4 | 15 | C |
| 19 | 17 | Male | DP, OFLFC | 12 | 14 | 4 | ASC knee, AT | 3 | 6 | C |
| Average | 13.7 ± 1.9 | 10 females, 9 males | 13.2 ± 4.9 | 22.6 ± 10.2 | 3.6 ± 1.4 | 11.3 ± 4.2 | 12 C, 7 T | |||
DP = dislocation patella; OPF = osteochondral patellar fragment; OCD = osteochondritis dissecans; MFC = medial femoral condyle; TOD = traumatic osteochondral defect; PFJ = patellofemoral joint; OFLFC = osteochondral fragment lateral femoral condyle; ASC = arthroscopy; AT = arthrotomy; GP = Goldthwait procedure; ETP = Elmslie-Trillat procedure; C = completed; T = timely.
Mean size of the osteochondral lesion was 2.3 ± 1.0 cm on sagittal and 1.3 ± 0.5 cm on coronal MRI views. In total 67 pins were used with a mean of 3.6 ± 1.4 pins per lesion (Table 1). In most cases these pins were inserted perpendicular to the joint surface to ensure maximum stability of the fixation. The diameter of the pins were 1.5 mm (n = 25) or 2.0 mm (n = 42); the length differed from 14 to 28 mm. Mean duration of surgery was 56 ± 31 minutes (26-126 minutes), including the associated surgical procedures (Elmslie-Trillat, Goldthwaith, malleolar osteotomy, and refixation). No fragmentation of the osteochondral fragments or failure of the pins occurred during operations. Intraoperative X-rays were performed only to document pin-positioning and reduction of the fragment. No prolonged wound healing or deep infections occurred. One girl complained about pain 11 weeks after fixation of an unstable femoral OCD lesion with 4 pins. The subsequently performed X-ray showed a broken pin with migration into the knee joint, requiring revision surgery ( Fig. 5 ).
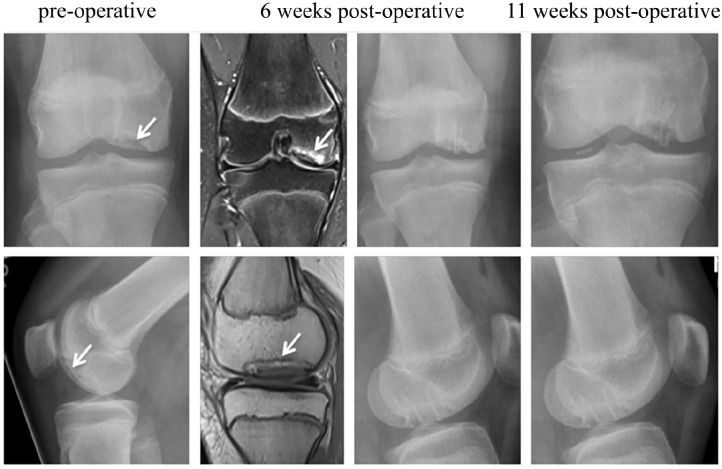
Figure 5.
Implant failure and pin migration into the knee joint 11 weeks after fixation of a very unstable femoral OCD lesion in a 12-year-old girl (patient 5).
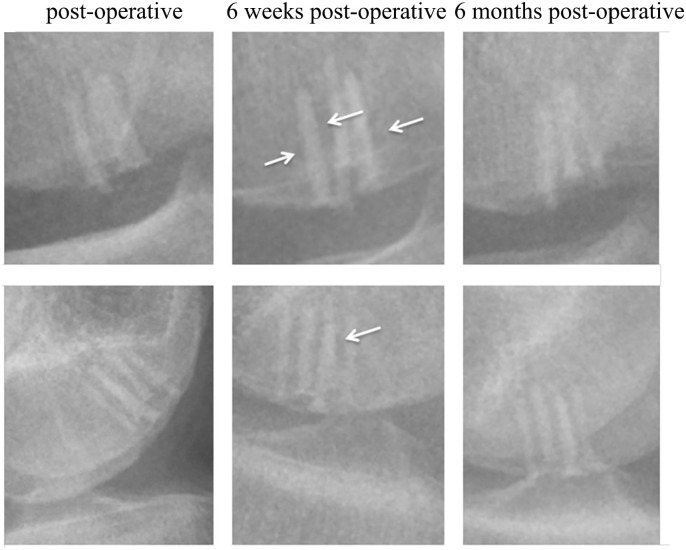
All remaining patients were pain-free and had full range of motion at the 6-month FU. Up to now a complete healing occurred in 12 cases. In the others timely signs of healing of the lesions were detected ( Table 1 , Fig. 6 ). No re-dislocation of the patella occurred. A radiolucent area around the pins was noticed in all cases 6 weeks after the operation. At the 6-month FU these areas decreased in size and were no more detectable on MRI imaging 12 months postoperatively ( Fig. 7 ).
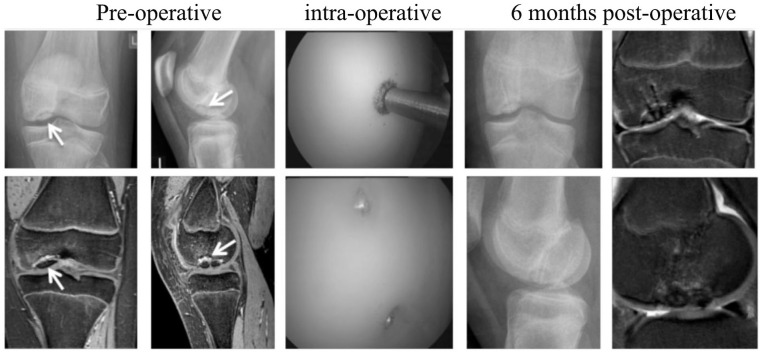
Figure 6.
Timely union of an unstable femoral OCD lesion 6 months after fixation with 6 pins in a 13-year-old girl (patient 6).
Figure 7.
Radiolucent area around the pins.
Discussion
In our study, we are reporting about fixation of unstable OCD lesions and displaced osteochondral fragments using new MAGNEZIX pins. The study indicates that magnesium-based bioabsorbable pin fixation provides adequate stability and leads to good clinical and radiologic outcomes at short-term FU.
Magnesium-Based Implants
In recent years magnesium alloys have been in the focus of research as biodegradable material. Several studies offered promising findings and reported that those devices may be used for various conditions in orthopedic surgery. 11 Biomechanical data suggested a stable bone-screw fixation related to pull out forces and maximum load capacity and therefore a great potential for medical application is given. 12 Lindtner et al. demonstrated that magnesium alloys exhibit superior bone-implant interface strength and a greater amount of peri-implant bone formation than copolymeric pins. 5 Histological analyses and micro-computed tomography scans showed new bone formation around the magnesium alloy implant indicating good osteoinductivity. 13 In 2013, the CE-certified magnesium based implants (MAGNEZIX) became commercially available and were mainly used for hallux-valgus surgery. In 2013, Windhagen et al. published results after biodegradable magnesium-based screw fixation of metatarsal-I (MTI) osteotomies in 12 patients. 14 In 2018, Plaass et al. demonstrated no differences in clinical outcome regarding fixation of distal metatarsale-I osteotomies with either a magnesium compared to a titanium implant after 3 years. Furthermore, magnesium-based implants were degraded but not fully remodeled after 3 years as seen on MRIs. 9
Klauser found no significant differences regarding wound healing and signs of healing within 6 weeks after magnesium-based (n = 100 patients) compared to titanium-based screw fixation of MTI osteotomies. However, one screw failure was found in the magnesium group. 15
Biodegradable Fixation of Unstable OCD Lesions and Osteochondral Fragments
Outcome after fixation of unstable osteochondral lesions with bioresorbable devices is well documented in literature. Abouassaly et al. published a systematic review addressing different surgical techniques in 2014. 3 For unstable OCD lesions arthroscopic and open fixation with bioabsorbable pins, metal or bioabsorbable screws, and transarticular drilling with bioabsorbable pin or screw fixation were studied and compared to other procedures. 3 Besides good mid- and long-term results, 1 implant failures were documented. Camathias et al. found a rate of 23% (14 of a total of 61 screws) implant failures after biodegradable screw fixation (made of poly-L-lactic acid 96L/4D copolymer) in femoral OCD in skeletally immature patients. 4 Millington et al. reported a low rate of clinical healing and high complication rate after bioabsorbable fixation of unstable OCD lesions. Two of 11 patients (18%) treated with bioabsorbable nails required revision surgery for nail back-out. 16 To prevent implant failure, technique of fixation of the device is crucial. Lindtner et al. reported experimental data, demonstrating superior bone-implant interface strength and a greater amount of peri-implant bone with magnesium-based pins than copolymeric pins. 5 Until now, reports focusing on magnesium-based pin fixation of unstable OCD lesions and osteochondral fragments are still missing.
Results and Complications
In this case series using magnesium-based pins no intraoperative complications occurred. The goal to maintain high stability of fixation for OCDs and osteochondral fragments was achieved. These results are consistent with the findings after the use of magnesium-based screw fixations of osteotomies and fractures. Only one of overall 67 pins broke and needed surgical revision. In this single case a femoral OCD lesion was fixed with 4 pins. The preoperative MRI showed multiple subchondral cysts indicating a very unstable situation. The stability of the pins after 75 days is supposed to be 80% of the initial stability according to the statement of the manufacturer. Most likely, the biomechanical strength of the pin 11 weeks after implantation was no longer strong enough to compensate for shear forces during joint motion. After revision and repeated drilling the OCD lesion healed. The good visibility of magnesium-based implants on X-rays and MRI films even several weeks after implantation facilitates the early diagnosis of implant failure and loosening. In all other OCD cases we noticed a stable situation of the lesion and a timely healing process 6 months after operation. All displaced osteochondral fragments associated with patellar dislocation were healed at this time. This could be caused by the pin design including symmetric collars on the pin shank and a nail-like head, enabling a good compression of the free osteochondral fragment during impaction of the pin. In OCD lesions with multiple large perifocal cysts indicating a very unstable situation, we recommend to fill the lesion with cancellous bone prior to pin fixation.
Radiolucent Area around the Implant
There are some reports about the radiolucent area around magnesium-based implants in the literature.11,15 In our study this phenomenon was apparent on radiographs in all cases 6 weeks after implantation. Klauser found radiolucent signs in 40% of the magnesium group 6 weeks after the operation. 15 No patient was complaining about pain, and all patients were allowed full weight bearing without consecutive complications. 15 Up to now, these radiolucencies are not fully understood. However, knowledge of their incidence should be made available to radiologists to avoid misinterpretations.15,17 Probably these findings are due to a hydrogen development as a natural phenomenon during the corrosion process of magnesium. 7 Kose et al. recommend that mild radiolucency around the implants during the first 12 months of the postoperative period should not be misinterpreted as osteolysis. They observed that this phenomenon does not cause any clinical symptoms and does not adversely affect fracture healing and normally disappears after 6 to 12 months. 8 Up to now there are 2 case series reporting problems after the application of magnesium-based screws. The first report is about fixation of scaphoid fractures in 5 cases with cyst formation in the early postoperative period in 3 of 5 patients but finally complete healing and excellent functional scores. 18 The second report is about one case of carpal fusion surgery with postoperative cyst formation und revision surgery. 19 All other previous reports with FU of 6 months to 3 years showed successful healing after osteotomies and fracture repairs with magnesium-based screws.7,8,15
Limitations and Strengths
Limitations of this study are the number of patients, the short FU, and the lack of a control group. However, (1) this is the first study reporting on short-term results with these implants and the method is becoming widespread, and (2) the FU is long enough to document healing in all cases of displaced osteochondral fragments associated with trauma and dislocation of the patella in children and adolescents.
Conclusion
In short-term FU of 11 months magnesium-based pins (MAGNEZIX) provide high stability for fixation of unstable OCD and osteochondral lesions after trauma or patella dislocation and allow for adequate bone healing. No intraoperative complications were seen. One implant failure (1 of 67) occurred, requiring revision surgery. A transient radiolucent area around the pins was seen in all cases 6 weeks after implantation.
Footnotes
Acknowledgments and Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Martin Rupprecht advises the Syntellix AG (Hannover, Germany) on clinical matters. The other authors have no conflicts of interest to disclose.
Ethical Approval: This study was approved by our institutional review board Ethikkommission Ärztekammer Hamburg WF-075/20.
Informed Consent: Written informed consent was obtained from all subjects before the study.
ORCID iD: Oliver D. Jungesblut  https://orcid.org/0000-0002-7092-7894
https://orcid.org/0000-0002-7092-7894
References
- 1. Perelli S, Romoli ARM, Costa-Paz M, Erquicia JI, Gelber PE, Monllau JC. Internal fixation of osteochondritis dissecans of the knee leads to good long-term outcomes and high degree of healing without differences between fixation devices. J Clin Med. 2019;10;8(11):1934. doi: 10.3390/jcm81119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Randsborg PH, Kjennvold S, Røtterud JH. Arthroscopic fixation of osteochondritis dissecans of the knee using a motorized pick and headless compression screws. Arthrosc Tech. 2019;10:1115-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Abouassaly M, Peterson D, Salci L, Farrokhyar F, D’Souza J, Bhandari M, et al. Surgical management of osteochondritis dissecans of the knee in the paediatric population: a systematic review addressing surgical techniques. Knee Surg Sports Traumatol Arthrosc. 2014;22:1216-24. [DOI] [PubMed] [Google Scholar]
- 4. Camathias C, Gögüs U, Hirschmann MT, Rutz E, Brunner R, Haeni D, et al. Implant failure after biodegradable screw fixation in osteochondritis dissecans of the knee in skeletally immature patients. Arthroscopy. 2015;31(3):410-5. [DOI] [PubMed] [Google Scholar]
- 5. Lindtner RA, Castellani C, Tangl S, Zanoni G, Hausbrandt P, Tschegg EK, et al. Comparative biomechanical and radiological characterization of osseointegration of a biodegradable magnesium alloy pin and a copolymeric control for osteosynthesis. J Mech Behav Biomed Mater. 2013;28:232-43. [DOI] [PubMed] [Google Scholar]
- 6. Könneker S, Krockenberger K, Pieh C, von Falck C, Brandewiede B, Vogt PM, et al. Comparison of SCAphoid fracture osteosynthesis by MAGnesium-based headless Herbert screws with titanium Herbert screws: protocol for the randomized controlled SCAMAG clinical trial. BMC Musculoskelet Disord. 2019;20:357. doi: 10.1186/s12891-019-2723-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Plaass C, Ettinger S, Sonnow L, Koenneker S, Noll Y, Weizbauer A, et al. Early results using a biodegradable magnesium screw for modified chevron osteotomies. J Orthop Res. 2016;34:2207-14. [DOI] [PubMed] [Google Scholar]
- 8. Kose O, Turan A, Unal M, Acar B, Guler F. Fixation of medial malleolar fractures with magnesium bioabsorbable headless compression screws: short-term clinical and radiological outcomes in eleven patients. Arch Orthop Trauma Surg. 2018;138:1069-75. [DOI] [PubMed] [Google Scholar]
- 9. Plaass C, von Falck C, Ettinger S, Sonnow L, Calderone F, Weizbauer A, et al. Bioabsorbable magnesium versus standard titanium compression screws for fixation of distal metatarsal osteotomies—3 year results of a randomized clinical trial. J Orthop Sci. 2018;23:321-7. [DOI] [PubMed] [Google Scholar]
- 10. Dipaola JD, Nelson DW, Colville MR. Characterizing osteochondral lesions by magnetic resonance imaging. Arthroscopy. 1991;7(1_suppl):101-4. [DOI] [PubMed] [Google Scholar]
- 11. Sonnow L, Könneker S, Vogt PM, Wacker F, von Falck C. Biodegradable magnesium Herbert screw—image quality and artifacts with radiography, CT and MRI. BMC Med Imaging. 2017;17:16 doi: 10.1186/s12880-017-0187-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Waizy H, Weizbauer A, Maibaum M, Witte F, Windhagen H, Lucas A, et al. Biomechanical characterisation of a degradable magnesium-based (MgCa0.8) screw. J Mater Sci Mater Med. 2012;23:649-55. [DOI] [PubMed] [Google Scholar]
- 13. Waizy H, Diekmann J, Weizbauer A, Reifenrath J, Bartsch I, Neubert V, et al. In vivo study of a biodegradable orthopedic screw (MgYREZr-alloy) in a rabbit model for up to 12 months. J Biomater Appl. 2014;28:667-75. [DOI] [PubMed] [Google Scholar]
- 14. Windhagen H, Radtke K, Weizbauer A, Diekmann J, Noll Y, Kreimeyer U, et al. Biodegradable magnesium-based screw clinically equivalent to titanium screw in hallux valgus surgery: short term results of the first prospective, randomized, controlled clinical pilot study. Biomed Eng Online. 2013;12:62. doi: 10.1186/1475-925X-12-62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Klauser H. Internal fixation of three-dimensional distal metatarsal I osteotomies in the treatment of hallux valgus deformities using biodegradable magnesium screws in comparison to titanium screws. Foot Ankle Surg. 2019;25:398-405. [DOI] [PubMed] [Google Scholar]
- 16. Millington KL, Shah JP, Dahm DL, Levy BA, Stuart MJ. Bioabsorbable fixation of unstable osteochondritis dissecans lesions. Am J Sports Med. 2010;38:2065-70. [DOI] [PubMed] [Google Scholar]
- 17. Seitz JM, Lucas A, Kirschner M. Magnesium-based compression screws: a novelty in the clinical use of implants. JOM. 2016;68:1177-82. [Google Scholar]
- 18. Meier R, Panzica M. First results with a resorbable MgYREZr compression screw in unstable scaphoid fractures show extensive bone cysts [in German]. Handchir Mikrochir Plast Chir. 2017;49:37-41. [DOI] [PubMed] [Google Scholar]
- 19. Wichelhaus A, Emmerich J, Mittlmeier T. A case of implant failure in partial wrist fusion applying magnesium-based headless bone screws. Case Rep Orthop. 2016;2016:7049130. [DOI] [PMC free article] [PubMed] [Google Scholar]