Abstract
Objective:
This cross-sectional study aimed to explore the differences of the medial and lateral sides of the knee joint and precise radiographic abnormalities in contribution to the knee pain and clinical outcomes.
Design:
Participants 60 years or older who underwent radiographic evaluation were included. Knee radiography was assessed using grading systems of the Osteoarthritis Research Society International (OARSI) atlas. The Japanese Knee Osteoarthritis Measure (JKOM) was evaluated as clinical outcomes. Serum high-sensitivity C-reactive protein (hsCRP) was used to evaluate systemic inflammation. We divided the participants into normal, medial-, lateral-, and medial & lateral-OA types and compared their JKOM using an analysis of covariance. Furthermore, we analyzed the relationship between the knee pain and stiffness of JKOM and the grading of each radiographic feature using a multiple regression model.
Results:
Lateral- and medial & lateral-OA groups had a significantly worse symptoms in the total and the pain score, especially in movement subscales, in JKOM score. Lateral-OA groups had higher hsCRP than medial-OA group. Multivariate analysis showed that medial joint space narrowing (JSN), and lateral femoral and tibial osteophytes significantly affected knee pain (adjusted odds ratios: 1.73, 1.28, and 1.55, respectively). The radiographic changes are associated with pain more in JSN in the medial side and osteophytes in the lateral side.
Conclusion:
Lateral- and medial & lateral-OA groups showed worth symptom. In addition, medial JSN and lateral osteophytes have potent effects on the knee pain.
Keywords: osteoarthritis, knee pain, radiography, inflammation, C-reactive protein
Introduction
Knee osteoarthritis (OA) is one of the most prevalent musculoskeletal diseases in the elderly population, and pain is the most frequent, predominant, and troublesome symptom of knee OA. 1 Although it is well known that many structural and degenerative changes occur in the radiolucent tissues of the knee joint, such as articular cartilage tissues, menisci, ligaments, and synovial tissues, radiographic changes are the most reliable features in diagnosing knee OA and in evaluating the severity of the disease. Numerous recent reports have shown that magnetic resonance imaging (MRI) has a superior capability to detect nonradiographic changes2,3; however, MRI has not surpassed the superiority of radiography in terms of cost, accessibility, availability, and handling. Thereby, radiographic diagnosis remains the gold standard for diagnosing knee OA and has been approved by experts for use in large cohort studies. 4
Although the radiographic features of knee OA have been well established, including joint space narrowing (JSN), osteophytes, subchondral sclerosis, and attrition, 5 the relationship between such features and knee pain has been inconsistently reported, and radiographic severity does not always correlate with pain intensity or functional impairment.6,7 One of the reasons for this is that the current grading of knee OA is a global assessment rather than a precise evaluation. The Kellgren-Lawrence (K-L) system, one of the most widely used classification systems, has only 5 grades. 8 In contrast, the Osteoarthritis Research Society International (OARSI) atlas criteria involve more precise evaluations, including grading of JSN, osteophytes, subchondral sclerosis, and attrition, separately in the medial and lateral tibiofemoral compartments.9,10 However, the relationship between individual features and symptoms has not been well elucidated in this grading system. Because defining the subgroups of knee OA may help resolve the discordance between radiographic findings and clinical outcomes, we previously compared knee OA subgroups by using simple radiographic features, as follows: knees with coexisting lateral OA and medial OA and knees with medial OA alone. 11 Knees with coexisting lateral OA and medial OA had more severe pain than knees with medial OA alone, and the presence of lateral knee OA was significantly associated with a higher risk of knee pain during stair descent and standing. However, the study included only participants with a K-L grade of 2, and the sample size was small. Moreover, the precise associations between individual radiographic features and symptoms remain to be investigated.
Therefore, the present cross-sectional study aimed to investigate whether radiographic abnormalities are precisely related to knee pain and clinical outcomes, especially in terms of differences in the medial and lateral sides of the joint. To address this aim, this study took advantage of a large community-based cohort that included almost 10,000 individuals with available data on various demographic and radiographic features.
Materials and Methods
Study Population
This cross-sectional study used data from the Nagahama Prospective Cohort for Comprehensive Human Bioscience (Nagahama Study). The Nagahama Study included 9850 middle-aged to elderly citizens who were recruited from 2013 to 2016 from the general population living in Nagahama City, a rural city of 125,000 inhabitants located in central Japan. Residents aged 34 to 80 years living independently in the community were recruited. The details of participant recruitment have been reported elsewhere. 12
Participants aged ≥60 years who underwent radiographic evaluation were included in the present study. Among them, those with the same total OARSI score for both knees but with a different distribution of features were excluded, and the knee with the worse OARSI score was considered the representative knee. Only participants who completed a questionnaire about knee symptoms without missing data were considered eligible for the analysis.
Research Ethics and Patient Consent
This study was conducted in accordance with the principles of the Declaration of Helsinki and was approved by the ethics committee of Kyoto University Graduate School of Medicine and by the Nagahama Municipal Review Board (No. C278). Written informed consent was obtained from all participants.
Radiographic Evaluation
The participants underwent anteroposterior radiography of the knee joints in the fully extended weight-bearing position. The radiological severity of the knee joints was evaluated by a registered orthopedic surgeon (TK) and a trained examiner (KaN) using the standard scale from the OARSI atlas9,10 and the K-L grade. 8 In the presence of any disagreement between the scores or grades assessed by the 2 examiners, a third examiner (HI) assessed the radiographs and determined the final scores and grades. JSN and osteophytes were graded on a 4-point scale (0-3; 0: normal, 1: mild, 2: moderate, and 3: severe) with reference to the example radiographs in the OARSI atlas.9,10
Radiographic OA (R-OA) according to the OARSI atlas grading system was considered to be present when any one of the following 3 criteria was met: (1) JSN ≥ grade 2, (2) sum of the 2 marginal osteophyte grades from the same compartment ≥2, or (3) grade 1 JSN combined with grade 1 osteophytes.5,13,14
The index knee was defined as follows: (1) the knee with greater total OARSI score (medial femoral osteophyte [MFO] + medial tibial osteophyte [MTO] + lateral femoral osteophyte [LFO] + lateral tibial osteophyte [LTO] + medial JSN [MJSN] + lateral JSN [LJSN]) or (2) both the right and left knees if they have the same total OARSI score and exactly the same OARSI score for each feature.
To examine whether there were differences in symptoms according to the radiographic structural characteristics of the knee, the analysis set was divided into 4 groups: (1) no R-OA on both the medial and lateral sides, normal group; (2) R-OA on the medial side only, medial-OA group; (3) R-OA on the lateral side only, lateral-OA group; and (4) R-OA on both the medial and lateral sides, medial & lateral-OA group.
To evaluate intrarater reliability, 50 randomly selected radiographs were rescored by the same examiner (KN) >1 week after the first assessment. The intrarater reliability was “almost perfect” for JSN (weighted κ = 0.92, 95% confidence interval [CI]: 0.85-0.99) and osteophytes (weighted κ = 0.90, 95% CI: 0.87-0.93). The interrater reliability, assessed using 50 randomly selected radiographs, between 2 examiners (KT and KN) was “almost perfect” for JSN (weighted κ = 0.83, 95% CI: 0.73-0.94) and osteophytes (weighted κ = 0.81, 95% CI: 0.77-0.86). 15
Clinical Outcome
We used the Japanese Knee Osteoarthritis Measure (JKOM), which is a validated outcome measure for Japanese patients with knee OA,7,16,17 to identify knee symptoms in the participants. The JKOM consists of 4 main items: pain and stiffness (pain; a total of 8 questions, 0-32 points), activities of daily living (ADL; a total of 10 questions, 0-40 points), participation in social activities (social activity; a total of 5 questions, 0-20 points), and general health conditions (general health; a total of 2 questions, 0-8 points), with a total score of 100 points. A higher JKOM score indicates a worse condition. A previous study has shown the reliability and validity of the JKOM for assessing clinical outcomes in comparison with other health-related scales such as the Western Ontario and McMaster Universities Arthritis Index (WOMAC) and the Medical Outcomes Study 36-Item Short-form Health Survey (SF-36). 16 All participants self-reported their responses on the JKOM questionnaire.
Clinical Biomarker
High-sensitivity C-reactive protein (hsCRP) was measured (reagent: CardioPhase hsCRP; instrumentation: BN II system; Siemens) as an inflammatory biomarker. We converted any undetectable hsCRP levels (≤0.05 µg/mL, 23 participants) to 0.05 µg/mL for the analysis.
Statistical Analyses
Descriptive statistics are reported as means and standard deviations for continuous variables, and as proportions for dichotomous/categorical variables. Differences in JKOM scores between subgroups were compared using analysis of covariance. Odds ratios of the presence of the individual items on the “pain and stiffness” scale were calculated for each group in comparison to the normal group, adjusted for age, sex, body mass index (BMI), presence of depression, and duration of knee symptoms. The hsCRP levels of the subgroups were compared using Student’s t-test. Single and multiple regression analyses were used to examine the associations between radiographic features defined by the OARSI atlas and the JKOM pain score, adjusted for age, sex, BMI, presence of depression, and muscle mass of the lower extremity. Subjects were analyzed as having symptoms if there were any symptoms in the knee (JKOM pain score ≥ 1). A linear mixed model was used to examine whether the effects of a high OARSI grade on the JKOM pain score differed at each site. The threshold for significance was set at P < 0.05. All statistical analyses were conducted using JMP Pro (version 14.0.0; SAS Institute, Cary, NC).
Results
Study Population
A total of 9,850 participants were assessed for eligibility in this study. Participants aged ≥60 years (n = 5,018) were included in the first surveillance and were asked to undergo further radiographic evaluation (knee radiography). Of them, 1,739 participants declined. The remaining 3,279 participants agreed to be included in this study. After the full set of data was surveyed, 384 participants with the same total OARSI score on both knees with a different distribution of features were excluded from further analyses. Of the remaining participants, 652 who did not complete the JKOM questionnaire were excluded. Finally, 2,253 participants were included in the full analysis set.
Clinical Outcomes
Table 1 shows the demographic data of each group. The medial & lateral-OA group was the most predominant, followed by the normal group. The medial-OA and medial & lateral-OA groups included more female participants, whereas the lateral-OA group had more male participants.
Table 1.
Demographic Data of Each Group.
| Normal (n = 663) | Medial (n = 363) | Lateral (n = 268) | Medial & Lateral (n = 959) | Analysis Population (n = 2,253) | |
|---|---|---|---|---|---|
| Age, years, mean (SD) | 67.7 (5.0) | 67.4 (4.9) | 69.1 (5.0) | 69.7 (5.2) | 68.7 (5.2) |
| Female | 349, 52.6 | 280, 77.1 | 102, 38.1 | 712, 74.2 | 1,443, 64.1 |
| BMI, kg/m2, mean (SD) | 21.5 (2.8) | 22.0 (3.1) | 22.5 (3.0) | 23.1 (3.2) | 22.4 (3.1) |
| Radiographic severity | |||||
| K/L grade 0 | 93, 14.0 | 1, 0.3 | 3, 1.1 | 0, 0 | 97, 4.3 |
| K/L grade 1 | 557, 84.0 | 259, 71.4 | 255, 95.2 | 191, 19.9 | 1262, 56.0 |
| K/L grade 2 | 13, 2.0 | 91, 25.1 | 9, 3.4 | 568, 59.2 | 681, 30.2 |
| K/L grade 3 | 0, 0 | 12, 3.3 | 1, 0.4 | 183, 18.9 | 194, 8.6 |
| K/L grade 4 | 0, 0 | 0, 0 | 0, 0 | 19, 2.0 | 19, 0.8 |
| OARSI atlas | |||||
| Medial femoral osteophyte | |||||
| Grade 0 (normal) | 344, 51.9 | 1, 0.3 | 147, 54.9 | 1, 0.1 | 493, 21.9 |
| Grade 1 (mild) | 319, 48.1 | 343, 94.5 | 121, 45.2 | 658, 68.6 | 1441, 64.0 |
| Grade 2 (moderate) | 0, 0 | 18, 5.0 | 0, 0 | 217, 22.6 | 235, 10.4 |
| Grade 3 (severe) | 0, 0 | 1, 0.3 | 0, 0 | 83, 8.7 | 84, 3.7 |
| Medial tibial osteophyte | |||||
| Grade 0 (normal) | 540, 81.5 | 2, 0.6 | 200, 74.6 | 4, 0.4 | 746, 33.1 |
| Grade 1 (mild) | 123, 18.6 | 349, 96.1 | 68, 25.4 | 711, 74.1 | 1251, 55.5 |
| Grade 2 (moderate) | 0, 0 | 11, 3.0 | 0, 0 | 198, 20.7 | 209, 9.3 |
| Grade 3 (severe) | 0, 0 | 1, 0.3 | 0, 0 | 46, 4.8 | 47, 2.1 |
| Medial joint space narrowing | |||||
| Grade 0 (normal) | 661, 99.7 | 336, 92.6 | 267, 99.6 | 679, 70.8 | 1943, 86.2 |
| Grade 1 (mild) | 2, 0.3 | 23, 6.3 | 1, 0.4 | 183, 19.1 | 209, 9.3 |
| Grade 2 (moderate) | 0, 0 | 3, 0.8 | 0, 0 | 60, 6.3 | 63, 2.8 |
| Grade 3 (severe) | 0, 0 | 1, 0.3 | 0, 0 | 37, 3.9 | 38, 1.7 |
| Lateral femoral osteophyte | |||||
| Grade 0 (normal) | 441, 66.5 | 282, 77.7 | 3, 1.1 | 5, 0.5 | 731, 32.5 |
| Grade 1 (mild) | 222, 33.5 | 81, 22.3 | 258, 96.3 | 769, 80.2 | 1330, 59.0 |
| Grade 2 (moderate) | 0, 0 | 0, 0 | 6, 2.2 | 156, 16.3 | 162, 7.2 |
| Grade 3 (severe) | 0, 0 | 0, 0 | 1, 0.4 | 29, 3.0 | 30, 1.3 |
| Lateral tibial osteophyte | |||||
| Grade 0 (normal) | 473, 71.3 | 173, 47.7 | 1, 0.4 | 1, 0.1 | 648, 28.8 |
| Grade 1 (mild) | 190, 28.7 | 190, 52.3 | 256, 95.5 | 744, 77.6 | 1380, 61.3 |
| Grade 2 (moderate) | 0, 0 | 0, 0 | 11, 4.1 | 173, 18.0 | 184, 8.2 |
| Grade 3 (severe) | 0, 0 | 0, 0 | 0, 0 | 41, 4.3 | 41, 1.8 |
| Lateral joint space narrowing | |||||
| Grade 0 (normal) | 662, 99.9 | 363, 100 | 268, 100 | 901, 94.0 | 2194, 97.4 |
| Grade 1 (mild) | 1, 0.2 | 0, 0 | 0, 0 | 46, 4.8 | 47, 2.1 |
| Grade 2 (moderate) | 0, 0 | 0, 0 | 0, 0 | 6, 0.6 | 6, 0.3 |
| Grade 3 (severe) | 0, 0 | 0, 0 | 0, 0 | 6, 0.6 | 6, 0.3 |
BMI = body mass index; K/L = Kellgren/Lawrence; OARSI = Osteoarthritis Research Society International.
Values are n, %, except where otherwise indicated.
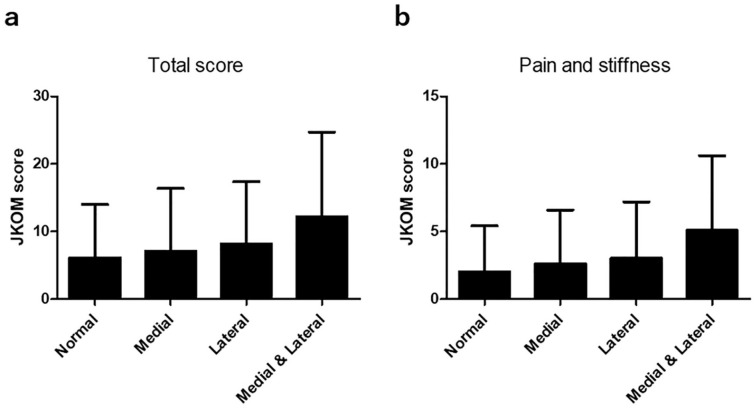
The JKOM score in each group and the odds ratio of the presence of pain to the normal group are shown in Figure 1 , Supplementary Table 1, and Table 2. Analysis of covariance showed statistically significant differences in all items, with the medial & lateral-OA group showing the worst symptoms. Table 2 shows that the lateral-OA group showed worse symptoms than the normal and medial-OA groups, as well as a significantly higher odds ratio in several items than the medial-OA group, especially in movement subscales such as descending and ascending stairs. These results suggest that the presence of structural abnormalities on the lateral side may result in worse symptoms than abnormalities on the medial side.
Figure 1.
JKOM value of each group. (a) Total score of JKOM. (b) Pain and stiffness score of JKOM. Higher JKOM score indicates worse condition. JKOM = Japanese Knee Osteoarthritis Measure.
Table 2.
The Odds Ratio of Presence of Pain in Each Group to the Normal Group a .
| Individual Item of JKOM Pain and Stiffness | Medial |
Lateral |
Medial & Lateral |
|||
|---|---|---|---|---|---|---|
| Adjusted OR (95% CI) | P Value | Adjusted OR (95% CI) | P Value | Adjusted OR (95% CI) | P Value | |
| Do you feel stiffness in your knees when you wake up in the morning? | 1.38 (1.02-1.89) | 0.0399 | 1.78 (1.29-2.46) | 0.0004 | 2.66 (2.08-3.39) | <0.0001 |
| Do you feel pain in your knees when you wake up in the morning? | 1.41 (1.04-1.92) | 0.0271 | 1.78 (1.29-2.46) | 0.0004 | 2.99 (2.35-3.82) | <0.0001 |
| How often do you wake up in the night because of pain in your knees? | 1.37 (0.86-2.18) | 0.1863 | 2.01 (1.27-3.20) | 0.0029 | 2.85 (1.99-4.07) | <0.0001 |
| Do you have pain in your knees when you walk on a flat surface? | 1.48 (1.06-2.07) | 0.0208 | 1.56 (1.09-2.23) | 0.0141 | 3.04 (2.34-3.96) | <0.0001 |
| Do you have pain in your knees when ascending stairs? | 1.20 (0.90-1.60) | 0.214 | 1.42 (1.04-1.93) | 0.0275 | 2.66 (2.11-3.34) | <0.0001 |
| Do you have pain in your knees when descending stairs? | 1.23 (0.92-1.65) | 0.1593 | 1.43 (1.04-1.95) | 0.0269 | 2.81 (2.22-3.54) | <0.0001 |
| Do you have pain in your knees when bending to floor or standing up? | 1.31 (1.00-1.72) | 0.05 | 1.42 (1.06-1.91) | 0.0197 | 2.85 (2.28-3.56) | <0.0001 |
| Do you have pain in your knees when standing? | 1.14 (0.82-1.58) | 0.4269 | 1.26 (0.89-1.78) | 0.1952 | 2.45 (1.90-3.15) | <0.0001 |
| Total | 1.18 (0.91-1.54) | 0.2195 | 1.35 (1.01-1.81) | 0.0428 | 2.44 (1.95-3.05) | <0.0001 |
JKOM = Japanese Knee Osteoarthritis Measure; OR = odds ratio; CI = confidence interval; BMI = body mass index.
Odds ratio of the presence of the individual items on the “pain and stiffness” scale were calculated for each group in comparison to the Normal group, adjusted for age, sex, BMI, presence of depression and duration of knee symptoms. Boldface indicates statistical difference.
Clinical Biomarker
The serum hsCRP levels (mean and standard deviation) in the normal, medial-OA, lateral-OA, and medial & lateral-OA groups were 0.74 (1.26), 0.75 (1.91), 1.29 (2.72), and 0.95 (2.16) µg/mL, respectively ( Fig. 2 ). The lateral-OA group showed significantly higher CRP levels than the other groups.
Figure 2.
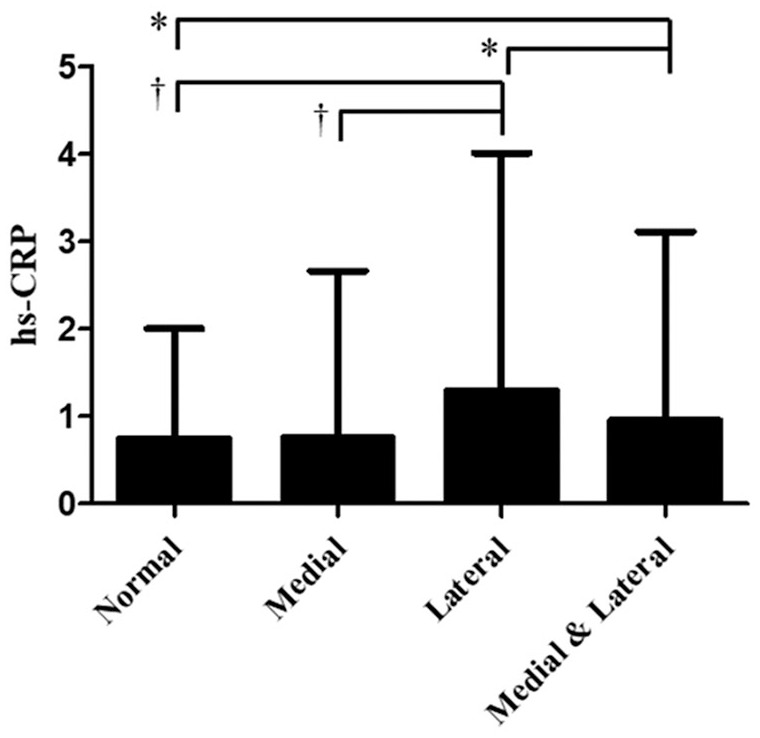
hs-CRP value of each group.
Bars show the mean and SD. P values were calculated using Student’s t test.
*P < 0.05, †P < 0.001.
hs-CRP = high sensitivity C-reactive protein.
Radiographic Features and Symptoms
To evaluate the associations between individual radiographic features and symptoms, we further analyzed the relationship between the JKOM pain and stiffness score and the grade of each radiographic feature ( Fig. 3 and Suppl. Table 2). In all items, the symptoms worsened as the grade increased, except for LJSN (grade 1 to grade 2). A simple regression analysis showed that each item had a significant effect on pain ( Table 3 ). Multivariate analysis showed that MJSN, LFO, and LTO significantly affected pain with higher adjusted odds ratios ( Table 3 ), indicating that the lateral compartment causes worse symptoms.
Figure 3.
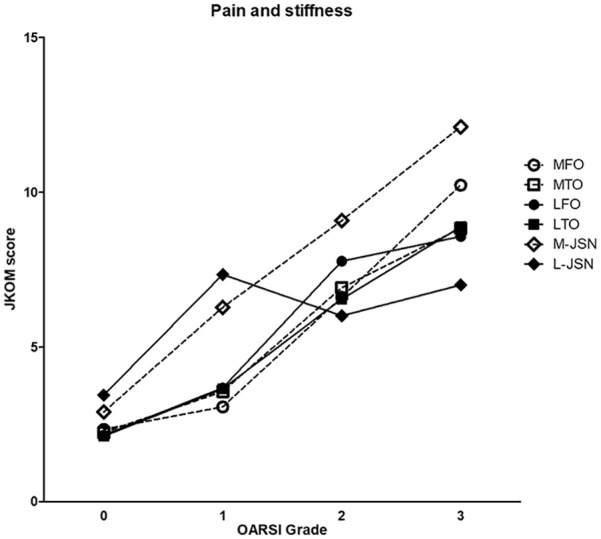
Relation between the pain and stiffness of JKOM and the grading of each radiographic feature. Higher JKOM score indicates worse condition.
MFO = medial femoral osteophyte; MTO = medial tibial osteophyte; LFO = lateral femoral osteophyte; LTO = lateral tibial osteophyte; M-JSN = medial joint space narrow; L-JSN = lateral joint space narrow; JKOM = Japanese Knee Osteoarthritis Measure.
Table 3.
Single and Multiple Regression Analysis to Examine the Associations between Radiographic Features Defined by OARSI Atlas and JKOM Pain Score.
| Simple Regression
Analysis |
Multiple Regression Analysis
a
|
|||
|---|---|---|---|---|
| OR (95% CI) | P Value | OR (95% CI) | P Value | |
| Medial femoral osteophyte | 2.05 (1.79-2.36) | <0.0001 | 1.18 (0.98-1.42) | 0.0768 |
| Medial tibial osteophyte | 2.01 (1.76-2.31) | <0.0001 | 1.12 (0.94-1.35) | 0.1969 |
| Medial joint space narrowing | 3.09 (2.39-4.00) | <0.0001 | 1.73 (1.32-2.28) | <0.0001 |
| Lateral femoral osteophyte | 2.14 (1.84-2.47) | <0.0001 | 1.28 (1.07-1.54) | 0.0065 |
| Lateral tibial osteophyte | 2.39 (2.06-2.78) | <0.0001 | 1.55 (1.29-1.86) | <0.0001 |
| Lateral joint space narrowing | 3.31 (1.67-5.87) | 0.0004 | 1.49 (0.82-2.70) | 0.1612 |
OR = odds ratio; CI = confidence interval; BMI = body mass index.
Adjusted by age, sex, BMI, presence of depression, and muscle mass of lower extremity. Boldface indicates statistical significance.
To evaluate the effect of increasing OARSI score among different radiographic features on the JKOM score, we used a linear mixed model by subtracting one score from another ( Table 4 ). The results of the analysis showed that pain was more likely to increase when the grades of osteophytes on the lateral side of the femur increased, with no difference in tibial osteophytes ( Table 4A ). With respect to JSN, the medial side had a greater effect than the lateral side ( Table 4A ). Between JSN and osteophytes, JSN in both the femur and tibia had greater effects. In contrast, lateral JSN was more frequently associated with pain than lateral osteophytes in both the femur and tibia only when the grade changed from 0 to 1, whereas lateral osteophytes had greater effects than lateral JSN when the grade changed from 1 to 2 and from 2 to 3 ( Table 4B ).
Table 4.
Differences of Changes in JKOM Values at Each Site with Worsening of OARSI Grade.
| (A) Difference in Lateral and Medial | |||
|---|---|---|---|
| Mean Difference | 95% CI | P Value | |
| Grade 0 → 1 | 0.799 | 0.185 to 1.413 | 0.011 |
| Grade 1 → 2 | 1.351 | 0.312 to 2.391 | 0.011 |
| Grade 2 → 3 | −1.474 | −3.431 to 0.483 | 0.140 |
| LTO-MTO | |||
| Grade 0 → 1 | 0.204 | −0.392 to 0.800 | 0.503 |
| Grade 1 → 2 | −0.252 | −1.280 to 0.776 | 0.631 |
| Grade 2 → 3 | 0.162 | −1.816 to 2.140 | 0.872 |
| LJSN-MJSN | |||
| Grade 0 → 1 | 0.524 | −0.991 to 2.039 | 0.498 |
| Grade 1 → 2 | −3.623 | −7.597 to 0.351 | 0.074 |
| Grade 2 → 3 | −5.649 | −9.722 to −1.576 | 0.007 |
| (B) Difference in Joint Space Narrow and Osteophyte | |||
| Mean Difference | 95% CI | P Value | |
| LFO-MFO | |||
| MJSN-MFO | |||
| Grade 0 → 1 | 2.646 | 1.864 to 3.429 | 0.000 |
| Grade 1 → 2 | 1.914 | 0.599 to 3.229 | 0.004 |
| Grade 2 → 3 | 1.314 | −0.450 to 3.077 | 0.144 |
| MJSN-MTO | |||
| Grade 0 → 1 | 2.048 | 1.290 to 2.807 | 0.000 |
| Grade 1 → 2 | 1.502 | 0.183 to 2.821 | 0.026 |
| Grade 2 → 3 | 2.607 | 0.645 to 4.570 | 0.009 |
| LJSN-LFO | |||
| Grade 0 → 1 | 2.371 | 0.936 to 3.806 | 0.001 |
| Grade 1 → 2 | −3.060 | −6.952 to 0.831 | 0.123 |
| Grade 2 → 3 | −2.861 | −7.021 to 1.298 | 0.178 |
| LJSN-LTO | |||
| Grade 0 → 1 | 2.368 | 0.928 to 3.809 | 0.001 |
| Grade 1 → 2 | −1.869 | −5.756 to 2.018 | 0.346 |
| Grade 2 → 3 | −3.204 | −7.284 to 0.876 | 0.124 |
MFO = medial femoral osteophyte; MTO = medial tibial osteophyte; LFO = lateral femoral osteophyte; LTO = lateral tibial osteophyte; MJSN = medial joint space narrow; LJSN = lateral joint space narrow.
P values were calculated using a linear mixed model. Boldface indicates statistical significance.
Taken together, the radiographic changes that were more associated with pain were JSN on the medial side and osteophytes on the lateral side.
Discussion
This study investigated the structural characteristics of the knee that affect knee pain using data from a large-scale cohort, including participants with no or less severe radiographic changes and symptoms. The lateral-OA and medial & lateral-OA groups had more pain in movements than the medial-OA group. The lateral-OA group showed higher hsCRP levels than the medial-OA group. Moreover, multivariate analysis also showed that among the R-OA changes, medial JSN and lateral osteophytes significantly affected knee pain even after adjusting for age, sex, BMI, presence of depression, and muscle mass of the lower extremities.
We previously reported that a group of patients with coexisting lateral OA and medial OA presented considerably more pain than patients with only medial OA. 11 A similar tendency was observed in this much larger study that included participants with no or less pain and radiographic abnormalities: the JKOM score was higher in the medial & lateral-OA group than in the medial-OA group. In addition to this observation, this study showed that the lateral-OA group also presented worse symptoms than the normal and medial-OA groups. Furthermore, there was an apparent tendency for pain to be considerably present in different movements in the lateral-OA and medial & lateral-OA groups than in the medial-OA group: pain with ascending and descending stairs was significantly higher in the lateral-OA and medial & lateral-OA groups. Although previous studies focused only on participants with a K-L grade of 2, we were able to confirm a similar trend in participants of all K-L grades in this study.
The reasons why lateral changes are more associated with pain are unknown, although a previous study reported that synovial inflammatory cytokine levels were significantly higher in the bilateral OA group than in the unilateral OA group. 18 CRP is known to be associated with the extent and severity of knee OA and with markers of pain in knee OA.19-22 Indeed, this study confirmed that hsCRP levels tended to be significantly higher in the lateral-OA group than in the other groups, suggesting a difference in the clinicopathologic features of the lateral-OA group, which may contribute to different clinical outcomes. However, the results should be interpreted with caution because the reason for the higher hsCRP levels is unknown.
This study showed that knee pain increased as the structural grade worsened in all regions (medial and lateral osteophytes and JSN). Although there are various reports on the degree of knee pain and structural knee abnormality in knee OA patients, a study using 2 large cohorts that compared both knees in the same participants, which minimizes between-person confounding, reported that knee pain increased as the K-L grade worsened. 23 Our study provides additional evidence that structural abnormalities exacerbate knee pain. Furthermore, this study elucidated, for the first time, that JSN has more profound effects on the medial side and osteophytes considerably affect pain on the lateral side. The reasons for these results are not clear; however, a previous report showed that the influence on the cartilage volume is greater than that on medial osteophytes, indicating a strong association between medial JSN and lateral osteophytes. 24 With respect to the associations between pain and radiographic features, another study showed that participants with lateral tibial or femoral osteophytes showed a higher risk ratio of pain than those with osteophytes in the medial tibia or femur, 25 suggesting that lateral osteophytes may have a stronger influence on knee pain than medial osteophytes.
This study also assessed the effects of JSN and osteophytes on pain on both the medial and lateral sides ( Table 4 ). Lateral femoral osteophytes affected pain more than osteophytes on the medial side; however, no difference was found in tibial osteophytes, suggesting that femoral osteophytes have a more potent influence ( Table 4a ). In contrast, JSN had greater effects than both femoral and tibial osteophytes on the medial side ( Table 4b ). However, the mean difference was greater in medial JNS-MTO than in medial JNS-MFO, suggesting a more potent influence of osteophytes in the femur ( Table 4b ). To our knowledge, this difference in associations with pain of osteophytes has not been reported thus far, and the reasons remain to be investigated. However, radiographic osteophytes in the femur are more reliable than those in the tibia for assessing pain in the knee joint.
This study had several limitations. First, we analyzed participants aged ≥60 years from a single ethnic group. It would be necessary to analyze other groups including younger individuals and/or participants of other ethnicities to determine whether the same tendency would be confirmed in such populations. Second, we adopted the OARSI criteria, which are more precise than the K-L grades; however, the results may be different when using other criteria of knee OA, other radiographic grading, or other imaging modalities such as MRI. Although there are concerns on its limited accessibility in clinical practice, MRI can detect more precise changes in early stage and has advantage to capture earlier structural features of patients with knee pain. In addition, the patellofemoral compartment was not assessed by any modality in this study. Third, differences in the location and pattern of knee pain have been reported in other studies. However, our study was not able to confirm this information due to the study design and this should be kept in consideration. Fourth, the causal relationship between high hsCRP levels and pain remains to be investigated. Fifth, although we adjusted the multivariate analysis for age, sex, BMI, presence of depression, and muscle mass of the lower extremity, other factors such as genetic background, mechanical misalignment, degenerative changes of the articular cartilage, inflammation in tissues including synovia, and subchondral bone changes may affect the results. Sixth, participants were analyzed as symptomatic if there were any symptoms in the knee (JKOM ≥1) in this study. Although we were able to confirm the same result even if the definition of symptomatic was changed to JKOM ≥2 (data not shown), the pain threshold may be different in each participant. Finally, the cross-sectional design of this study precluded any conclusions about the causal relationship between group characteristics and clinical outcomes.
In conclusion, we identified the specific radiographic features of the knee that contribute to knee pain. Groups with lateral-side changes showed worse symptoms and higher hsCRP levels. In addition, medial JSN and lateral osteophytes had potent effects on knee pain.
Supplemental Material
Supplemental material, sj-docx-1-car-10.1177_19476035211025817 for Differential Contribution of the Medial and the Lateral Side of the Joint to Symptoms in Knee Osteoarthritis: A Radiographic and Laboratory Analysis in the Nagahama Study by Kazuya Nigoro, Hiromu Ito, Tomotoshi Kawata, Shinichiro Ishie, Yugo Morita, Kohei Nishitani, Tomoki Aoyama, Yasuharu Tabara, Fumihiko Matsuda, Shu Narumiya and Shuichi Matsuda in CARTILAGE
Supplemental material, sj-docx-2-car-10.1177_19476035211025817 for Differential Contribution of the Medial and the Lateral Side of the Joint to Symptoms in Knee Osteoarthritis: A Radiographic and Laboratory Analysis in the Nagahama Study by Kazuya Nigoro, Hiromu Ito, Tomotoshi Kawata, Shinichiro Ishie, Yugo Morita, Kohei Nishitani, Tomoki Aoyama, Yasuharu Tabara, Fumihiko Matsuda, Shu Narumiya and Shuichi Matsuda in CARTILAGE
Supplemental material, sj-docx-3-car-10.1177_19476035211025817 for Differential Contribution of the Medial and the Lateral Side of the Joint to Symptoms in Knee Osteoarthritis: A Radiographic and Laboratory Analysis in the Nagahama Study by Kazuya Nigoro, Hiromu Ito, Tomotoshi Kawata, Shinichiro Ishie, Yugo Morita, Kohei Nishitani, Tomoki Aoyama, Yasuharu Tabara, Fumihiko Matsuda, Shu Narumiya and Shuichi Matsuda in CARTILAGE
Footnotes
Author Contributions: HI, TA, YT, FM, and SM designed the study. KaN and HI wrote the manuscript. HI, KaN, YT, KoN, and FM collected data and information of the subjects. KaN, HI, TK, and SI analyzed radiography. KaN and YM performed the statistical analyses. HI, YT, FM, SN, and SM collected funding. SN, FM, and SM supervised the works. All authors read and approved the final manuscript.
Acknowledgment and Funding: We are grateful to Dr. Yoshihiko Kotoura for his tremendous help regarding clinical measurements, Nagahama City Office, and the Zeroji Club, a nonprofit organization, for their assistance in conducting this study. We thank Drs. T. Tsuboyama, T. Ikezoe, N. Ichihashi, and N. Taniguchi (Kyoto University Graduate School of Medicine) for their valuable technical assistance and thoughtful discussion. The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The Nagahama study was supported by a university grant; the Center of Innovation Program; the Global University Project; Grant-in-Aid for Scientific Research (25293141, 26670313, 26293198, 17H04182,17H04126, 18K18450, 17H04123) from the Ministry of Education, Culture, Sports, Science and Technology in Japan; the Practical Research Project for Rare/Intractable Diseases (ek0109070, ek0109070,ek0109196, ek0109348); the Comprehensive Research on Aging and Health Science Research Grants for Dementia R&D (dk0207006); the Program for an Integrated Database of Clinical and Genomic Information (kk0205008); the Practical Research Project for Life-Style related Diseases including Cardiovascular Diseases and Diabetes Mellitus (ek0210066, ek0210096), and the Research Program for Health Behavior Modification by Utilizing IoT (le0110005) from Japan Agency for Medical Research and Development; the Takeda Medical Research Foundation; the Mitsubishi Foundation; the Daiwa Securities Health Foundation, and the Sumitomo Foundation.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: KaN is an employee of Mitsubishi-Tanabe Pharma. HI belongs to the department that is financially supported by Nagahama City, Toyooka City, and five pharmaceutical companies (Mitsubishi-Tanabe, Chugai, UCB Japan, Ayumi, and Asahi-Kasei) and has received a research grant and/or speaker fee from Bristol-Myers Squibb and Asahi-Kasei. SM has received a research grant and/or speaker fee from Kyocera, Zimmer-Biomet, and Smith & Nephew. TK, KoN, YT, FM, and SN declared no conflicts of interest. The sponsors were not involved in the study design; in the collection, analysis, interpretation of data; in the writing of this manuscript; or in the decision to submit the article for publication. The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Ethical Approval: This study was conducted in accordance with the principles of the Declaration of Helsinki and was approved by the ethics committee of Kyoto University Graduate School of Medicine and by the Nagahama Municipal Review Board (No. C278).
Informed Consent: Written informed consent was obtained from all participants.
ORCID iDs: Hiromu Ito  https://orcid.org/0000-0002-1827-382X
https://orcid.org/0000-0002-1827-382X
Kohei Nishitani  https://orcid.org/0000-0002-8327-3826
https://orcid.org/0000-0002-8327-3826
References
- 1. Hunter DJ, Bierma-Zeinstra S. Osteoarthritis. Lancet. 2019;393:1745-59. [DOI] [PubMed] [Google Scholar]
- 2. Eckstein F, Wirth W, Culvenor AG. Osteoarthritis year in review 2020: imaging. Osteoarthritis Cartilage. 2021;29(2):170-9. [DOI] [PubMed] [Google Scholar]
- 3. Kijowski R, Demehri S, Roemer F, Guermazi A. Osteoarthritis year in review 2019: imaging. Osteoarthritis Cartilage. 2020;28(3):285-95. [DOI] [PubMed] [Google Scholar]
- 4. Leyland KM, Gates LS, Nevitt M, Felson D, Bierma-Zeinstra SM, Conaghan PG, et al. Harmonising measures of knee and hip osteoarthritis in population-based cohort studies: an international study. Osteoarthritis Cartilage. 2018;26(7):872-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Culvenor AG, Engen CN, Øiestad BE, Engebretsen L, Risberg MA. Defining the presence of radiographic knee osteoarthritis: a comparison between the Kellgren and Lawrence system and OARSI atlas criteria. Knee Surg Sport Traumatol Arthrosc. 2015;23(12):3532-9. [DOI] [PubMed] [Google Scholar]
- 6. Bedson J, Croft PR. The discordance between clinical and radiographic knee osteoarthritis: a systematic search and summary of the literature. BMC Musculoskelet Disord. 2008;9:116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Nigoro K, Ito H, Kawata T, Nishitani K, Tabara Y, Matsuda F, et al. Obesity with radiological changes or depression was associated with worse knee outcome in general population: a cluster analysis in the Nagahama study. Arthritis Res Ther. 2020;22(1_suppl):280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494-502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Altman RD, Gold GE. Atlas of individual radiographic features in osteoarthritis, revised. Osteoarthritis Cartilage. 2007;15(Suppl A):A1-A56. [DOI] [PubMed] [Google Scholar]
- 10. Altman RD, Hochberg M, Murphy WA, Jr, Wolfe F, Lequesne M. Atlas of individual radiographic features in osteoarthritis. Osteoarthritis Cartilage. 1995;3(Suppl A):3-70. [PubMed] [Google Scholar]
- 11. Iijima H, Aoyama T, Nishitani K, Ito H, Fukutani N, Isho T, et al. Coexisting lateral tibiofemoral osteoarthritis is associated with worse knee pain in patients with mild medial osteoarthritis. Osteoarthritis Cartilage. 2017;25(8):1274-81. [DOI] [PubMed] [Google Scholar]
- 12. Matsumoto T, Tabara Y, Murase K, Setoh K, Kawaguchi T, Nagashima S, et al. Nocturia and increase in nocturnal blood pressure: the Nagahama study. J Hypertens. 2018;36:2185-92. [DOI] [PubMed] [Google Scholar]
- 13. Englund M, Roos EM, Lohmander LS. Impact of type of meniscal tear on radiographic and symptomatic knee osteoarthritis: a sixteen-year follow-up of meniscectomy with matched controls. Arthritis Rheum. 2003;48(8):2178-87. [DOI] [PubMed] [Google Scholar]
- 14. Lohmander LS, Östenberg A, Englund M, Roos H. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum. 2004;50(10):3145-52. doi: 10.1002/art.20589 [DOI] [PubMed] [Google Scholar]
- 15. Landis JR, Koch GG. An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers. Biometrics. 1977;33:363-74. [PubMed] [Google Scholar]
- 16. Akai M, Doi T, Fujino K, Iwaya T, Kurosawa H, Nasu T. An outcome measure for Japanese people with knee osteoarthritis. J Rheumatol. 2005;32:1524-32. [PubMed] [Google Scholar]
- 17. Ito H, Tominari S, Tabara Y, Nakayama T, Furu M, Kawata T, et al.; Nagahama Study Group. Low back pain precedes the development of new knee pain in the elderly population; a novel predictive score from a longitudinal cohort study. Arthritis Res Ther. 2019;21(1_suppl):98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Moradi B, Rosshirt N, Tripel E, Kirsch J, Barié A, Zeifang F, et al. Unicompartmental and bicompartmental knee osteoarthritis show different patterns of mononuclear cell infiltration and cytokine release in the affected joints. Clin Exp Immunol. 2015;180(1_suppl):143-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Stannus OP, Jones G, Blizzard L, Cicuttini FM, Ding C. Associations between serum levels of inflammatory markers and change in knee pain over 5 years in older adults: a prospective cohort study. Ann Rheum Dis. 2013;72(4):535-40. [DOI] [PubMed] [Google Scholar]
- 20. Zhang J. Meta-analysis of serum C-reactive protein and cartilage oligomeric matrix protein levels as biomarkers for clinical knee osteoarthritis. BMC Musculoskelet Disord. 2018;19(1_suppl):22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Otterness IG, Weiner E, Swindell AC, Zimmerer RO, Ionescu M, Poole AR. An analysis of 14 molecular markers for monitoring osteoarthritis. Relationship of the markers to clinical end-points. Osteoarthritis Cartilage. 2001;9(3):224-31. [DOI] [PubMed] [Google Scholar]
- 22. Pearle AD, Scanzello CR, George S, Mandl LA, DiCarlo EF, Peterson M, et al. Elevated high-sensitivity C-reactive protein levels are associated with local inflammatory findings in patients with osteoarthritis. Osteoarthritis Cartilage. 2007;15(5):516-23. [DOI] [PubMed] [Google Scholar]
- 23. Neogi T, Felson D, Niu J, Nevitt M, Lewis CE, Aliabadi P, et al. Association between radiographic features of knee osteoarthritis and pain: results from two cohort studies. BMJ. 2009;339(7719):498-501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Zhu Z, Laslett LL, Han W, Antony B, Pan F, Cicuttini F, et al. Associations between MRI-detected early osteophytes and knee structure in older adults: a population-based cohort study. Osteoarthritis Cartilage. 2017;25(12):2055-62. [DOI] [PubMed] [Google Scholar]
- 25. Kaukinen P, Podlipská J, Guermazi A, Niinimäki J, Lehenkari P, Roemer FW, et al. Associations between MRI-defined structural pathology and generalized and localized knee pain—the Oulu Knee Osteoarthritis study. Osteoarthritis Cartilage. 2016;24(9):1565-76. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-car-10.1177_19476035211025817 for Differential Contribution of the Medial and the Lateral Side of the Joint to Symptoms in Knee Osteoarthritis: A Radiographic and Laboratory Analysis in the Nagahama Study by Kazuya Nigoro, Hiromu Ito, Tomotoshi Kawata, Shinichiro Ishie, Yugo Morita, Kohei Nishitani, Tomoki Aoyama, Yasuharu Tabara, Fumihiko Matsuda, Shu Narumiya and Shuichi Matsuda in CARTILAGE
Supplemental material, sj-docx-2-car-10.1177_19476035211025817 for Differential Contribution of the Medial and the Lateral Side of the Joint to Symptoms in Knee Osteoarthritis: A Radiographic and Laboratory Analysis in the Nagahama Study by Kazuya Nigoro, Hiromu Ito, Tomotoshi Kawata, Shinichiro Ishie, Yugo Morita, Kohei Nishitani, Tomoki Aoyama, Yasuharu Tabara, Fumihiko Matsuda, Shu Narumiya and Shuichi Matsuda in CARTILAGE
Supplemental material, sj-docx-3-car-10.1177_19476035211025817 for Differential Contribution of the Medial and the Lateral Side of the Joint to Symptoms in Knee Osteoarthritis: A Radiographic and Laboratory Analysis in the Nagahama Study by Kazuya Nigoro, Hiromu Ito, Tomotoshi Kawata, Shinichiro Ishie, Yugo Morita, Kohei Nishitani, Tomoki Aoyama, Yasuharu Tabara, Fumihiko Matsuda, Shu Narumiya and Shuichi Matsuda in CARTILAGE