Abstract
Objective:
Focal cartilage injuries, and posttraumatic osteoarthritis (OA) in the wrist are likely common and a cause of wrist pain. To estimate the incidence of cartilage lesions and to understand the pathomechanisms leading to wrist cartilage injuries and OA, a literature review on the subject was performed combined with a presentation of one of the authors’ own experience.
Design:
This study includes a literature review of the topic. As a comparison to the review findings, the observations of one of the authors’ consecutive 48 wrist arthroscopies, were assessed. PubMed, Scholar, and Cochrane databases were searched using the keywords “cartilage injury AND wrist AND treatment” and “wrist AND cartilage AND chondral AND osteochondral AND degenerative OA.”
:Result
A total of 11 articles, including 9 concerning chondral and osteochondral repair and treatment and 2 regarding posttraumatic OA, were retrieved. The cartilage repair treatments used in these articles were drilling, osteochondral autograft, juvenile articular cartilage allograft, and chondrocyte implantation. One article displayed concomitant cartilage injuries in displaced distal radius fractures in 32% of the patients. The review of our findings from a 1-year cohort of wrist arthroscopies showed 17% cartilage injuries.
Conclusion:
There is a lack of knowledge in current literature on cartilage injuries and treatment, as well as posttraumatic OA in the wrist. Cartilage injuries appear to be common, being found in 17% to 32% of all wrist arthroscopies after trauma, but no guidelines regarding conservative or surgical treatment can be recommended at the moment. Larger prospective comparative studies are needed.
Keywords: wrist, cartilage repair, chondral injury, degenerative arthritis wrist, arthroscopy
Introduction
Focal chondral and osteochondral injuries in the wrist are likely common and a cause of wrist pain. 1 Those injuries could be divided into 3 groups related to injuries of ligaments, fractures, and the vascular supply.
Ligament Injuries
The wrist joint connects the ends of the radius and ulna with 8 carpal bones (the scaphoid, lunate, triquetrum, pisiform, trapezium, trapezoid, capitate, and hamate), which are stabilized by 24 ligaments ( Fig. 1 ). 2 Subsequently, chondral and osteochondral injuries and secondary development of osteoarthritis (OA) are often concomitant with ligament injuries, such as:
Figure 1.

The bones and joints of the wrist. Numerals 1 to 5 display the most common described locations of chondral injuries in the wrist (S = Scaphoid, L = Lunate, Tq = Triquete, P = Pisiforme, Tm = Trapezium, Td = Trapezoid, C = Capitate, H = Hamate).
Scapholunate ligament injuries (SL)—leading to development to an advanced scapholunate collapse (SLAC) and a gradually increasing development of OA. 3
Lunotriqeutral injuries (LT) and the associated chondral injury; hamate arthrosis lunotriquetral ligament tear (HALT).4,5
Injuries to the triangular fibrocartilage complex (TFCC), Palmer Type 1. 6
Degenerative TFCC lesions (Palmer class 2) all involve the central portion and are staged from A to E, depending on the presence or absence of a TFCC perforation, lunate and ulnar chondromalacia, lunotriquetral ligament perforation, or degenerative radiocarpal arthritis. Besides in connection with ligament injuries, those lesions could more be seen in connection with fractures such as in secondary ulnar impaction,7,8 with chondral injury at the head of the ulna and the opposing surface of the lunate ( Fig. 2 ).
Figure 2.

The gradual development of OA in ulnar impaction. The cause is an ulnar positive variance (ulna longer than radius) giving increased load of the ulnar aspects of the wrist, beginning with a chondral lesion at the ulnar-proximal part of the lunate and the radial ulnar proximal part of the hamate (HALT), as well as a central part of the triangular fibrocartilage complex (TFCC), followed by chondral impact at the ulnar head, finally ending up with degenerative OA in the distal radio-ulnar joint (DRUJ).
Fractures
Posttraumatic chondral lesions after carpal bone fractures
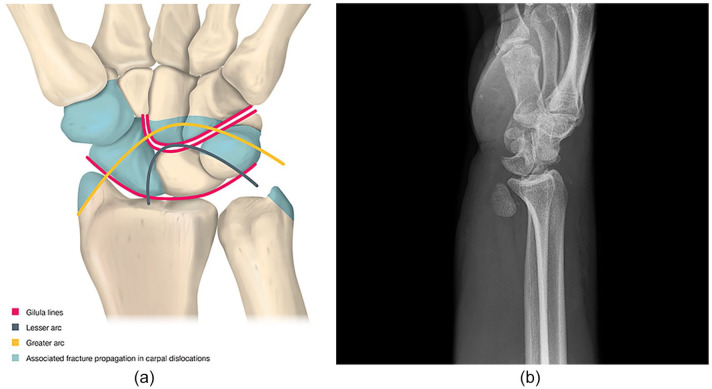
Fractures of the radial styloid, the scaphoid, the trapezium, the capitate, and the triquetrum could all be associated with dorsal or volar perilunate dislocations and subsequent cartilage damage ( Fig. 3a and b )
Gradually increasing development of OA is seen after nontreated scaphoid fractures with nonunion (SNAC)
Figure 3.
(a) Schematic presentation of typical patterns of perilunate dislocations and transscaphoid perilunate fracture dislocations. Normal Gilula’s lines are also displayed. (b) Perilunar dislocation X-ray, AP view could almost be normal. The diagnosis is obvious in the lateral view.
A majority of those carpal fractures involves the scaphoid bone. 9
Vascular Cause
Injuries to the vascular supply of the carpal bones may result in osteonecrosis and collapse of the cartilage surface with subsequent OA development. The causes of the vascular disruptions could be multifactorial but a massive single impact or repeated micro-trauma could be causative in conditions such as
Preiser’s disease (avascular necrosis of the scaphoid bone). Mainly of unknown origin but injuries to the nutrient artery through trauma could lead to ischemia throughout the scaphoid with bone collapse and OA development. 10
Kienböcks disease (avascular necrosis of the lunate bone). Disruption of the vascular supply induces osteonecrosis and overlying collapse of cartilage layer developing into OA. Trauma involvement is common. 11
To what extent the various ligament injuries with concomitant cartilage injuries and solitary cartilage injuries progress into OA is not known ( Figs. 4 and 5 ). There is still no evidence that different wrist injury treatments will alter such a development. Furthermore, there is still no consensus in terms of the treatment of cartilage injuries in the wrist. While microfracturing and methods of cartilage repair and transplantation have been described and used in the clinical setting at hand surgery departments, the treatments have only been presented by other authors in a limited number of patients, as case reports or at scientific meetings.12,13
Figure 4.

Scapholunate advanced collapse after an SL injury, with subsequent arthritic changes at the RC and MC joints (SLAC III).
Figure 5.

The use of intraarticular contrast fluid and cone-beam computer tomography (CBCT) can reveal even small cartilage injuries. The arrow shows the cartilage injury proximal at the scaphoid. Contrast is seen in the SL and LT spaces caused by SLAC.
This is a review of the reported existence of cartilage lesions and posttraumatic OA found in the wrist after trauma in combination with one of the authors’ (JKA) cartilage lesion findings in 48 wrist arthroscopies, performed during 1 year, evaluated in 2019.
The purpose of the study was to analyze the current treatment options of cartilage injuries in the wrist and the current knowledge found in the literature in this field of interest. The aims were to find out how common these injuries are and if any specific treatment is superior to others, as well as assessing the possible gradually development to posttraumatic OA.
Methods
Literature Search Strategies: Cartilage Injuries and Posttraumatic Degenerative OA
A systematic review according to PRISMA 14 was not possible, due to the limited number of articles, with only level of evidence (LoE) IV-V and heterogeneous follow-up assessments.
The broad search strategy “cartilage injury AND wrist” in PubMed, Scholar, and Cochrane’s databases was performed on February 2, 2021, and revealed 906 articles. More directed and focused search strategies (“cartilage injury AND wrist AND treatment” and “wrist AND cartilage AND chondral AND osteochondral AND degenerative OA”) were performed the same day. “Chondral AND injury hand wrist” revealed 23 articles, “cartilage injury AND wrist AND treatment” 26 articles, and “osteochondral injuries AND hand wrist” 78 articles.
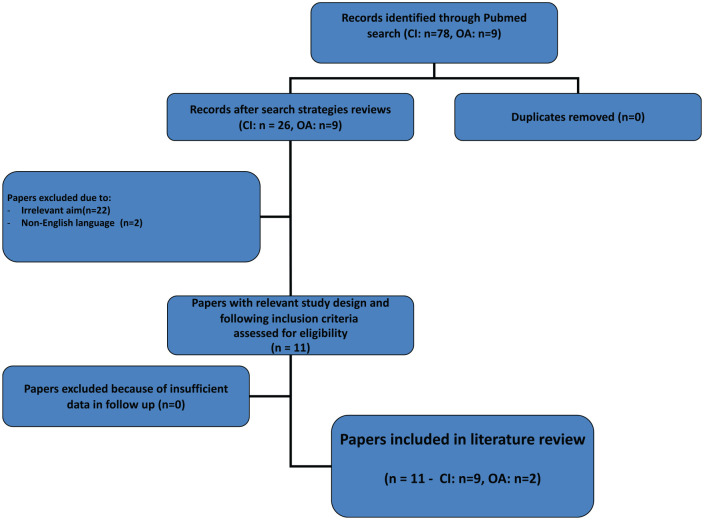
Among those 78 hits, articles with irrelevant topic for this article were excluded (n = 52), leaving a total of 26 articles for primary inclusion. After exclusion of all reviews, any duplicates, and non-English studies, 9 articles could finally be included in terms of cartilage injuries.
Data extraction included categorizing the articles in the diagnostics and frequency of chondral and osteochondral injuries and a description of different methods of treating these injuries in the wrist. The search strategies in Scholar and Cochrane did not add any articles compared with PubMed, but only duplicates.
Thus, 26 (n = 9 after excluding the others because of irrelevant aim) related to chondral repair and treatment in the wrist were found. This should be compared with 9,670 articles found dealing with chondral and osteochondral injuries in the knee where, among those, the majority were of significant relevance. Level of evidence (LoE), according to Sackett, 15 of the articles was also analyzed.
In terms of posttraumatic OA the following search strategies were used:
Wrist AND cartilage AND chondral AND osteochondral AND OA AND degenerative AND repair AND subchondral (n = 0)
Wrist AND cartilage AND chondral AND osteochondral AND degenerative OA (n = 15, but all excluded due to irrelevant aim)
Wrist AND cartilage AND chondral AND osteochondral AND post traumatic arthritis (n = 0)
Wrist AND cartilage AND chondral AND osteochondral AND OA (n = 9, but all irrelevant aim)
Wrist AND cartilage AND chondral AND osteochondral AND osteoarthrosis (n = 3, 1 excluded because of irrelevant aim, included: n = 2)13,16
Wrist AND cartilage AND chondral AND osteochondral AND degenerative OA/osteoarthrosis (n = 0)
Wrist AND degenerative arthritis (n = 1825, after exclusion, n = 1, that also describes the treatment). 16 Rheumatoid arthritis was the main subjects in these found articles.
Wrist AND degenerative OA (n = 258, n = 9 after exclusion for irrelevant topic, after exclusion for irrelevant topic; n = 2).12,16 Thus, only 2 articles were included in terms of wrist and OA. Articles of salvage procedures in wrist OA 17 was also discussed in the Discussion section.
Articles about nontraumatic midcarpal instability (carpal instability non-dissociative, CIND) as a cause of OA, as well as cartilage injuries and degenerative arthritis in the basal thumb and the scaphotrapeziotrapezoidal joint were excluded as the focus of this review was on pure wrist trauma.
The search strategies are displayed in Figure 6 .
Figure 6.
Search strategies (CI = cartilage injuries, OA = osteoarthrosis).
Wrist Arthroscopies
An assessment of a single surgeon’s experience of 48 arthroscopies (JKA), performed during 1 year—assessed in 2019—in terms of the incidence of diagnosed chondral and osteochondral injuries was performed. The results of this review and assessment serve as indicator of a possible comparison with former published papers in this area of interest.
Ethics and Statistics
Ethical approval was performed by the University of Gothenburg, in terms of the review of the author’s performed wrist arthroscopies (Dnr: 977-1). Informed consent was approved by all participants.
Data are presented as numeric values and no statistical analysis was used.
Results
Literature Review
The search strategies “cartilage injury AND wrist” in PubMed, Scholar, and Cochrane databases revealed 906 articles, and the search strategies “cartilage injury AND wrist AND treatment” displayed 26 articles.
The treatments used in these articles were arthroscopic drilling, osteochondral autograft (13), and/or juvenile articular cartilage allograft (12).
Only LoE IV-V articles were found.
Diagnosis and Evaluation
The bones and joints of the wrist are shown in Figure 1 , as well as the most commonly described localizations of chondral and osteochondral injuries.
Lesion Classification
To better describe the appearance of wrist cartilage injuries, Culp et al. 18 have provided a modified Outerbridge classification, 19 with Grade I representing softening of the hyaline surface, Grade II consisting of fibrillation and fissuring, Grade III representing a fibrillated lesion of varying depth in the articular surface, and Grade IV having a full-thickness defect down to bone. Culp et al. suggested that Grades I to III lesions are treated with debridement and synovectomy. Grade IV lesions can be treated with abrasion chondroplasty and subchondral drilling. The International Cartilage Regeneration and Joint Preservation Society (ICRS) classification has never been used in research on the wrist, but as it describes the depth of cartilage lesions one may consider use of this classification as well. 20
Wrist Imaging
In order to adequately diagnose lesions that appear after trauma, imaging is of great importance. Magnetic resonance imaging (MRI) is not reliable enough to disclose wrist ligament injuries and cartilage injuries. 21 The use of intraarticular contrast fluid and cone-beam computer tomography (CBCT) can reveal even small cartilage injuries and is a promising new diagnostic tool in these cases ( Fig. 5 ). CBCT arthrograms 22 have been shown to have a slightly higher specificity than magnetic resonance arthrography. The sensitivity of CBCT arthrography is also better for cartilage lesions, except for those on the chondral surface of the lunate, according to Suojärvi et al. 23 Suojärvi et al. showed that 10/21 patients with wrist pain had cartilage injuries (47, 6%), indicating that cartilage injuries may be far more prevalent than previously documented.
On regular radiographs, minor triquetral or ulnar-sided lunate sclerosis or cyst formation may be signs of ulnocarpal wear. Few studies have been conducted to investigate the use of MRI for diagnosing the etiology of wrist pain. MRI has not been shown to be sufficient enough to disclose ligament or cartilage injuries, 21 as the sensitivity, specificity, positive predicted value, and negative predicted value are too low. In cases of rheumatoid arthritis affecting the wrist joint, MRI has revealed that cartilage damage progression is preceded by osteitis and synovitis, but is most influenced by preexisting cartilage damage suggesting primacy of the cartilage damage pathway in certain patients. 24 No other studies were found in our search strategies in terms of comparison between the different imaging methods to diagnose solitary cartilage injuries.
The use of intraarticular contrast fluid and CBCT can reveal even small cartilage injuries ( Fig. 5 ) and have higher accuracy than MRI in terms of chondral injuries in the wrist.21,22
Anatomical Variations
There are 2 types of the carpal bone lunate. 25 In type II lunate a facet exists on the medial side of the lunate to be in articulation with the proximal pole of the hamate. Type I lunate lacks such a facet. Type II lunates have different biomechanical behaviors with a higher risk of developing degenerative changes in the hamato-lunate joint causing ulnar-sided wrist pain.
The scaphoid is the most prominent bone of the carpal bones and its motion pattern in relation to other carpal bones is important to know about when to understand injury mechanisms. Variations in scaphoid motion secondary to lunate morphology may contribute to the development of STT OA (scaphoid-trapezium-trapezoid arthritis). 26
Diagnostic Studies: Cartilage Injuries
Cartilage Injuries in Relation to Distal Radius Fractures
Focal chondral and osteochondral injuries following intraarticular distal radius fractures are common. 1 Cottias et al. 27 described in 1997 that intraarticular distal radial fractures with a step of more than 2 mm are prone to lead to focal cartilage lesion and subsequently development of OA. They also concluded that focal cartilage lesions are probably a common cause of chronic wrist pain.
The incidence of associated cartilage and ligament lesions in distal radial fractures in young adults were evaluated arthroscopically by Lindau et al. 1 Fifty initially displaced fractures were evaluated. Cartilage lesions were found in 16 patients (32%). The authors concluded that cartilage lesions were rather common and may explain poor outcomes after well-healed distal radial fractures. Subchondral hematomas—without any significant focal cartilage injury—in distal radial fractures does not lead to the early onset of OA. However, an inferior outcome 1 year after surgery, compared with patients without fractures, was seen, according to Mrkonjic et al. 28
Forty-two patients who underwent open reduction and internal fixation of distal radial fractures were arthroscopically evaluated for SL and TFCC injuries with or without chondral surface damages in a study by Swart and Tang. 29 Forty-five percent of the patients had SL injuries, 50% had TFCC injuries, and 29% had articular cartilage injuries.
Tarabin et al. 30 showed that posttraumatic radiocarpal articular cartilage damage did not differ between fractures with intraarticular and extra-articular extensions, but patients with fractures had notably higher risk of articular cartilage degradation compared with healthy controls.
Cartilage Injuries and Carpal Bone Fractures
Scaphoid bone
Caloia et al. 31 found that 15 of 24 patients with acute scaphoid fractures had associated ligamentous and/or chondral/osteochondral injuries. They concluded that fluoroscopy during the placement of a compression screw may decrease the rate of subchondral penetration, that may happen in as much as approximately 20% of the patients. 31
Scaphoid impaction injuries occur in sports involving a forced and repetitive hyperextension of the wrist, where the dorsal lip of the radius is forced into contact with the proximal/dorsal articular surfaces of the scaphoid. These injuries are primarily seen in weightlifters and gymnasts. If conservative treatment fails, a dorsal scaphoid ridge or dorsal radial lip cheilectomy has most often been performed. If the procedure is unsuccessful in relieving pain, a coexisting cartilage defect may be the source of pain.32,33
Midcarpal bones
Dautel and Merle 34 showed that chondral defects and/or arthritic lesions of the ulnar portion of the midcarpal joints were observed more often in wrists with type II lunates (2 joint facets articulating with the capitate and hamate). Cartilage lesions of the midcarpal joints in type I lunates (1 joint facet) were always associated with other ligamentous and/or osteochondral lesions, whereas the same lesions could be found isolated in type II lunates. The observed association of lesions appeared to point to a specific trauma and specific anatomical variations as causes of some cartilage lesions. However, Viegas 35 showed no pathologic conditions of the hamate bone (HALT) in type I lunates.
Iatrogenic cartilage injuries
Iatrogenic cartilage penetration injuries especially after compression screw fixation of scaphoid fracture and nonunion have also been described. 36
Posttraumatic Osteoarthritis
Wrist OA is usually secondary to posttraumatic events and most often develops in the joints that involve the scaphoid. 3
Several general causes of wrist OA are listed below:
• Senescence
• Gender—women are more likely to develop OA 37
• Obesity
• Previous wrist injuries
• Kienböck’s disease 40
• Preiser’s disease 41
• Rheumatoid arthritis
• Postinfectious arthritis
The search strategies in PubMed in terms of OA displayed 2 articles, apart from the duplicates found in the search strategies regarding wrist cartilage/chondral injuries. No conclusion could be stated in terms of the incidence of secondary development of posttraumatic OA, after solitary primary cartilage injuries.
Laulan et al. 16 published a review (LoE V) in 2015 describing the different types of OA in the wrist, mainly after ligament injuries and scaphoid nonunion, ending up in SLAC and SNAC wrist, and the proper treatment options available. There are, however, several articles describing more specific ligament injuries and subsequent OA development and treatments. Weiss and Rodner point out that chronic scapholunate tears are known to produce intercarpal instability with an altered kinematics and joint loading, and subsequent development of joint degeneration of the radiocarpal joint. 42
Weiss and Rodner also pointed out common causes of wrist post-traumatic OA:
Scapho-lunate advanced collapse (SLAC)
Scaphoid fracture nonunion collapse (SNAC)
OA secondary to an intraarticular fracture of the distal radius or ulna, or from an extra-articular fracture resulting in malunion and abnormal joint loading
However, Weiss and Rodner did no not describe any percentages of trauma types involved in the development of wrist OA. 42
Repetitive use of the wrist has been discussed as a risk factor for OA development and may be seen as microtrauma of the joint. However, strong and moderate evidence exists for no increased risk of hand and wrist OA related to highly repetitive tasks. 43
The possible development of OA after solitary cartilage injuries is not proven in studies, apart from in intraarticular distal radius fractures and iatrogenic cartilage penetration injuries after compression screw fixation of scaphoid fractures and nonunions. 36
To summarize, osteoarthritis in the wrist is most commonly a result of untreated SL injuries and scaphoid nonunions, 3 where the injuries lead to carpal instability (carpal instability dissociative, CID), carpal collapse, and finally scapholunate advanced collapse (SLAC) or scaphoid nonunion advanced collapse (SNAC) wrist ( Fig. 4 ).
Regarding frequency, high-energy injuries, in particular perilunate and transscaphoid perilunate fracture dislocations ( Fig. 3a and b ), are associated with a mean incidence of posttraumatic osteoarthritis of almost 40% (range, 7% to 92%).44,45 Signs of posttraumatic OA after perilunate dislocations and trans-scaphoid perilunate fracture dislocations increase progressively, but some patients have minor symptoms at follow-up after more than 10 years.44,45 However, approximately 30% of these patients are not able to return to heavy manual work.44,45
Treatment of Local Cartilage Defects and OA
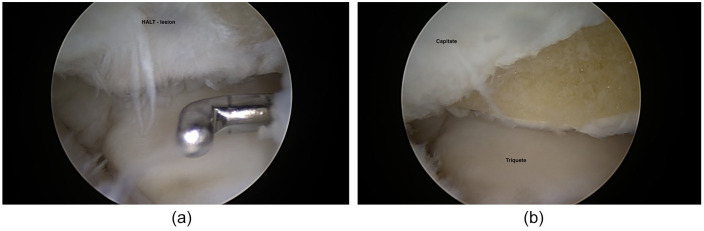
Figures 7 to 9 display common arthroscopic treatment options of wrist cartilage injuries.
Figure 7.
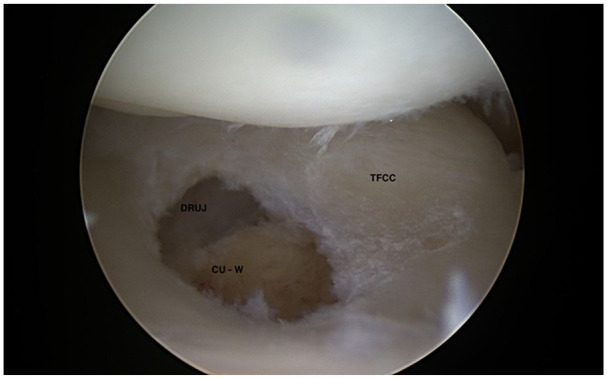
Arthroscopic Wafer osteotomy in ulnar impaction (CU-W = Caput ulna after Wafer osteotomy).
Figures 9.
HALT lesion at proximal-radial part on hamate (a), treated by shaving and abrasion (b).
Chondroplasty
The use of radiofrequency (RF) to smooth fibrillated wrist cartilage surfaces have been reported, most of them concerning the knee joint. In a recent study, Huber et al. 46 examined the thermal risks using RF for the wrist and found that the RF bipolar device could be applied if used with caution since peak temperature in the lunate fossa almost reached 70°C even under continuous irrigation.
Bone Marrow Stimulations
No articles about microfracturing of wrist chondral injuries could be found in PubMed, Scholar, or Cochrane, although this surgical technique, according to our knowledge, is used in hand surgery clinics. However, as another bone marrow stimulation technique, Whipple recommended arthroscopic drilling for small chondral defects of 5 mm or less. 47
Juvenile Articular Allografts
Juvenile articular cartilage allografts have been used for treatment of Outerbridge IV 19 injuries in the knee, ankle, and elbow joints with good outcome.48-54 In 2017, a case report showed good result and return to sports with this type of treatment in a wrist osteochondral injury in one patient. 12 Particulated juvenile articular cartilage (PJAC) allograft has been used to treat Outerbridge Grade IV chondral lesions on the proximal pole of a scaphoid and distal radius scaphoid facet in a patient who had failed conservative management. 12
Autologous Osteochondral Graft
Arthroscopic transplantation of osteochondral autograft from the lateral femoral condyle to distal radius with satisfactory outcome in 4 consecutive patients was reported by Ho et al. 13 In all cases, graft incorporation was complete within 3 to 4 months. All patients showed improvement in wrist function with no pain at follow-up (average of 70.5 month follow-up). Second-look arthroscopy in 3 patients confirmed the preservation of macroscopic normal articular cartilage. 13 Osteochondral allografts have also been used to treat local cartilage defects of lunate bone. Gaspar et al. reported on 2 patients treated by such treatment with good results up to 6 years. 55
Lee et al. reported on one patient treated by osteochondral autograft due to osteochondritis dissecans (OCD) in the scaphoid bone. OCD may have traumatic origin. 56
Chondrocostal Autografts
Chondrocostal grafts have been used and harvested from the ribs, inserted and fixed with plates in place of the articular defect in cases of a malunited intraarticular distal radius fracture (7 cases) or to replace the proximal pole of the scaphoid in cases of SNAC or SLAC (18 cases). In Kienböck’s disease, reports exist of the use of this graft as a free cartilage spacer (4 cases).57,58
Autologous Chondrocyte Implantations
Autologous chondrocyte implantation is used for failed local cartilage repairs and for large cartilage defects. There is only one case report on successful use of chondrocyte transplantation for the wrist, but no specific results in terms of functional scores, pain, or range of motion were reported in this single case. 59
Bone Resections, Bone Fusions, and Osteotomies
Many techniques exist, but only the most common techniques are described. The HALT chondral injuries (impingement between hamate and lunate) and OA are in 90% of the cases found with concomitant lunotriquetral (LT) ligament injuries. A recommended choice of treatment here is described to be arthroscopic resection of the proximal radial pole of the hamate4,5 ( Fig. 9a and b ). Degenerative TFCC injuries and ulnar impaction syndrome (impingement between caput ulna and carpus)—see Figure 2 —are often treated by arthroscopic central TFCC resection and Wafer osteotomy ( Fig. 7 ) or in severe cases—with concomitant ulnar positive variance of more than 3 to 4 mm (so-called ulnar impaction)—with open ulnar osteotomy.7,8 Ulnar styloid impaction syndrome also exists, with a big ulnar styloid causing conflict, impaction between the tip of the styloid and carpus with focal cartilage injuries at the lunate and triquete.
In SLAC and SNAC I, a radial styloidectomy may relieve the pain and postpone further need for surgery. In SLAC and SNAC II, the most used options are proximal row carpectomy (PRC) or 4-corner fusion (4CF). In the short term, these 2 operations produce similar results with pain relief and an ROM (range of motion) of flexion 30° to 40°, extension 30° to 40°, and 75% maintained grip force.60-62
In SLAC and SNAC III (midcarpal arthritis), the only alternative is 4CF or perhaps PRC plus resurfacing of the proximal part of the capitate with RCPI (resurfacing capitate pyrocarbon implant). However, the RCPI implant technique is currently not widely used in the daily clinical routine. 63
In older patients, with a low ROM preoperatively and a round and blunt-shaped capitate, PRC can be recommended. In patients younger than 35 years or with a pointed, peaked and narrow capitate, 4CF can be recommended. Some skepticism is, however, in order in terms of the long-term viability of a joint with a completely mismatched articular surface between the capitate and the lunate fossa of the radius. Long-term radio-capitate degeneration after more than 10 years of follow-up is seen; however, often asymptomatic and generally only present in about 10% to 20% of patients after PRC. 64
However, several other studies have reported a significantly larger number of patients with secondary arthritic changes after PRC, although most are symptom free. 65
There is a lack of well-conducted studies, but Mulford et al. 60 reported and confirmed in a systematic review that both 4CF and PRC produce a clear improvement in pain and subjective outcome measurements for patients with symptomatic SLAC wrists. PRC can perhaps provide a better postoperative ROM, with less risk of the potential complications specific to 4CF (10% more complications occurring; such as nonunion, hardware problems, and dorsal impingement). This systematic review reported that the risk of subsequent OA, albeit most often asymptomatic, is significantly higher after PRC. Subjective outcomes and quality of life, pain relief, motion, and grip strength appear to be similar in both groups.
Radioscapholunate (RSL) fusion could be an alternative in radiocarpal OA after distal radius fracture if the scaphoid and lunate fossae are affected and the midcarpal joint still is intact. Furthermore, when there is complex fragmentation of the articular surface of the distal radius, a silicon foil sheet could be used implanted into the radiocarpal joint to induce a substitute chondral tissue. 66
With a bone collapse as seen in Kienböck’s and Preiser’s diseases, the cartilage surface is destroyed, and OA has developed. Treatment alternatives are proximal row carpectomy, total wrist arthrodesis, scapho-trapezio-trapezoid arthrodesis, excisional arthroplasty, vascularized bone grafting (VBG), radial shortening osteotomy, radial corrective osteotomy, capitate shortening osteotomy combined with or without VBG, and tendon ball arthroplasty.41,67
Wrist Denervation
Wrist denervation is regarded to be a safe procedure for the treatment of chronic wrist pain due to OA or ligament instability. 68
Recently, partial wrist denervation has become popular as a procedure to alleviate chronic pain. However, in a recent review, the authors found improvement in short-term pain relief and functional status but a high re-operation rate. It must be stated, however, that denervation is a treatment of a symptom (pain) and not of the actual cause of pain. Denervation should therefore be used with caution in patients where the root cause of wrist pain is not known, and only after performing adequate preoperative nerve blocks to evaluate the effect of denervation surgery.69-71
Total Wrist Fusions and Arthroplasties
Total wrist fusion 72 historically provides predictable pain relief at the cost of a complete loss of motion and shock absorption. The complication rate in total wrist fusion is up to 6%, according to a recent published systematic review. 73
Total wrist fusion is an option in SLAC and SNAC IV, but total wrist replacement is now also an option, as the survival rate of the new generation of arthroplasties has increased markedly.17,72,73
Retrospective Review of Recorded Wrist Arthroscopies
Due to the disappointment with a low number of reports of cartilage findings after wrist joint trauma, a retrospective analysis of one of the authors’ (JKA) wrist arthroscopies during 1 year was investigated. In the consecutive series (n = 48) of wrist arthroscopies (unpublished data), that was evaluated in 2019, 8 cases (16.7%) with chondral lesions were found, often together with concomitant partial or total ligament injuries. Two of them were full-thickness chondral injuries. 19 Three solitary chondral injuries (2 posttraumatic after intraarticular distal radial fractures and one iatrogenic due to intraarticular screw penetration) were found. The remaining 3 chondral injuries had concomitant partial or total ligament injuries or ulnar impaction syndrome with ulnar positive variance. Ulnar impaction syndrome was treated by Wafer osteotomy 8 ( Fig. 7 ) or converted to open surgery with ulnar shortening osteotomy procedure. 7 The chondral lesions at the proximal ulnar part of lunate, often seen in conjunction with ulnar impaction were treated by microfracturing ( Fig. 8 ) and HALT lesions by shaving and abrasion4,5 ( Fig. 9a and b ).
Figure 8.
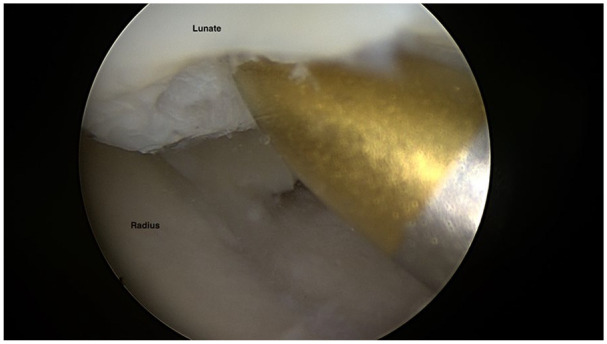
Microfracture of a proximal ulnar chondral injury at lunate.
The surgeon has the surgical skills level 4 according to Tang and Giddins. 74
Discussion
Our literature review concluded that very few articles on cartilage trauma of relevance are present in the current literature and that no consensus can be reached regarding treatment of cartilage injuries in the wrist. Only level of evidence IV-V articles was found. No reports on only isolated cartilage lesions in the wrist were found, rather cartilage lesions were reported in combination with ligament injuries emphasizing the complex interplay between the multiple bones involved in joint motions.1,29 About 30% of patients examined with wrist arthroscopies had cartilage lesions findings,1,29 while in our reported consecutive series of one year (n = 48) of wrist arthroscopies, 16.7% showed cartilage injuries, all related to fractures or ligament injuries.
The difference in incidence may be explained by different patient groups, different diagnostic parameters and different surgical skills, according to Tang and Giddins. 74 However, the author’s findings that most of the chondral injuries in the wrist have concomitant ligament injuries, is in line with the findings of Lindau et al. 1 and Swart and Tabg. 29
Posttraumatic OA in the wrist is most often the cause of former ligament injury with gradual development of carpal instability, followed by carpal collapse and degenerative OA (SLAC/SNAC) 3 ( Fig. 6 ) or seen after an intraarticular distal radius fracture. A vascular disruption with subsequent osteonecrosis and OA development as seen in Preiser’s and Kienböck’s diseases might have traumatic origin.
Wrist ligament injuries are, in our clinical experience, often initially neglected as sprains (patient’s and/or doctor’s delay) and with the patients not remembering a former significant trauma, leading to difficulties in associating the initial traumatic injury to the later displayed posttraumatic osteoarthrosis.75,76
The wrist is not a weight-bearing joint like the hip, knee, and ankle. Therefore, not all patients suffer from symptoms after wrist cartilage injuries, even if osteoarthritis, such as in SLAC and SNAC has developed. 3 At the same time, one must keep in mind that the cartilage in the wrist is thin (2 mm) compared with for instance 7 to 8 mm in the patella. 77 Different anatomical variations in the wrist such as lunate types I or II appear to influence the incidence and localization of chondral injuries.25,26 Further studies of different patterns of cartilage injuries compared with anatomical variations in the wrist are needed.
For the development of wrist OA, repetitive microtrauma could be of importance. Jones et al. 78 examined the prevalence of hand and wrist OA in elite former cricket and rugby union players and found that former elite cricketers reported more hand pain than rugby players and speculated that risk factors aside from injury, such as chronic load or repetitive microtrauma, may be more prominent in the development and progression of hand and wrist OA in former elite male athletes.
There are several limitations to this study. No follow-up or functional scores in terms of the author’s (JKA) recorded wrist arthroscopy cases were used. There is a risk of selection bias in the small series of wrist arthroscopies performed. There is also always a risk of publication bias in articles with small sample sizes. The scarce numbers of available articles limited the results and conclusions. The articles found in the literature review were case reports (LoE V) or case series (LoE IV) with few included patients with short term follow-ups. Only English written articles were included in the literature review which is a limitation related to existing papers published in other languages describing also wrist injuries.
However, the techniques of wrist arthroscopy were developed throughout the early 1980s. At first, arthroscopy of the wrist was an innovative diagnostics, but a few years later, wrist arthroscopy became increasingly used also as a therapeutic tool.79-85
Cartilaginous lesions in the wrist may be fairly common.1,29,36 Ulnar impaction, degenerative LT injuries, and HALT are often seen with concomitant cartilage lesions as a sign of prior trauma affecting the whole ulnar column of the wrist.4,7 Diagnosis of cartilage lesions in the wrist remains difficult, 21 and the determination of when to operate is not at all clear. However, as wrist OA is a common finding in middle-aged persons indicating that more knowledge is needed to determine better the fate of isolated cartilage lesions related to progression into wrist OA. Careful attention to the medical history and physical examination can make cartilage lesion diagnosis easier, and appropriate surgical intervention can be useful in alleviating symptoms and returning the patients to normal activities as well as being joint protective. Although short-term results are promising, long-term studies are needed before the efficacy of arthroscopic management of cartilage lesions of the wrist is known.18,20,59,85
Larger prospective comparative studies are needed to get any further ideas about the real incidence of chondral injuries in the wrist, their localizations, and severity, the outcome after surgery 20 as well as comparative studies to learn which chondral repair techniques may be recommended in the different types of injuries. A limiting factor, however, is that the number of wrist arthroscopic procedures is inferior to knee and shoulder arthroscopies. However, perhaps a noninferiority study 86 —comparing microfracturing with more novel techniques—or multicenter study could be possible to perform in the future.
Conclusion
There is a lack of knowledge in current literature on cartilage and osteochondral injuries, as well as posttraumatic OA in the wrist. There is also a lack of knowledge with regard to treatment of these injuries. Cartilage injuries appear to be rather common, being found in 17% to 32% of all wrist arthroscopies after trauma, but no guidelines regarding conservative or surgical treatment can be recommended at the moment. Larger prospective comparative studies, noninferiority studies, or multicenter studies are needed.
Footnotes
Acknowledgments and Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Informed Consent: Informed consent was obtained from all individual participants for being included in the study.
ORCID iD: Jonny K. Andersson  https://orcid.org/0000-0002-7002-7239
https://orcid.org/0000-0002-7002-7239
References
- 1. Lindau T, Arner M, Hagberg L. Chondral and ligamentous wrist lesions in young adults with distal radius fractures. A descriptive, arthroscopic study in 50 patients. J Hand Surg Br. 1997;22(5):638-43. [DOI] [PubMed] [Google Scholar]
- 2. Berger RA. The anatomy of the ligaments of the wrist and distal radioulnar joints. Clin Orthop Relat Res. 2001;383(2):32-40. [DOI] [PubMed] [Google Scholar]
- 3. Watson HK, Ballet FL. The SLAC wrist: scapholunate advanced collapse pattern of degenerative arthritis. J Hand Surg Am. 1984;9(3):358-65. [DOI] [PubMed] [Google Scholar]
- 4. Thurston AJ, Stanley JK. Hamato-lunate impingement. Arthroscopy. 2000;16(5):540-4. [DOI] [PubMed] [Google Scholar]
- 5. Harley BJ, Palmer AK, Boles SD, Werner FW. Arthroscopic resection of arthrosis of the proximal hamate: a clinical and biomechanical study. J Hand Surg Am. 2004;29(4):661-7. [DOI] [PubMed] [Google Scholar]
- 6. Palmer AK, Werner FW. The triangular fibrocartilage complex of the wrist: anatomy and function. J Hand Surg Am. 1981;6(2):153-62. [DOI] [PubMed] [Google Scholar]
- 7. Minami K, Kato H. Ulnar shortening for triangular fibrocartilage complex tears associated with ulnar positive variance. J Hand Surg Am. 1998;23(5):904-8. [DOI] [PubMed] [Google Scholar]
- 8. Tomaino MM, Weiser RW. Combined arthroscopic TFCC debridement and wafer resection of the distal in wrists with triangular fibrocartilage complex tears and positive ulnar variance. J Hand Surg Am. 2001;26(6):1047-52. [DOI] [PubMed] [Google Scholar]
- 9. Aitken S, Court-Brown CM. The epidemiology of sports-related fractures of the hand. Injury. 2008;39:1377-83 [DOI] [PubMed] [Google Scholar]
- 10. Amillo-Garayoa S, Romero-Muñoz LM, Pons-DeVillanueva J. Bilateral Preiser’s disease: a case report and review of the literature. Musculoskelet Surg. 2011;95(2):131-3. [DOI] [PubMed] [Google Scholar]
- 11. Schuind F, Eslami S, Ledoux P. Kienbock’s disease. J Bone Joint Surg Br. 2008;90(2):133-9. [DOI] [PubMed] [Google Scholar]
- 12. Hess DE, Werner BC, Deal DN. Use of particulated juvenile articular cartilage allograft for osteochondral lesions of the wrist. Hand (NY). 2017;12(5):NP62-NP67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ho PC, Tse WL, Wong WY. Arthroscopic transplantation of osteochondral autograft for treatment of cartilage defects in the wrist. Hand Clin. 2017;33(4):755-67. [DOI] [PubMed] [Google Scholar]
- 14. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006-12. [DOI] [PubMed] [Google Scholar]
- 15. Sackett DL. Rules of evidence and clinical recommendations on the use of antithrombotic agents. Chest. 1986;89(2 Suppl):2S-3S. [PubMed] [Google Scholar]
- 16. Laulan J, Marteau E, Bacle G. Wrist osteoarthritis. Orthop Traumatol Surg Res. 2015;101(1 Suppl):S1-S9. [DOI] [PubMed] [Google Scholar]
- 17. Cooney W, Manuel J, Froelich J, Rizzo M. Total wrist replacement: a retrospective comparative study. J Wrist Surg. 2012;1(2):165-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Culp RW, Osterman AL, Kaufmann RA. Wrist arthroscopy: operative procedures. In: Green DP, Hotchkiss RN, Pederson WC, Wolfe SW, eds. Green’s operative hand surgery. 5th ed. Elsevier; 2005. p 781-803. [Google Scholar]
- 19. Outerbridge RE. The etiology of chondromalaciae patellae. J Bone Joint Surg Br. 1961;43-B:752-57. [DOI] [PubMed] [Google Scholar]
- 20. Brittberg M, Winalski CS. Evaluation of cartilage injuries and repair. J Bone Joint Surg Am. 2003;85-A(Suppl 2):58-69. [DOI] [PubMed] [Google Scholar]
- 21. Andersson JK, Andernord D, Karlsson J, Fridén J. Efficacy of magnetic resonance imaging and clinical tests in diagnostics of wrist ligament injuries: a systematic review. Arthroscopy. 2015;31(10):2014-20. [DOI] [PubMed] [Google Scholar]
- 22. Pallaver A, Honigmann P. The role of cone-beam computed tomography (CBCT) scan for detection and follow-up of traumatic wrist pathologies. J Hand Surg Am. 2019;44(12):1081-87. [DOI] [PubMed] [Google Scholar]
- 23. Suojärvi N, Haapamäki V, Lindfors N, Koskinen SK. Radiocarpal injuries: cone beam computed tomography arthrography, magnetic resonance arthrography, and arthroscopic correlation among 21 patients. Scand J Surg. 2017;106(2):173-79. [DOI] [PubMed] [Google Scholar]
- 24. McQueen FM, McHaffie A, Clarke A, Lee AC, Reeves Q, Curteis B, et al. MRI osteitis predicts cartilage damage at the wrist in RA: a three-year prospective 3T MRI study examining cartilage damage. Arthritis Res Ther. 2014;16(1_suppl):R33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Dharap AS, Lutfi I, Abu-Hijleh MF. Population variation in the incidence of the medial (hamate) facet of the carpal bone lunate. Anthropol Anz. 2006;64(1_suppl):59-65. [PubMed] [Google Scholar]
- 26. McLean JM, Turner PC, Bain GI, Rezaian N, Field J, Fogg Q. An association between lunate morphology and scaphoid-trapezium-trapezoid arthritis. J Hand Surg Eur. 2009;34(6):778-82. [DOI] [PubMed] [Google Scholar]
- 27. Cottias P, Alnot JY, Masmejean E, Touam B, Cesari B, Cadot B. Fractures of the wrist with cartilage rupture in young adults. Apropos of 18 cases [in French]. Ann Chir Main Memb Super. 1997;16(1_suppl):39-48. [DOI] [PubMed] [Google Scholar]
- 28. Mrkonjic A, Geijer M, Lindau T, Tägil M. No long-term risk of wrist osteoarthritis due to subchondral haematomas in distal radial fractures. J Plast Surg Hand Surg. 2018;52(3):163-5. [DOI] [PubMed] [Google Scholar]
- 29. Swart E, Tang P. The effect of ligament injuries on outcomes of operatively treated distal radius fractures. Am J Orthop (Belle Mead NJ). 2017;46(1_suppl):E41-E44. [PubMed] [Google Scholar]
- 30. Tarabin N, Gehrmann S, Mori V, Oezel L, Wollschläger L, Rommelfanger G, et al. Assessment of articular cartilage disorders after distal radius fracture using biochemical and morphological nonenhanced magnetic resonance imaging. J Hand Surg Am. 2020;45(7):619-25. [DOI] [PubMed] [Google Scholar]
- 31. Caloia MF, Martínez Gallino RN, Caloia H, Rivarola H. Incidence of ligamentous and other injuries associated with scaphoid fractures during arthroscopically assisted reduction and percutaneous fixation. Arthroscopy. 2008;24(7):754-9. [DOI] [PubMed] [Google Scholar]
- 32. Linscheid RL, Dobyns JH. Athletic injuries of the wrist. Clin Orthop Relat Res. 1985;198:141-51. [PubMed] [Google Scholar]
- 33. Mitchell JA, Adams BD. Hand and wrist injuries: wrist pain in gymnasts. In: Renstrom PAFH, ed. Clinical practice of sports injury prevention and care, volume V of the Encyclopedia of sports medicine. Blackwell Scientific; 1993. p 78-83. [Google Scholar]
- 34. Dautel G, Merle M. Chondral lesions of the midcarpal joint. Arthroscopy. 1997;13(1_suppl):97-102. [DOI] [PubMed] [Google Scholar]
- 35. Viegas SF. The lunatohamate articulation of the midcarpal joint. Arthroscopy 1990;6(1_suppl):5-10. [DOI] [PubMed] [Google Scholar]
- 36. Tumilty JA, Squire DS. Unrecognized chondral penetration by a Herbert screw in the scaphoid. J Hand Surg Am. 1996;21(1_suppl):66-8. [DOI] [PubMed] [Google Scholar]
- 37. Zhang Y, Jordan JM. Epidemiology of osteoarthritis. Clin Geriatr Med. 2010;26(3):355-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Marshall M, Watt FE, Vincent TL, Dziedzic K. Hand osteoarthritis: clinical phenotypes, molecular mechanisms and disease management. Nat Rev Rheumatol. 2018;14(11):641-56. [DOI] [PubMed] [Google Scholar]
- 39. Vina ER, Kwoh CK. Epidemiology of osteoarthritis: literature update. Curr Opin Rheumatol. 2018;30(2):160-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Stahl S, Hentschel PJ, Held M, Manoli T, Meissner C, Schaller HE, et al. Characteristic features and natural evolution of Kienböck’s disease: five years’ results of a prospective case series and retrospective case series of 106 patients. J Plast Reconstr Aesthet Surg. 2014;67(10):1415-26. [DOI] [PubMed] [Google Scholar]
- 41. Claessen FMAP, Schol I, Kolovich GP, Ring D. Avascular necrosis of the scaphoid Preiser disease. Arch Bone Jt Surg. 2020;8(1_suppl):94-8. doi: 10.22038/abjs.2019.39187.2047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Weiss KE, Rodner CM. Osteoarthritis of the wrist. J Hand Surg Am. 2007;32(5):725-46. [DOI] [PubMed] [Google Scholar]
- 43. Gignac MAM, Irvin E, Cullen K, Van Eerd D, Beaton DE, Mahood Q, et al. Men and women’s occupational activities and the risk of developing osteoarthritis of the knee, hip, or hands: a systematic review and recommendations for future research. Arthritis Care Res (Hoboken). 2020;72(3):378-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Mayfield JK, Johnson RP, Kilcoyne RK. Carpal dislocations: pathomechanics and progressive perilunar instability. J Hand Surg Am. 1980,;5(3):226-41. [DOI] [PubMed] [Google Scholar]
- 45. Herzberg G, Comtet JJ, Linscheid RL, Amadio PC, Cooney WP, Stalder J. Perilunate dislocations and fracture-dislocations: a multicenter study. J Hand Surg Am. 1993;18(5):768-79. [DOI] [PubMed] [Google Scholar]
- 46. Huber M, Eder C, Loibl M, Berner A, Zellner J, Kujat R, et al. RFE based chondroplasty in wrist arthroscopy indicates high risk for chondrocytes especially for the bipolar application. BMC Musculoskelet Disord. 2015;16(1_suppl):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Whipple TL. Chronic wrist pain. Instr Course Lect. 1995;44:129-37. [PubMed] [Google Scholar]
- 48. Grawe B, Burge A, Nguyen J, Strickland S, Warren R, Rodeo S, et al. Cartilage regeneration in full-thickness patellar chondral defects treated with particulated juvenile articular allograft cartilage: an MRI analysis. Cartilage. 2017;8(4):374-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Buckwalter JA, Bowman GN, Albright JP, Wolf BR, Bollier M. Clinical outcomes of patellar chondral lesions treated with juvenile particulated cartilage allografts. Iowa Orthop J. 2014;34:44-9. [PMC free article] [PubMed] [Google Scholar]
- 50. Griffin JW, Gilmore CJ, Miller MD. Treatment of a patellar chondral defect using juvenile articular cartilage allograft implantation. Arthrosc Tech. 2013;2(4):e351-e354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Giza E, Delman C, Coetzee JC, Schon LC. Arthroscopic treatment of talus osteochondral lesions with particulated juvenile allograft cartilage. Foot Ankle Int. 2014;35(10):1087-94. [DOI] [PubMed] [Google Scholar]
- 52. Lanham NS, Carroll JJ, Cooper MT, Perumal V, Park JS. A comparison of outcomes of particulated juvenile articular cartilage and bone marrow aspirate concentrate for articular cartilage lesions of the talus. Foot Ankle Spec. 2017;10(4):315-21. [DOI] [PubMed] [Google Scholar]
- 53. Ng A, Bernhard K. The use of particulated juvenile allograft cartilage in foot and ankle surgery. Clin Podiatr Med Surg. 2018;35(1_suppl):11-8. [DOI] [PubMed] [Google Scholar]
- 54. Chawla S, Saper MG. Fresh precut osteochondral allograft core transplantation for the treatment of capitellum osteochondritis dissecans. Arthrosc Tech. 2020;9(6):e797-e802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Gaspar MP, Jacoby SM, Marchetto PA, DeLuca PF, Culp RW. Osteochondral autograft transplantation for proximal lunate articular defects. J Wrist Surg. 2017;6(4):329-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Lee YK, Lee M, Lee JM. Osteochondral autograft transplantation for osteochondritis dissecans of the scaphoid: case report. J Hand Surg Am. 2011;36(5):820-3. [DOI] [PubMed] [Google Scholar]
- 57. Obert L, Lepage D, Ferrier M, Tropet Y. Rib cartilage graft for posttraumatic or degenerative arthritis at wrist level: 10-year results. J Wrist Surg. 2013;2(3):234-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Obert L, Lepage D, Sergent P, Rochet S, Gallinet D, Tropet Y, et al. Post-traumatic malunion of the distal radius treated with autologous costal cartilage graft: a technical note on seven cases. OrthopTraumatol Surg Res. 2011;97(4):430-7. [DOI] [PubMed] [Google Scholar]
- 59. Carelli F, Sgherzi S, Sillani A, Magris C. Effective implantation of autologous chondrocytes in a patient suffering from a painful and invalidating rizoarthrosis: a case report. Cases J. 2009;18(2):7886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Mulford JS, Ceulemans LJ, Nam D, Axelrod TS. Proximal row carpectomy vs four corner fusion for scapholunate (SLAC) or scaphoid nonunion advanced collapse (SNAC) wrists: a systematic review of outcomes. J Hand Surg Eur. 2009;4(2):256-63. [DOI] [PubMed] [Google Scholar]
- 61. Saltzman BM, Frank JM, Slikker W, Fernandez JJ, Cohen MS, Wysocki RW. Clinical outcomes of proximal row carpectomy versus four-corner arthrodesis for post-traumatic wrist arthropathy: a systematic review. J Hand Surg Eur Vol. 2015;40(5):450-7. [DOI] [PubMed] [Google Scholar]
- 62. Van Nuffel M, Vanhees M, Maeckelbergh L, Degreef I, De Smet L. Four-corner fusion versus proximal row carpectomy: a retrospective review with a minimal follow-up of 9 years. Acta Orthop Belg. 2020;86(1_suppl):146-50. [PubMed] [Google Scholar]
- 63. Fulchignoni C, Caviglia D, Rocchi L. Resurfacing capitate pyrocarbon implant after proximal row carpectomy: a literature review. Orthop Rev (Pavia). 2020;2512(Suppl 1):8679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Montiel V, Payo-Ollero J, Amillo S. Proximal row carpectomy in patients older than 50 years: 3 to 16 years of follow-up. Rev Esp Cir Ortop Traumatol. 2019;63(4):295-9. [DOI] [PubMed] [Google Scholar]
- 65. Williams JB, Weiner H, Tyser AR. Long-term outcome and secondary operations after proximal row carpectomy or four-corner arthrodesis. J Wrist Surg. 2018;7(1_suppl):51-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Pillukat T, Schädel-Höpfner M, Prommersberger KJ. Complex fragmentation of the articular surface of the distal radius: management with small Kirschner wires and bone graft. Tech Hand Up Extrem Surg. 2012;16(1_suppl):1-4. doi: 10.1097/BTH.0b013e318225473e [DOI] [PubMed] [Google Scholar]
- 67. Kolovich GP, Kalu CM, Ruff ME. Current trends in treatment of Kienböck disease: a survey of hand surgeons. Hand (NY). 2016;11(1_suppl):113-8. doi: 10.1177/1558944715616953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Wu CH, Strauch RJ. Wrist denervation: techniques and outcomes. Orthop Clin North Am. 2019;50(3):345-56. [DOI] [PubMed] [Google Scholar]
- 69. Dellon AL. Joint denervation. An atlas of surgical techniques. Springer Nature; 2019. p 45-60. doi: 10.1007/978-3-030-05538-7 [DOI] [Google Scholar]
- 70. Rein S, Winter J, Kremer T, Siemers F, Range U, Euchner N. Evaluation of proprioception in denervated and healthy wrist joints. J Hand Surg Eur. 2020;45(4):408-13. doi: 10.1177/1753193419897192 [DOI] [PubMed] [Google Scholar]
- 71. Kadhum M, Riley N, Furniss D. Is partial wrist denervation beneficial in chronic wrist pain? A systematic review. J Plast Reconstr Aesthet Surg. 2020;73(10):1790-800. [DOI] [PubMed] [Google Scholar]
- 72. Hazewinkel MHJ, Lans J, Lunn KN, Garg R, Eberlin KR, Chen NC. Complications and factors associated with reoperation following total wrist fusion. J Wrist Surg. 2020;9(6):498-508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Berber O, Garagnani L, Gidwani S. Systematic review of total wrist arthroplasty and arthrodesis in wrist arthritis. J Wrist Surg. 2018;7(5):424-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Tang JB, Giddins G. Why and how to report surgeons’ levels of expertise. J Hand Surg Eur. 2016;41(4):365-6. [DOI] [PubMed] [Google Scholar]
- 75. Fredericson M, Ho C, Waite B, Jennings F, Peterson J, Williams C, et al. Magnetic resonance imaging abnormalities in the shoulder and wrist joints of asymptomatic elite athletes. PM R. 2009;1(2):107-16. [DOI] [PubMed] [Google Scholar]
- 76. Lisle DA, Shepherd GJ, Cowderoy GA, O’Connell PT. MR imaging of traumatic and overuse injuries of the wrist and hand in athletes. Magn Reson Imaging Clin N Am. 2009;17(4):639-54. [DOI] [PubMed] [Google Scholar]
- 77. Draper CE, Besier TF, Gold GE, Fredericson M, Fiene A, Beaupre GS, et al. Is cartilage thickness different in young subjects with and without patellofemoral pain? Osteoarthritis Cartilage. 2006;14(9):931-7. [DOI] [PubMed] [Google Scholar]
- 78. Jones ME, Davies MAM, Shah K, Kemp S, Peirce N, Leyland KM, et al. The prevalence of hand and wrist osteoarthritis in elite former cricket and rugby union players. J Sci Med Sport. 2019;22(8):871-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Obdeijn MC, Tuijthof GJ, van der Horst CM, Mathoulin C, Liverneaux P. Trends in wrist arthroscopy. J Wrist Surg. 2013;2(3):239-46. doi: 10.1055/s-0033-1351355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Jackson RW. Quo venis quo vadis: the evolution of arthroscopy. Arthroscopy. 1999;15(6):680-5. [DOI] [PubMed] [Google Scholar]
- 81. Sennwald G. Diagnostic arthroscopy: indications and interpretations of findings. J Hand Surg Br. 2001;26B(3):241-6. [DOI] [PubMed] [Google Scholar]
- 82. Bain GI, Munt J, Turner PC. New advances in wrist arthroscopy. Arthroscopy. 2008;24(3):355-67. [DOI] [PubMed] [Google Scholar]
- 83. Jackson RW. A history of arthroscopy. Arthroscopy. 2010;26(1_suppl):91-103. [DOI] [PubMed] [Google Scholar]
- 84. Michelotti BF, Chung KC. Diagnostic wrist arthroscopy. Hand Clin. 2017;33(4):571-83. doi: 10.1016/j.hcl.2017.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Savoie FH, 3rd. The role of arthroscopy in the diagnosis and management of cartilaginous lesions of the wrist. Hand Clin. 1999;15(3):423-8. [PubMed] [Google Scholar]
- 86. Leung JT, Barnes SL, Lo ST, Leung DY. Non-inferiority trials in cardiology: what clinicians need to know. Heart. 2020;106(2):99-104. [DOI] [PMC free article] [PubMed] [Google Scholar]