Abstract
Objectives
The impact of anterior cruciate ligament (ACL) reconstruction on knee osteoarthritis (OA) is still unclear. The aim of the current meta-analysis was to compare surgical treatment versus nonoperative management of ACL tears to assess the impact of these approaches on knee OA development at a 5 and 10 years of follow-up.
Design
A meta-analysis was performed after a systematic literature search (May 2021) was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines. Both randomized and nonrandomized comparative studies with more than 5 years of follow-up were selected. Influence of the treatment was assessed in terms of knee OA development, subjective and objective clinical results, activity level, and risk of further surgeries. Risk of bias and quality of evidence were assessed following the Cochrane guidelines.
Results
Twelve studies matched the inclusion criteria, for a total of 1,004 patients. Level of evidence was rated low to very low. No difference was documented in terms of knee OA development, Tegner score, subjective International Knee Documentation Committee (IKDC), and Lysholm scores. A significant difference favoring the surgical treatment in comparison with a nonsurgical approach was observed in terms of objective IKDC score (P = 0.03) and risk of secondary meniscectomy (P < 0.0001). The level of evidence was considered very low for subjective IKDC, low for knee OA development, objective IKDC, number of secondary meniscectomies, and Lysholm score, and moderate for post-op Tegner score.
Conclusions
The meta-analysis did not support an advantage of ACL reconstruction in terms of OA prevention in comparison with a nonoperative treatment. Moreover, no differences were reported for subjective results and activity level at 5 and 10 years of follow-up. On the contrary, patients who underwent surgical treatment of their ACL tear presented important clinical findings in terms of better objective knee function and a lower rate of secondary meniscectomies when compared with conservatively managed patents.
Protocol Registration: CRD420191156483 (PROSPERO)
Keywords: anterior cruciate ligament, ACL reconstruction, conservative treatment, osteoarthritis, radiologic evaluation
Introduction
Anterior cruciate ligament (ACL) tears are common injuries among young and active individuals involved in sport activities that imply contact, deceleration, twisting, cutting, and jumping. Approximately 200,000 ACL tears occur every year in the United States with an increasing number of ACL reconstructions (from 32.4 patients per 100,000 person/year in the early 1990s to 43.5 patients per 100,000 person/year in the 2010s).1-5 Laxity due to ACL injury causes reduced knee function and abnormal changes at different levels in terms of joint homeostasis, with lower activity levels and poorer quality of life.6,7 While the consequences of the detrimental biomechanical changes are well recognized, more debated remains their management, with both surgical and conservative treatments being proposed to date. 8
Restoring knee anatomy and biomechanics through surgery can minimize sheer and torsional forces on menisci and cartilage surface, legitimating a safer return to previous levels of activity.9,10 On the contrary, there is also evidence that injured patients could cope well with ACL deficiency and thus they may undergo a conservative approach, which could lead to enough functional stability and no secondary injuries, as well as to the desired level of pivoting and cutting activities.11-16 While the clinical benefit of surgery versus conservative treatment is still debated, even more controversial is the possibility to limit joint degeneration by reconstructing the ACL, with conflicting results regarding the most effective approach to prevent knee osteoarthritis (OA).17,18
The aim of the present meta-analysis was to quantitatively synthesize the best literature evidence on this topic, including only studies directly comparing surgical treatment versus nonoperative management of an ACL tear, with a clear radiological knee OA evaluation and at least 5 years of follow-up. The hypothesis was that surgical treatment could provide lower rates of knee OA, while ensuring better knee function and higher activity levels compared with the conservative management of ACL tears.
Materials and Methods
Search Strategy and Article Selection
A systematic literature search was performed on May 10, 2021, using PubMed, Web of Science, Cochrane library, Scopus literature, and gray literature databases using the following string: (ACL injury OR ACL tear OR ACL rupture) AND (ACL reconstruction OR ACL surgery OR non-operative OR conservative OR non-reconstructive) AND (osteoarthritis OR OA). All duplicates were removed and then all records were assessed for eligibility by title and abstract, with full-text reading evaluation when needed. Inclusion/exclusion criteria are reported in Table 1. The Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines were used. The article selection process was independently performed by 2 authors (M.C., D.P.) with disagreement solved by consensus or by the intervention of a third author (L.D.). 19
Table 1.
Inclusion and Exclusion Criteria for Study Selection.
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Studies comparing conservative versus surgical management of ACL tears | Included patients that underwent revision ACL injury |
| Level of evidence I-II-III | Level IV studies and expert opinions, systematic reviews and meta-analyses |
| Studies with at least 5 years of follow-up | Preclinical or ex vivo studies |
| Data about radiological outcomes for the evaluation of knee OA | Articles not in English, German, or Italian |
ACL = anterior cruciate ligament; OA = osteoarthritis.
Data Extraction, Synthesis, and Measurement of Outcomes
Relevant data from the included articles were independently extracted by 2 authors from the full-text version or supplementary data (M.C., L.D.), using a previously extraction form according to Cochrane’s guidelines. Nonoperative approach was defined as all the treatment options not involving a surgical reconstruction, that is, physiotherapy, functional training, wait and see, bracing, and so on. Information on study methodology concerned level of evidence, study design, inclusion/exclusion criteria, graft source, time from injury to intervention, other associated surgical treatments, post-surgical rehabilitation, and follow-up length. Patients’ characteristics and clinical outcomes of treatments were also collected: number of patients included and assessed at follow-up, patients’ sex, age, body mass index (BMI), and cause of injuries, previous surgical treatment on the index knee, associated lesions, pre-surgical and post-surgical clinical scores (objective International Knee Documentation Committee [IKDC], subjective IKDC, Lysholm, Tegner, Knee injury and Osteoarthritis Outcome Score [KOOS]), rate of re-tears, rate of complications, knee stability, secondary meniscectomies, and radiological results (IKDC, Kellgren and Lawrence, Fairbank, Ahlbäck, and joint space narrowing Osteoarthritis Research Society International – OARSI – scoring systems). To normalize data from the different radiological scores, the equivalence table reported in the article by Kohn et al. 20 and a cutoff higher than second grade on Kellgren and Lawrence, Ahlbäck and OARSI scoring system, and C grade on Fairbank and IKDC scoring systems were set to identify clinically significant OA according to previous literature.21-24 As such, OA was considered as a dichotomous outcome.
Assessment of Risk of Bias and Quality of Evidence
The risk of bias was assessed using the revised tool for Risk of Bias in randomized trials (RoB 2.0) and in nonrandomized trials (ROBINS-I) approved by the Cochrane collaboration group.25,26
Randomized studies were considered as “low risk” of bias if a low risk of bias was scored in all domains of the analysis; it was rated as “some concerns” if a score of “some concerns” was obtained in at least one domain of the analysis. In the end, randomized studies were judged as “high risk” if the study was judged to be at high risk of bias in at least one domain of the analysis or it had risen some concerns for multiple domains.
Nonrandomized studies were rated as at a low risk of bias if data were reasonably complete, proportions, and reasons for missing participants were similar across intervention groups, the analysis addressed missing data, and is likely to have removed any risk of bias. A study was judged as moderate risk of bias if there were deviations from usual practice, but their impact on the outcome is expected to be slight and proportions of and reasons for missing participants differ slightly across intervention groups. In the end a study was rated at a high risk of bias if methods of outcome assessment were not comparable across intervention groups and there were important co-interventions not balanced across intervention groups, or there were deviations from the intended interventions (in terms of implementation and/or adherence) that were likely to impact on the outcome.
The overall quality of evidence for each outcome was graded according to the Grading of Recommendations Assessment, Development and Evaluation (GRADE) guidelines. 27 An outcome was deemed to have a very low level of evidence if the true effect was probably markedly different from the estimated effect. A low level of evidence was marked when that the true effect is similar to the estimated effect. Similarly, a moderate and high level of evidence was assigned when the true effect of intervention was deemed very close or almost the same of the true effect.
Statistical Analysis
To investigate the effect of treatment on all outcomes, different analyses were conducted. Using RevMan software 5.3, the differences between surgical and conservative management of ACL injury in terms of knee OA, subjective and objective IKDC, Tegner activity level, Lysholm score, and need of a secondary meniscectomy were assessed through the Mantel-Hanszel test and expressed as risk ratios for dichotomous variables (RR = risk ratio surgical/conservative), and through the inverse variance method and expressed as mean differences for continuous variables (MD = mean difference surgical-conservative). Heterogeneity was tested using Cochran’s Q statistic and I2 metric and was considered significant when I2 > 25%. A fixed-effect model was preferred in the absence of significant heterogeneity; when the I2 was above the cutoff of 25%, a random effect model was used. Due to the high clinical heterogeneity of the included studies (heterogeneous rehabilitation protocols, different activity levels, etc.), a sensitivity statistical analysis was performed, applying the random effect model for all the considered outcomes. A P value of 0.05 was set as level of significance. When data from the same study population were available at different follow-ups or in different studies, the longest-term follow-up was selected. This choice was made in light of the nature of OA evolution, as it is a condition which often requires many years to be clinically evident. As such, a sensitivity analysis was performed including only studies with a follow-up longer than 10 years. A sensitivity analysis excluding all confounding factors (i.e., age, meniscal injuries.) was considered; however, single patient data were not available. As such, a pair match analysis to normalize confounders could not be performed.
When mean and standard deviations were not available from the full-text articles, they were estimated from median range and sample size using the formula proposed by Hozo et al. 28 or following the Cochrane guidelines, and sensitivity analyses excluding these studies were performed.
Results
Article Selection and Patients’ Characteristics
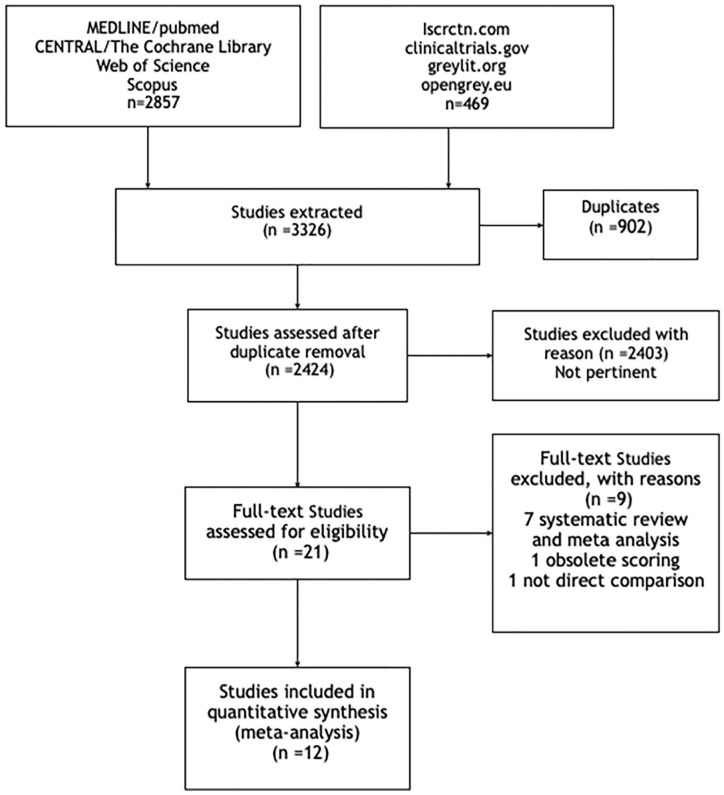
The PRISMA flowchart of the article’s selection process is presented in Figure 1. Out of 2,424 identified studies, 12 were included in the quantitative synthesis (3 randomized controlled trials [RCTs] and 9 non-randomized comparative studies). To evaluate OA rates, 4 studies used the Kellgren and Lawrence score, 4 opted for the IKDC radiological score, 2 opted for the OARSI joint space narrowing scoring system, 1 study used the Fairbank score, and 1 used the Ahlbäck score. The mean follow-up was 11 years ranging from 5 to 24 years. Ten studies opted for a bone patellar tendon bone (BPTP) graft; in one article, both BPTP and hamstring grafts were included, and one article did not specify the graft used. Subjective IKDC was reported in 5 studies, objective IKDC was assessed in 7 articles, Lysholm was reported in 9 studies, and Tegner activity level was analyzed in 9 studies. Secondary meniscectomies were reported in 5 studies.
Figure 1.
PRISMA flowchart of the article selection process. PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-analysis.
Overall, 1,004 patients were included in this meta-analysis, 547 in the surgical group, and 457 in the conservative group. The male/female ratio was 2:3, and the overall mean age at the time of injury was 30 years (range: 18-56 years). No significant differences in baseline characteristics of the patients were found between the 2 treatment approaches in all included studies. Further details on studies and patients are reported in Table 2.
Table 2.
Characteristics of the Included Studies and Patients.
| Study | Inclusion Criteria | Patients | Sex | Age | F-U | Associated Lesions | Associated Treatments | Graft Source | Treatment Protocols | Time to Treatment | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Incl. | F-U | Surgical | Conservative | ||||||||||
| Fink et al. 2001 | S | No additional ligamentous injury greater than grade 2, no chondrosis greater than grade 1, and time from injury to diagnostic arthroscopy of less than 4 weeks. To be included in the operative group, reconstruction had to be performed within 6 months after injury | 72 | I:52 II:46 |
55 M 16 F |
32 y | I:74,2 m II:132 m |
11 MM tears, 12 LM tears, 7 MCL sprains | At I follow-up: 3 MM tear, 2 LM tear, 1 graft
rupture At II follow-up: 2 MM tear |
BPTP | Surgery was performed through arthroscopy with a BPTP graft. Graft was fixed with sutures tied over a bone bridge. Postop protocol consisted in immobilization at 208° of knee flexion for 6 weeks with partial weight bearing, followed by a structured physical therapy protocol | Home exercise program emphasizing hamstring strengthening, cycling, and swimming was prescribed. Pts with limited ROM were sent to physical therapy first. All pts were followed regularly for up to 6 m after diagnosis was established, depending on their progress and symptoms | 3.3 m |
| C | 41 | I:32 II:25 |
I:84,2 m II:140 m |
At time of injury: 6 MM tear, 5 LM tear, 4 MCL sprains | At I follow-up: 3 MM tear, 1 MCL sprain At II follow-up: 1 MM tear, 2 instabilities |
||||||||
| Fithian et al. 2005 | S | Examination of knee within 4 weeks of index injury, KT-1000 arthrometer measurements indicate an injured minus normal knee anterior displacement difference of 3 mm or more on the 20 lb, 30 lb, or manual maximum test | 96 | 96 | 108 M 101 F |
39 y | 6.6 y | NR | 1 meniscal repair | BPTP | All ACL reconstructions during this study used mid-third patellar tendon autograft and were performed endoscopically (single incision), following the technique originally described by Jackson | In pts conservatively treated wb was allowed as tolerated. 3 m of strengthening and ROM exercises were performed. Jogging and sport-specific drills were permitted between 6 and 12 w after inj. Pts were encouraged to avoid any contact sports for at least 3 m. All kind of sports were permitted at 3 m unless symptomatic. ACL bracing was not advised | NR |
| C | 113 | 113 | 6.6 y | NR | 21 meniscectomies 8 meniscal repairs | ||||||||
| Frobell et al. 2013 | S | 18-35 y, <4w knee trauma, signs of ACL tear, Tegner 5-9. No LCL, MCL, full-thickness cartilage injuries, grade III meniscal tears, previous knee surgery, bilateral injuries, PL complex injuries, pregnancy, DVT or coagulative conditions, claustrophobia, steroids, systemic diseases, unstable meniscal lesion | 89 | 89 | 88 M 30 F |
26 y | 58 m | NR | 29 meniscectomies | HQG BPTP |
The patellar tendon procedure was performed in 25 subjects and the hamstring tendon procedure was used in 36 subjects. Surgery was performed while pts were under general anesthesia, and meniscal surgery was carried out as needed, followed by ACL reconstruction. | The protocol included 4 levels described by exercise examples and goals for ROM, muscle function, and functional performance for first 24 w of rehabilitation. Goals for each level should be met prior to progression to the next level. Pain, swelling and discomfort slowed progression and, if persistent, a visit to the treating clinician was scheduled. Use of anti- inflammatory drugs was allowed as needed. | NR |
| C | 29 | 29 | 60 m | NR | 17 meniscectomies | ||||||||
| Kessler et al. 2008 | S | ACL rupture confirmed by arthroscopy | 60 | 60 | 68 M 41 F |
30 y | 11.1 y | NR | 7 meniscectomies | BPTP | ACL-reconstruction was performed by various senior registrars specialized in knee ligament surgery. The reconstruction was performed with bone patellar tendon bone graft with extra-articular screw fixation of tibia and femur in arthroscope-assisted and mini-arthrotomy technique | Both groups followed the same rehabilitation program. Bracing for 6 w, training of hamstrings and quadriceps muscle, proprioception training, no flexion under load greater than 60° for 6 w, return to sports activities after 3 m and return to pivoting sports after 9 m. Criteria to return to sports were no pain, swelling, instability during or after activity | NR |
| C | 49 | 49 | 7.5-16.3 y | NR | 18 meniscectomies | ||||||||
| Lohmander et al. 2004 | S | All 338 players with an ACL injury sustained while playing league soccer in Sweden in 1986 were identified through the insurance company archives | 52 | 41 | 0 M 67 F |
19 y | 12 y | 34 meniscal injuries | 34 meniscal surgeries performed simultaneously to ACL rec or as a separate procedure | BPTP | Open ACL reconstruction | NR | 3 y |
| C | 32 | 26 | 12 y | ||||||||||
| Meunier et al. 2007 | S | Acute and total rupture of the ACL age under 30 | 42 | 58 | 68 M 33 F |
22 y | 15 y | 22 Meniscus injury 27 MCL injury |
2 reoperations due to graft failure | BPTB | 44 pts underwent repair using multiple sutures fixed in both stumps of the ACL and tied over staples to the external tibial and femoral cortices. 10 pts, had no aug., and 34 pts had aug. with a 15-mm-wide strip from the iliotibial routed through the same drill holes and on top of the ACL remnant | An intensive rehabilitation program was then instituted. When ROM was regained, pts in group S followed essentially the same rehabilitation program, focusing on strength and coordination, as those in group C. | NR |
| C | 52 | 36 | 15 y | 32 Meniscus injury 25 MCL injury |
17 me | ||||||||
| Mihelic et al. 2011 | S | Acute isolated ACL injury with possible meniscus lesion, no combined or cartilage injury, or previous trauma or surgery on the index knee | 36 | 36 | 44 M 10 F | 25 y | 17-20 y | 6 MM injuries and 5 bilat. menisci lesions | NR | BPTP | Reconstruction with double incisions technique | Plaster cast for 3 w. After that period, patients were sent to rehab for 2 m. They performed exercises to regain full ROM and strengthen their quadriceps | 19 m |
| C | 18 | 18 | 17-20 y | 10 MM inj. and 13 had bilat. menisci injury | NR | ||||||||
| Myklebust et al. 2003 | S | 87 ACL injuries of players in the 3 upper divisions of Norwegian team handball were recorded prospectively during the 1989 to 1990 and 1990 to 1991 seasons | 57 | 37 | 50 M 29 F | NR | 9.4 y | NR | NR | BPTP | 82% of patients underwent ACL reconstruction while 18% had their ligament sutured | NR | NR |
| C | 22 | 13 | 9.4 y | NR | NR | ||||||||
| Neuman et al. 2008 | S | ACL rupture with no previous major injury to lower limbs, no x-ray documented fracture, no psychosocial disorders no professional-level athletes | 22 | 17 | 58 M 42 F | 26 y | 15 y | 8 MM tears 16 LM tears 7 bilateral menisci injury |
94 secondary meniscectomies | NR | NR | Pts underwent 2 types of treatment with the same aim of regaining joint ROM and improve neuromuscular function. Pts were advised not to participate in contact sports | 4 y |
| C | 78 | 62 | 15 y | ||||||||||
| Streich et al. 1994 | S | Anterior cruciate ligament insufficiency | 40 | 40 | 56 M 24 F |
25 y | 15.4 y | NR | 9 partial meniscectomies | BPTP | Arthroscopic reconstruction with transtibial approach | Neuromuscular-based rehabilitation program to regain joint mobility and knee stability. As subjective stability improved, the level of activity was raised. All conservatively treated patients were instructed to avoid high demand pivot-shift activities such as sky soccer and comparable sports | 7.3 m |
| C | 40 | 40 | 15.4 y | NR | 10 partial meniscectomies | ||||||||
| Tsoukas et al. 2016 | S | Isolated ACL injuries, a body mass index of <30, no previous major injury or surgery of the knee and patients who successfully completed the final follow-up | 17 | 17 | 17 M 15 F | 37y | 10.1 y | NR | NR | BPTP | Arthroscopic reconstruction with anteromedial technique | Partial wb with a full-time extension brace was permitted for the first 6 w. Stationary bike, proprioception exercises, short arc quadriceps sets, and hamstring curls were performed for the next 6 w. At 3 m, jogging, swimming in straight line, and bicycle were started. At 6 m, pivot sports were permitted, while contact sports were allowed at 8-9 m | NR |
| C | 15 | 15 | 10.1 y | NR | NR | ||||||||
| van Yperen et al. 2018 | S | ACL rupture treated operatively or nonoperatively | 25 | 25 | 38 M 12 F | 27 y | 21.2 y | NR | 18 meniscectomies 4 reruptures |
BPTP | Arthroscopic reconstruction with transtibial approach | Pts who were treated nonoperatively were advised to follow a physical therapist–led exercise program for a minimum duration of 3 m | NR |
| C | 25 | 25 | 24.1 y | NR | 19 meniscectomies | ||||||||
Incl. = included; F-U = follow-up; M = male; F = female; Y = years; MM = medial meniscus; LM = lateral meniscus; MCL = medial collateral ligament; BPTP = bone patellar tendon bone; ROM = range of motion; Inj. = injury; NR = not reported; ACL = anterior cruciate ligament; LCL = lateral collateral ligament; PL: postero-lateral; HQG = Hamstring Quadrupled Graft; BPTB = bone patellar to bone graft; DVT = Deep Vein Thrombosis.
Outcomes of Surgical versus Conservative ACL Reconstruction
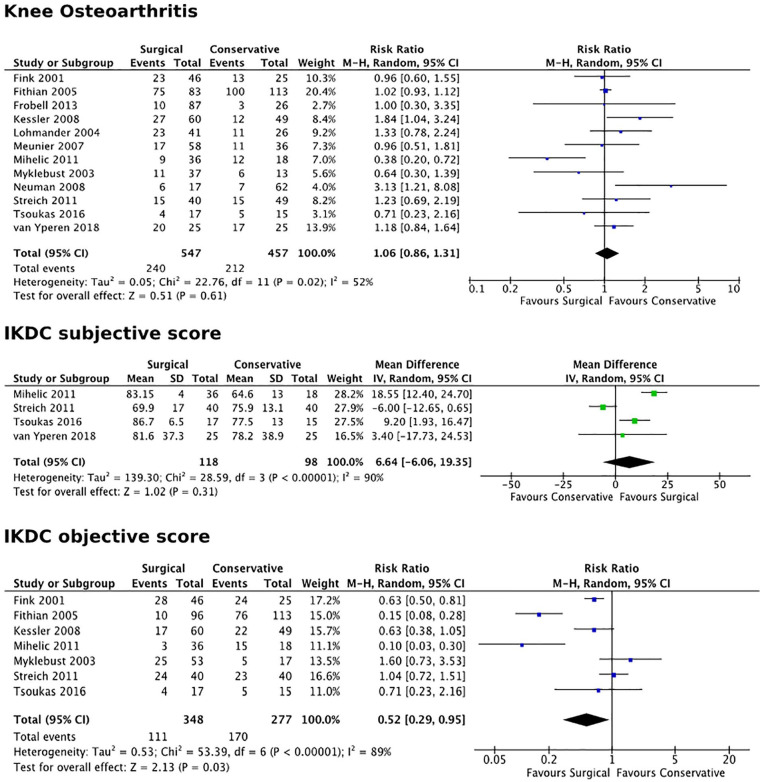
In the surgical versus conservative analysis, no significant differences were found in terms of development rates of knee OA (12 studies, RR = 0.93, P = 0.19, confidence interval [CI]: 0.86-1.31; Figure 2). These results were confirmed by the sensitivity analysis including only studies with a follow-up longer than 10 years (8 studies, RR = 1.14, P = 0.49, CI: 0.74-1.28).
Figure 2.
Forest plots for knee osteoarthritis rates and IKDC subjective and objective evaluation forms. IKDC = International Knee Documentation Committee; CI = confidence interval.
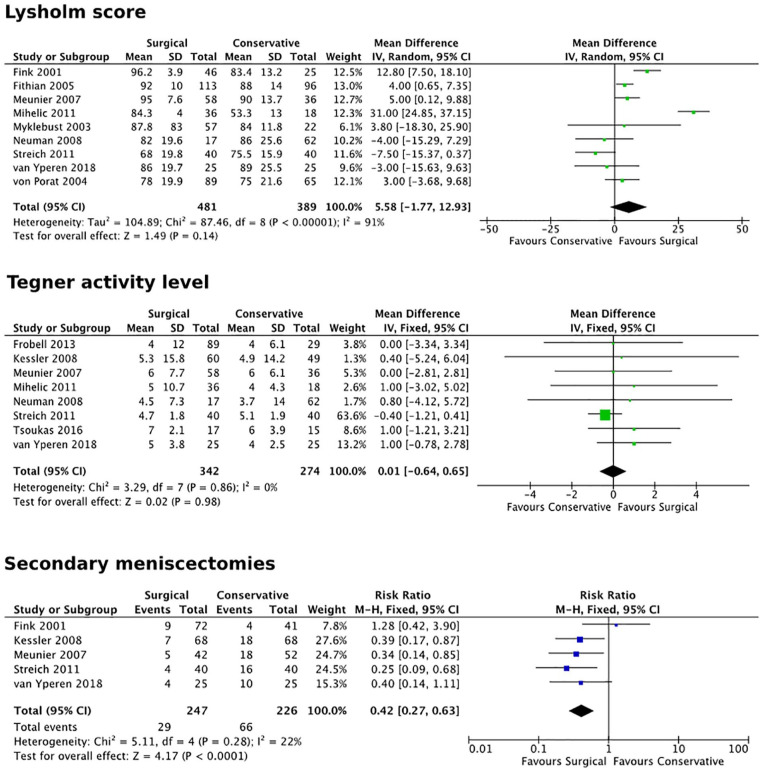
No statistically significant differences were also found in terms of subjective IKDC score (4 studies, MD = 6.6, P = 0.31, CI: −6.06 to 19.35; Figure 2), Lysholm score (8 studies, MD = 5.6, P = 0.14, CI: −1.77 to 12.93), and Tegner activity level (9 studies, MD = 0.1 P = 0.69, CI: −0.64 to 0.65; Figure 3) at final follow-up. Objective evaluation in terms of abnormal/severely abnormal IKDC objective score was found statistically significant (7 studies, RR = 0.52, P = 0.03, CI: 0.29-0.95; Figure 2) in favor of the surgical treatment in comparison with the nonsurgical treatment. A higher number of patients (66 out of 226 assessed) in the conservative group required secondary arthroscopic meniscectomy, whereas only 29 of the 249 included in the surgical group went through this procedure during follow-up (5 studies, RR = 0.42, P < 0.0001, CI: 0.27-0.63; Figure 3).
Figure 3.
Forest plots for Lysholm and Tegner scores and risk of secondary meniscectomies. CI = confidence interval.
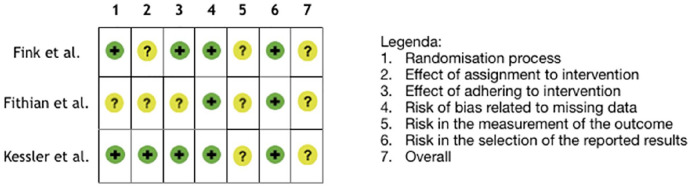
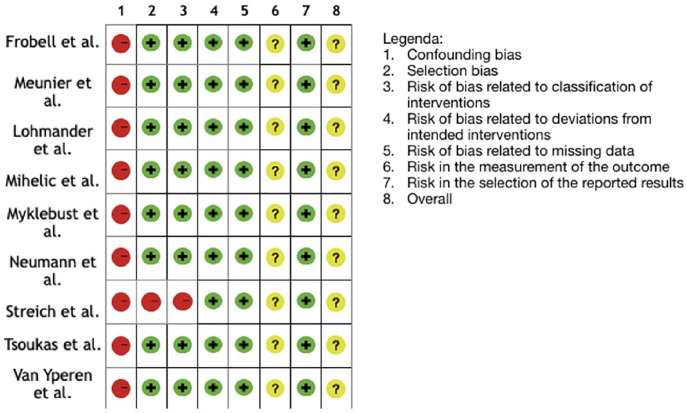
Risk of Bias and Quality of Evidence
The risk of bias was rated moderate (“some concerns”) in the 3 RCTs: the main source of bias was the lack of blinding of the assessor, which could influence the evaluation of the outcome. Moreover, the possibility to undergo surgery given to the patients of the conservative group in 2 of the RCTs included29,30 may have directed the patients with a worst outcome outside the conservative group. In the nonrandomized comparative trials, the risk of bias should be considered high. The main problem was the presence of confounders that cannot be controlled: among all, the level of activity after intervention may be different in the 2 groups and this could seriously affect results at long-term follow-up.
The level of evidence was considered very low for subjective IKDC, low for knee OA development, objective IKDC, number of secondary meniscectomies, and Lysholm score, and moderate for post-op Tegner score. The risk of bias of the included studies was considered to have influenced the results of all outcomes. Statistical heterogeneity was above the cutoff of I2 = 25% in the results of 4 out of 7 outcomes: this may be due to the heterogeneity in the characteristics of the included patients and in the rehabilitation protocols. Finally, the low number of patients included caused further downgrading of the level of evidence for “imprecision” for subjective IKDC and number of meniscectomies. Details of risk of bias assessments are listed in Figures 4 and 5.
Figure 4.
Risk of Bias of Included Randomized Controlled Trial.
Green ( )
stands for “low risk”; yellow (
)
stands for “low risk”; yellow ( ) for “moderate
risk”; red for (
) for “moderate
risk”; red for ( ) “high risk.”
) “high risk.”
Figure 5.
Risk of Bias of Included Nonrandomized Controlled Trial.
Green ( )
stands for “low risk”; yellow (
)
stands for “low risk”; yellow ( ) for “moderate
risk”; red for (
) for “moderate
risk”; red for ( ) “high risk.”
) “high risk.”
Discussion
The main finding of this meta-analysis is that there is no evidence supporting that ACL reconstruction prevents knee OA. Moreover, similar results were obtained in terms of subjective outcomes and activity level versus the nonoperative approach. On the contrary, the objective knee evaluation was in favor of surgery, which also reduced the need for secondary meniscectomies.
Patients who withstand an ACL rupture are at a higher risk of developing knee OA than the general population (prevalence 24.5%-51.2%). 31 The detrimental effects on joint biomechanics have been well-demonstrated by several studies, both ex vivo and in patients.32,33 Residual chronic instability can result in a bigger risk of cartilage damage and, consequently, higher rates of knee OA, due to the higher stress endured by the joint for the lack of one of the knee’s main static stabilizers. From this perspective, surgery has been considered an effective option to reduce instability with the aim of preventing the development of secondary degeneration.34-38
However, the exact pathogenic mechanisms through which ACL injury influences the progression of joint degeneration are still not clear, as many factors, aside from joint instability, concur in the pathogenesis and progression of knee OA. 39 In this light, an ACL rupture must be considered as a lesion involving the whole joint rather than a mere ligament injury. Many other knee structures can be affected, which can also be responsible for the development of knee OA. 40
The frequent presence of associated lesions underlines an important aspect: the impact of the acute trauma on all knee structures.39,41,42 To this regard, bone bruise has a high prevalence (up to 55.2% in the most recent papers) among ACL injured individuals, and its persistence has been correlated to a more severe degenerative progression of the entire joint. 42 Recent evidence also suggested possible effects on the long-term clinical outcome.41,42 The altered subchondral bone signal can be the expression of a worse joint derangement.43,44 In fact, size and location of bone bruise correlate with the presence of meniscal lesions, which are one of the main risk factors for post-traumatic knee OA. 45 Other studies46-48 also showed a correlation with an increased rate of cartilage damage, another trigger for the development of knee OA. 49
Cartilage lesions are often described in correspondence to the index trauma at the BME (Bone Marrow Edema) level, with an estimate overall prevalence of 32% among patients undergoing primary ACL reconstruction. 50 The presence of cartilage lesions can negatively affect the outcome of ACL injuries. Many studies on large cohorts of patients, such as those from the Scandinavian national registry51-53 and the MOON cohort,54,55 pointed out how patients with cartilage defects benefit less from an ACL reconstruction, achieving significantly lower Patient-Reported Outcome Measure (PROM) scores at mid-term follow-up. Moreover, this joint derangement can go beyond the local damage to the articular surface. High-energy traumas can trigger an immune response in both chondrocytes and synoviocytes, which produce inflammatory mediators such as interleukins 1, 6, and 8 as well as tumor necrosis factor (TNF). 56 These molecules are able to induce proteoglycans degradation, collagen destruction, as well as chondrocytes necrosis. Recent evidence shows that prolonged activation of inflammatory pathways due to an ACL injury can alter joint homeostasis and OA biomarkers: fluid aggrecan, MMP-1, MMP-3, and ADAM12 were found increased, whereas the metalloprotease inhibitor TIMP-1 tended to decrease after ACL injury. 57 Thus, besides causing the first insult at the cartilage level, the index trauma can alter the joint homeostasis by triggering detrimental inflammatory and degenerative processes.
Another key aspect that can influence knee OA progression is the meniscal status, as the incidence of degeneration after ACL rupture ranges from 16% for an isolated lesion to 50% when the injury involves a meniscal lesion. 58 A previous meta-analysis on 1,554 patients after an ACL reconstruction pointed out that OA prevalence was significantly higher in those undergoing meniscectomy, yielding a 3.5 higher odds of developing knee OA at long term. 59 Moreover, cartilage lesions associated with meniscal tears have been correlated with poorer subjective and objective results. 60 Secondary meniscectomies, especially of the medial meniscus, wielded a higher risk of post-traumatic knee OA also in conservatively treated patients. 61
The results of this meta-analysis confirmed previous literature36,62 showing a higher number of secondary meniscal procedures in patients treated conservatively. However, while the protection of the meniscal structure from ACL reconstruction was demonstrated, the impact of the lower number of secondary meniscectomies in terms of knee OA preventions is still controversial. A recent study of Lien-Iversen et al. suggested higher OA rates in surgically treated patients, although with some limitations due to the low number of included patients. 62 On the contrary, the paper of Øiestad et al. 63 pointed out that patients who returned to pivoting sport had lower rates of knee OA, although with a high risk of selection bias due to the retrospective nature of this study. This meta-analysis overcame some of the limitations of previous publications, including all published comparative studies on this topic. Data from the available literature showed a lower number of meniscectomies after ACL reconstruction, but still similar rates of OA at 5 and at 10 years of follow-up. The unexpected results in terms of lack of OA protection from surgical ACL reconstruction and joint biomechanics restoration might be explained from different perspectives.
A possible explanation of the finding that ACL surgery did not have an impact over OA development may be that, aside from 3 rather small RCTs,29,30,40 most of the literature relies on cohort studies where the choice of treatment was made according both to the surgeons’ opinion and the patients’ desires. Patients who chose a surgical treatment might have different expectations and desired level of activity, whereas individuals choosing a nonsurgical approach could have been advised on the importance of lowering their level of activity, avoiding activities which could be detrimental for their joints.13,64 Patients often opt for surgery aiming at a return to sport, which can entail remarkable stress on their knees. This higher level of stress could impact on the development of knee OA. However, this remains a mere speculation. While the sport activity level after surgery is a key aspect, it was unfortunately poorly documented by the available studies. Future research should monitor and properly report both return to sport and activity level of treated patients, as this factor may be crucial in concealing the potential benefits of surgery in terms of knee OA development.34,65
Another aspect should be considered while interpreting these findings. The current literature presents limitations which are inevitably reflected in this meta-analysis. The majority of the studies are nonrandomized trials with a serious risk of bias. Besides the high risk of selection bias with uncontrolled confounders, in 2 out of 3 included RCTs patients were given the possibility to undergo surgery in case of unsatisfactory results with the conservative treatment: this unavoidably has led to the exclusion from the conservative group of patients with the worst outcome. Moreover, current studies do not allow to properly handle statistically the data from cross-over patients and delayed surgeries. As a result, the documented level of evidence is low for the evaluation of the risk of OA development (primary outcome of the study) and in almost all the secondary outcomes. This hinders the possibility to draw definitive conclusions on this issue, and new high-level trials should shed light on this topic. 66 Furthermore, the use of different radiological scoring systems to evaluate OA may be an important source of heterogeneity and represents another weakness of this evaluation: the IKDC scoring system could overreport the severity of OA 67 and the Ahlbäck classification has a poor inter- and intraobserver agreement. 68 Finally, we analyzed papers with more than 5 years of follow-up and performed a sensitivity analysis at 10 years. Still, the latter was based on a lower number of patients, which warrants more research efforts toward documenting results at long term, when a difference in terms of OA development may be more likely detected. Nonetheless, despite these limitations, this meta-analysis, performed according to Cochrane guidelines, was able to quantitatively synthesize several aspects and to underline some interesting findings. ACL reconstruction is a common and effective procedure able to restore knee biomechanics; however, despite the better objective outcome and the protection from further meniscal lesions, there is no evidence of benefits in terms of OA development after surgical treatment of ACL tears.
In the end, this meta-analysis of the current literature did not support an advantage of ACL reconstruction in terms of OA prevention. Moreover, no differences were also reported for subjective results and activity level at mid/long-term follow-up. On the contrary, some clinically relevant findings have been underlined, both in terms of joint derangement and functional outcome. Patients who underwent a surgical treatment of their ACL tear presented better knee function and a lower rate of secondary meniscectomies in comparison with nonoperatively managed patents.
Footnotes
Acknowledgments and Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr. Cuzzolin, Dr. Deabate, Professor Filardo, and Dr. Previtali declare they have no conflict of interest. Professor Zaffagnini reports personal fees from I+ SRL, grants from Fidia Farmaceutici SPA, CartiHeal ltd, IGEA Clinical Biophysics, BIOMET, and Kensey Nash, outside the submitted work. In addition, Professor Zaffagnini has a Springer patent with royalties paid. Professor Candrian reports grants from Medacta International SA, Johnson & Johnson, Lima Corporate, Zimmer Biomet, and Oped AG, outside the submitted work.
Ethical Approval: This study was approved by our institutional review board.
ORCID iDs: Marco Cuzzolin  https://orcid.org/0000-0002-2653-6677
https://orcid.org/0000-0002-2653-6677
Davide Previtali  https://orcid.org/0000-0002-0284-4368
https://orcid.org/0000-0002-0284-4368
References
- 1. Gianotti SM, Marshall SW, Hume PA, Bunt L. Incidence of anterior cruciate ligament injury and other knee ligament injuries: a national population-based study. J Sci Med Sport. 2009;12(6): 622-7. [DOI] [PubMed] [Google Scholar]
- 2. Lyman S, Koulouvaris P, Sherman S, Do H, Mandl LA, Marx RG. Epidemiology of anterior cruciate ligament reconstruction: trends, readmissions, and subsequent knee surgery. J Bone Joint Surg Am. 2009;91(10): 2321-8. [DOI] [PubMed] [Google Scholar]
- 3. Majewski M, Susanne H, Klaus S. Epidemiology of athletic knee injuries: a 10-year study. Knee. 2006;13(3): 184-8. [DOI] [PubMed] [Google Scholar]
- 4. Mall NA, Chalmers PN, Moric M, Tanaka MJ, Cole BJ, Bach BR, Jr, et al. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med. 2014;42(10): 2363-70. [DOI] [PubMed] [Google Scholar]
- 5. Sanders TL, Maradit Kremers H, Bryan AJ, Larson DR, Dahm DL, Levy BA, et al. Incidence of anterior cruciate ligament tears and reconstruction: a 21-year population-based study. Am J Sports Med. 2016;44(6): 1502-7. [DOI] [PubMed] [Google Scholar]
- 6. Filbay SR, Culvenor AG, Ackerman IN, Russell TG, Crossley KM. Quality of life in anterior cruciate ligament-deficient individuals: a systematic review and meta-analysis. Br J Sports Med. 2015;49(16): 1033-41. [DOI] [PubMed] [Google Scholar]
- 7. Lai CCH, Ardern CL, Feller JA, Webster KE. Eighty-three per cent of elite athletes return to preinjury sport after anterior cruciate ligament reconstruction: a systematic review with meta-analysis of return to sport rates, graft rupture rates and performance outcomes. Br J Sports Med. 2018;52(2): 128-38. [DOI] [PubMed] [Google Scholar]
- 8. Andersson C, Odensten M, Good L, Gillquist J. Surgical or non-surgical treatment of acute rupture of the anterior cruciate ligament. A randomized study with long-term follow-up. J Bone Joint Surg Am. 1989;71(7): 965-74. [PubMed] [Google Scholar]
- 9. Allen CR, Livesay GA, Wong EK, Woo SL. Injury and reconstruction of the anterior cruciate ligament and knee osteoarthritis. Osteoarthritis Cartilage. 1999;7(1_suppl): 110-21. [DOI] [PubMed] [Google Scholar]
- 10. Jarvela T, Kannus P, Jarvinen M. Anterior cruciate ligament reconstruction in patients with or without accompanying injuries: a re-examination of subjects 5 to 9 years after reconstruction. Arthroscopy. 2001;17(8): 818-25. [DOI] [PubMed] [Google Scholar]
- 11. Barrance PJ, Williams GN, Snyder-Mackler L, Buchanan TS. Do ACL-injured copers exhibit differences in knee kinematics? an MRI study. Clin Orthop Relat Res. 2007;454:74-80. [DOI] [PubMed] [Google Scholar]
- 12. Lohmander LS, Ostenberg A, Englund M, Roos H. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum. 2004;50(10): 3145-52. [DOI] [PubMed] [Google Scholar]
- 13. Meuffels DE, Favejee MM, Vissers MM, Heijboer MP, Reijman M, Verhaar JAN. Ten year follow-up study comparing conservative versus operative treatment of anterior cruciate ligament ruptures. A matched-pair analysis of high level athletes. Br J Sports Med. 2009;43(5): 347-51. [DOI] [PubMed] [Google Scholar]
- 14. Moksnes H, Snyder-Mackler L, Risberg MA. Individuals with an anterior cruciate ligament-deficient knee classified as noncopers may be candidates for nonsurgical rehabilitation. J Orthop Sports Phys Ther. 2008;38(10): 586-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Neuman P, Englund M, Kostogiannis I, Friden T, Roos H, Dahlberg LE. Prevalence of tibiofemoral osteoarthritis 15 years after nonoperative treatment of anterior cruciate ligament injury: a prospective cohort study. Am J Sports Med. 2008;36(9): 1717-25. [DOI] [PubMed] [Google Scholar]
- 16. von Porat A, Roos EM, Roos H. High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study of radiographic and patient relevant outcomes. Ann Rheum Dis. 2004;63(3): 269-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Daniel D. Who benefits from ACL surgery. Oral presentation on the American Academy of Orthopaedic Surgeons Instructional Course “Anterior Cruciate Ligament,” Washington, DC. 1992. February 21-25. [Google Scholar]
- 18. Strehl A, Eggli S. The value of conservative treatment in ruptures of the anterior cruciate ligament (ACL). J Trauma. 2007;62(5): 1159-62. [DOI] [PubMed] [Google Scholar]
- 19. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4): 264-9. [DOI] [PubMed] [Google Scholar]
- 20. Kohn MD, Sassoon AA, Fernando ND. Classifications in brief: Kellgren-Lawrence classification of osteoarthritis. Clin Orthop Relat Res. 2016;474(8): 1886-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chalmers PN, Mall NA, Moric M, Sherman SL, Paletta GP, Cole BJ, et al. Does ACL reconstruction alter natural history? a systematic literature review of long-term outcomes. J Bone Joint Surg Am. 2014;96(4): 292-300. [DOI] [PubMed] [Google Scholar]
- 22. Culvenor AG, Engen CN, Oiestad BE, Engebretsen L, Risberg MA. Defining the presence of radiographic knee osteoarthritis: a comparison between the Kellgren and Lawrence system and OARSI atlas criteria. Knee Surg Sports Traumatol Arthrosc. 2015;23(12): 3532-9. [DOI] [PubMed] [Google Scholar]
- 23. KELLGREN JH, LAWRENCE JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4): 494-502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Oiestad BE, Engebretsen L, Storheim K, Risberg MA. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med. 2009;37(7): 1434-43. [DOI] [PubMed] [Google Scholar]
- 25. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ryan R, Hill S. How to GRADE the quality of the evidence. Cochrane Consumers and Communication Group; 2016. Available from: https://colorectal.cochrane.org/sites/colorectal.cochrane.org/files/public/uploads/how_to_grade.pdf.
- 28. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5(1_suppl): 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Frobell RB, Roos HP, Roos EM, Roemer FW, Ranstam J, Lohmander LS. Treatment for acute anterior cruciate ligament tear: five year outcome of randomised trial. BMJ. 2013;346:f232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Meunier A, Odensten M, Good L. Long-term results after primary repair or non-surgical treatment of anterior cruciate ligament rupture: a randomized study with a 15-year follow-up. Scand J Med Sci Sports. 2007;17(3): 230-7. [DOI] [PubMed] [Google Scholar]
- 31. Harris KP, Driban JB, Sitler MR, Cattano NM, Balasubramanian E, Hootman JM. Tibiofemoral osteoarthritis after surgical or nonsurgical treatment of anterior cruciate ligament rupture: a systematic review. J Athl Train. 2017;52(6): 507-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. He C, He W, Li Y, Wang F, Tong L, Zhang Z, et al. Biomechanics of knee joints after anterior cruciate ligament reconstruction. J Knee Surg. 2018;31(4): 352-8. [DOI] [PubMed] [Google Scholar]
- 33. Markolf KL, Burchfield DM, Shapiro MM, Shepard MF, Finerman GA, Slauterbeck JL. Combined knee loading states that generate high anterior cruciate ligament forces. J Orthop Res. 1995;13(6): 930-5. [DOI] [PubMed] [Google Scholar]
- 34. Ajuied A, Wong F, Smith C, Norris M, Earnshaw P, Back D, et al. Anterior cruciate ligament injury and radiologic progression of knee osteoarthritis: a systematic review and meta-analysis. Am J Sports Med. 2014;42(9): 2242-52. [DOI] [PubMed] [Google Scholar]
- 35. Cinque ME, Dornan GJ, Chahla J, Moatshe G, LaPrade RF. High rates of osteoarthritis develop after anterior cruciate ligament surgery: an analysis of 4108 patients. Am J Sports Med. 2018;46(8): 2011-9. [DOI] [PubMed] [Google Scholar]
- 36. Hagmeijer MH, Hevesi M, Desai VS, Sanders TL, Camp CL, Hewett TE, et al. Secondary meniscal tears in patients with anterior cruciate ligament injury: relationship among operative management, osteoarthritis, and arthroplasty at 18-year mean follow-up. Am J Sports Med. 2019;47(7): 1583-90. [DOI] [PubMed] [Google Scholar]
- 37. Lin SH, Wang TC, Lai CF, Tsai RY, Yang CP, Wong CS. Association of anterior cruciate ligament injury with knee osteoarthritis and total knee replacement: a retrospective cohort study from the Taiwan National Health Insurance Database. PLoS One. 2017;12(5): e0178292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Struewer J, Ziring E, Frangen TM, Efe T, Meissner S, Buecking B, et al. Clinical outcome and prevalence of osteoarthritis after isolated anterior cruciate ligament reconstruction using hamstring graft: follow-up after two and ten years. Int Orthop. 2013;37(2): 271-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Luc B, Gribble PA, Pietrosimone BG. Osteoarthritis prevalence following anterior cruciate ligament reconstruction: a systematic review and numbers-needed-to-treat analysis. J Athl Train. 2014;49(6): 806-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Tsoukas D, Fotopoulos V, Basdekis G, Makridis KG. No difference in osteoarthritis after surgical and non-surgical treatment of ACL-injured knees after 10 years. Knee Surg Sports Traumatol Arthrosc. 2016;24(9): 2953-9. [DOI] [PubMed] [Google Scholar]
- 41. Filardo G, Andriolo L, di Laura Frattura G, Napoli F, Zaffagnini S, Candrian C. Bone bruise in anterior cruciate ligament rupture entails a more severe joint damage affecting joint degenerative progression. Knee Surg Sports Traumatol Arthrosc. 2019;27(1_suppl): 44-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Filardo G, Kon E, Tentoni F, Andriolo L, Di Martino A, Busacca M, et al. Anterior cruciate ligament injury: post-traumatic bone marrow oedema correlates with long-term prognosis. Int Orthop. 2016;40(1_suppl): 183-90. [DOI] [PubMed] [Google Scholar]
- 43. Illingworth KD, Hensler D, Casagranda B, Borrero C, van Eck CF, Fu FH. Relationship between bone bruise volume and the presence of meniscal tears in acute anterior cruciate ligament rupture. Knee Surg Sports Traumatol Arthrosc. 2014;22(9): 2181-6. [DOI] [PubMed] [Google Scholar]
- 44. Bisson LJ, Kluczynski MA, Hagstrom LS, Marzo JM. A prospective study of the association between bone contusion and intra-articular injuries associated with acute anterior cruciate ligament tear. Am J Sports Med. 2013;41(8): 1801-7. [DOI] [PubMed] [Google Scholar]
- 45. Englund M, Lohmander L. Risk factors for symptomatic knee osteoarthritis fifteen to twenty-two years after meniscectomy. Arthritis Rheum. 2004;50(9): 2811-9. [DOI] [PubMed] [Google Scholar]
- 46. Faber KJ, Dill JR, Amendola A, Thain L, Spouge A, Fowler PJ. Occult osteochondral lesions after anterior cruciate ligament rupture. Six-year magnetic resonance imaging follow-up study. Am J Sports Med. 1999;27(4): 489-94. [DOI] [PubMed] [Google Scholar]
- 47. Nishimori M, Deie M, Adachi N, Kanaya A, Nakamae A, Motoyama M, et al. Articular cartilage injury of the posterior lateral tibial plateau associated with acute anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2008;16(3): 270-4. [DOI] [PubMed] [Google Scholar]
- 48. Potter HG, Jain SK, Ma Y, Black BR, Fung S, Lyman S. Cartilage injury after acute, isolated anterior cruciate ligament tear: immediate and longitudinal effect with clinical/MRI follow-up. Am J Sports Med. 2012;40(2): 276-85. [DOI] [PubMed] [Google Scholar]
- 49. Theologis AA, Kuo D, Cheng J, Bolbos RI, Carballido-Gamio J, Ma CB, Li X. Evaluation of bone bruises and associated cartilage in anterior cruciate ligament-injured and -reconstructed knees using quantitative t(1rho) magnetic resonance imaging: 1-year cohort study. Arthroscopy. 2011;27(1_suppl): 65-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Filardo G, de Caro F, Andriolo L, Kon E, Zaffagnini S, Marcacci M. Do cartilage lesions affect the clinical outcome of anterior cruciate ligament reconstruction? a systematic review. Knee Surg Sports Traumatol Arthrosc. 2017;25(10): 3061-75. [DOI] [PubMed] [Google Scholar]
- 51. Barenius B, Forssblad M, Engstrom B, Eriksson K. Functional recovery after anterior cruciate ligament reconstruction, a study of health-related quality of life based on the Swedish National Knee Ligament Register. Knee Surg Sports Traumatol Arthrosc. 2013;21(4): 914-27. [DOI] [PubMed] [Google Scholar]
- 52. Røtterud JH, Risberg MA, Engebretsen L, Årøen A. Patients with focal full-thickness cartilage lesions benefit less from ACL reconstruction at 2–5 years follow-up. Knee Surg Sports Traumatol Arthrosc. 2012;20(8): 1533-9. [DOI] [PubMed] [Google Scholar]
- 53. Røtterud JH, Sivertsen EA, Forssblad M, Engebretsen L, Årøen A. Effect of meniscal and focal cartilage lesions on patient-reported outcome after anterior cruciate ligament reconstruction: a nationwide cohort study from Norway and Sweden of 8476 patients with 2-year follow-up. Am J Sports Med. 2013;41(3): 535-43. [DOI] [PubMed] [Google Scholar]
- 54. Cox CL, Huston LJ, Dunn WR, Reinke EK, Nwosu SK, Parker RD, et al. Are articular cartilage lesions and meniscus tears predictive of IKDC, KOOS, and Marx activity level outcomes after anterior cruciate ligament reconstruction? a 6-year multicenter cohort study. Am J Sports Med. 2014;42(5): 1058-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Dunn WR, Wolf BR, Harrell FE, Jr, Reinke EK, Huston LJ, Spindler KP. Baseline predictors of health-related quality of life after anterior cruciate ligament reconstruction: a longitudinal analysis of a multicenter cohort at two and six years. J Bone Joint Surg Am. 2015;97(7): 551-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Vaishya R, Okwuchukwu MC, Agarwal AK, Vijay V. Does anterior cruciate ligament reconstruction prevent or initiate knee osteoarthritis? a critical review. J Arthrosc Jt Surg. Epub 2019. April 5. [Google Scholar]
- 57. King JD, Rowland G, Villasante Tezanos AG, Warwick J, Kraus VB, Lattermann C, et al. Joint fluid proteome after anterior cruciate ligament rupture reflects an acute posttraumatic inflammatory and chondrodegenerative state. Cartilage. 2020;11:329-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Neyret P, Donell ST, Dejour H. Results of partial meniscectomy related to the state of the anterior cruciate ligament. Review at 20 to 35 years. J Bone Joint Surg Br. 1993;75(1_suppl): 36-40. [DOI] [PubMed] [Google Scholar]
- 59. Claes S, Hermie L, Verdonk R, Bellemans J, Verdonk P. Is osteoarthritis an inevitable consequence of anterior cruciate ligament reconstruction? a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2013;21(9): 1967-76. [DOI] [PubMed] [Google Scholar]
- 60. Shelbourne KD, Jari S, Gray T. Outcome of untreated traumatic articular cartilage defects of the knee: a natural history study. J Bone Joint Surg Am. 2003;85-A(Suppl 2):8-16. [DOI] [PubMed] [Google Scholar]
- 61. van Meer BL, Meuffels DE, van Eijsden WA, Verhaar JA, Bierma-Zeinstra SM, Reijman M. Which determinants predict tibiofemoral and patellofemoral osteoarthritis after anterior cruciate ligament injury? a systematic review. Br J Sports Med. 2015;49(15): 975-83. [DOI] [PubMed] [Google Scholar]
- 62. Lien-Iversen T, Morgan DB, Jensen C, Risberg MA, Engebretsen L, Viberg B. Does surgery reduce knee osteoarthritis, meniscal injury and subsequent complications compared with non-surgery after ACL rupture with at least 10 years follow-up? a systematic review and meta-analysis. Br J Sports Med. 2020;54:592-8. [DOI] [PubMed] [Google Scholar]
- 63. Øiestad BE, Holm I, Risberg MA. Return to pivoting sport after ACL reconstruction: association with osteoarthritis and knee function at the 15-year follow-up. Br J Sports Med. 2018;52(18): 1199-204. [DOI] [PubMed] [Google Scholar]
- 64. Segawa H, Omori G, Koga Y. Long-term results of non-operative treatment of anterior cruciate ligament injury. Knee. 2001;8(1_suppl): 5-11. [DOI] [PubMed] [Google Scholar]
- 65. Paschos NK. Anterior cruciate ligament reconstruction and knee osteoarthritis. World J Orthop. 2017;8(3): 212-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Altman DG, Bland JM. Absence of evidence is not evidence of absence. BMJ. 1995;311(7003): 485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Beard DJ, Knezevic K, Al-Ali S, Dawson J, Price AJ. The use of outcome measures relating to the knee. Orthop Trauma. 2010;24(4): 309-16. [Google Scholar]
- 68. Galli M, De Santis V, Tafuro L. Reliability of the Ahlback classification of knee osteoarthritis. Osteoarthritis Cartilage. 2003;11(8): 580-4. [DOI] [PubMed] [Google Scholar]