Abstract
Background
Cerebrospinal fluid (CSF) Aβ1–42 levels and the Aβ1–42/Aβ1–40 ratio are markers of amyloid pathology, but previous studies suggest that their levels might be influenced by additional pathophysiological processes.
Aims
To compare Aβ1–42 and the Aβ1–42/Aβ1–40 ratio in CSF in different neurodegenerative disorders and study their association with other biomarkers (tTau, pTau181, and NfL) and with cognitive and functional progression.
Methods
We included all participants from the Sant Pau Initiative on Neurodegeneration (SPIN) with CSF Aβ1–42 and Aβ1–42/Aβ1–40. Participants had diagnoses of Alzheimer’s disease (AD), dementia with Lewy bodies, frontotemporal lobar degeneration-related syndromes, non-neurodegenerative conditions, or were cognitively normal. We classified participants as “positive” or “negative” according to each marker. We compared CSF levels of tTau, pTau181, and NfL between concordant and discordant groups through ANCOVA and assessed differences in cognitive (MMSE, FCSRT) and functional (GDS, CDR-SOB) progression using Cox regression and linear-mixed models.
Results
In the 1791 participants, the agreement between Aβ1–42 and Aβ1–42/Aβ1–40 was 78.3%. The Aβ1–42/Aβ1–40 ratio showed a stronger correlation with tTau and pTau181 than Aβ1–42 and an agreement with tTau and pTau181 of 73.1% and 77.1%, respectively. Participants with a low Aβ1–42/Aβ1–40 ratio showed higher tTau and pTau181 and worse cognitive and functional prognosis, regardless of whether they were positive or negative for Aβ1–42. The results were consistent across stages, diagnostic categories, and use of different cutoffs.
Conclusion
Although Aβ1–42 and Aβ1–42/Aβ1–40 are considered markers of the same pathophysiological pathway, our findings provide evidence favoring the use of the Aβ1–42/Aβ1–40 ratio in clinical laboratories in the context of AD.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13195-022-00967-z.
Keywords: Amyloid, Aβ1–40, Aβ1–42, Cerebrospinal fluid, Tau, Biomarkers
Introduction
Cerebrospinal fluid (CSF) biomarkers of Alzheimer’s disease (AD) have changed the management of patients with cognitive impairment [1]. In particular, CSF levels of β-amyloid 1–42 (Aβ1–42), total tau (tTau), and its phosphorylated form on threonine 181 (pTau181) have shown very high accuracy for the diagnosis of AD [2–4]. They are consequently being implemented in clinical laboratories [5–9] both for diagnosis and research settings, as well as in clinical trials.
The role of Aβ1–42 in CSF as a marker of amyloid pathology is widely accepted [6, 9, 10]. However, a series of studies have shown that reduced levels of CSF Aβ1-42 can also be found in a variety of conditions different from AD, such as inflammatory diseases, prionopathies, amyloid angiopathy, or frontotemporal dementia [10–15]. The Aβ1–42/Aβ1–40 ratio has proven to be of great value in detecting amyloid pathology both in CSF [16, 17] and plasma [18, 19] and has shown a better correlation with amyloid burden in PET than Aβ1–42 alone [20–22]. However, Aβ1–40 levels are not systematically assessed in many clinical laboratories alleging that this marker alone has no diagnostic value. A large-scale head-to-head comparison between Aβ1–42 and the Aβ1–42/Aβ1–40 ratio would address the question of whether these two markers are equally tracking the same pathophysiological process. It would also inform laboratories on whether to implement the Aβ1–42/Aβ1–40 ratio into the clinical routine.
In the present work, we studied the CSF markers Aβ1–42 and Aβ1–42/Aβ1–40 ratio in a large cohort of participants with a variety of neurodegenerative disorders. We compared the agreement between both measures in different contexts and studied their association with other CSF biomarkers (tTau, pTau181, and NfL) and with cognitive and functional progression. This information is highly relevant in the implementation and interpretation of these markers in clinical routine.
Material and methods
Study participants and clinical classification
We included all participants in the Sant Pau Initiative on Neurodegeneration (SPIN) cohort [23] that underwent lumbar puncture for CSF biomarkers between November 2013 and August 2021. The diagnostic groups included patients with mild cognitive impairment (MCI) or dementia and with either pathophysiological evidence of Alzheimer’s disease (AD), frontotemporal lobar degeneration (FTLD)-related syndromes [24, 25], or probable dementia with Lewy bodies (DLB). Diagnoses were established following internationally accepted diagnostic criteria [6, 7, 9, 26–28]. Clinical symptoms, neuroimaging and CSF biomarkers were considered for the diagnostic classification of patients. We also included participants with Down syndrome (DS) [29, 30] and cognitively normal controls (CN). All CN participants had normal cognitive scores in a formal neuropsychological evaluation [23, 31]. Patients with other diagnoses were grouped as “others” and included participants with prionopathy and other non-neurodegenerative conditions such as psychiatric etiology, vascular cognitive impairment, inflammatory, and those with uncertain etiology. Details about the SPIN cohort have been reported previously [23].
CSF collection and analysis
CSF was obtained by lumbar puncture, collected, and processed in polypropylene tubes following international recommendations [32, 33]. The same pre-analytical handling was followed in all samples [23]. Concentrations of Aβ1–42, Aβ1–40, total tau (tTau), and 181-phosphorylated tau (pTau181) in CSF were measured using commercially available kits in the Lumipulse fully automated platform (Fujirebio-Europe), as previously described [22, 34], and following provider’s instructions in line with Global Biomarker Standardization [35, 36]. For each sample, Aβ1–42, Aβ1–40, tTau, and pTau181 were quantified simultaneously in the same run immediately after the first freeze-thaw cycle of each sample using pristine aliquots containing 500 μL of CSF [22, 34]. The results of the Lumipulse G β-amyloid 1–42 have been standardized according to certified reference material developed by the International Federation of Clinical Chemistry and Laboratory Medicine as recommended by their working group for CSF proteins. Our laboratory participates in the Alzheimer’s Association Quality Control Program led by the University of Gothenburg [37]. Three levels of internal quality controls provided by the manufacturer were assessed for each analyte to assess the reproducibility of the assays. We included at least one level of quality control per analyte in each run. Inter-assay coefficients of variation (CV%) were between 1.7% and 6.8% for all levels and analytes.
Neurofilament light (NfL) levels in CSF were measured using a commercially available ELISA kit (NF-light, UMAN DIAGNOSTICS, Umea, Sweden) as previously described [24, 25]. The mean inter- and intra-assay coefficients of variation were 3.4% and 11.4%, respectively.
Definition of amyloid profile
To ensure that the cutoffs for Aβ1–42 and Aβ1–42/Aβ1–40 had comparable levels of sensitivity and specificity, we applied cutoffs corresponding to one-sided 95% quantile (Q95%) values in a middle-aged cognitively healthy population (age range 23–60 years, 67% female). This age range was selected to minimize the presence of preclinical AD in the reference population. We used these Q95% cutoffs for Aβ1–42 (637 pg/mL) and Aβ1–42/Aβ1–40 (0.070) to classify all participants in four different profiles: two concordant profiles in which both Aβ1–42 and Aβ1–42/Aβ1–40 ratio were above (Aβ1–42[−]Ratio[−]) or below (Aβ1–42[+]Ratio[+]) their respective cutoffs, and two discordant profiles, in which only one of the two amyloid parameters, Aβ1–42 or the Aβ1–42/Aβ1–40 ratio, was abnormal (Aβ1–42[+]Ratio[−] and Aβ1–42[−]Ratio[+], respectively). The objective of classifying participants in four amyloid profiles is to assess the particularities of those groups where Aβ1–42 and the Aβ1–42/Aβ1–40 ratio are discordant (Aβ1–42[−]Ratio[+] and Aβ1–42[+]Ratio[−]) and compare them to those that are clearly amyloid negative (Aβ1–42[–]Ratio[−]) or clearly amyloid positive (Aβ1–42[+]Ratio[+]) according to both markers. More details about the cognitively healthy reference population and results after applying other cutoffs can be found in Additional file 1.
Measures of cognitive and functional impairment
Cognition was assessed by the Mini-Mental State Examination (MMSE) and the free and cued selective reminding test (FCSRT). Global functional impairment was assessed by the Clinical Dementia Rating Scale Sum of Boxes (CDR-SOB) and the Global Deterioration Scale (GDS). Outcomes for cognitive and functional impairment were defined as MMSE < 24 and GDS ≥ 4, respectively [31].
APOE genotyping
DNA was extracted from whole blood using standard procedures and APOE was genotyped according to previously described methods [38].
Statistical analysis
Non-normally distributed variables were log-transformed. Differences in the frequency of categorical variables were assessed by the χ2 test, and we used age- and sex-adjusted analysis of covariance (ANCOVA) to compare CSF levels of tTau, pTau181, and NfL between concordant and discordant groups. We determined Spearman’s correlation coefficients between biomarkers in the whole sample and after stratification by diagnostic category, clinical stage, and amyloid profile. We assessed the association with cognitive and functional progression in patients with mild cognitive impairment through Kaplan-Meier survival curves and age- and sex-adjusted Cox regression analysis. We studied the association of amyloid profiles with a cognitive decline through linear-mixed models. The initial model included baseline MMSE score, baseline age, sex, years of education, pTau181 levels, diagnosis, time, APOE4 status, and amyloid profile together with its interaction with time and with APOE4 status as fixed factors. We defined random intercepts for diagnosis and at the participant level to account for repeated measures and modeled residual errors per diagnostic group. The alpha threshold was set at 0.05, and all analysis were performed using MEDCALC (MEDCALC software ver 15.2.2) and packages “survival” (v.3.1-12), “survminer” (v.0.4.6), “nlme” (v.3.1-147), “multcomp” (v.1.4-13), “ggplot2” (v.3.3.0), and “ggpubr” (v.0.3.0), as implemented in the R statistical software (v 3.6.2). The alpha threshold was set at 0.05 for all analyses.
Ethical approval and consent to participate
All procedures in the study were approved by the Sant Pau Ethics Committee following the standards for medical research in humans recommended by the Declaration of Helsinki. All participants or their legally authorized representatives gave written informed consent.
Results
Demographics and core CSF biomarkers
We included a total of 1791 participants from the SPIN cohort. The demographic characteristics and biomarker results are summarized in Table 1. There were differences in age and male/female proportion between the groups. As expected, the APOEε4 allele was more frequent in AD patients (50%; p < 0.001), and no differences were observed among the other groups. MMSE scores were lower in all symptomatic groups compared to CN (p < 0.001).
Table 1.
Demographics, clinical information, and biomarkers across diagnostic categories
| CN | AD | DLB | FTLD | Down | Others | ||
|---|---|---|---|---|---|---|---|
| N | 197 | 518 | 128 | 186 | 225 | 536 | |
| AGE, years | Mean (SD) | 53.5 (12.5) | 73.1 (6.88) | 75.7 (5.49) | 70.8 (8.58) | 45.1 (10) | 70 (9.18) |
| Median [IQR] | 55 [46–62] | 74 [69–78] | 76 [71–80] | 72 [66–77] | 48 [40–52] | 71 [65–77] | |
| SEX, females/males (% females) | 132/65 (67%) | 311/207 (60%) | 64/64 (50%) | 77/109 (41.4%) | 103/122 (45.8%) | 310/226 (57.8%) | |
| MMSE score | Mean (SD) | 29.2 (0.889) | 23.6 (4.52) | 24 (4.09) | 24 (5.08) | NAa | 25.4 (4.12) |
| Median [IQR] | 29 [29–30] | 25 [22–27] | 24.5 [22–27] | 25 [21–28] | NAa | 27 [24–28] | |
| Education, years | Mean (SD) | 15.6 (3.99) | 10.7 (4.72) | 9.18 (5.05) | 12 (5.13) | 15.3 (3.07) | 10.7 (4.93) |
| Median [IQR] | 16 [12–20] | 10 [8–13] | 8 [7–12] | 12 [8–16] | NAa | 9 [8–13] | |
| APOEε4, APOEε4−/APOEε4+ (%APOEε4+) | 46/151 (23.4%) | 254/251 (50.3%) | 33/93 (26.2%) | 37/139 (21%) | 44/177 (19.9%) | 115/413 (21.8%) | |
| Follow-up, years | Mean (SD) | 2.02 (1.99) | 1.09 (1.49) | 3.33 (1.93) | 1.71 (1.47) | 1.76 (2.09) | 0.59 (1.23) |
| Median [IQR] | 1.71 [0–2.82] | 0 [0–2.06] | 3.46 [2.07–4.52] | 1.52 [0.242–2.66] | NAa | 0 [0–0.383] | |
| Aβ1–42, pg/ml | Mean (SD) | 1148 (397) | 562 (165) | 817 (399) | 938 (446) | 715 (417) | 1000 (500) |
| Median [IQR] | 1118 [849–1371] | 556 [432–673] | 703 [542–1009] | 850 [569–1229] | 583 [430–892] | 896 [609–1323] | |
| Aβ1–40, pg/ml | Mean (SD) | 11,694 (3595) | 12,790 (3781) | 11,506 (4189) | 10,806 (4357) | 11,673 (4678) | 11,399 (4390) |
| Median [IQR] | 11,329 [9238–13,777] | 12,541 [10,125–15,122] | 10,885 [8882–14,234] | 10,140 [7710–13,334] | 11,035 [8346–14,594] | 10,638 [8112–13,986] | |
| Aβ1–42/Aβ1–40 | Mean (SD) | 0.0991 (0.0181) | 0.0453 (0.0108) | 0.0727 (0.0263) | 0.0877 (0.0221) | 0.0615 (0.0226) | 0.0862 (0.0225) |
| Median [IQR] | 0.104 [0.0986–0.109] | 0.0445 [0.0376–0.0514] | 0.0662 [0.0503–0.0996] | 0.0964 [0.0731–0.103] | 0.0562 [0.0422–0.078] | 0.0943 [0.0665–0.103] | |
| tTau, pg/ml | Mean (SD) | 255 (152) | 748 (358) | 456 (334) | 387 (260) | 644 (520) | 334 (231) |
| Median [IQR] | 230 [174–291] | 656 [488–915] | 361 [253–525] | 322 [222–456] | 489 [262–870] | 292 [213–378] | |
| pTau181, pg/ml | Mean (SD) | 37.3 (27.3) | 122 (60.3) | 70.5 (55.5) | 49.9 (39.2) | 100 (96.8) | 45 (27.4) |
| Median [IQR] | 31.6 [24.9–42] | 105 [78.7–145] | 51 [35.7–83] | 39.7 [29.2–54.1] | 63.6 [29.8–151] | 41 [29.3–52.7] | |
| NfL, pg/ml | Mean (SD) | 475 (256) | 1330 (1824) | 1108 (570) | 2079 (1836) | 815 (773) | 1488 (1340) |
| Median [IQR] | 458 [320–533] | 981 [791–1254] | 918 [719–1297] | 1412 [884–2767] | 614 [357–1014] | 1089 [595–1878] | |
| Clinical stage, CN/MCI/dementia (% MCI) | 177/0/0 | 0/296/208 | 2/60/64 | 5/90/80 | NAa | 27/348/125 | |
| Amyloid profile (Aβ1–42[−]Ratio[−]/Aβ1–42[−]Ratio[+]/Aβ1–42[+]Ratio[−]/Aβ1–42[+]Ratio[+]) | 165/13/11/8 | 4/154/2/358 | 50/29/7/42 | 120/8/23/35 | 61/37/13/114 | 345/45/47/100 | |
MMSE Mini-Mental State Examination, CSF cerebrospinal fluid, CN cognitively normal, AD Alzheimer’s disease, DLB dementia with Lewy bodies; FTLD frontotemporal lobar degeneration-related syndrome, MCI mild cognitive impairment
aDue to specific particularities of the clinical and cognitive assessment in the context of intellectual disability, participants with Down syndrome were excluded from the prognostic analysis
Aβ1–42 and the Aβ1–42/Aβ1–40 ratio in CSF show high but not perfect agreement
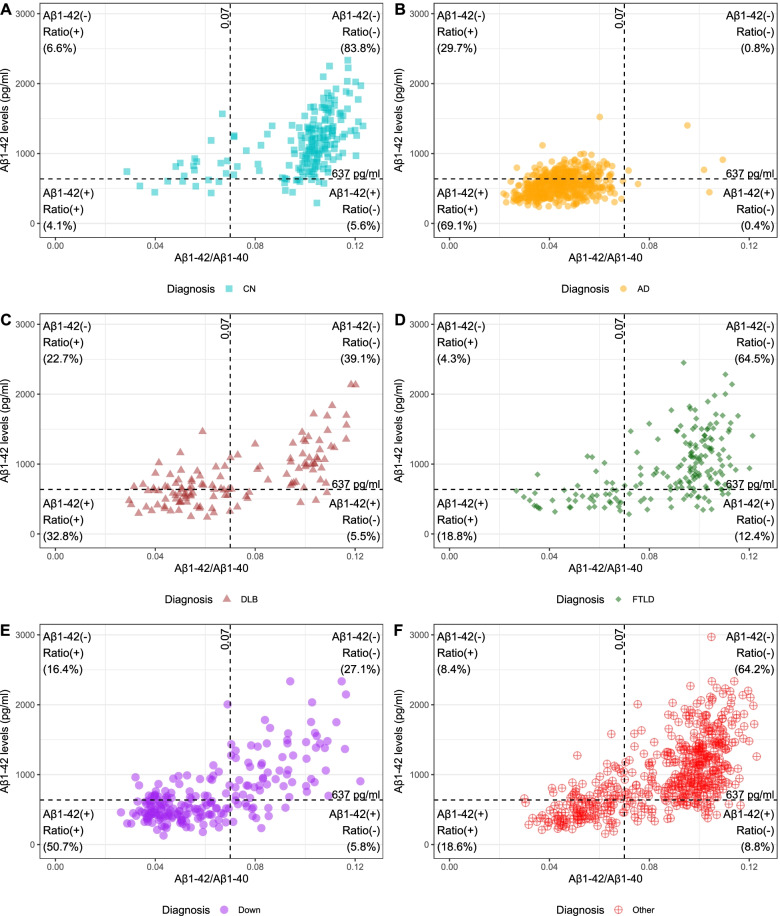
Figure 1 shows the distribution of participants based on their CSF Aβ1–42 and Aβ1–42/Aβ1–40 ratio measures. The correlation between these two parameters was rho = 0.71, p < 0.001. Using Q95% cutoffs as described in the “Material and methods” section, Aβ1–42 and Aβ1–42/Aβ1–40 ratio had an overall agreement of 78.3% in the whole sample, as both measures were normal (Aβ1–42[−]Ratio[−]) in 41.6% and both were abnormal (Aβ1–42[+]Ratio[+]) in 36.7% of participants. Within each diagnostic category, the agreement ranged from 69.9% (AD group) to 87.9% (CN group). More details about the agreement after applying other cutoffs values and with other biomarkers can be found in Additional file 1.
Fig. 1.
Distribution of participants according to CSF levels of Aβ1–42 and amyloid ratio within diagnostic categories. CN, cognitively normal; AD, Alzheimer’s disease; DLB, dementia with Lewy bodies; FTLD, frontotemporal lobar degeneration-related syndrome. Dashed lines indicate 95% quantile values (Q95%) for Aβ1–42 and Aβ1–42/Aβ1–40 in a middle-aged cognitively normal population as described in the “Material and methods” section
Aβ1–42/Aβ1–40 ratio is more strongly associated with tau markers than Aβ1–42
We next studied the association of Aβ1–42 and the Aβ1–42/Aβ1–40 ratio with the other CSF biomarkers by assessing Spearman correlations in the whole sample and within diagnostic groups. In the whole sample, Aβ1–42 showed a significant correlation with tTau (rho = − 0.25, p < 0.001) and pTau181 (rho = − 0.32, p < 0.001). These correlations were stronger for the Aβ1–42/Aβ1–40 ratio (rho = − 0.69 and rho = − 0.75, respectively, both p < 0.001). Both Aβ1–42 and the Aβ1–42/Aβ1–40 ratio showed a similar correlation with NfL (rho = − 0.26 and rho = − 0.32, respectively, both p < 0.001). These stronger associations of Aβ1–42/Aβ1–40 ratio with tTau and pTau181 were observed within all symptomatic diagnostic categories (Additional file 1).
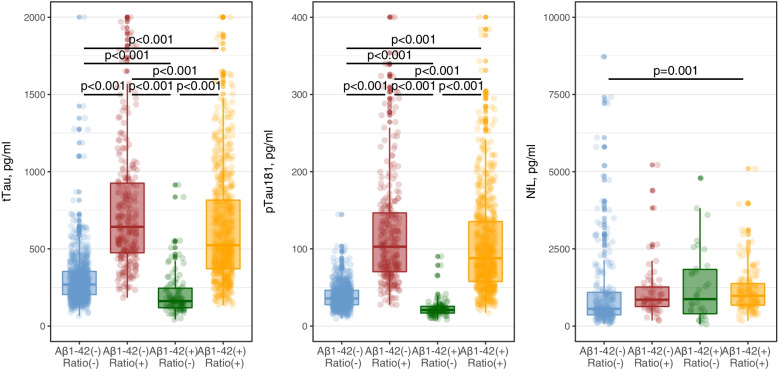
Next, we compared CSF levels of tTau, pTau181 and NfL between all four amyloid profiles. The objective of this analysis was to assess the particularities of those groups where the Aβ1–42 and the Aβ1–42/Aβ1–40 ratio are discordant. As expected, compared to the Aβ1–42[−]Ratio[−] group and after adjusting by age and sex, the Aβ1–42[+]Ratio[+] profile was associated with higher levels of tTau (Tukey post hoc p < 0.001), pTau181 (Tukey post hoc p < 0.001), and NfL (Tukey post hoc p = 0.001). But we also found differences in tTau and pTau181 levels between the two discordant profiles. As seen in Fig. 2, Aβ1–42[−]Ratio[+] participants showed higher levels of tTau (Tukey post hoc p < 0.001) and pTau181 (Tukey post hoc p < 0.001) compared to those with Aβ1–42[+]Ratio[−]. These differences were also observed within all diagnostic categories and in all clinical stages (Additional file 1). These results indicate that reduced levels of the Aβ1–42/Aβ1–40 ratio are associated with high levels of CSF tau markers, regardless of the status of Aβ1–42 alone.
Fig. 2.
Levels of tTau (A), pTau181 (B), and NfL (C) in CSF according to their amyloid profile
Aβ1–42/Aβ1–40 ratio is more strongly associated with cognitive and functional progression than Aβ1–42
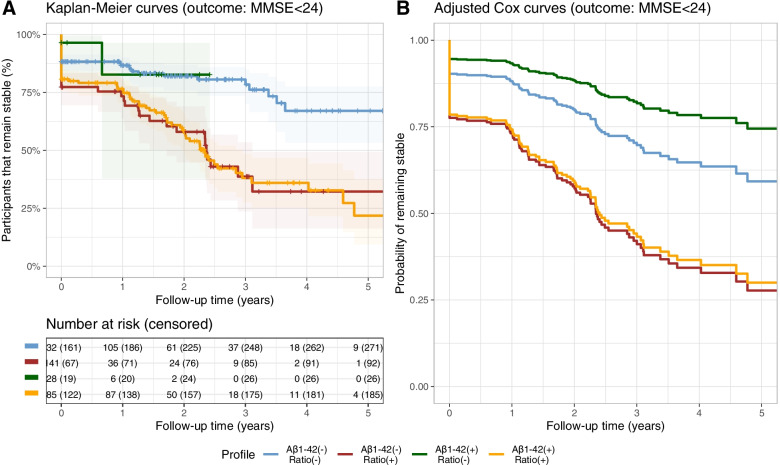
We studied the association of amyloid profiles with cognitive and functional progression in patients with MCI (n = 794) through Kaplan-Meier survival curves and age- and sex-adjusted Cox regression analysis. Supplementary Table 3 describes the characteristics of this subgroup. Due to specific particularities of the clinical and cognitive assessment in the context of intellectual disability, participants with Down syndrome were not included in this analysis. As displayed in Fig. 3, we found that patients with MCI with a low Aβ1–42/Aβ1–40 ratio had worse cognitive outcomes reflected by an earlier decline in MMSE scores. Compared to the Aβ1–42[−]Ratio[−] group, the adjusted risk of presenting a MMSE score lower than 24 during follow-up was 1.77 (1.25–2.49) times higher in the Aβ1–42[−]Ratio[+] group, 1.78 (1.33–2.39) times higher in the Aβ1–42[+]Ratio[+], but not different in the Aβ1–42[+]Ratio[−] group (p = 0.28). Similarly, the adjusted risk of progression to dementia was 1.55 (0.96–2.50) times higher in the Aβ1–42[−]Ratio[+] group and 2.07 (1.43–2.99) times higher in the Aβ1–42[+]Ratio[+] group compared to that of the Aβ1–42[−]Ratio[−]. The adjusted risk of progression to dementia in the Aβ1–42[+]Ratio[−] group was not significantly different from the Aβ1–42[−]Ratio[−] group (p = 0.26).
Fig. 3.
Cognitive progression in patients with mild cognitive impairment according to their amyloid profile. A Kaplan-Meier curve and B age- and sex-adjusted Cox regression display the risk of cognitive progression of all four amyloid profiles (outcome defined as MMSE < 24)
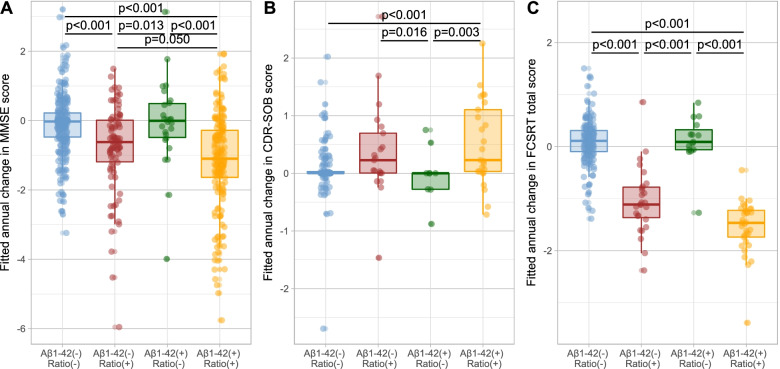
We also fitted linear-mixed models to assess the changes in longitudinal cognitive and functional measures by amyloid profiles. As shown in Fig. 4, after adjusting by baseline MMSE score, baseline age, sex, years of education, pTau181 levels, APOEε4 status and diagnosis, participants with low Aβ1–42/Aβ1–40 ratio presented larger decreases in MMSE scores. The model estimated an annual decrease of − 1.32 (− 1.55 to − 1.09) points when Aβ1–42 was low and of − 0.86 (− 1.18 to − 0.55) points when Aβ1–42 was in the normal range. However, the annual change in MMSE scores in the two groups with normal Aβ1–42/Aβ1–40 ratio was not significantly different from zero. As displayed in Fig. 4, we also found that both groups with low Aβ1–42/Aβ1–40 had larger annual decreases in the FCSRT total score, estimated in − 1.21 in Aβ1–42[−]Ratio[+] and − 1.5 in Aβ1–42[+]Ratio[+], compared to 0.05 in Aβ1–42[−]Ratio[−] and 0.1 in Aβ1–42[+]Ratio[−]. Positivity in the amyloid ratio was also associated to larger annual increases in the cognitive-functional scale CDR-SOB, of 0.46 (0.22–0.71) in Aβ1–42[−]Ratio[+] and 0.65 (0.46-0.85) in Aβ1–42[+]Ratio[+], compared to 0.27 (0.16–0.39) in Aβ1–42[−]Ratio[−] and no significant changes in Aβ1–42[+]Ratio[−].
Fig. 4.
Estimation of the annual change in cognitive and functional scores across amyloid profiles. Estimations of the annual change in MMSE (A), CDR-SOB (B), and FCSRT total score (C) were calculated through linear-mixed models adjusted by baseline MMSE score, baseline age, sex, years of education, pTau181 levels, APOEε4 status, and diagnosis. MMSE, Mini-Mental State Examination; CDR-SOB, Clinical Dementia Rating Sum of Boxes; FCSRT, free and cued selective reminding test
Discussion
The results of our study indicate that, compared to Aβ1–42 alone, the Aβ1–42/Aβ1–40 CSF ratio is more strongly associated with tau markers and with cognitive and functional progression. Regardless of the Aβ1–42 status, participants with low CSF Aβ1–42/Aβ1–40 ratio showed a biochemical and clinical profile characterized by increased levels of CSF tTau and pTau181, worse functional prognosis and larger cognitive decline. Interestingly, when the Aβ1–42/Aβ1–40 ratio was normal, participants with low Aβ1–42 levels had a biochemical and clinical profile similar to that of participants with normal Aβ1–42. Our findings provide evidence suggesting that the use of the Aβ1–42/Aβ1–40 ratio is less confounded by other comorbidities or processes, and thus, this work favors the use of the Aβ1–42/Aβ1–40 ratio as a marker of AD in clinical laboratories and in clinical trials.
The use of CSF Aβ1–42 alone as a marker of amyloid plaques entails some limitations. Numerous studies have reported that low concentrations of Aβ1–42 can be found in some non-AD conditions such as prionopathies, bacterial meningitis, inflammatory diseases, amyloid angiopathy, or frontotemporal dementia [10–14, 39], thus limiting its diagnostic accuracy. Different hypotheses have been suggested to explain these findings. Among other possibilities, low levels of Aβ1–42 in these contexts could be in relation with a decrease in Aβ generation due to neuronal or synaptic loss [10, 15] or the consequence of abnormal clearance through the blood-brain barrier [10]. As Aβ1–40 would be similarly affected by these processes, the use of the Aβ1-42/Aβ1-40 ratio could compensate the reduction in these situations to some extent, thus being less influenced by these processes and reflecting more accurately the presence of amyloid plaques. The stronger association of the Aβ1–42/Aβ1–40 ratio to other AD markers (tau markers) is in line with these hypotheses. Another limitation for the use of Aβ1–42 alone is that it is particularly sensitive to preanalytical and analytical variations, such as changes in the material of collection or storage tubes, number of freeze-thaw cycles, and volume of aliquoted CSF for storage [33, 40, 41]. In our study, we took advantage of a large cohort of subjects with various neurodegenerative and non-neurodegenerative conditions where CSF was collected using the same preanalytical protocol and analyzed under the same standard operating procedures. We found that the overall agreement between Aβ1–42 and the Aβ1–42/Aβ1–40 ratio did not exceed 85% in the whole sample, regardless of the cutoffs definition, suggesting that both markers might be tracking similar but not identical processes or that they are influenced differently by other factors.
We found that CSF concentrations of tTau and pTau181 were higher in the presence of low Aβ1–42/Aβ1–40 ratio, regardless of the Aβ1–42 status. This association was present in the whole sample but also within each diagnostic group. Thus, in the groups of CN, AD, and Down syndrome, less likely affected by non-AD pathology, low Aβ1–42/Aβ1–40 ratio values, but not low Aβ1–42 levels alone, were associated with high concentrations of markers of neurofibrillary pathology and neurodegeneration (pTau181, tTau, and NfL). In other contexts (DLB, FTLD, and other diagnoses), low levels of Aβ1–42 were only associated with markers of neurofibrillary pathology in the presence of reduced Aβ1–42/Aβ1–40 ratio. Our findings indicate that the ratio is more strongly associated to the AD pathophysiological process (both as main and comorbid pathology) and also support the idea that the isolated reduction of Aβ1–42 levels in CSF might reflect additional processes (such as neuronal or synaptic loss) or that the chrono pathology of their changes along the disease is not identical. These results are in line with our previous study showing that the Aβ1–42/Aβ1–40 ratio presents a stronger correlation with cerebral amyloid burden than Aβ1–42 alone [22].
Baseline levels of the Aβ1–42/Aβ1–40 ratio were also influential in the cognitive and functional outcomes of participants in our study. We found that participants with low Aβ1–42/Aβ1–40 ratio had faster cognitive and functional worsening, especially in the group with low Aβ1–42 but also when Aβ1–42 was in the normal range. The group with a low Aβ1–42/Aβ1–40 ratio also presented a more rapid decline in episodic memory measured by the free and cued selective reminding test. These findings support the use of the Aβ1–42/Aβ1–40 ratio over Aβ1–42 alone in the prognostic assessment of patients with cognitive decline.
The major strengths of our study are the large sample size and the inclusion of a variety of diagnoses. Another relevant strength is the fact that the same standard operating procedures were used in the processing and analysis of all samples. Aβ1–42 and Aβ1–40 were measured simultaneously, and we followed the same preanalytical and analytical protocol in all samples, thus minimizing the impact of confounders, which are critical in the case of amyloid-β peptides. Lastly, we replicated our results by using different levels of cutoffs, defined as percentiles from a cognitively normal population. This approach allowed us to match pairs of cutoffs for Aβ1–42 and Aβ1–42/Aβ1–40 ratio that had comparable levels of sensitivity and specificity. But we also acknowledge some limitations.
Limitations of the study
Despite the large sample size, extensive cognitive repeated measures were not available for all participants, thus limiting the statistical power in the longitudinal analysis. On the other hand, amyloid PET imaging was only available in a reduced group of participants previously reported [22].
Conclusions of the study
The present work highlights the importance of routinely measuring Aβ1–40 in the CSF in combination with Aβ1–42 to assess the Aβ1–42/Aβ1–40 ratio, as this measure reflects more accurately the presence of amyloid plaques and is a useful and robust tool for the diagnostic and prognostic evaluation of patients with cognitive decline. The fact that the Aβ1–42/Aβ1–40 ratio shows a stronger association than Aβ1–42 with markers of neurofibrillary pathology and with cognitive and functional decline strengths the utility of this ratio in the clinical context of symptomatic and preclinical AD but also to detect concomitant pathology in other neurodegenerative diseases.
Supplementary Information
Additional file 1. Supplementary tables and figures.
Acknowledgements
We are grateful to all participants in the study and their families. We also thank all the clinical team members that were involved in the selection and assessment of participants in the SPIN cohort and the laboratory teams for sample handling, biomarker analyses, and structural support. We also thank Fujirebio for providing technical support and part of the reagents necessary to complete the study.
Authors’ contributions
DA and AL designed the study. TE, NZ, JA, IB, MC-I, II-G, MAS-S, MA, IS, MBS-S, LV, SV, AS, MT, FB-V, RB, JF, AL, and DA acquired the data relevant for the study. MC-I, II-G, MAS-S, OB, RB, JF, AL, and DA contributed vital reagents/tools/patents. MC-I, II-G, MAS-S, OB, RB, JF, AL, and DA obtained funding for the study. DA and CD performed the statistical analysis. DA, CD, and AL contributed to the analysis and interpretation of the data. DA and AL participated in the study supervision or coordination. CD and DA drafted the first version of the manuscript. The authors read and approved the final manuscript.
Funding
This study was supported by the Fondo de Investigaciones Sanitario (FIS), Instituto de Salud Carlos III (PI14/01126, PI17/01019, and PI20/01473 to JF; PI13/01532 and PI16/01825 to RB; PI18/00335 to MCI; PI18/00435 and INT19/00016 to DA; PI17/01896 and AC19/00103 to AL) and the CIBERNED program (Program 1, Alzheimer Disease to AL), jointly funded by Fondo Europeo de Desarrollo Regional, Unión Europea, “Una manera de hacer Europa.”
This work was also supported by the National Institutes of Health (NIA grants 1R01AG056850-01A1, R21AG056974, and R01AG061566 to JF), by Generalitat de Catalunya (2017-SGR-547 and SLT006/17/125 to DA, SLT006/17/119 to JF, SLT002/16/408 to AL) and “Marató TV3” foundation grants 20141210 to JF, 044412 to RB, and 20142610 to AL. This work was also supported by a grant from the Fundació Bancaria La Caixa to RB (DABNI project). Fundació Catalana Síndrome de Down and Fundació Víctor Grífols i Lucas partly supported this work. The Horizon 21 Consortium is partly funded by Jérôme Lejeune Foundation (Clinical and trial outcome measures for dementia in individuals with Down syndrome).
Part of the reagents necessary to complete the study was funded by Fujirebio-Europe.
The sponsors of the study did not take part in the design and conduct of the study; collection, management, analysis, and interpretation of the data; writing and review of the report; or the decision to submit the article for publication.
Availability of data and materials
Raw anonymized data and code for the statistical analysis are available upon reasonable request. All requests should be sent to the corresponding author detailing the study hypothesis and statistical analysis plan. The steering committee of this study will decide whether data/code sharing is appropriate based on the novelty and scientific rigor of the proposal. All applicants will be asked to sign a data access agreement.
Declarations
Ethics approval and consent to participate
The ethics committee of Hospital Sant Pau approved all procedures included in this study following the standards for medical research in humans recommended by the Declaration of Helsinki. All participants or their legally authorized representatives gave written informed consent before enrolment in the study.
Consent for publication
All authors revised the manuscript for content and provided critical feedback.
Competing interests
Daniel Alcolea is employed by Hospital de la Santa Creu i Sant Pau and received research grants from Pla Estratègic de Recerca i Innovació en Salut (PERIS SLT006/17/125) and from Instituto de Salud Carlos III (PI18/00435 and INT19/00016). He participated in the advisory boards from Fujirebio-Europe and Roche Diagnostics and received speaker honoraria from Fujirebio-Europe, Roche Diagnostics, Nutricia, Zambon S.A.U., Esteve, and from Krka Farmacéutica S.L.
Constance Delaby is employed by Université de Montpellier and CHU de Montpellier. Declarations of interest: none
Teresa Estellés is employed by Biomedical Research Institute Sant Pau. Declarations of interest: none
Nuole Zhu is employed by Hospital de la Santa Creu i Sant Pau. Declarations of interest: none
Javier Arranz is employed by Biomedical Research Institute Sant Pau. Declarations of interest: none
Isabel Barroeta is employed by Hospital de la Santa Creu i Sant Pau. Declarations of interest: none
María Carmona-Iragui is employed by Hospital de la Santa Creu i Sant Pau. Declarations of interest: none
Ignacio Illán-Gala is supported by the Global Brain Health Institute (Atlantic Fellow for Equity in Brain Health and pilot award for global brain health leaders GBHI ALZ UK-21-720973) and the “Juan Rodés” grant from the Institute of Health Carlos III (JR20/00018).
Miguel Santos-Santos is employed by Hospital de la Santa Creu i Sant Pau. He is funded by a “Juan Rodés” research grant from the Institute of Health Carlos III.
Miren Altuna is employed by Biomedical Research Institute Sant Pau. Dr. Altuna is funded by a “Río Hortega” research grant from the Institute of Health Carlos III.
Isabel Sala is employed by Hospital de la Santa Creu i Sant Pau. Declarations of interest: none
M. Belén Sánchez-Saudinós is employed by Biomedical Research Institute Sant Pau. Declarations of interest: none
Laura Videla is employed by Fundació Catalana Síndrome de Down. Declarations of interest: none
Sílvia Valldeneu is employed by Biomedical Research Institute Sant Pau. Declarations of interest: none
Andrea Subirana is employed by Biomedical Research Institute Sant Pau. Declarations of interest: none
Mireia Tondo is employed by Hospital de la Santa Creu i Sant Pau. Declarations of interest: none
Francisco Blanco-Vaca is employed by Hospital de la Santa Creu i Sant Pau. Declarations of interest: none.
Sylvain Lehmann is employed by the University and the Hospital of Montpellier. He participated in advisory boards from Fujirebio-Europe and Roche.
Olivia Belbin is employed by Biomedical Research Institute Sant Pau. Dr. Belbin is funded by a “Miguel Servet” research grant from the Institute of Health Carlos III.
Rafael Blesa is employed by Hospital de la Santa Creu i Sant Pau and received research grants from Institute of Health Carlos III, Fundació Bancària Obra Social La Caixa, and Fundació La Marató de TV3. He participated in the advisory boards from Lilly and Nutricia, and he received speaker honoraria and travel funding from Novartis and Nutricia.
Juan Fortea is employed by Hospital de la Santa Creu i Sant Pau and received research grants from Institute of Health Carlos III, National Institutes of Health, Fundació La Marató de TV3, and Pla Estratègic de Recerca i Innovació en Salut (PERIS). Dr. Fortea has served as a consultant for Novartis and Lundbeck; has received honoraria for lectures from Roche, NovoNordisk, Esteve, and Biogen; and served at advisory boards for AC Immune, Zambon, and Lundbeck.
Alberto Lleó is employed by Hospital de la Santa Creu i Sant Pau and received research grants from CIBERNED, Institute of Health Carlos III, Generalitat de Catalunya (PERIS and AGAUR), and Fundación BBVA. He participated in the advisory boards from Fujirebio-Europe, Novartis, Roche Diagnostics, Otsuka Pharmaceutical, Nutricia, Zambón S.A.U., and Biogen and received speaker honoraria from Lilly, Biogen, KRKA, and Zambon.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Scheltens P, De Strooper B, Kivipelto M, Holstege H, Chételat G, Teunissen CE, et al. Alzheimer’s disease. Lancet. 2021;397(10284):1577–90. [DOI] [PMC free article] [PubMed]
- 2.Olsson B, Lautner R, Andreasson U, Öhrfelt A, Portelius E, Bjerke M, et al. CSF and blood biomarkers for the diagnosis of Alzheimer’s disease: a systematic review and meta-analysis. Lancet Neurol. 2016;4422:1–12. doi: 10.1016/S1474-4422(16)00070-3. [DOI] [PubMed] [Google Scholar]
- 3.Fagan AM, Roe CM, Xiong C, Mintun MA, Morris JC, Holtzman DM. Cerebrospinal fluid tau/β-amyloid42 ratio as a prediction of cognitive decline in nondemented older adults. Arch Neurol. 2007;64:343–349. doi: 10.1001/archneur.64.3.noc60123. [DOI] [PubMed] [Google Scholar]
- 4.Gabelle A, Dumurgier J, Vercruysse O, Paquet C, Bombois S, Laplanche JL, et al. Impact of the 2008-2012 french Alzheimer plan on the use of cerebrospinal fluid biomarkers in research memory center: the PLM study. J Alzheimers Dis. 2013;34:297–305. doi: 10.3233/JAD-121549. [DOI] [PubMed] [Google Scholar]
- 5.Dubois B, Feldman HH, Jacova C, Hampel H, Molinuevo JL, Blennow K, et al. Advancing research diagnostic criteria for Alzheimer’s disease: the IWG-2 criteria. Lancet Neurol. 2014;13:614–629. doi: 10.1016/S1474-4422(14)70090-0. [DOI] [PubMed] [Google Scholar]
- 6.McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR, Kawas CH, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:263–269. doi: 10.1016/j.jalz.2011.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dubois B, Villain N, Frisoni GB, Rabinovici GD, Sabbagh M, Cappa S, et al. Clinical diagnosis of Alzheimer’s disease: recommendations of the International Working Group. Lancet Neurol. 2021;20:484–496. doi: 10.1016/S1474-4422(21)00066-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lleó A, Cavedo E, Parnetti L, Vanderstichele H, Herukka SK, Andreasen N, et al. Cerebrospinal fluid biomarkers in trials for Alzheimer and Parkinson diseases. Nat Rev Neurol. 2015;11:41–55. doi: 10.1038/nrneurol.2014.232. [DOI] [PubMed] [Google Scholar]
- 9.Jack CR, Bennett DA, Blennow K, Carrillo MC, Dunn B, Haeberlein SB, et al. NIA-AA research framework: toward a biological definition of Alzheimer’s disease. Alzheimer’s Dement. 2018;14:535–562. doi: 10.1016/j.jalz.2018.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lewczuk P, Riederer P, O’Bryant SE, Verbeek MM, Dubois B, Visser PJ, et al. Cerebrospinal fluid and blood biomarkers for neurodegenerative dementias: an update of the Consensus of the Task Force on Biological Markers in Psychiatry of the World Federation of Societies of Biological Psychiatry. World J Biol Psychiatry. 2018;19:244–328. doi: 10.1080/15622975.2017.1375556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Iadanza MG, Jackson MP, Hewitt EW, Ranson NA, Radford SE. A new era for understanding amyloid structures and disease. Nat Rev Mol Cell Biol. 2018;19(12):755–73. [DOI] [PMC free article] [PubMed]
- 12.Frost B, Diamond MI. Prion-like mechanisms in neurodegenerative diseases. Nat Rev Neurosci. 2010;11:155–159. doi: 10.1038/nrn2786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Spies PE, Slats D, Sjögren JMC, Kremer BPH, Verhey FRJ, Rikkert MGMO, et al. The cerebrospinal fluid amyloid beta42/40 ratio in the differentiation of Alzheimer’s disease from non-Alzheimer’s dementia. Curr Alzheimer Res. 2010;7:470–476. doi: 10.2174/156720510791383796. [DOI] [PubMed] [Google Scholar]
- 14.Llorens F, Schmitz M, Karch A, Cramm M, Lange P, Gherib K, et al. Comparative analysis of cerebrospinal fluid biomarkers in the differential diagnosis of neurodegenerative dementia. Alzheimers Dement. 2016;12:577–589. doi: 10.1016/j.jalz.2015.10.009. [DOI] [PubMed] [Google Scholar]
- 15.Spies PE, Verbeek MM, van Groen T, Claassen JAHR. Reviewing reasons for the decreased CSF Abeta42 concentration in Alzheimer disease. Front Biosci (Landmark Ed) 2012;17:2024–2034. doi: 10.2741/4035. [DOI] [PubMed] [Google Scholar]
- 16.Lehmann S, Delaby C, Boursier G, Catteau C, Ginestet N, Tiers L, et al. Relevance of Aβ42/40 ratio for detection of Alzheimer disease pathology in clinical routine: the PLMR Scale. Front Aging Neurosci. 2018;10:138. doi: 10.3389/fnagi.2018.00138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hansson O, Lehmann S, Otto M, Zetterberg H, Lewczuk P. Advantages and disadvantages of the use of the CSF amyloid β (Aβ) 42/40 ratio in the diagnosis of Alzheimer’s disease. Alzheimers Res Ther. 2019;11:34. doi: 10.1186/s13195-019-0485-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cullen NC, Leuzy A, Janelidze S, Palmqvist S, Svenningsson AL, Stomrud E, et al. Plasma biomarkers of Alzheimer’s disease improve prediction of cognitive decline in cognitively unimpaired elderly populations. Nat Commun. 2021;12:3555. doi: 10.1038/s41467-021-23746-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alcolea D, Delaby C, Muñoz L, Torres S, Estellés T, Zhu N, et al. Use of plasma biomarkers for AT(N) classification of neurodegenerative dementias. J Neurol Neurosurg Psychiatry. 2021;92(11):1206–14. [DOI] [PubMed]
- 20.Doecke JD, Pérez-Grijalba V, Fandos N, Fowler C, Villemagne VL, Masters CL, et al. Total Aβ42/Aβ40 ratio in plasma predicts amyloid-PET status, independent of clinical AD diagnosis. Neurology. 2020;94:E1580–E1591. doi: 10.1212/WNL.0000000000009240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nakamura A, Kaneko N, Villemagne VL, Kato T, Doecke J, Doré V, et al. High performance plasma amyloid-β biomarkers for Alzheimer’s disease. Nature. 2018;554:249–254. doi: 10.1038/nature25456. [DOI] [PubMed] [Google Scholar]
- 22.Alcolea D, Pegueroles J, Muñoz L, Camacho V, López-Mora D, Fernández-León A, et al. Agreement of amyloid PET and CSF biomarkers for Alzheimer’s disease on Lumipulse. Ann Clin Transl Neurol. 2019;6(9):1815–24. [DOI] [PMC free article] [PubMed]
- 23.Alcolea D, Clarimón J, Carmona-Iragui M, Illán-Gala I, Morenas-Rodríguez E, Barroeta I, et al. The Sant Pau Initiative on Neurodegeneration (SPIN) cohort: a data set for biomarker discovery and validation in neurodegenerative disorders. Alzheimer’s Dement Transl Res Clin Interv. 2019;5:597–609. doi: 10.1016/j.trci.2019.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alcolea D, Vilaplana E, Suárez-Calvet M, Illán-Gala I, Blesa R, Clarimón J, et al. CSF sAPPβ, YKL-40, and neurofilament light in frontotemporal lobar degeneration. Neurology. 2017;89:178–188. doi: 10.1212/WNL.0000000000004088. [DOI] [PubMed] [Google Scholar]
- 25.Illán-Gala I, Pegueroles J, Montal V, Alcolea D, Vilaplana E, Bejanin A, et al. APP-derived peptides reflect neurodegeneration in frontotemporal dementia. Ann Clin Transl Neurol. 2019;6:2518–2530. doi: 10.1002/acn3.50948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McKeith IG, Boeve BF, Dickson DW, Halliday G, Taylor J-PP, Weintraub D, et al. Diagnosis and management of dementia with Lewy bodies. Neurology. 2017;89:88–100. doi: 10.1212/WNL.0000000000004058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Strong MJ, Abrahams S, Goldstein LH, Woolley S, Mclaughlin P, Snowden J, et al. Amyotrophic lateral sclerosis - frontotemporal spectrum disorder (ALS-FTSD): revised diagnostic criteria. Amyotroph Lateral Scler Front Degener. 2017;18:153–174. doi: 10.1080/21678421.2016.1267768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:270–279. doi: 10.1016/j.jalz.2011.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fortea J, Carmona-Iragui M, Benejam B, Fernández S, Videla L, Barroeta I, et al. Plasma and CSF biomarkers for the diagnosis of Alzheimer’s disease in adults with Down syndrome: a cross-sectional study. Lancet Neurol. 2018;17:860–869. doi: 10.1016/S1474-4422(18)30285-0. [DOI] [PubMed] [Google Scholar]
- 30.Fortea J, Vilaplana E, Carmona-Iragui M, Benejam B, Videla L, Barroeta I, et al. Clinical and biomarker changes of Alzheimer’s disease in adults with Down syndrome: a cross-sectional study. Lancet. 2020;395:1988–1997. doi: 10.1016/S0140-6736(20)30689-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sala I, Illán-Gala I, Alcolea D, Sánchez-Saudinós MBMB, Salgado SASA, Morenas-Rodríguez E, et al. Diagnostic and prognostic value of the combination of two measures of verbal memory in mild cognitive impairment due to Alzheimer’s disease. J Alzheimers Dis. 2017;58:909–918. doi: 10.3233/JAD-170073. [DOI] [PubMed] [Google Scholar]
- 32.Alcolea D, Martínez-Lage P, Izagirre A, Clerigué M, Carmona-Iragui M, Alvarez RMRM, et al. Feasibility of lumbar puncture in the study of cerebrospinal fluid biomarkers for Alzheimer’s disease: a multicenter study in Spain. J Alzheimers Dis. 2014;39:719–726. doi: 10.3233/JAD-131334. [DOI] [PubMed] [Google Scholar]
- 33.del Campo M, Mollenhauer B, Bertolotto A, Engelborghs S, Hampel H, Simonsen AH, et al. Recommendations to standardize preanalytical confounding factors in Alzheimer’s and Parkinson’s disease cerebrospinal fluid biomarkers: an update. Biomark Med. 2012;6:419–430. doi: 10.2217/bmm.12.46. [DOI] [PubMed] [Google Scholar]
- 34.Delaby C, Muñoz L, Torres S, Nadal A, Le Bastard N, Lehmann S, et al. Impact of CSF storage volume on the analysis of Alzheimer’s disease biomarkers on an automated platform. Clin Chim Acta Elsevier. 2019;490:98–101. doi: 10.1016/j.cca.2018.12.021. [DOI] [PubMed] [Google Scholar]
- 35.Global Biomarker Standardization Consortium (GBSC) | Alzheimer’s Association [Internet]. [cited 2021 Dec 27]. Available from: https://www.alz.org/research/for_researchers/partnerships/gbsc
- 36.Carrillo MC, Blennow K, Soares H, Lewczuk P, Mattsson N, Oberoi P, et al. Global standardization measurement of cerebral spinal fluid for Alzheimer’s disease: an update from the Alzheimer’s Association Global Biomarkers Consortium. Alzheimers Dement. 2013;9:137–140. doi: 10.1016/j.jalz.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 37.Mattsson N, Andreasson U, Persson S, Carrillo MC, Collins S, Chalbot S, et al. CSF biomarker variability in the Alzheimer’s Association quality control program. Alzheimers Dement. 2013;9:251–261. doi: 10.1016/j.jalz.2013.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Carmona-Iragui M, Balasa M, Benejam B, Alcolea D, Fernández S, Videla L, et al. Cerebral amyloid angiopathy in Down syndrome and sporadic and autosomal-dominant Alzheimer’s disease. Alzheimers Dement. 2017;13:1251–1260. doi: 10.1016/j.jalz.2017.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Strydom A, Coppus A, Blesa R, Danek A, Fortea J, Hardy J, et al. Alzheimer’s disease in Down syndrome: an overlooked population for prevention trials. Alzheimer’s Dement Transl Res Clin Interv. Elsevier Inc. 2018;4:703–713. doi: 10.1016/j.trci.2018.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Perret-Liaudet A, Pelpel M, Tholance Y, Dumont B, Vanderstichele H, Zorzi W, et al. Risk of Alzheimer’s disease biological misdiagnosis linked to cerebrospinal collection tubes. J Alzheimers Dis. 2012;31:13–20. doi: 10.3233/JAD-2012-120361. [DOI] [PubMed] [Google Scholar]
- 41.Lehmann S, Schraen S, Quadrio I, Paquet C, Bombois S, Delaby C, et al. Impact of harmonization o tubes on Alzheimer’s disease diagnosis. Alzheimers Dement. 2014;10:S390–S394.e2. doi: 10.1016/j.jalz.2013.06.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Supplementary tables and figures.
Data Availability Statement
Raw anonymized data and code for the statistical analysis are available upon reasonable request. All requests should be sent to the corresponding author detailing the study hypothesis and statistical analysis plan. The steering committee of this study will decide whether data/code sharing is appropriate based on the novelty and scientific rigor of the proposal. All applicants will be asked to sign a data access agreement.