Introduction
Hemodialysis therapy was first performed in Japan at United States military base hospitals during the Korean War (1950–1953) to treat injured American soldiers with crush syndrome transferred from the combat zone. Encouraged by such experiences, several university hospitals started to offer acute hemodialysis treatment in 1955 and chronic hemodialysis treatment in the early 1960s. The health insurance program started to cover chronic hemodialysis treatment in 1967. Initially, the costs were not fully covered by the program: a 30% to even 50% copayment was required for patients who were not beneficiaries of the public insurance plan. In 1972, the national government started a program that also covered copayment on the basis of the Basic Act for Persons with Disabilities as a result of lobbying activities by patient groups and academic societies. Since then, hemodialysis treatment has become almost free of charge, except for high-income patients (up to 20,000 Japanese Yen [JPY] or approximately United States $200 per month).
A History of Dialysis Therapy and the Reimbursement System in Japan
Typically, the total monthly cost for a patient on maintenance dialysis is approximately 320,000 JPY or approximately United States $3000, excluding any additional fees or medications. The cost consists of the medical management fee, including routine laboratory tests (22,500 JPY per month), and technical fees (21,400 JPY × approximately 14/mo). The reimbursement system is updated every 2 years. In April 2006, the costs for erythropoiesis-stimulating agents were bundled with the technical fees of hemodialysis and with anticoagulant and normal saline for rinsing. Roxadustat has recently been approved and bundled.
Current Status of Dialysis Therapy in Japan
According to the recent annual report of the Japanese Society for Dialysis Therapy Renal Data Registry (JRDR) (1), a total of 334,505 patients (2640.0 per million people in the general population) are receiving dialysis treatment in Japan as of 2017. In 40,959 incident patients (323 per million people in the general population), the average eGFR at the start of dialysis therapy was 5.43±3.43 ml/min per 1.73 m2 (2). As detailed in Tables 1 and 2 (1), most of the patients are treated with hemodialysis, and only a few (2.7%) are treated with peritoneal dialysis. Reasons for such low numbers of patients on peritoneal dialysis may include concerns about encapsulating peritoneal sclerosis, longer dialysis vintage, and easy access to hemodialysis facilities. (According to the Global Kidney Health Atlas of the International Society of Nephrology, the number of facilities per patient is the highest in Japan.) Recently, the population receiving online hemodiafiltration, especially the predilution method, has remarkably increased because all patients became potentially eligible for therapy in 2012 as long as the water purity of the facility meets the standard set by the Japanese Society for Dialysis Therapy (JSDT). The number of patients on home hemodialysis therapy is still limited (684 as of 2017) but is gradually increasing (1).
Table 1.
Summary of dialysis therapy in Japan as of 2017 (summarized from ref. 1)
| Modalities | No. (%) |
| Prevalence | |
| Hemodialysis | 228,089 (68.2) |
| Hemodiafiltration | 95,140 (28.4) |
| Other blood purification types | 1502 (0.4) |
| Home hemodialysis | 684 (0.2) |
| Peritoneal dialysis | 9090 (2.7) |
| Total | 334,505 (2640.0 per million people in the general population) |
| Incidence | |
| Hemodialysis | 38,842 (94.8) |
| Peritoneal dialysis | 2117 (5.2) |
| Total | 40,959 (323 per million people in the general population) |
| Deceased patients | 32,532 |
Table 2.
Summary of dialysis therapy in Japan as of 2017 (summarized from ref. 1)
| Patient Backgrounds | Prevalent Patients | Incident Patients |
| Age, yr | 68.4±12.5 | 69.7±13.4 |
| Sex, men/women | 208,870 (65.0%)/112,648 (35.0%) | 26,677 (68.8%)/12,109 (31.2%) |
| Diabetes as the primary diagnosis of ESKD | 125,247 (39.0%) | 16,492 (42.5%) |
The dialysis unit team in Japan is usually composed of several health care professionals, such as doctors, clinical engineers (CEs), nurses, pharmacists, dieticians, social workers, and physical therapists. The doctors are typically physicians (including board-certified nephrologists endorsed by the Japanese Society of Nephrology), surgeons, or urologists. Among them, 6000 are also qualified as fellows of the JSDT.
CEs specializing in the operation and maintenance of life-supporting devices or machines used for RRT have been endorsed by national licenses on the basis of the Clinical Engineers Act since 1987. Twenty-three thousand CEs had jobs in dialysis facilities as of 2016 (2). They not only support the maintenance and performance of dialysis machines but are also highly responsible for maintaining dialysate quality, including water purity. This is quite important because dialysis fluid is delivered from a central system in most facilities in Japan, except for a few patients who need special prescriptions. For the nursing care of patients on dialysis, a total of 43,000 registered nurses were involved in dialysis therapy as of 2016 (2) (i.e., 1 nurse for every eight patients). The Japanese Nursing Association accredits the title of certified nurse to leaders in the field of dialysis nursing, but only approximately 300 nurses have been accredited.
In Japan, a total of 4413 facilities were providing dialysis treatment as of 2017 (1). There are many groups of facilities, usually owned by private health care corporations. However, the size of each group is usually small with several facilities, except for very few with several thousand patients. According to a JRDR report, 1.2%, 19.4%, 1.7%, 30.3%, and 47.4% of the total facilities were national university hospitals, public hospitals, private university hospitals, private hospitals, and private clinics, respectively (2). Because the Medical Care Act of Japan prohibits paying any dividend to shareholders, all medical corporations in Japan are technically nonprofit organizations.
Practice Pattern and Prognosis of Japanese Patients on Dialysis
The survival of Japanese patients on dialysis is reportedly one of the best in the world (3). The survival of the entire Japanese dialysis population may be superior to that of healthier patients on the waiting list in the United States. The JRDR in 2007 demonstrated that patients aged 60–74 years old had a crude 5-year mortality rate of 40.7%, whereas patients aged 60–64 years old who were on the waiting list between 1995 and 2007 experienced a 5-year mortality rate of 49% in the United States (4). These data suggest that the survival advantage of Japanese patients may not be due to the lower incidence of kidney transplantation. Many attempts have been made to elucidate the reasons for the longevity of Japanese patients on dialysis, including the Dialysis Outcomes and Practice Patterns Study (DOPPS). It has been reported that several clinical practice patterns in Japan are different from those in other countries (Table 3).
Table 3.
Characteristics of clinical practice patterns in Japanese dialysis therapy
| Factors | Values |
| eGFR at the start of dialysis therapy | 5.43±3.43 ml/min per 1.73 m2 (2) |
| Percentage of home dialysis | 2.9% (9774; 9090 on PD and 684 on HHD) (1) |
| Insurance coverage | Almost 100% (out-of-pocket payment of up to 20,000 JPY for the high-income patients) |
| Hospital affiliated or free standing | Hospital affiliated 52.6%; free standing 47.4% (2) |
| For profit/nonprofit | Entirely nonprofit; the national government does not allow for-profit medical facilities in Japan |
| Basic cost to be reimbursed for a single hemodialysis session | Approximately United States $200 |
| Professionals managing patients | Doctors and government-licensed clinical engineers as well as registered nurses |
| Patient-nurse ratio | 7.8 patients per nurse (2) |
| Length of session, mean ± SD (min) | 239.3±32.9 (2) |
| Times of nephrologist consultation | Every session: dialysis therapy without consultation with a doctor is prohibited by the law |
| Types of vascular access | AVF 89.0%, AVG 7.3%, CVC (both temporary and cuffed) 1.8%, superficialized artery 1.8%, others 0.1% (1) |
| Blood flow rate, ml/min | 206.5±36.5 (lower) (1) |
| Kt/V | 1.51±0.30 (lower) (1) |
| Bicarbonate levels in dialysis fluid, meq/L | 25–30 for acetate-containing DF, 35 for acetate-free DF (lower) |
| ESA use, kU/wk | 6±5 (lower) (4) |
| Iron use | 33% (lower) (4) |
| Iron dose among treated, mg/wk | 32±21 (lower) (4) |
| Serum ferritin level, ng/ml | 145±205 (lower) (4) |
| Inflammation status, mg/L, median (IQR) | 1 (1–3) (lower) (4) |
| ESA responsiveness | Higher (ESA dose is much smaller, whereas hemoglobin of 10.7 g/dl is almost equivalent or slightly lower [4]) |
| PTH target, pg/ml | 60–240 (lower) (6,8) |
| Adherence of the patients to therapies (represented by the proportion of missed treatment; in the text) | Higher (0.4% in Japan, whereas 24% in the United States [10]) |
The factors potentially related to the better clinical outcome of Japanese patients on dialysis are listed. PD, peritoneal dialysis; HHD, home hemodialysis; JPY, Japanese Yen; AVF, arteriovenous fistula; AVG, arteriovenous graft; CVC, cental venous catheter; DF, dialysis fluid; ESA, erythropoiesis-stimulating agent; IQR, interquartile range; PTH, parathyroid hormone.
The causes of death are different between Japan and other countries, partly due to the definitions. The Annual Data Report of the US Renal Data System in 2017 delineates that the leading cause of death was arrhythmia or cardiac arrest (40%) followed by withdrawal (18%) and septicemia (8%). Congestive heart failure comprised only 3% of the total deaths. In contrast, the most prevalent cause in Japan is congestive heart failure (24.0%) followed by infection (21.1%) and malignancy (9.0%). Withholding or foregoing dialysis therapy is rare in Japan compared with in the United States, but it is currently under detailed discussion.
Another striking difference in clinical practice is the proportions of vascular access used for hemodialysis. Almost all vascular access is arteriovenous fistula with native veins; 89.0%, 7.3%, and 1.4% of the patients had arteriovenous fistula, arteriovenous graft, and tunneled catheter procedures, respectively (1). In addition, elevated or superficialized brachial arteries are occasionally (1.8%) used in patients with reduced cardiac function. Regarding the dialysis prescription, the blood flow rate is lower in Japanese patients than in patients in other countries, which might be a reflection of the smaller body size of the Japanese dialysis population. The dialysis duration is 239±33 minutes per session on average (2).
Anemia management in Japan is also different from that in other countries. The hemoglobin level was lower in the early 2000s (10.2±1.4 and 10.9±1.3 g/dl in 2005 and 2017, respectively), probably due to a limitation on epoetin for use in patients on dialysis (up to 9000 U/wk). Even after erythropoiesis-stimulating agents with longer half-lives have become available in higher doses than epoetin, the doses are still kept low in Japan. This trend might be explained by the fact that erythropoiesis-stimulating agent responsiveness has been reported to be higher in Japan than in other DOPPS countries (5). Furthermore, as proposed by the JSDT guidelines (6), the target level of parathyroid hormone is also kept lower at 60–240 pg/ml than that recommended by other guidelines. Accordingly, the median parathyroid hormone level was 126 pg/ml, much lower than that in Europe (233 pg/ml) or North America (283 pg/ml) (7). The reasons may include racial differences in skeletal resistance to parathyroid hormone, drug availability, and the health care system; however, these explanations still remain to be elucidated (8).
The law, namely the Medical Practitioners’ Act of Japan, prohibits the provision of treatment without examination by any doctor. Therefore, every patient must legally be seen by a doctor at every dialysis session, although not necessarily by a full-time nephrologist; part-time nephrologists or doctors with various backgrounds, including surgeons, are also acceptable. Although each patient is seen by a doctor for just 5 minutes (9), this consultation might be a reason for the better clinical outcomes of Japanese patients on dialysis. Additionally, the adherence of the patients is higher in Japan; only 0.4% of patients skipped one or more sessions over 4 months according to the DOPPS data, whereas 24% of patients skipped sessions in the United States (10).
Future Perspectives
Many factors can account for the better prognosis of Japanese patients on dialysis, including more intensive care and the broader coverage of drugs by the health insurance system. Nevertheless, the number of patients on dialysis continues to increase, especially older diabetic patients with lower physical activity (Figure 1, Table 2). The expansion of this older population in Japan can also lead to an increase in the number of frail people in terms of physical, mental, cognitive, and social functioning. Moreover, there will be fewer health care workers caring for such patients with multiple comorbidities.
Figure 1.
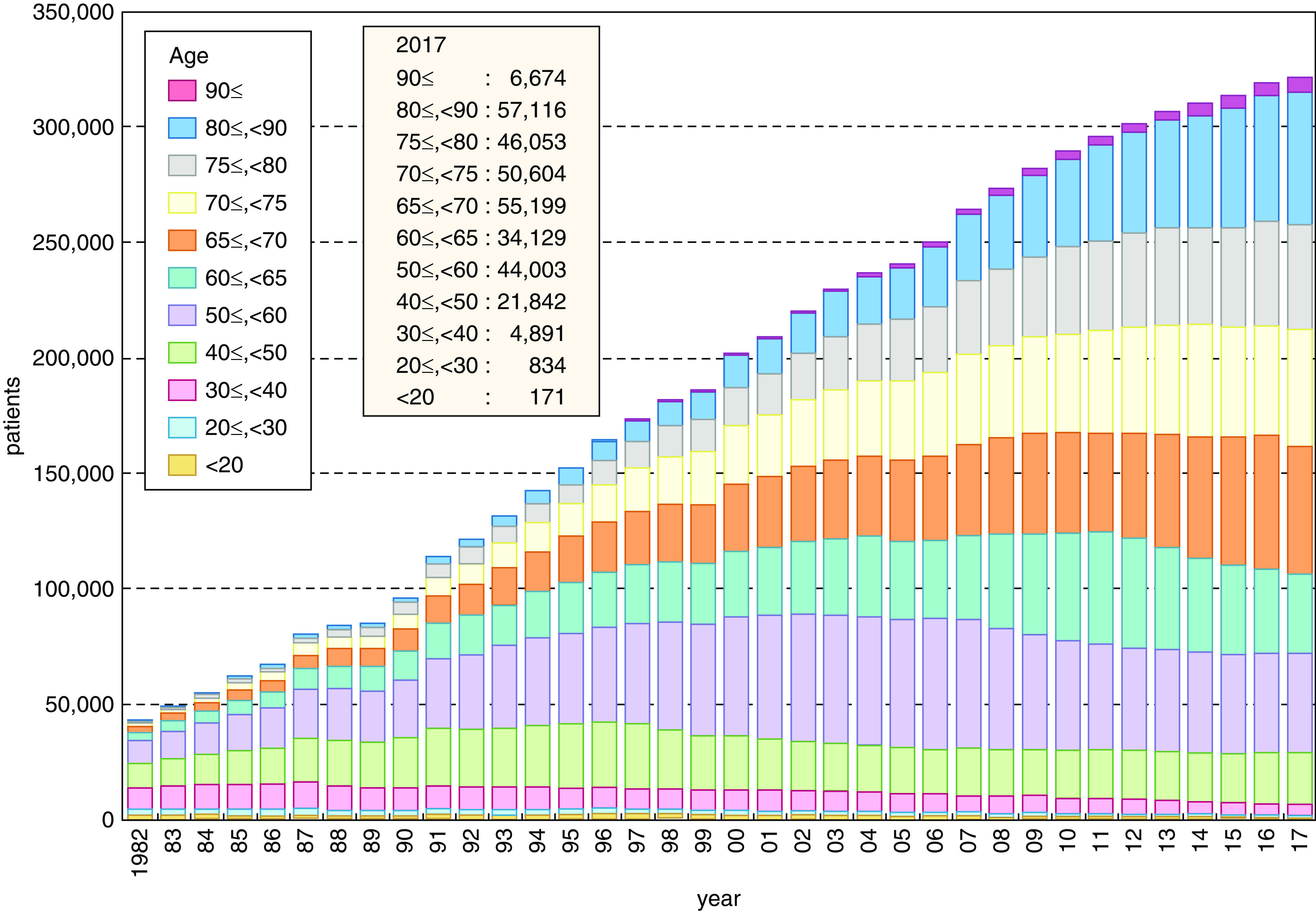
The trend of patients on prevalent dialysis by age. Reprinted from ref. 1, which is available under the terms of the Creative Commons Attribution License 4.0.
According to the estimates of national medical care expenditure by the Ministry of Health, Labor, and Welfare, Japan, the total cost of hemodialysis therapy currently accounts for 5% of the total medical expenditure in Japan. Thus, it is mandatory for Japanese society to find a solution to these issues for sustainability. The increase in the number of peritoneal dialysis procedures (1) and kidney transplants (still fewer than 2000/yr and nearly 90% from living donors) (11) might be one of the keys.
Disclosures
M. Fukagawa received grants and personal fees from Kyowa Kirin Co. Ltd. and personal fees from Bayer Yakuhin, Ltd., and grants and personal fees from Ono Pharmacentical, outside the submitted work. N. Hanafusa received lecture fees from Kyowa Kirin Co., Ltd. and Bayer Yakuhin, Ltd., outside the submitted work.
Funding
None.
Author Contributions
M. Fukagawa and N. Hanafusa conceptualized the study, wrote the original draft, and reviewed and edited the manuscript.
References
- 1.Nitta K, Masakane I, Hanafusa N, Taniguchi M, Hasegawa T, Nakai S, Goto S, Wada A, Hamano T, Hoshino J, Joki N, Abe M, Yamamoto K, Nakamoto H: Annual dialysis data report 2017, JSDT renal data registry. Ren Replace Ther 5: 53, 2019 [Google Scholar]
- 2.The Japanese Society for Dialysis Therapy : An overview of regular dialysis treatment in Japan. Available at: https://www.jsdt.or.jp/english/2426.html. Accessed April 24, 2020
- 3.Goodkin DA, Bragg-Gresham JL, Koenig KG, Wolfe RA, Akiba T, Andreucci VE, Saito A, Rayner HC, Kurokawa K, Port FK, Held PJ, Young EW: Association of comorbid conditions and mortality in hemodialysis patients in Europe, Japan, and the United States: The Dialysis Outcomes and Practice Patterns Study (DOPPS). J Am Soc Nephrol 14: 3270–3277, 2003 [DOI] [PubMed] [Google Scholar]
- 4.Schold J, Srinivas TR, Sehgal AR, Meier-Kriesche HU: Half of kidney transplant candidates who are older than 60 years now placed on the waiting list will die before receiving a deceased-donor transplant. Clin J Am Soc Nephrol 4: 1239–1245, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Karaboyas A, Morgenstern H, Pisoni RL, Zee J, Vanholder R, Jacobson SH, Inaba M, Loram LC, Port FK, Robinson BM: Association between serum ferritin and mortality: Findings from the USA, Japan and European dialysis outcomes and practice patterns Study. Nephrol Dial Transplant 33: 2234–2244, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fukagawa M, Yokoyama K, Koiwa F, Taniguchi M, Shoji T, Kazama JJ, Komaba H, Ando R, Kakuta T, Fujii H, Nakayama M, Shibagaki Y, Fukumoto S, Fujii N, Hattori M, Ashida A, Iseki K, Shigematsu T, Tsukamoto Y, Tsubakihara Y, Tomo T, Hirakata H, Akizawa T; CKD-MBD Guideline Working GroupJapanese Society for Dialysis Therapy: Clinical practice guideline for the management of chronic kidney disease-mineral and bone disorder. Ther Apher Dial 17: 247–288, 2013 [DOI] [PubMed] [Google Scholar]
- 7.Yamamoto S, Karaboyas A, Komaba H, Taniguchi M, Nomura T, Bieber BA, De Sequera P, Christensson A, Pisoni RL, Robinson BM, Fukagawa M: Mineral and bone disorder management in hemodialysis patients: Comparing PTH control practices in Japan with Europe and North America: The Dialysis Outcomes and Practice Patterns Study (DOPPS). BMC Nephrol 19: 253, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang AY-M, Akizawa T, Bavanandan S, Hamano T, Liew A, Lu K-C, Lumlertgul D, Oh K-H, Zhao M-H, Ka-Shun Fung S, Obi Y, Sumida K, Choong LHL, Goh BL, Hao C-M, Kwon Y-J, Tarng DC, Zuo L, Wheeler DC, Tsukamoto Y, Fukagawa M: 2017 Kidney Disease: Improving Global Outcomes (KDIGO) chronic kidney disease-mineral and bone disorder (CKD-MBD) guideline update implementation: Asia summit conference report. Kidney Int Rep 4: 1523–1537, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kawaguchi T, Karaboyas A, Robinson BM, Li Y, Fukuhara S, Bieber BA, Rayner HC, Andreucci VE, Pisoni RL, Port FK, Morgenstern H, Akizawa T, Saran R: Associations of frequency and duration of patient-doctor contact in hemodialysis facilities with mortality. J Am Soc Nephrol 24: 1493–1502, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Al Salmi I, Larkina M, Wang M, Subramanian L, Morgenstern H, Jacobson SH, Hakim R, Tentori F, Saran R, Akiba T, Tomilina NA, Port FK, Robinson BM, Pisoni RL: Missed hemodialysis treatments: International variation, predictors, and outcomes in the dialysis outcomes and practice patterns Study (DOPPS). Am J Kidney Dis 72: 634–643, 2018 [DOI] [PubMed] [Google Scholar]
- 11.Yagisawa T, Mieno M, Ichimaru N, Morita K, Nakamura M, Hotta K, Kenmochi T, Yuzawa K: Trends of kidney transplantation in Japan in 2018: Data from the kidney transplant registry. Renal Rep Ther 5: 3, 2019 [Google Scholar]


