Abstract
Currently recommended control measures for treating leprosy with multidrug therapy should control the spread of drug-resistant strains; however, dapsone (DDS) resistance continues to be reported. Comprehensive estimates of drug-resistant leprosy are difficult to obtain due to the cumbersome nature of the conventional drug susceptibility testing method using mouse footpad inoculation, which requires at least 6 months to obtain results. Recently, it has been determined that DDS-resistant strains contain missense mutations in codon 53 or 55 of the folP1 gene of Mycobacterium leprae, and definitive evidence linking these mutations with DDS resistance in M. leprae has been obtained. Based on these mutations, a heteroduplex DDS M. leprae (HD-DDS-ML) assay was developed for the simultaneous detection of M. leprae and of its susceptibility to DDS. The assay relies on the PCR amplification of an M. leprae-specific 231-bp fragment of folP1 containing codons 53 and 55. The PCR products are allowed to anneal to a universal heteroduplex generator, and the separation of the resultant DNA duplexes is accomplished by polyacrylamide gel electrophoresis. M. leprae was detected in crude cell lysates of skin biopsy specimen homogenates from eight leprosy patients and from M. leprae-infected mouse or armadillo tissues infected with 14 separate strains using the HD-DDS-ML assay. The assay was specific for M. leprae in a comparison with results obtained from 14 species of mycobacteria other than M. leprae and four bacterial species known to colonize human skin. The HD-DDS-ML assay detected as few as 100 M. leprae organisms present in homogenates of human skin and demonstrated a 93% correlation with DDS susceptibility as determined by both DNA sequencing of folP1 and mouse footpad susceptibility testing. The HD-DDS-ML assay provides a new tool for the simultaneous detection of M. leprae and of its susceptibility to DDS from a single specimen. The assay should prove useful for drug resistance surveillance in leprosy control programs when combined with similar molecular tests developed for other drug resistance markers.
Prior to the development and implementation of multidrug therapy (MDT) for leprosy, most patients were treated with dapsone (DDS) monotherapy. During this period, DDS-resistant strains of Mycobacterium leprae were identified and DDS-resistant leprosy became a significant problem for leprosy control programs (10, 12, 16). The currently recommended leprosy treatment with DDS, clofazimine, and rifampin (11) should control the spread of drug-resistant strains; however, DDS-resistant strains of M. leprae continue to be reported even in areas of the world with successful implementation of MDT (1, 5, 13).
M. leprae has yet to be cultivated on artificial medium; therefore, to obtain drug susceptibility patterns, the bacteria must be tested in Shepard's mouse footpad (MFP) assay (19). Because of the cumbersome nature of this drug-screening method, comprehensive estimates of drug resistance in leprosy have been difficult to obtain. Recently, there have been advances in the elucidation of molecular events responsible for drug resistance in mycobacteria (17, 21, 24). This information has been used to develop new tools for drug resistance screening (2, 21, 22–24). However, no tools of this nature exist for detecting DDS-resistant M. leprae.
DDS, 4,4-diaminodiphenylsulfone, is a synthetic sulfone with effective antileprosy activity (14, 15, 18). Because the antibacterial activity of DDS is inhibited by para-aminobenzoate (14), it is thought that DDS has a mechanism of action similar to that of the sulfonamides, involving inhibition of folic acid synthesis (4, 9). Sulfonamides block the condensation of para-aminobenzoate and 7,8-dihydro-6-hydroxymethylpterin-pyrophosphate to form 7,8-dihydropteroate. The key bacterial enzyme in this step is dihydropteroate synthase (DHPS), encoded by folP. The subsequent conversion of 7,8-dihydropteroate to tetrahydrofolate by dihydrofolate synthase and dihydrofolate reductase is critical to the formation of various cellular cofactors, including thymidylate, glycine, methionine, pantothenic acid, and n-formylmethionyl-tRNA.
DDS resistance in M. leprae has been shown to be associated with DHPS (25) in a manner similar to resistance developed in other bacteria to the sulfonamides (4, 7, 20). Recent studies have identified point mutations in the sulfone resistance-determining region (SRDR) of M. leprae folP1 in DDS-resistant strains of M. leprae (13, 25), and enzymatic data have been described supporting the linkage of these mutations with the development of DDS resistance (25).
We report here the development of a DNA heteroduplex DDS M. leprae (HD-DDS-ML) assay to simplify the detection of mutations responsible for DDS resistance in M. leprae. The assay utilizes PCR to generate an M. leprae-specific folP1 gene fragment. The PCR product is denatured and allowed to anneal to a synthetic universal heteroduplex generator (UHG) derived from the SRDR region of the folP1 gene of M. leprae, and specific heteroduplex and homoduplex electrophoretic banding profiles are identified by polyacrylamide gel electrophoresis. The HD-DDS-ML assay proved to be sensitive and specific for M. leprae, identifying DDS-susceptible and -resistant genotypes within 6 hours of sample acquisition.
MATERIALS AND METHODS
Bacterial strains.
DDS-resistant and -susceptible strains of M. leprae were originally obtained from either biopsy materials of leprosy patients or M. leprae-infected MFPs or armadillo lymph nodes from the Anandaban Leprosy Hospital, Kathmandu, Nepal; the National Hansen's Disease Programs, Baton Rouge, La.; the Schieffelin Leprosy Research & Training Centre, Karigiri, India; and The Leprosy Research Center, National Institute of Infectious Diseases, Tokyo, Japan (Table 1). Resistance to DDS was determined by the MFP system using Shepard's kinetic method (19). DDS-resistant strains grew in the footpads of mice receiving either 0.001 or 0.01% DDS as a percentage of the weight of their mouse chow. DDS-susceptible strains did not grow at 0.0001% DDS, which is the minimal effective dose for M. leprae in the MFP.
TABLE 1.
M. leprae strains used in this study
| M. leprae strain | Sample typea | Origin | DDS susceptibilityb | PCR resultsc | Mutant alleled | HDA-DDS-ML profilee |
|---|---|---|---|---|---|---|
| 2262 | HSB | United States | >0.01 | + | Thr53Ala (ACC→GCC) | R |
| CDC-DDS-1 | MFP | United States | >0.01 | + | Thr53Ala (ACC→GCC) | R |
| 61-00 | MFP | India | >0.01 | + | Thr53Ala (ACC→GCC) | R |
| India-2, 63-00 | MFP | India | >0.01 | + | Thr53Arg (ACC→AGG) | R |
| 2898 | HSB | United States | >0.01 | + | Thr53Ile (ACC→ATC) | R |
| Airaku-3, Zensho-4 | MFP | Japan | >0.01 | + | Thr53Ile (ACC→ATC) | R |
| 591 | MFP | Nepal | >0.01 | + | Pro55Arg (CCC→CGC) | R |
| India-4, 62-00 | MFP | India | >0.01 | + | Pro55Arg (CCC→CGC) | R |
| 64-00 | MFP | India | >0.01 | + | Pro55Leu (CCC→CTC) | R |
| Zensho-2 | MFP | Japan | >0.01 | + | Pro55Leu (CCC→CTC) | R |
| SA26 | HSB | United States | >0.01 | + | None | S |
| 569 | MFP | Nepal | >0.001 and <0.01 | + | None | S |
| H101, H103, H107, NIH-1 | HSB | United States | >0.001 and <0.01 | + | None | S |
| Thai-53 | MFP | Thailand | <0.0001 | + | None | S |
| 19-F-1 | ALN | Philippines | <0.0001 | + | None | S |
| H105 | HSB | United States | <0.0001 | + | None | S |
HSB, human skin biopsy specimen; ALN, armadillo lymph node.
DDS susceptibility in MFP assay (<0.0001% DDS as a percentage of food is considered susceptible).
+, DNA template generates a 231-bp folP1 fragment and a 360-bp 18-kDA gene fragment (8).
Mutant alleles in the SRDR of folP1 obtained by PCR and automated DNA sequencing.
Heteroduplex analysis results: S, DDS-susceptible profile; R, DDS-resistant profile.
Bacteria were harvested from 70% ethanol-fixed tissues following rehydration in 10 mM Tris–1 mM EDTA buffer (pH 7.4) for 60 min (8). The rehydrated tissues were minced with scissors, resuspended in 0.3 ml of Tris-EDTA buffer, and frozen in liquid nitrogen. The specimens were thawed at 95°C, and the freeze-thaw treatment was repeated twice. If the original specimens contained at least 105 bacilli/ml, the crude cell lysates were stored at −70°C until use. If a specimen contained fewer than 105 bacteria, the DNA was purified as previously described (25).
Bacterial strains used for specificity analysis were obtained from the American Type Culture Collection (ATCC; Manassas, Va.) or from our strain collection (Laboratory Research Branch [LRB], National Hansen's Disease Programs, Baton Rouge, La.). The bacteria used in this study were Clostridium perfringens (ATCC 13124), Corynebacterium glutamicum (ATCC 13032), Escherichia coli (LRB), Staphylococcus epidermidis (LRB), and Streptococcus pyogenes (LRB). The mycobacterial species used were M. avium (ATCC 25291), M. bovis BCG (ATCC 27291), M. chelonae (ATCC 35749), M. flavescens (ATCC 14474), M. gordonae (ATCC 14470), M. intracellulare (ATCC 13950), M. kansasii (ATCC 12478), M. lufu (LRB), M. phlei (ATCC 11758), M. simiae (LRB), M. smegmatis (ATCC 14468), M. tuberculosis (ATCC 27294), M. ulcerans (LRB), and M. marinum (LRB). Crude cell lysates were obtained from M. ulcerans, M. marinum, C. perfringens, C. glutamicum, E. coli, S. epidermidis, and S. pyogenes by incubating 107 bacteria, suspended in 100 μl of sterile distilled water, in a boiling-water bath for 10 min. Genomic DNA was purified from all other bacteria by standard procedures.
PCR amplification.
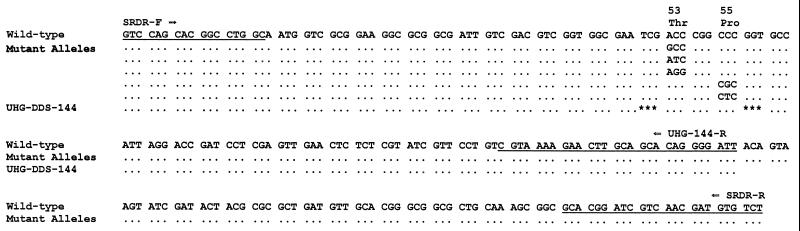
A 231-bp fragment of folP1 of M. leprae, encoding the SRDR (Fig. 1), was amplified from the crude cell lysates (8) of biopsy specimen homogenates or homogenates of MFPs by using PCR. The 231-bp fragment was amplified with the SRDR-F and SRDR-R primers (Fig. 1) in a PCR program consisting of one hold cycle for 7 min at 94°C linked to a three-step cycle of 30 s at 94°C, 30 s at 69°C, and 30 s at 72°C for 40 cycles, followed by a final hold cycle for 10 min at 72°C. The PCR amplicons were separated by gel electrophoresis on a 3% NuSieve-SeaKem (1:1) agarose gel (FMC BioProducts, Rockland, Maine). The ethidium bromide-stained gels were visualized by UV transillumination and photographed. To confirm the presence of M. leprae in these samples, the M. leprae-specific 18-kDa gene PCR was also run on the samples (26).
FIG. 1.
Map of M. leprae folP1 SRDR. Wild-type is the nucleic acid sequence of folP1 SRDR of DDS-susceptible M. leprae Thai-53. The underlined bases indicate the PCR primers for amplification of a 231-bp SRDR fragment (SRDR-F and -R) and a 144-bp UHG-DDS-144 generator (SRDR-F and UHG-144-R). Mutant alleles are those mutations found in DDS-resistant strains; UHG-DDS-144 is the 144-bp UHG containing two 3-bp deletions (∗∗∗) and used in the HD-DDS-ML assay to enhance the detection of mutant alleles associated with DDS resistance in M. leprae.
DNA sequencing.
To identify mutations associated with DDS resistance in M. leprae strains, the folP1 SRDRs from the strains were amplified by PCR as described above. The resultant PCR products were purified using a QIAQuick PCR purification kit (Qiagen, Valencia, Calif.), and the DNA sequences were obtained on a BioSystems 377 automated DNA sequencer (Perkin-Elmer, Gaithersburg, Md.) using the SRDR-F and -R primers. The sequence data were compared to those obtained for a DDS-susceptible strain of M. leprae, Thai-53.
UHG.
The universal heteroduplex generator (UHG) UHG-DDS-144, containing two 3-bp deletions which flank the 53 and 55 codon region (Fig. 1), was constructed in the following manner. A single-stranded, 144-bp “longmer” of the folP1 SRDR, containing these 3-bp deletions, was synthesized using an ABI DNA synthesizer (GeneLab, School of Veterinary Medicine, Louisiana State University, Baton Rouge) and amplified by PCR using the SRDR-F and UHG-144-R primers (Fig. 1) in a PCR program including one cycle of 5 min at 94°C followed by 40 cycles of 94°C for 30 s, 64°C for 30 s, and 72°C for 30 s, and one cycle of 72°C for 7 min. This fragment was ligated into pCR 2.1 (The Original TA Cloning Kit; Invitrogen Corp., San Diego, Calif.) to form pUHG-144 according to the manufacturer's recommendations. E. coli INVαF′ cells (Invitrogen) were transformed with pUHG-144, and positive clones were identified by PCR using the SRDR-F and UHG-144-R primer set. Plasmid DNA from an appropriate clone was purified with a QIAprep Spin Miniprep kit (Qiagen). The concentration of plasmid DNA was determined spectrophotometrically using a GeneQuant RNA-DNA calculator (Amersham Pharmacia Biotech, Piscataway, N.J.). The DNA sequence of this plasmid was obtained by automated DNA sequencing using the M13 sequencing primer, which is located upstream of the cloning site of pCR 2.1. The UHG-DDS-144 generator was amplified from pUHG-144 as described above, the concentration of the generator was determined and adjusted to 10 μg/ml, and the generator was stored at −20°C in 100-μl aliquots.
Heteroduplex analysis.
HD-DDS-ML analysis was used to detect the presence of point mutations associated with DDS resistance. Briefly, 10 μl of PCR products from specimens was mixed with 10 μl of the UHG-DDS-144 generator, and heteroduplexes were induced using a programmable thermal cycler and the following method: 5 min at 94°C, after which the temperature was decreased to 34°C using one cycle of a seven-step program (2-min ramp and 30-s hold for each 10°C decrease in temperature). Migration profiles of the heteroduplexes were obtained with precast, nondenaturing Novex 6% Tris-borate EDTA polyacrylamide gels (Invitrogen) in 0.6× Tris-borate-EDTA buffer by electrophoresis for 60 min at 170 V using an XCell II Mini-Cell (Invitrogen). Heteroduplex profiles were detected by UV transillumination of ethidium bromide-stained gels. HD-DDS-ML profiles for each strain were compared to the susceptible profile and to the DNA sequence of the folP1 SRDR of M. leprae Thai-53, as well as MFP DDS susceptibility data for each strain.
Specificity of HD-DDS-ML.
The ability of the HD-DDS-ML assay to amplify the M. leprae-specific 231-bp folP1 fragment from crude cell lysates of skin biopsy specimen homogenates and to correctly determine the DDS susceptibility from these specimens was analyzed. The specificity for detecting M. leprae was determined both at the PCR amplification step, using the SRDR-F and -R primer set, and at the heteroduplex detection step, using PCR products from a collection of well-characterized M. leprae strains from patients previously shown to have leprosy. The negative controls were (i) skin biopsy specimen homogenates (n = 10) that were negative for M. leprae by both microscopic observation and PCR for the M. leprae-specific 360-bp fragment of the 18-kDa protein gene (8, 26), (ii) purified human DNA (Sigma Chemical Co., St. Louis, Mo.), and (iii) purified DNA or crude cell lysates from a variety of bacteria. Each sample was subjected to PCR, and samples containing DNA fragments on agarose gels were further analyzed by HD-DDS-ML analysis. The specificity of the assay for detection of DDS susceptibility was determined by comparing the HD-DDS-ML profiles generated from M. leprae strains to the DNA sequence data from the SRDR of folP1 and the MFP DDS susceptibility data from these strains. Bacterial extracts testing negative by HD-DDS-ML analysis were tested by PCR for 16S ribosomal DNA common to all bacteria to rule out the presence of general PCR inhibitory activity (3).
Sensitivity of HD-DDS-ML.
The lower limit of detection of DDS susceptibility by the HD-DDS-ML assay was determined by seeding dilutions containing 107 to 0 nude-mouse-derived M. leprae Thai-53 organisms into pooled 100-μl skin biopsy specimen homogenates. The biopsy specimen homogenates were determined to be negative for both the M. leprae-specific 360-bp fragment of the 18-kDa protein gene (26) and the 231-bp fragment of the SRDR of folP1 prior to seeding (data not shown). Crude cell lysates from these samples were made as previously described (8), and the folP1 SRDR from 10 μl of these crude cell lysates was amplified by PCR using the SRDR-F and -R primers. Heteroduplex analysis was performed as described above. The lower limit of detection was defined as the lowest number of M. leprae giving a visible HD-DDS-ML profile on ethidium bromide-stained polyacrylamide gels.
RESULTS
PCR amplification of samples containing M. leprae produced a 231-bp fragment. Each PCR-positive sample was sequenced to confirm the amplification of the SRDR-containing region of folP1 (Table 1). Strains identified as having mutations in folP1 showed characteristic missense mutations at codons 53 and 55 (Fig. 1). The 231-bp product was not amplified from control samples consisting of either biopsy specimen homogenates devoid of M. leprae or purified human DNA. Similarly, the 231-bp PCR product was not amplified from the bacterial control samples, which consisted of 14 mycobacterial species, E. coli, and four microorganisms often associated with human skin or skin infections. However, very faint aberrant bands were found in M. tuberculosis and E. coli. All bacterial extracts reacted strongly in the 16S ribosomal DNA PCR, ruling out the presence of general PCR inhibitors (data not shown).
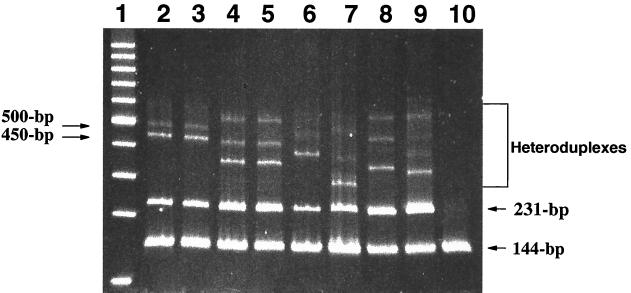
Samples containing M. leprae 231-bp DNA generated characteristic patterns consisting of homoduplexes and heteroduplexes when annealed to the UHG-DDS-144 generator (Fig. 2). All M. leprae-containing samples produced a 231-bp homoduplex as well as a 144-bp homoduplex formed by UHG-DDS-144 DNA (Fig. 2, lanes 2 to 9). Specimens not containing M. leprae gave only the 144-bp homoduplex (Fig. 2, lane 10). Faint aberrant bands generated by M. tuberculosis and E. coli in the PCR assay did not interfere with the interpretation of M. leprae HD-DDS-ML profiles.
FIG. 2.
Ethidium bromide-stained polyacrylamide minigel containing HD-DDS-ML profiles generated from DDS-susceptible and -resistant M. leprae. Lane 1, 100-bp DNA ladder (Promega); lanes 2 and 3, DDS-susceptible M. leprae Thai-53 and 19-F-1, respectively; lane 4, DDS-resistant M. leprae Airaku-3 containing the Thr53Ile folP1 mutant allele; lane 5, DDS-resistant M. leprae 2898 containing the Thr53Ile folP1 mutant allele; lane 6, DDS-resistant M. leprae 2262 containing the Thr53Ala folP1 mutant allele; lane 7, DDS-resistant M. leprae India-2 containing the Thr53Arg folP1 mutant allele; lane 8, DDS-resistant M. leprae Zensho-2 containing the Pro55Leu folP1 mutant allele; lane 9, DDS-resistant M. leprae 591 containing the Pro55Arg folP1 mutant allele; lane 10, H2O control (no M. leprae).
DDS-susceptible strains of M. leprae (MIC < 0.0001), containing the wild-type folP1, gave identical HD-DDS-ML profiles consisting of a predominant heteroduplex band at approximately 450 bp and a weaker heteroduplex band at 500 bp (Table 1 and Fig. 2, lanes 2 and 3). In contrast, all high-level (MIC > 0.01) DDS-resistant M. leprae strains except SA26 gave distinct HD-DDS-ML profiles easily discernible from the DDS-susceptible heteroduplex profiles (Table 1 and Fig. 2, lanes 4 to 9). The reproducibility of the assay was excellent, as judged by heteroduplex profiles generated from M. leprae strains with identical folP1 genes. All susceptible strains gave identical patterns, and strains carrying identical mutations produced identical heteroduplex patterns (Fig. 2, lane 2 versus 3 and lane 4 versus 5).
All intermediate-level DDS-resistant strains (MIC > 0.001 < 0.01) tested produced an HD-DDS-ML profile consistent with the DDS-susceptible genotype (Table 1). In each case, the DDS-susceptible genotype was confirmed by DNA sequencing of the SRDR.
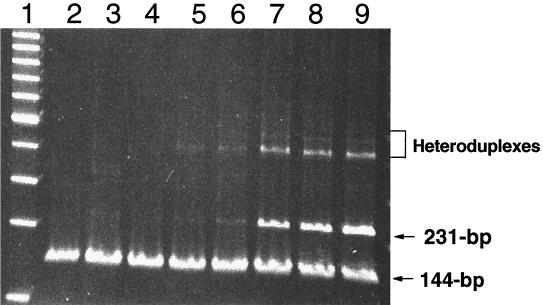
The sensitivity of the HD-DDS-ML assay was determined by using DDS-susceptible M. leprae Thai-53. Decreasing amounts of M. leprae organisms were added to aliquots of pooled biopsy specimen homogenate. Cell lysates were prepared, and each sample was amplified by PCR. The 231-bp amplicons were allowed to form DNA duplexes with the UHG-DDS-144 generator and were analyzed on gels for DNA duplex patterns. Heteroduplex band patterns diagnostic of DDS-susceptible M. leprae were visually discernible at concentrations as low as 100 organisms (Fig. 3, lane 5).
FIG. 3.
Ethidium bromide-stained polyacrylamide minigel containing HD-DDS-ML profiles of Thai-53 seeded into human biopsy specimen homogenates. Lane 1, 100-bp DNA ladder (Promega); lane 2, PCR buffer control and UHG-DDS-144; lane 3, 100 M. leprae organisms; lane 4, 101 M. leprae organisms; lane 5, 102 M. leprae organisms; lane 6, 103 M. leprae organisms; lane 7, 104 M. leprae organisms; lane 8, 105 M. leprae organisms; lane 9, 106 M. leprae organisms.
DISCUSSION
In an attempt to understand the genetic basis of DDS resistance in M. leprae, as a prelude to developing a DNA-based heteroduplex assay for DDS resistance, we evaluated a large collection of DDS-resistant strains of M. leprae for mutations in folP1 by DNA sequencing. The majority (93%) of high-level-resistant strains in our collection contained missense mutations within either codon 53 or 55 of folP1. These results supported our earlier findings that mutations in these two codons were strongly associated with proven DDS resistance (25).
By utilizing M. leprae-specific PCR primers, we were able to exploit both the species-specificity of folP1 and the unique location of the mutations in codons 53 and 55 for assay development. Under these conditions, we produced a single test which detected M. leprae in skin biopsy specimens and identified DDS susceptibility patterns which were in agreement with specific folP1 genotypes. The UHG used in the assay contained two 3-base deletions, corresponding to codons 52 and 56 of folP1, to enhance the detection of mutations within codons 53 and 55. A similarly configured DNA heteroduplex assay, employing a UHG containing deliberate nucleotide changes at nucleotide positions contiguous with known mutations within the rpoB gene, has been used successfully in our laboratory to detect mutations associated with rifampin resistance in M. tuberculosis (22, 23).
An M. leprae-specific folP1 231-bp PCR product was obtained from 100% of M. leprae strains tested. PCR results for folP1 were negative for this fragment for human skin biopsy specimen homogenates devoid of M. leprae and bacteria from several different genera. These bacteria represented species found in the normal flora of human skin and the soil or as coinhabitants of leprosy lesions. Various species of mycobacteria associated with human disease also tested negative by PCR. While this is not a complete study of the specificity of the PCR phase of the assay, it does suggest that routine skin biopsy specimens are not likely to harbor organisms or contain DNA which would interfere in the assay.
Heteroduplex profiles generated from all but one high-level DDS-resistant strain (SA26) were readily distinguishable from that of the susceptible profile. In addition, heteroduplex profiles obtained from DDS-resistant strains with the same mutation gave identical profiles, indicating that specific mutations yielded specific heteroduplex profiles. A thorough test of the specificity of mutation detection by HD-DDS-ML will require further screening of DDS-resistant isolates to develop a better understanding of the extent of mutations in folP1 associated with DDS resistance.
One of 14 (7%) high-level-resistant and all intermediate-level-resistant strains exhibited DDS-susceptible heteroduplex profiles and were found to contain the wild-type folP1 by DNA sequencing. While these results demonstrated 100% concordance between the HD-DDS-ML assay and the folP1 genotypes, the lack of concordance between the HD-DDS-ML assay and the MFP results for these strains requires explanation. The simplest interpretation is that a small percentage of high-level and intermediate-level resistance in M. leprae is not associated with mutations in the SRDR of folP1. This explanation requires the assumption of the absolute accuracy of the MFP assay in assigning levels of DDS resistance. We feel that it is important to explore this issue in terms of objective genetic data to support the existence of resistance and that the work should be extended to evaluate possible alternative mechanisms of DDS resistance with emphasis primarily on high-level-resistant strains of M. leprae. This does not rule out the possibility that in some instances the phenotypic manifestation of DDS resistance may be the result of other mechanisms not amenable to mutational analysis.
An alternative explanation for the lack of concordance between HD-DDS-ML and MFP testing for the high-level-resistant strain SA26 is related to the fact that this strain was tested directly from a biopsy specimen. It is possible that the biopsy specimen contained a preponderance of DDS-susceptible M. leprae organisms which when tested exhibited the susceptible profile by both HD-DDS-ML and DNA sequencing. However, inoculation of this same bacterial suspension into mice treated with DDS could have resulted in the outgrowth of a small resistant population of M. leprae, explaining the discrepancy observed between the two assays. Unfortunately, the M. leprae strain harvested from the MFP was not available for testing to determine the genotype present in the MFP-grown M. leprae.
Whether low-level (MIC > 0.0001 < 0.001) and intermediate-level DDS resistance in a patient is significant in terms of the clinical response to treatment with DDS has been debated for decades (10, 11). Our earlier results support the view that only specific mutations in the SRDR of folP1 reflect DDS resistance and that these mutations can be traced to changes in DHPS enzymatic activity (25). For example, enzymatic studies with mutant M. leprae DHPS (codon 53 or 55) showed that elevated levels of DDS were needed to inhibit DHPS activity compared to those needed for the wild-type DDS-susceptible enzyme. Moreover, in these studies only mutant M. leprae folP1 produced E. coli transformants for which the MICs of DDS were enhanced (25).
The HD-DDS-ML assay was able to detect the presence of M. leprae and its DDS susceptibility genotype from as little as 100 M. leprae organisms when known concentrations of M. leprae Thai-53 were seeded into aliquots of pooled biopsy specimen homogenates and amplified by PCR. While this was not the same as analyzing skin biopsy specimen homogenates with specific numbers of M. leprae directly from leprosy patients, the results gave an estimation of the sensitivity of the assay and demonstrated that it was capable of detecting the presence and DDS susceptibility of M. leprae directly from skin biopsy specimen homogenates of several lepromatous leprosy patients. These homogenates contained bacterial counts ranging from 2 × 106 to 1 × 107 bacteria/ml of homogenate. Since lepromatous patients have been shown to harbor large numbers of M. leprae organisms in the nasal mucosa (6) and are thought to be a likely source of infection for others, the HD-DDS-ML may be useful for rapidly identifying patients infected with high-level DDS-resistant M. leprae.
In summary, a rapid DNA-based assay was developed for the simultaneous detection of M. leprae and of its susceptibility to DDS directly from clinical specimens. The HD-DDS-ML assay was highly sensitive and specific for detection of M. leprae and demonstrated that DDS susceptibility profiles could be obtained from biopsy specimens within 6 h of sample acquisition. The immediate usefulness of HD-DDS-ML is the potential for supplanting the MFP assay for DDS resistance screening. While implementing HD-DDS-ML for screening purposes is likely beyond the capabilities of most clinical laboratories, it would not be unrealistic for many reference laboratories with modest equipment and training in PCR techniques. Accordingly, HD-DDS-ML may find its greatest utility as an epidemiological tool for studying the transmission of DDS-resistant M. leprae or by identifying high-level DDS-resistant leprosy cases early in the course of disease. Both applications could help us gain insight into the global burden of DDS-resistant leprosy.
ACKNOWLEDGMENTS
We thank N. Robbins and C. Lewis for their expert technical help and C. K. Job, G. J. Ebenezer, and P. Roche for well-characterized DDS-resistant M. leprae strains.
This research was supported in part by a grant from the Heiser Program for Research in Leprosy and Tuberculosis.
REFERENCES
- 1.Butlin C R, Neupane K D, Failbus S S, Morgan A, Britton W J. Drug resistance in Nepali leprosy patients. Int J Lepr Other Mycobact Dis. 1996;64:136–141. [PubMed] [Google Scholar]
- 2.Cockerill E R., III Genetic methods for assessing antimicrobial resistance. Antimicrob Agents Chemother. 1999;43:199–212. doi: 10.1128/aac.43.2.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cox R A, Kempsell K, Fairclough L, Colston M J. The 16S ribosomal RNA of Mycobacterium leprae contains a unique sequence which can be used for identification by the polymerase chain reaction. J Med Microbiol. 1991;35:284–290. doi: 10.1099/00222615-35-5-284. [DOI] [PubMed] [Google Scholar]
- 4.Dallas W S, Gowen J E, Ray P H, Cox M J, Dev I K. Cloning, sequencing and enhanced expression of the dihydropteroate synthase gene of Escherichia coli MC4100. J Bacteriol. 1992;174:5961–5970. doi: 10.1128/jb.174.18.5961-5970.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.dela Cruz E, Cellona R V, Balagon M V, Villahermosa L G, Fajardo T T, Jr, Abalos R M, Tan E V, Walsh G P. Primary dapsone resistance in Cebu, The Philippines; cause for concern. Int J Lepr Other Mycobact Dis. 1996;64:264–267. [PubMed] [Google Scholar]
- 6.deWit M Y L, Douglas J T, McFadden J, Klatser P R. Polymerase chain reaction for detection of Mycobacterium leprae in nasal swab specimens. J Clin Microbiol. 1993;32:502–506. doi: 10.1128/jcm.31.3.502-506.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fermer C, Swedberg G. Adaptation to sulfonamide resistance in Neisseria meningitidis may have required compensatory changes to retain enzyme function: kinetic analysis of dihydropteroate synthases from N. meningitidis expressed in a knockout mutant of Escherichia coli. J Bacteriol. 1997;179:831–837. doi: 10.1128/jb.179.3.831-837.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fiallo P, Williams D L, Chan G P, Gillis T P. Effects of fixation on polymerase chain reaction detection of Mycobacterium leprae. J Clin Microbiol. 1992;30:3095–3098. doi: 10.1128/jcm.30.12.3095-3098.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hampele I C, D'Arcy A, Dale G E, Kostrewa D, Nielsen J, Oefner C, Page M G, Schonfeld H, Stuber D, Then R L. Structure and function of the dihydropteroate synthase from Staphylococcus aureus. J Mol Biol. 1997;268:21–30. doi: 10.1006/jmbi.1997.0944. [DOI] [PubMed] [Google Scholar]
- 10.Jacobson R R, Hastings R C. Primary sulfone resistance leprosy. Int J Lepr Other Mycobact Dis. 1978;46:116. [PubMed] [Google Scholar]
- 11.Jacobson R R. Treatment. In: Hastings R C, editor. Leprosy. New York, N.Y: Churchhill Livingstone, Inc.; 1994. pp. 317–349. [Google Scholar]
- 12.Ji B. Drug resistance in leprosy—a review. Lepr Rev. 1985;56:262–278. [PubMed] [Google Scholar]
- 13.Kai M, Matsuoka M, Nakata N, Maeda S, Gidoh M, Maeda Y, Hashimoto K, Kobayashi K, Kashiwabara Y. Diaminodiphenylsulfone resistance of Mycobacterium leprae due to mutations in the dihydropteroate synthase gene. FEMS Microbiol Lett. 1999;177:231–235. doi: 10.1111/j.1574-6968.1999.tb13737.x. [DOI] [PubMed] [Google Scholar]
- 14.Kulkari V M, Seydel J K. Inhibitory activity and mode of action of diaminodiphenylsulphone in cell-free folate synthesizing systems prepared from Mycobacterium lufu and Mycobacterium leprae. Chemotherapy. 1983;29:58–67. doi: 10.1159/000238174. [DOI] [PubMed] [Google Scholar]
- 15.Levy L. Activity of derivatives and analogs of dapsone against Mycobacterium leprae. Antimicrob Agents Chemother. 1978;14:791–793. doi: 10.1128/aac.14.5.791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pearson J M H, Haile G S, Barnetson R S C. Dapsone-resistant leprosy in Ethiopia. Lepr Rev. 1979;50:183–199. doi: 10.5935/0305-7518.19790024. [DOI] [PubMed] [Google Scholar]
- 17.Ramaswamy S, Musser J M. Molecular genetic basis of antimicrobial agent resistance in Mycobacterium tuberculosis: 1998 update. Tubercle Lung Dis. 1998;79:3–29. doi: 10.1054/tuld.1998.0002. [DOI] [PubMed] [Google Scholar]
- 18.Seydel J K, Richter M, Wempe E. Mechanism of action of the folate blocker diaminodiphenylsulfone (dapsone, DDS) studied in E. coli cell-free extracts in comparison to sulfonamides (SA) Int J Lepr. 1980;48:18–29. [PubMed] [Google Scholar]
- 19.Shepard C C. A kinetic method for the study of activity of drugs against Mycobacterium leprae in mice. Int J Lepr. 1967;35:429–435. [Google Scholar]
- 20.Swedberg G, Ringertz S, Skold O. Sulfonamide resistance in Streptococcus pyogenes is associated with differences in the amino acid sequence of its chromosomal dihydropteroate synthase. Antimicrob Agents Chemother. 1998;42:1062–1067. doi: 10.1128/aac.42.5.1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Williams D L, Waguespack C, Eisenach K, Crawford J T, Portaels F, Salfinger M, Nolan C M, Abe C, Sticht-Groh V, Gillis T P. Characterization of rifampin resistance in pathogenic mycobacteria. Antimicrob Agents Chemother. 1994;38:2380–2386. doi: 10.1128/aac.38.10.2380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Williams D L, Limbers C, Spring L, Jayachandra S, Gillis T P. PCR-heteroduplex detection of rifampin-resistant Mycobacterium tuberculosis. In: Persing D H, editor. PCR protocols for emerging infectious diseases. Washington, D. C.: ASM Press; 1997. pp. 122–129. [Google Scholar]
- 23.Williams D L, Spring L, Gillis T P, Salfinger M, Persing D H. Evaluation of a polymerase chain reaction-based universal heteroduplex generator assay for direct detection of rifampin susceptibility of Mycobacterium tuberculosis from sputum samples. Clin Infect Dis. 1998;26:446–450. doi: 10.1086/516313. [DOI] [PubMed] [Google Scholar]
- 24.Williams D L, Gillis T P. Detection of drug-resistant Mycobacterium leprae using molecular methods. Indian J Lepr. 1999;71:137–153. [PubMed] [Google Scholar]
- 25.Williams D L, Spring L, Harris E, Roche P, Gillis T P. The dihydropteroate synthase of Mycobacterium leprae and dapsone resistance. Antimicrob Agents Chemother. 2000;44:1530–1537. doi: 10.1128/aac.44.6.1530-1537.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Williams D L, Gillis T P, Booth R J, Looker D, Watson J D. The use of a specific DNA probe and polymerase chain reaction for the detection of Mycobacterium leprae. J Infect Dis. 1990;162:193–200. doi: 10.1093/infdis/162.1.193. [DOI] [PubMed] [Google Scholar]