Introduction
Rural hospitals rarely have the capacity and expertise to deliver timely and appropriate care for patients with ESKD because providing effective dialysis care requires a staff nephrologist readily available to coordinate care for patients on dialysis as well as proper infrastructure for water treatment systems and dialysis equipment. For these reasons, clinicians in rural hospitals typically transfer patients requiring dialysis to other, larger hospitals, sometimes hundreds of miles away. These transfers reflect broader deficits in access to timely and effective specialty care services, and may lead to poorer outcomes for rural residents (1). An analysis of the hospital admission data from the state of Georgia revealed that almost all patients with ESKD were admitted to regional or tertiary care hospitals, even when the patient resides in the primary service area of a nearby rural hospital (J. Tannenbaum, J. Lea, D. Brunn, unpublished data).
Telemedicine is the delivery of healthcare services using information and communication strategies for the exchange of valid data for the diagnosis and treatment of disease to advance the health of individuals in remote areas (2,3). Tele-nephrology uses these technologies to provide care to patients with kidney disease. Asynchronous telehealth occurs when medical data are transmitted between participants for assessment when convenient and oftentimes uses remote monitoring devices such as BP monitors. This store-and-carry-forward telehealth method in the form of e-consults (electronic clinician-to-clinician communications) has been the most used form of tele-nephrology in ambulatory settings (4) and has the potential to overcome limited specialist availability, travel distance, and other barriers to expert specialty care for rural residents. In nephrology, active United States–based telehealth programs include those in specialized populations, such as veterans and the Zuni tribe in New Mexico, and others primarily in outpatient clinic settings (4–8). However, there is very little experience with telemedicine for patients with renal disorders in rural hospitals using real-time (synchronous) videoconferencing and virtual examination, although there is experience in the home dialysis space (9).
Other non-nephrology telemedicine services such as tele-stroke and tele-ICU (tele-intensive care unit) that use real-time monitoring have been implemented in hospital settings and have shown positive health outcomes (10,11). In addition, telemedicine interventions decreased overall mortality and length of stay (LOS) within progressive care units in a large hospital system without substantial cost incurrences (12). In this Perspective, we report our 2-year experiences, processes of care, and clinical outcomes for our tele-nephrology program serving rural hospitals.
Emory/Sanderling Renal Services Tele-nephrology Program
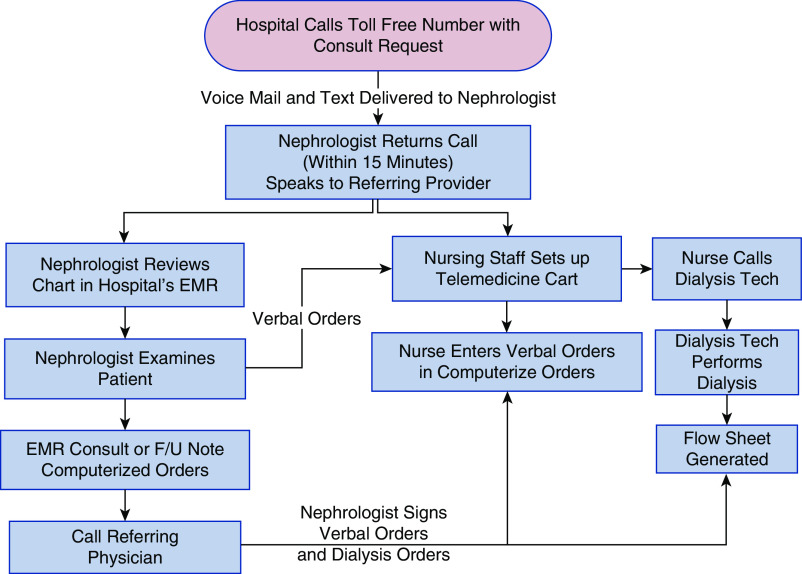
The Emory Tele-nephrology Program—affiliated with Sanderling Renal Services (SRS) (13), a large network of privately operated tele-nephrology programs connecting generalist physicians in rural hospitals to nephrologists in urban and suburban communities since 2014 across 12 states—was launched in September 2017 by Emory nephrology faculty based in Atlanta, Georgia (14). We provided consults for patients on chronic dialysis and those with CKD, AKI, and electrolyte disturbances in three rural southern Georgia hospitals (14) that had between 45 and 80 inpatient beds and employed no local nephrologists. Emory tele-nephrologists were credentialed by proxy at each rural hospital and received WebEx training on each hospital electronic medical record (EMR). See Figure 1 for workflow processes for the tele-nephrology consults. Physical examination was facilitated by audiovisual technology (FaceTime using end-to-end encryption) and Littmann electronic stethoscope. We followed patients on a daily basis until discharge or resolution of AKI or electrolyte abnormality based on clinical judgment. Initial consultation time averaged 20–30 minutes for connecting to the videoconference and interviewing and examining the patient, with an additional 20 minutes to document the note in EMR; however, subsequent follow-up visits totaled only 20–30 minutes.
Figure 1.
Tele-nephrology workflow process. EMR, electronic medical record; F/U, follow-up; tech, technician.
Dialysis services were provided by local certified clinical dialysis technicians (CCHTs) employed by SRS using NxStage (System One S) portable equipment. This platform was simple to use in any hospital room because it is self-contained and requires no disinfection or water maintenance. Dialysis treatments performed in the patient’s room had several advantages including elimination of nursing handoff and medication errors, and continuity of care provided by the floor nurse. Our hemodialysis (HD) platform is described as “e-Dialysis” because it provides real-time alerts to the nephrologist and the acute dialysis nurse who remotely supervises the dialysis technician. The CCHT at the patient’s bedside enters all of the flow-sheet data into a web-based EMR, including BP, blood flow rate, volume removed, and ultrafiltration rate. These data are immediately available to the nephrologist and the remote acute HD nurse via a mobile application, and thus both will receive instant notification through a secure email if any of the patient parameters are outside the preset ranges. The supervising HD nurse and/or nephrologist can view the patient or communicate with the CCHT at any time during the session via tele-video conference.
Our tele-nephrology program is funded through a medical director contract with SRS. Our tele-nephrologists are compensated with a reimbursement rate typical for Medicare payments for inpatient consults paid by SRS, while the rural hospitals pay a consult fee to SRS under a purchase service agreement to provide turnkey tele-nephrology and dialysis services to the hospital.
Experiences and Outcomes of Our Tele-nephrology Program
In our 2-year experience we have treated a total of 125 unique patients including 350 follow-up consults. See Table 1 for a description of clinical outcomes for both the patients with ESKD and non-ESKD including mortality rate, LOS, transfers, and case mix index, as well as for details on dialysis sessions and vascular access type. For the 65% of non-ESKD consults for AKI, 78% had a complete or near complete renal recovery rate at discharge. Of the non-ESKD consults, 35% were for electrolyte disorders, 40% of which were for hyponatremia, and all patients had safe correction rates of <10 meq/L in the first 24 hours. The most common causes for admission among the patients with ESKD were congestive heart failure (34%) and pneumonia (8%). No access-related infections or failures were admitted because the rural hospitals did not have a vascular surgeon on staff, and thus those patients on dialysis required transfer to a tertiary facility. Very few HD complications were observed with only 5% of HD sessions resulting in hypotension defined as systolic BP <90 mm Hg. Of our overall renal consult population, 34% was managed in the intensive care unit, with 8% requiring pressor support.
Table 1.
Tele-nephrology consult patient and dialysis characteristics, outcomes, and vascular access type
| Characteristic | Age | LOS | Transfer (%) | Mortality (%) | Case Mix Index | ||
| ESKD (N=73) | 60 | 3.8 | 6 | 0 | 1.41 | ||
| Non-ESKD (N=52) | 63 | 6.3 | 11 | 6 | 1.1 | ||
| AKI (n=34) | |||||||
| Non-AKI (n=18) | |||||||
| Hypona (40%) | |||||||
| HD treatment data | Total HD Sessions | Mean no. HD per Admit | Time (h) | QB | QD | Total Dialysate Volume (L) | Total UF Volume (L) |
| 157 | 1.8 | 3.8 | 365 | 300 | 60 | 1.6 | |
| Vascular access type (%) | AVF | AVG | Permcath | ||||
| 57 | 38 | 6 | |||||
All numerical values are means. LOS, length of stay in days; non-AKI, electrolyte abnormalities; hypona, hyponatremia; QB, blood flow (ml/min); QD, dialysate flow (ml/min); UF, ultrafiltration; AVF, arteriovenous fistula; AVG, arteriovenous graft; Permcath, permanent catheter.
Survey data indicated that patients were comfortable with this new model of renal care that enabled family visitation. Subjectively, the tele-nephrologists’ experience was positive, as noted by the satisfaction with the quality of the physical exam (i.e., volume status) via videoconferencing and electronic stethoscope. Anecdotally, rural hospitalists and nursing staff appreciated the comradery and clinical support in comanaging these complex renal patients.
Limitations of Hospital-Based Tele-nephrology
We have noted several limitations in our telemedicine service that need to be addressed to sustain such programs in the future. One limitation is the inability of our nephrologists to remotely examine urine sediment microscopically for AKI consults as per usual nephrology practice. Other limitations include characteristics unique to rural hospitals such as the lack of multispecialty expertise which limits the care for patients with more complex needs, the historically poor perceptions of medical care at these small nontertiary rural hospitals, lack of financial security and billing expertise, and the need for buy-in of local nephrologists not employed by the rural hospital. These hospitals did not have employed local nephrologists on staff due to low patient volumes; instead, the nephrologists were credentialed at larger remote hospitals where they oftentimes referred their patients. Finally, the lack of individual hospital EMRs interfacing with one another as well as poor information technology infrastructure in rural locations are also important barriers.
Tele-nephrology in Rural Hospitals: Summary and Future Applications
Patients in rural hospitals who received nephrology care via our telemedicine program were effectively managed in their local hospitals, had minimal transfers out to higher levels of care, experienced low mortality rates, and did not have unusually long stays in hospital. The higher case mix index in patients with ESKD allows for a greater level of reimbursement to the rural hospitals which can increase their financial viability. Expansion of tele-nephrology services will be vital to the larger renal community due to the shortages of nephrologists that now exist in rural areas and to the concerning decreasing numbers of medical house staff pursuing nephrology fellowships in the United States (15). The use of e-Dialysis, using “tele-nursing” to supervise remote acute dialysis performed by a CCHT is a potential solution to the shortage of HD nurses. Furthermore, with the recent coronavirus pandemic, upscaling remote delivery of hospital tele-nephrology services can provide premium value by reducing disease transmission, preserving the renal workforce, and offloading the stretched resources of many hospitals.
Next steps to establish the clinical benefits and cost-effectiveness of rural tele-nephrology services are to analyze and link our database to larger national data sets to compare LOS, hospital readmissions, and mortality. Our work will provide a natural stepping stone for additional work of value to payers and policymakers concerned about the health of rural residents with complex chronic conditions with inadequate access to specialty care. In conclusion, tele-nephrology is an innovative, safe, and feasible option to provide specialty renal care in underserved rural hospitals that will help mitigate the current shortage of nephrologists and dialysis nurses, positively affect healthcare delivery, and potentially reduce costs.
Disclosures
Emory University Renal Division has a medical director contract with SRS to provide tele-nephrology services for the rural hospitals in Georgia. J. Lea reports other from SRS during the conduct of the study, and other from SRS outside the submitted work. J. Tannenbaum reports nonfinancial support from SRS during the conduct of the study, and other from SRS outside the submitted work.
Funding
None.
Acknowledgments
We want to acknowledge our Emory tele-nephrologists: Tahsin Masud, James Someren, Jason Cobb, Anees Quyyumi, and Jose Navarrete.
Author Contributions
J. Lea wrote the original draft; J. Tannenbaum was responsible for data curation and formal analysis; J. Lea and J. Tannenbaum conceptualized the study, reviewed and edited the manuscript, and were responsible for project administration and supervision.
References
- 1.Rodriguez RA, Hotchkiss JR, O’Hare AM: Geographic information systems and chronic kidney disease: racial disparities, rural residence and forecasting. J Nephrol 26: 3–15, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tuckson RV, Edmunds M, Hodgkins ML: Telehealth. N Engl J Med 377: 1585–1592, 2017 [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization : Telemedicine: opportunities and developments in member states. Report on the second global survey on eHealth, Geneva, Switzerland, World Health Organization, 2010
- 4.Rohatgi R, Ross MJ, Majoni SW: Telenephrology: Current perspectives and future directions. Kidney Int 92: 1328–1333, 2017 [DOI] [PubMed] [Google Scholar]
- 5.Ladino MA, Wiley J, Schulman IH, Sabucedo AJ, Garcia D, Cardona JM, Valdes A, Pedraza F, Echeverri RJ: Tele-nephrology: a feasible way to improve access to care for patients with kidney disease who reside in underserved areas. Telemed J E Health 22: 650–654, 2016 [DOI] [PubMed] [Google Scholar]
- 6.Narva AS, Romancito G, Faber T, Steele ME, Kempner KM: Managing CKD by telemedicine: The zuni telenephrology clinic. Adv Chronic Kidney Dis 24: 6–11, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crowley ST, Belcher J, Choudhury D, Griffin C, Pichler R, Robey B, Rohatgi R, Mielcarek B: Targeting access to kidney care via telehealth: The VA experience. Adv Chronic Kidney Dis 24: 22–30, 2017 [DOI] [PubMed] [Google Scholar]
- 8.Tan J, Mehrotra A, Nadkarni GN, He JC, Langhoff E, Post J, Galvao-Sobrinho C, Thode HC Jr., Rohatgi R: Telenephrology: Providing healthcare to remotely located patients with chronic kidney disease. Am J Nephrol 47: 200–207, 2018 [DOI] [PubMed] [Google Scholar]
- 9.Krishna VN, Managadi K, Smith M, Wallace E: Telehealth in the delivery of home dialysis care: catching up with technology. Adv Chronic Kidney Dis 24: 12–16, 2017 [DOI] [PubMed] [Google Scholar]
- 10.Akbik F, Hirsch JA, Chandra RV, Frei D, Patel AB, Rabinov JD, Rost N, Schwamm LH, Leslie-Mazwi TM: Telestroke-the promise and the challenge. Part one: growth and current practice. J Neurointerv Surg 9: 357–360, 2017 [DOI] [PubMed] [Google Scholar]
- 11.Young LB, Chan PS, Lu X, Nallamothu BK, Sasson C, Cram PM: Impact of telemedicine intensive care unit coverage on patient outcomes: A systematic review and meta-analysis. Arch Intern Med 171: 498–506, 2011 [DOI] [PubMed] [Google Scholar]
- 12.Armaignac DL, Saxena A, Rubens M, Valle CA, Williams LS, Veledar E, Gidel LT: Impact of telemedicine on mortality, length of stay, and cost among patients in progressive care units: experience from a large healthcare system. Crit Care Med 46: 728–735, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sanderling Renal Services , Jerome Tannenbaum: Enhancing life through teamwork technology and innovation. 2018. Available at: http://www.srs-usa.com. Accessed April 30, 2020
- 14.Powers L: Emory launches new initiative to improve dialysis patient care, Atlanta, Georgia, Emory University, 2018. Available at: http://news.emory.edu/stories/2018/02/telenephrology_clinics/index.html. Accessed April 27, 2020
- 15.Parker MG, Ibrahim T, Shaffer R, Rosner MH, Molitoris BA: The future nephrology workforce: Will there be one? Clin J Am Soc Nephrol 6: 1501–1506, 2011 [DOI] [PubMed] [Google Scholar]