Many countries in sub-Saharan Africa face enormous economic and human resource challenges in the management of patients with ESKD (1). Dialysis, the most common form of RRT in these countries, requires costly equipment (2) and is inaccessible to patients that are poor. This situation is exacerbated by a limited number and the busy schedules of dialysis centers. The hemodialysis population rate remains low at between 0 and 200 per million inhabitants in sub-Saharan Africa, so many patients die without accessing dialysis because of a lack of means. In many countries in sub-Saharan Africa, dialysis facilities are unavailable (3,4).
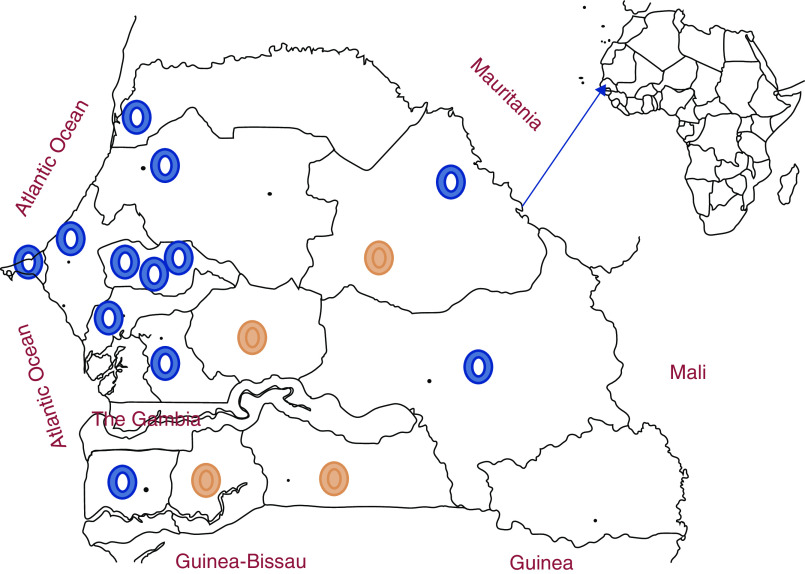
Senegal is a country in West Africa bordered by the Atlantic Ocean to the west, Mauritania to the north, Mali to the east, Guinea and Guinea-Bissau to the south, and the Gambia located within (Figure 1). It covers 196,712 km2 and has 16,209,125 inhabitants (5), with an average density of 82 inhabitants per km2. There is a disparity in the distribution of the population between the 14 administrative regions: Dakar, the capital, constitutes the smallest area and includes 23% of the total population and 75% of the urban population, whereas the southeastern regions house only 6% of the total population. Young people aged <20 years represent 55% of the population, with an annual growth rate of 4%. According to the World Bank, the country has a lower-middle-income classification on the basis of gross national income, which is US$1410 per capita. Since 1987, patients with ESKD have been treated with hemodialysis. Only 25 patients were on dialysis in 2004 in the country. There are currently no national data on the incidence or causes of ESKD. However, in the Dakar University Hospital, the causes are dominated by hypertensive nephropathy followed by diabetic nephropathy. There are currently no national mortality data for patients on hemodialysis; however, infectious and cardiovascular complications are mainly noted as causes of mortality.
Figure 1.
Distribution of dialysis centers across regions of Senegal. Functional dialysis centers are shown in blue and dialysis centers under construction are shown in orange.
Dialysis: A Concern of the Authorities
In Senegal, good awareness and advocacy made by patient associations and health professionals has made dialysis a major governmental concern. In recent years, with the opening of dialysis centers, care for patients with ESKD has improved. Dialysis companies compete for government contracts and, if they are selected, deliver machines, manage maintenance, water treatment, and consumables, according to the specifications. Currently, there are 26 centers in the country, including 22 in the public sector (five are under construction) and four in the private sector. Six public dialysis centers and all four private dialysis centers are located in Dakar. There is only one peritoneal dialysis (PD) center that is located in the main university hospital in Dakar. Basic information about dialysis in Senegal is summarized in Table 1.
Table 1.
Basic information about dialysis in Senegal
| Main Characteristics | N or % | |
| Number of nephrologists in the country (per million inhabitants) | 28 | 1.75 |
| Number of patients on dialysis (total number, per million people in the general population) | 1092 | 67,3 |
| Number of patients on hemodialysis in the public sector (private) | 846 | 246 |
| Percent of patients on hemodialysis (patients on peritoneal dialysis) | 95.79% | 4.21% |
| Percent of patients on home dialysis in my country | 4.21% | |
| Number of dialysis machines (public sector) | 311 | 247 |
| Number of dialysis units in the country (public sector) | 26 | 22 |
| Number of hospital-based dialysis units (freestanding) | 21 | 3 (Private) |
| Number of dialysis units for nonprofit (for profit) | 22 | 4 (Private) |
| Percentage of patients covered by insurance (out-of-pocket expenses) in the private sector | 20% | 80% |
| Reimbursement per dialysis session in public sector in US$ (private) | 20 | 110 |
| Percent of staff who deliver dialysis (dialysis nurses, patient care technicians) | 70% | 30% |
| Typical patient-to-RN ratio in the dialysis units | 6:1 | |
| Average length of a dialysis session | 4 h | |
| How many times per month does a nephrologist see patients during dialysis sessions? | 8 | |
| Proportion of patients on hemodialysis in the country using an AVF, CVC, and AVG | AVF, 69% | |
| CVC, 30% | ||
| AVG, 1% | ||
RN, renal nurse; AVF, arteriovenous fistula; CVC, central venous catheter; AVG, arteriovenous graft.
Dialysis: Free-of-Charge Treatment for the Patient in the Public Sector
A dialysis session costs US$110 in the private sector. Since 2012, dialysis has been available free of charge in the public sector for all Senegalese patients with ESKD, on prescription of a nephrologist. This implies the possibility of free hemodialysis or PD sessions, and of having hemodialysis sessions at a reduced rate in private centers who have signed an agreement with the national agency for universal health coverage, but depends on the availability. To benefit from this free treatment, the patient must register on the waiting list in a public dialysis center. The dialysis session and the hemodialysis kit are free. However, patients pay the costs associated with dialysis, such as antihypertensive drugs, vitamin D, iron, and erythropoietin-stimulating agents. There are currently 1046 (96%) patients on hemodialysis and 46 (4%) patients on PD (Table 1). More than 1000 patients are regularly registered on the different waiting lists in the public sector dialysis centers. Over 75% of patients with ESKD die without having access to dialysis because of the lack of available machines. Almost 69% of patients on hemodialysis have an arteriovenous fistula (6). The only vascular surgery department is located in Dakar. Creation of an arteriovenous fistula and placement of a nontunneled femoral hemodialysis catheter are done at no cost to the patient. Placement of a tunneled hemodialysis catheter is also free in hospital, but the catheter must be purchased out of pocket by the patient (approximately US$220). The average duration of use of central venous catheters is 7.66 months: a tunneled catheter in 63% of patients, a nontunneled jugular catheter in 21% of patients, and a nontunneled femoral catheter in 17% of patients (6). Nontunneled central catheters are frequently complicated by infection (49%) because of the lack of financial resources available for the immediate purchase of tunneled catheter. Arteriovenous grafts are infrequently used because of their cost, which is paid by the patient.
Human Resources: A Real Need
Senegal currently has 28 nephrologists (including five nephrology professors, three nephrology assistant professors, and two pediatric nephrologists) and 22 Senegalese nephrology trainees. Excluding the three senior professors of nephrology, the remaining 25 nephrologists have been trained locally with 1 year of training in western countries, mostly in France. The Department of Nephrology at the University of Dakar has trained 126 nephrologists from 19 African countries from 2005 to 2019. Each Senegalese public dialysis center is managed by at least one nephrologist. In each center, a head nurse is responsible for administrative organization and care. Head nurses receive specialized education in nephrology and dialysis and graduate after following a 2-year curriculum at nursing school. Seventy three nurses specialized in dialysis have been trained to run dialysis units in Senegal. Hemodialysis units operate 6 days a week for an average of 8–12 hours a day. The patients do thrice-weekly sessions of 4 hours in 60% of cases. Incremental dialysis with twice-weekly sessions is applied for 40% of patients The dialysis adequacy is monitored online during the session by the Kt/V of the dialysis machine, as well as by regular biologic monitoring of patients every 2 months.
The PD Center
Senegal is currently the only West African country where PD is available for ESKD treatment. The center was inaugurated in March of 2004, with different modalities (continuous ambulatory PD and automated PD) (7). Forty six patients are currently treated with this modality (35 continuous ambulatory PD and 11 automated PD). The costs associated with PD are borne by the state, but patients pay the associated costs, such as antibiotics, antihypertensive drugs, and erythropoietin-stimulating agents. Advocacy efforts have been directed toward the promotion of domestic manufacturing, which could significantly reduce the cost of dialysis and translate into substantial financial gain, with a larger number of patients receiving treatment (7).
Issues and Challenges
Despite being free, dialysis remains difficult to access because demand far exceeds supply, hence the existence of waiting lists. The government covers the costs of the dialysis sessions. However, patients must pay for their predialysis treatment and their treatment associated with dialysis. Only 20% of patients are covered by insurance (in general, patients working for large companies). The government is making efforts to lower the costs, but these remain astronomical for the local population. Also, hemodialysis centers are mainly located in cities, as in most countries in sub-Saharan Africa, and patients in rural areas have to travel a long distance to access treatment. This imposes an additional financial burden and patients sometimes skip sessions, making dialysis inadequate (8). The average age of patients on dialysis is 47 years (range, 11–85 years). This is a young and productive population, and many of the patients are the main breadwinners (9). Job losses are also reported upon diagnosis, which makes management difficult.
Patients are generally seen late by a nephrologist, and 79% of patients with ESKD start unplanned dialysis. Patients do not have free access to the other professionals, such as dietitians and social workers, that form an integral part of the dialysis service.
Financial challenges remain at the heart of the care of patients with ESKD in Senegal. Although efforts have been made, there is still important work to be done to improve the life expectancy of patients on dialysis and develop PD. This will require better financial management, a strengthening of the means of prevention and early detection of CKD, and collaboration between high-income and low- and middle-income countries. Transplantation is the most cost-effective way to manage ESKD in low- and middle-income countries, but has not yet begun in Senegal. A national committee for organ donation and transplantation has just been set up. The first renal transplant in Senegal is planned shortly.
Disclosures
All authors have nothing to disclose.
Funding
None.
Acknowledgments
We thank Valerie Luyckx for proofreading the manuscript.
Author Contributions
A. Niang conceptualized the study, was responsible for data curation, wrote the original draft, and reviewed and edited the manuscript. A.T. Lemrabott was responsible for data validation, wrote the original draft, and reviewed and edited the manuscript.
References
- 1.Bamgboye EL: Hemodialysis: Management problems in developing countries, with Nigeria as a surrogate. Kidney Int Suppl 63: S93–S95, 2003 [DOI] [PubMed] [Google Scholar]
- 2.Liyanage T, Ninomiya T, Jha V, Neal B, Patrice HM, Okpechi I, Zhao MH, Lv J, Garg AX, Knight J, Rodgers A, Gallagher M, Kotwal S, Cass A, Perkovic V: Worldwide access to treatment for end-stage kidney disease: A systematic review. Lancet 385: 1975–1982, 2015 [DOI] [PubMed] [Google Scholar]
- 3.Davids R, Benghanem Gharbi M: Global considerations in kidney disease: Africa. In: Brenner & Rector’s The Kidney, 11th Ed, edited by Yu A, Chertow G, Luyckx V, Marsden P, Skorecki K, Taal M, Amsterdam, The Netherlands, Elsevier, 2019, pp 2493–2516 [Google Scholar]
- 4.Ashuntantang G, Osafo C, Olowu WA, Arogundade F, Niang A, Porter J, Naicker S, Luyckx VA: Outcomes in adults and children with end-stage kidney disease requiring dialysis in sub-Saharan Africa: A systematic review. Lancet Glob Health 5: e408–e417, 2017 [DOI] [PubMed] [Google Scholar]
- 5.National Agency for Statistics and Demography of Senegal : National Agency for Statistics and Demography of Senegal. Available at: www.ansd.sn. Accessed February 17, 2020
- 6.Kane Y, Lemrabott AT, Faye M, Cissé MM, Seck, Ka EHF, Niang A, Diouf B: Etat des lieux des abords vasculaires chez les hémodialysés chroniques au Sénégal. Nephrol Ther 13: 312, 2017 [Google Scholar]
- 7.Niang A, Cisse MMM, Mahmoud SM, Lemrabott AT, Ka HF, Diouf B: Pilot experience in Senegal with peritoneal dialysis for end-stage renal disease. Perit Dial Int 34: 539–543, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Naicker S: End-stage renal disease in sub-Saharan and South Africa. Kidney Int Suppl 63: S119–S122, 2003 [DOI] [PubMed] [Google Scholar]
- 9.Salako BL: Management of chronic renal failure. Afr Health 19: 26–27, 1997 [Google Scholar]