Clinical Images in Nephrology and Dialysis
Case Report
A 69-year-old woman with a medical history of diabetes, hypertension, coronary artery disease, and acute embolic cerebrovascular event postcardiac catheterization in 2016 presented to the emergency department with acute abdominal pain. Before this, she had been evaluated for symptoms of cough, shortness of breath, and myalgias which were conservatively managed with improvement. She now presented with intermittent pain of diffuse, nonspecific distribution, associated with nausea and nonbloody emesis. The patient also had lower back pain but not in either flank region. She denied history of trauma or urinary symptoms. Her medications included aspirin, clopidogrel, furosemide, and insulin.
Examination was significant for diffuse nonspecific abdominal tenderness without rebound or guarding. Laboratory assessment revealed creatinine of 1.10 mg/dl, elevated level of c-reactive protein at 20 mg/dl, sedimentation rate of 112 mm/h, lactic dehydrogenase level of 458 U/L, fibrinogen level of 737 mg/dl, and she tested positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Urine evaluation had 1.5 g of protein/g creatinine without hematuria.
A computed tomography of the abdomen and pelvis with intravenous contrast revealed a nonocclusive thrombus in the left renal artery (Figure 1, A and B) with several large wedge-shaped areas of decreased enhancement, consistent with multiple left renal infarctions (Figure 1C). She was started on an intravenous heparin drip and transitioned to apixaban. During her hospitalization, her abdominal pain improved, renal function remained preserved, and she was then discharged.
Figure 1.
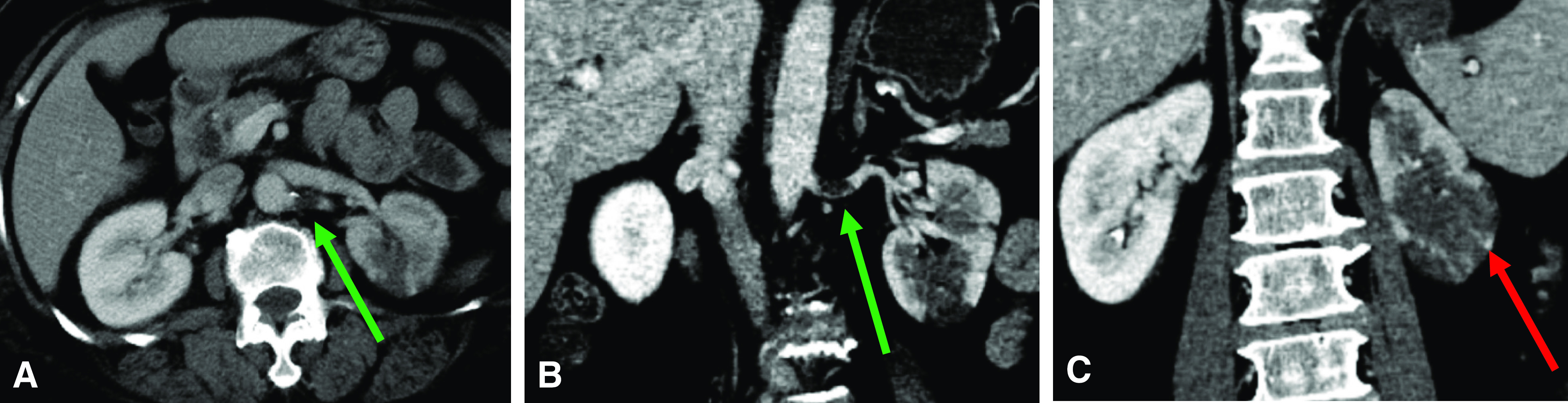
Computerized tomography (CT) scan. (A and B) Thrombus in the left renal artery represented by greens arrows. (C) Decreased enhancement consistent with multiple left renal infarctions represented by red arrow.
Discussion
What began as a series of cases of viral pneumonia initially described in Wuhan, Hubei, China, rapidly spread to emerge as a global pandemic. The virus was identified as SARS-CoV-2 and is the cause of coronavirus disease 2019 (COVID-19). Kidney injury has been associated with this infection, although the exact mechanism of injury remains unclear. Increased severity of illness has been associated with the development of coagulopathy (1). Laboratory abnormalities including leukopenia, lymphopenia, elevated prothrombin time, and d-dimer have been found in patients who are critically ill (2). A case series from Wuhan described patients with COVD-19 testing positive for anti-cardiolipin IgA and anti–β2-glycoprotein I IgA and IgG antibodies (3). Although not specific to this infection, it is hypothesized to be associated with the development of both micro- and macrovascular thrombi. A small study observed a mortality benefit in patients with severe sepsis receiving anticoagulation with low mol wt heparin (low mol wt heparin 40% versus controls 64%) (4). These preliminary data have led international societies to recommend anticoagulation in patients who are critically ill and infected with SARS-CoV-2.
Literature has described both microvascular and macrovascular coagulopathy to be associated with severe COVID-19 infection (1); however, abnormal coagulation with the development of clots has not been described in patients with relatively mild disease. Whereas venous thromboembolism and pulmonary embolism have been reported (5), no reports of renal artery thrombosis or renal infarction have been described. Our patient with relatively mild COVID-19 had derangements in coagulation markers and had a renal artery thrombus with renal infarction. Further studies are warranted to evaluate whether renal infarctions are playing a role in the AKI and whether prophylactic anticoagulation could have benefit in renal outcomes.
Teaching Points
Patients who present with SARS-CoV-2 infection, regardless of severity of disease, should be evaluated for coagulopathy and development of thrombi because these may potentially contribute to infarction and end-organ damage.
Renal infarction should be considered part of the differential when evaluating a patient with COVID-19 presenting with abdominal pain or AKI.
Initiation of anticoagulation should be considered in those who are critically ill, although it would be imperative to weigh the risks and benefits of this intervention.
Disclosures
All authors have nothing to disclose.
Funding
None.
Author Contributions
N. Kumar and R. Mocerino wrote the original draft.
References
- 1.Tang N, Li D, Wang X, Sun Z: Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost 18: 844–847, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B: Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China [published correction appears in Lancet 395: 496, 2020]. Lancet 395: 497–506, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang Y, Xiao M, Zhang S, Xia P, Cao W, Jiang W, Chen H, Ding X, Zhao H, Zhang H, Wang C, Zhao J, Sun X, Tian R, Wu W, Wu D, Ma J, Chen Y, Zhang D, Xie J, Yan X, Zhou X, Liu Z, Wang J, Du B, Qin Y, Gao P, Qin X, Xu Y, Zhang W, Li T, Zhang F, Zhao Y, Li Y, Zhang S: Coagulopathy and antiphospholipid antibodies in patients with covid-19. N Engl J Med 382: e38, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tang N, Bai H, Chen X, Gong J, Li D, Sun Z: Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost 18: 1094–1099, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rotzinger DC, Beigelman-Aubry C, von Garnier C, Qanadli SD: Pulmonary embolism in patients with COVID-19: time to change the paradigm of computed tomography. Thromb Res 190: 58–59, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]


