Abstract
Objectives:
To develop a consensus framework that can guide the process of classifying and reviewing pediatric in-hospital cardiac arrest in the PICU.
Design:
A three-round electronic Delphi consensus study with an additional in-person session with pediatric resuscitation experts. The modified electronic Delphi consisted of survey questions sent to the expert panel with the goals of (1) achieving consensus on definitions of avoidable, potentially avoidable, and unavoidable PICU in-hospital cardiac arrest and (2) achieving consensus and ranking of a list of factors that contribute to potentially avoidable PICU in-hospital cardiac arrest.
Setting:
Electronic surveys of resuscitation experts including pe- diatric critical care, cardiac critical care, emergency medicine, and hospital medicine physicians, nurses, advance practice nurses, and resuscitation researchers.
Patients:
Not applicable.
Interventions:
Not applicable.
Measurements and Main Results:
Over three rounds of an electronic Delphi, 24 resuscitation experts participated. In Round 1, consensus was reached for the definitions of potentially avoidable and unavoidable cardiac arrest. Consensus was not reached for avoidable cardiac arrest. In Round 2, the expert panel agreed with seven factors from the literature and achieved consensus on an additional seven factors. Consensus was achieved on the modified definition of avoidable cardiac arrest. In Round 3, participants were asked to rank the contributing factors in order of their importance. For the in-person session, the consensus definitions and contributing factors from the modified electronic Delphi were presented to a multidisciplinary group of pediatric resuscitation experts and reached consensus for all three definitions.
Conclusions:
A multidisciplinary group of pediatric resuscitation experts generated a consensus-based framework to classify and review pediatric in-hospital cardiac arrest in the PICU. Future work will focus on the application of this framework and further validation of these definitions and contributing factors for in-hospital cardiac arrest both within and outside the PICU. (Pediatr Crit Care Med 2020; 21:992–999)
Keywords: cardiopulmonary resuscitation, pediatrics
BACKGROUND
Pediatric in-hospital cardiac arrest (IHCA) remains an infrequent but serious problem with an estimated 7,100 children in the United States receiving in-hospital cardiopulmonary resuscitation (CPR) annually for pulseless events (1). Although pediatric IHCA outcomes have improved over recent decades, the mortality burden remains high with only 40% survival to hospital discharge (2). Although ongoing efforts to improve the delivery of high quality CPR may continue to improve survival trends, efforts should also focus on the prevention of pediatric IHCA.
To date, systematic efforts to reduce the frequency of IHCA in pediatric patients have focused on preventing cardiac arrest on the wards, prioritizing early identification of clinically decompensating inpatients with rapid transfer to a higher level of care (3–6). Some pediatric centers have shown a decrease in hospital-wide mortality rates and the rate of resuscitation events outside the PICU with implementation of rapid response teams for evaluation of decompensating patients (7, 8). Accordingly, the proportion of pediatric IHCA occurring in the PICU rather than the ward has been steadily increasing, such that the vast majority of pediatric IHCA now occurs in the PICU (9, 10). Despite this shift in event location, parallel work to prevent IHCA within the PICU has been more gradual perhaps because the events are not perceived as preventable in a higher risk population. Importantly, there is no consensus definition of avoidable or potentially avoidable PICU IHCAs that could be used to evaluate the effect of interventions targeted at prevention. Furthermore, consensus definitions of avoidable, potentially avoidable, and unavoidable PICU IHCAs could also be useful to target cases that would most benefit from in-depth formal event review to identify modifiable contributing factors. Formal safety event reviews, including root cause analyses and debriefing following resuscitation events, have been shown to decrease the occurrence of serious safety events in pediatric hospitals and improve IHCA survival, respectively (11, 12).
The Delphi method provides a structured group communication technique well-suited to gaining expert consensus on these complex and important questions (13). The overall aim of this study was to develop a consensus framework to classify and review pediatric IHCA in the PICU. First, we used the Delphi method to develop consensus around definitions of avoidable, potentially avoidable, and unavoidable pediatric IHCA in the PICU. Second, to improve understanding of events, we sought agreement around a list of important factors that contribute to potentially avoidable PICU IHCA. Last, we developed a framework to guide review of PICU IHCA using the consensus definitions and contributing factors.
MATERIALS AND METHODS
Study Design
To develop a consensus for framework for classifying and reviewing PICU IHCA events, we used the Delphi method. The Delphi method is a well-established method for solving problems, creating research agendas, and conducting needs assessments through expert consensus (13). The Delphi method develops expert consensus through a six-step process including the following: (1) Problem identification, (2) Literature search, (3) Survey development, (4) Iterative survey rounds by a predetermined expert panel, (5) Feedback between rounds to the experts, and (6) Summary of findings (13). Although the Delphi process traditionally begins with an open-ended questionnaire, it is an acceptable and common modification to use a structured questionnaire in the first round based on literature review (14). We conducted a modified Delphi administered electronically (eDelphi) (15, 16). Individual responses were deidentified. This study was determined to be nonhuman subjects research by the Institutional Review Board at Cincinnati Children’s Hospital Medical Center.
Literature Search
We completed a literature search for definitions of avoidable or preventable cardiac arrest and for lists of factors contributing to potentially avoidable or preventable cardiac arrest to derive the initial definitions and contributing factors evaluated during this study. The reviewed articles were identified through a PubMed search using MeSH terms CPR and prevention, as well as other general search terms including cardiac arrest, prevent, avoid, intensive care, and pediatrics. In addition, articles cited by these initially identified articles were also reviewed. These articles were reviewed by two of the authors (M.D., H.A.W.) and assessed for inclusion. The definitions and contributing factors were mainly derived from the adult literature due to a lack of pediatric studies (17–21).
Establishment of Expert Panel
A multidisciplinary group including physicians, nurses, resuscitation scientists, and experts from key stakeholder organizations including the American Heart Association, International Liaison Committee of Resuscitation, and the Society of Critical Care Medicine were invited to participate in the consensus process. We generated a list of corresponding authors of key published studies on pediatric IHCA referenced in the 2015 American Heart Association Guidelines (22). We used a snowball sampling technique (23), asking invitees to identify other informed individuals, who were then asked to participate. Experts were defined as anyone with in-depth knowledge of pediatric IHCA, acquired through practice or education with no minimum years of experience being a requirement. No maximum or minimum number of participants was established a priori; however, the authors did compile the list of invited participants with gender and regional balance. Following agreement to participate in the consensus process, all experts reviewed a document and video introducing them to the study, including an introduction to the aims, process, and participation (video viewable here: https://youtu.be/35zDFrAwXaY).
Survey and Iterative Feedback
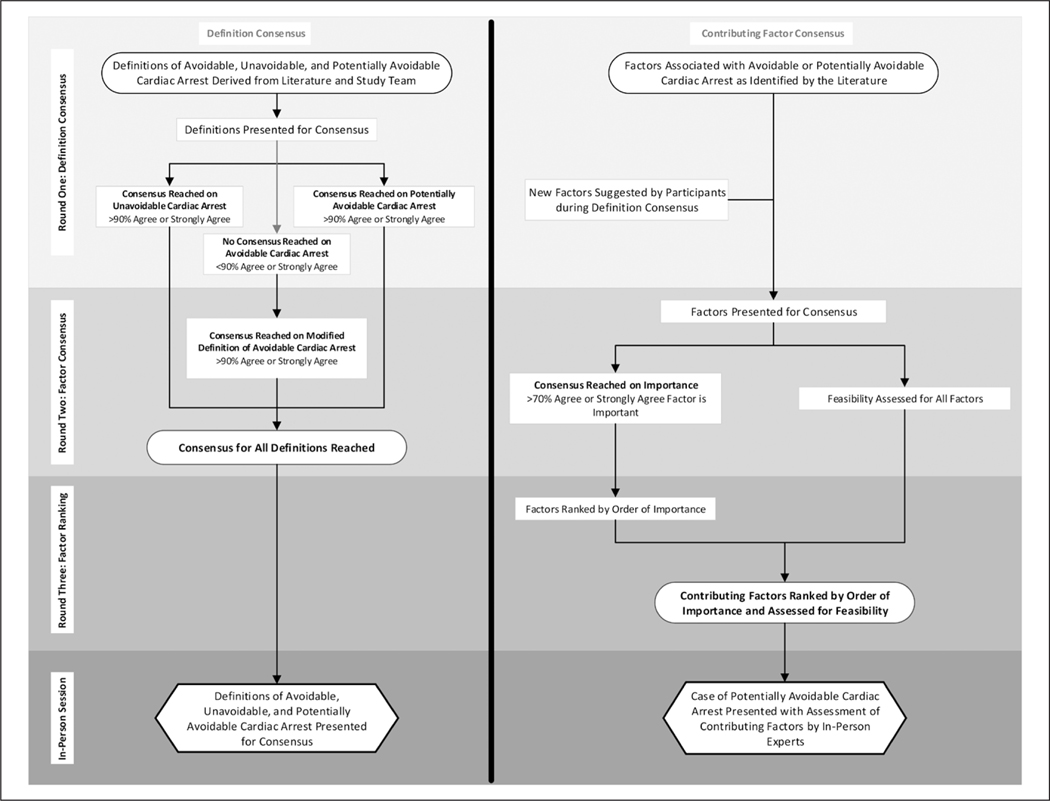
The modified eDelphi consisted of three rounds of survey questions sent to the expert panel with the goals of (1) achieving consensus on definitions of avoidable, potentially avoidable, and unavoidable PICU IHCA and (2) achieving consensus on a list of factors that contribute to potentially avoidable PICU IHCA. Figure 1 includes a visual depiction of the rounds of the eDelphi, which are described below, and Appendix I (Supplemental Digital Content 1, http://links.lww.com/PCC/B395) includes the full survey instruments as they were distributed to the expert panel.
Figure 1.
Methodology for achieving consensus on definitions and contributing factors through three electronic Delphi rounds.
Round 1: Definition Consensus.
In the first round of the modified eDelphi, we presented definitions of avoidable, potentially avoidable, and unavoidable PICU IHCA with brief clinical examples to the expert panel. The definition of unavoidable PICU IHCA was divided into three subdefinitions to address three distinct relevant clinical scenarios (for survey instruments, see Appendix I, Supplemental Digital Content 1, http://links.lww.com/PCC/B395). Experts were asked to rate their level of agreement with each definition or subdefinition on a five-point Likert scale (strongly agree, agree, neither agree nor disagree, disagree, strongly disagree). Free-text comments could be provided for feedback on each definition. Consensus was defined a priori as greater than 90% of participants either strongly agreeing or agreeing with the definition. We determined that achieving consensus for a particular definition through multiple iterations would be feasible if there was 51–90% agreement initially. If agreement was less than 50%, we determined that achieving consensus would be unlikely and planned to abandon this component. This level of consensus has been considered to be appropriate in prior Delphi studies and defined as “clear consensus” (24, 25). The list of factors that contribute to potentially avoidable PICU IHCA derived from the literature was presented to the expert panel. They were asked to provide additional factors for inclusion in the list in Round 2.
Round 2: Contributing Factor Consensus.
We combined the list of factors that contribute to potentially avoidable PICU IHCA derived from the literature with the expert panel’s additions from Round 1. A list of 14 factors was presented to participants to seek consensus on the importance of each factor’s contribution to potentially avoidable IHCA. Experts were asked to rate their level of agreement that the factor was an important contributor to potentially avoidable PICU IHCA on a five-point Likert scale (strongly agree, agree, neither agree nor disagree, disagree, strongly disagree). Consensus was defined a priori as greater than 70% of participants either strongly agreeing or agreeing that the factor was an important contributor. We set the threshold for consensus at 70% lower than the threshold for consensus on the definitions, due to variability in patient populations served with variable applicability of certain contributing factors. This level of consensus has been considered to be appropriate in prior Delphi studies (26–30). For each of the 14 factors, experts used the same Likert scale to rate their agreement that the contribution of the factor to potentially avoidable PICU IHCA would be feasible to assess during retrospective event review. Consensus was not sought for this component of the survey. Free-text comments could be provided about each factor.
Due to a lack of consensus on the definition of avoidable PICU IHCA in Round 1, modifications were made to this definition based on feedback from the expert panel, and the modified definition was presented to the participants during Round 2. The same Likert scale and threshold for consensus established for the definitions during Round 1 was used.
Round 3: Factor Ranking.
During Round 2, there was consensus among the expert panel that all 14 factors were important contributors to potentially avoidable PICU IHCA, and so no further consensus rounds were needed. Consensus was reached on the modified definition of avoidable PICU IHCA. In Round 3, participants were asked to rank the contributing factors in order of their importance. In addition, the study team grouped the contributing factors into four categories (Diagnostic Factors, Treatment/Therapeutic Factors, Communication, and Facilities and Resources), and participants were asked to rank the categories in order of their importance in contributing to potentially avoidable PICU IHCA.
In-Person Session
To further discussion around the definitions and contributing factors, as well as, identify opportunities for application, the consensus definitions and contributing factors from the modified eDelphi were presented on November 14, 2019, in Philadelphia, PA, to a multidisciplinary group of pediatric resuscitation experts and researchers assembled for a pediatric resuscitation research and quality collaborative meeting. All participants at the Pediatric Resuscitation Quality Improvement Collaborative were invited to participate including medical students, trainees, and nonclinical providers. Not all participants remained for the entirety of the session. In-person participants were asked if they agreed or disagreed with the expert panel’s definitions of avoidable, potentially avoidable, and unavoidable PICU IHCA. Polling was performed by participants holding up cards marked with agree or disagree (digital interactive polling was not technologically feasible in this location). Feedback on the draft framework was also requested from participants.
RESULTS
Description of Expert Panel
A total of 55 experts were invited including 44 physicians, nine nurses, and two resuscitation science nonclinical researchers through our snowball technique. Twenty-four experts (44%) agreed to participate from 20 institutions throughout the United States, Canada, and Europe (Appendix II, Supplemental Digital Content 2, http://links.lww.com/PCC/B396). There was 100% response rate for all rounds of the modified eDelphi. The experts were predominately physicians (83%) who worked in the PICU (65%). Other disciplines represented were pediatric hospital medicine, pediatric emergency medicine, and pediatric cardiac intensive care. More than half were female, and the median years of clinical experience for physicians and nurses was 13.5 years (interquartile range, 9.5–18 yr) (Table 1).
TABLE 1.
Self-Report Characteristics of Participants
| Characteristics | n (%) |
|---|---|
|
| |
| Healthcare profession | |
| Physician | 20 (83) |
| Pediatric intensive care | 13 (65) |
| Pediatric hospital medicine | 2 (10) |
| Pediatric emergency medicine | 1 (5) |
| Combined pediatric and cardiac intensive care | 2 (10) |
| Cardiac intensive care | 1 (5) |
| Combined pediatric intensive and emergency care | 1 (5) |
| Nonphysician healthcare provider | |
| Registered nurse/nurse practioner | 3 (13) |
| Resuscitation science researcher | 1 (4) |
| Median years of clinical experience (interquartile range) | 13.5 (9.0–18.0) |
| Gender | |
| Female | 14 (58) |
Definitions
During the first round of the modified eDelphi, consensus was reached for the definitions of potentially avoidable and unavoidable cardiac arrest. For the definition of potentially avoidable cardiac arrest, 33.3% of participants (n = 8) strongly agreed with the definition and 58.3% of participants (n = 14) agreed. For the definition of unavoidable cardiac arrest, all three scenarios reached greater than 90% of participants agreeing or strongly agreeing with the definition. For the definition of avoidable cardiac arrest, initial consensus was not reached with only 20 participants (83.3%) either agreeing or strongly agreeing with the definition. Following revision of the definition using the participant comments, it was presented again to the expert panel during Round 2, and 75.0% of participants (n = 18) strongly agreed and 16.7% (n = 4) agreed with the definition meeting consensus. See Table 2 for consensus results and definitions.
TABLE 2.
Definitions and Consensus Results From Round When Consensus Achieved
| Cardiac Arrest Type | Definition | Strongly Agree, % (n) | Agree, % (n) | Neither Agree Nor Disagree, % (n) | Disagree, % (n) | Strongly Disagree, % (n) |
|---|---|---|---|---|---|---|
|
| ||||||
| Unavoidable, consensus achieved in round 1 | Events that the PICU TEAM cannot prevent or avoidb | 68.1 (16.3) | 22.2 (5.3) | 5.6 (1.3) | 1.4 (0.3) | 2.7 (0.7) |
| CPR in progress | 75.0 (18) | 16.7 (4) | 4.2 (1) | 4.2 (1) | 0.0 (0) | |
| Terminal disease | 70.8 (17) | 20.8 (5) | 4.2 (1) | 0.0 (0) | 4.2 (1) | |
| Optimal care | 58.3. (14) | 29.2 (7) | 8.3 (2) | 0.0 (0) | 4.2 (1) | |
| Potentially avoidable, consensus achieved in round 1 | When a patient experiences care WITHIN THE PICU that is determined to be suboptimal and that patient later experiences a cardiac arrest that MAY OR MAY NOT be related to the suboptimal care. | 33.3 (8) | 58.3 (14) | 4.2 (1) | 4.2 (1) | 0.0 (0) |
| Avoidable, presented in round 1, consensus achieved in round 2 | Events in which deviations from accepted practice standards within the PICU lead directly to cardiac arresta. | 75.0 (18) | 16.7 (4) | 8.3 (2) | 0.0 (0) | 0.0 (0) |
Modified definition.
Averaged response.
Contributing Factors
The expert panel agreed with seven factors recommended from the literature (17–21) and achieved consensus on an additional seven factors identified by the study authors or expert panel. Due to consensus being reached on the importance of all 14 factors in the second round of the modified eDelphi, participants were also asked to rank contributing factors in order of importance and to rank the importance of factor categories (for summary of results, Appendix III, Supplemental Digital Content 3, http://links.lww.com/PCC/B397).
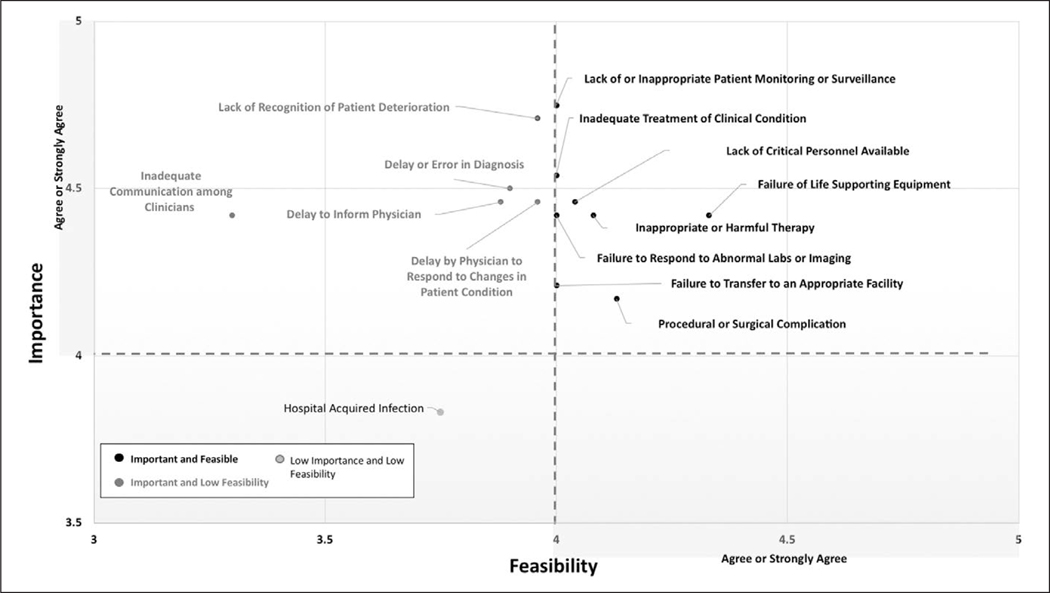
Factors were plotted to assess the relationship between feasibility and importance (Fig. 2) demonstrating that eight factors (57.1%) were thought to be feasible and important, five factors (35.7%) were thought to be important but not feasible to assess, and one factor (7.1%) was thought to be neither feasible nor important to assess. No factors were assessed as being feasible but not important.
Figure 2.
Each factor is plotted by feasibility score versus importance score. Score was determined by the average of the Likert Score (1 = strongly disagree, 2 = disagree, 3 = neither agree nor disagree, 4 = agree, 5 = strongly agree).
In-Person Session
Feedback during the in-person session demonstrated ongoing agreement with all three definitions reaching greater than 90% consensus. Seven members of the original eDelphi expert panel were also present at the in-person session and participated. In addition, during application of definitions to sample cases, there was 100% agreement with case definition. Consensus results from the in-person session as well as general feedback from participants is presented in Appendix IV (Supplemental Digital Content 4, http://links.lww.com/PCC/B398).
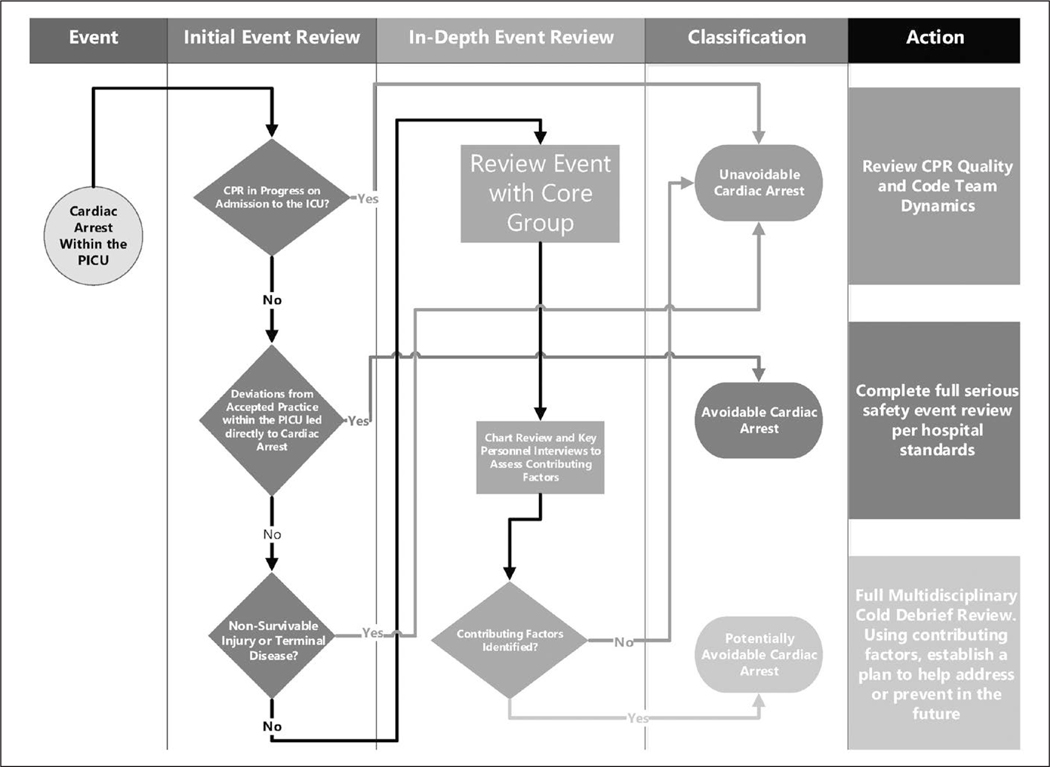
Proposed Framework for Event Review
The final result of the three rounds of eDelphi and the in-person session are presented in Figure 3 and consists of the following: (1) an initial event review to determine if an in-depth event review or a serious safety event review is needed; (2) an in-depth event review to identify possible contributing factors; (3) classification of events as avoidable, unavoidable, or potentially avoidable; and (4) recommended action for type of review. After each PICU IHCA, the framework would be applied and then we would expect the local version of the framework to be enriched with additional details regarding review participants, review specifics, and other important local factors.
Figure 3.
Proposed consensus-based framework for PICU in-hospital cardiac arrest event review based upon definitions and use of contributing factors. CPR = cardiopulmonary resucitation.
DISCUSSION
Through this modified eDelphi approach, we developed a consensus framework for classifying and reviewing PICU IHCA. This consensus has drawn on the contribution of a large panel of pediatric resuscitation experts who participated in the initial consensus gathering, as well as, an in-person session with further consensus, agreement, and application to assess feasibility of use of this work. We achieved consensus on definitions for avoidable, potentially avoidable, and unavoidable cardiac arrest within the PICU. In addition, we also achieved consensus on 14 factors that may contribute to potentially avoidable cardiac arrest to assist in evaluation of cases for review. Using these results, we developed a PICU IHCA review framework focused on identification of contributing factors that can be targeted for team- and system-level performance improvement efforts.
Improvement efforts within the PICU may be hampered by false reassurance that the care of the ICU patient is optimized due to the increased cardiorespiratory and hemodynamic monitoring and low nurse-patient ratio (31). This may lead to the belief that IHCA within the PICU is inevitable and therefore cannot be avoided. However, data from adult ICUs show that 10–40% of in-ICU IHCAs may be avoidable or potentially avoidable (18–20). As the number of pediatric IHCAs continue to shift to within the PICU, there is an acute need to identify avoidable cardiac arrests and develop tools to assist clinicians in preventing them. Through the use of our consensus framework including expert definitions and contributing factors, we propose that each PICU IHCA is reviewed using the framework to identify gaps in care and opportunities for improvement.
Prior work to identify avoidable cardiac arrests has focused on retrospective chart review and expert agreement without the establishment of clear a priori definitions (17–20). The advantage of the proposed framework and consensus definitions is to facilitate standardized review of PICU IHCA and development of metrics related to IHCA prevention. These consensus definitions of avoidable, potentially avoidable, and unavoidable PICU IHCAs can be used to identify cases on an ongoing basis that would most benefit from in-depth formal event review. Using the developed framework (Fig. 3), local resuscitation leaders will complete an initial event review, followed by a full more in-depth event review for events that meet criteria for potentially avoidable IHCA or otherwise do not meet the immediate definition of avoidable or unavoidable IHCA. It is our hope that an in-depth chart review and personnel interviews to assess contributing factors will enable resuscitation leaders to track possible contributing factors and, using quality improvement methodology, seek to reduce their impact on future events. We expect that institutions will customize the expert recommended list of contributing factors to their local context but recommend inclusion of the eight factors assessed to be feasible and important (Fig. 2). By identifying those cases most likely to benefit from review, we hope to decrease the burden of these reviews while optimizing lessons learned. Alternatively, we recommend that events meeting criteria for avoidable IHCA undergo a root cause analysis per local serious safety event review protocols (12). For events meeting criteria for unavoidable IHCA, we recommend a review of CPR quality and team dynamics which may improve future IHCA survival (11).
There are multiple limitations to this study. First, there is no established sample size required for an adequate Delphi process (32), so it is possible that we did not fully sample the range of opinions and possible contributing factors. However, our addition of an in-person session following the modified eDelphi attempted to address this limitation by further evaluating the definitions and attempting applicability with an audience of resuscitation experts and researchers. Second, our study is limited by the demographics of our respondents who represent mostly the United States. This may limit the generalizability of these results to PICU IHCA outside of the United States. Furthermore, we prioritized expertise in pediatric critical care as we sought to create definitions for IHCA within the PICU. These definitions may have limited applicability to other areas of the hospital including the cardiac ICU, emergency department, operating rooms, and general ward.
CONCLUSIONS
We used a multidisciplinary group of pediatric resuscitation experts to generate an eDelphi consensus-based frame- work to classify and review pediatric IHCA in the PICU. This framework and consensus definitions can be used as metrics for quality improvement efforts and benchmarking between institutions, as well as outcome measures for multicenter trials aimed at reduction in avoidable events. Future work will focus on the application of this framework and further validation of these definitions and contributing factors for IHCA both within and outside the PICU.
Supplementary Material
Acknowledgments
Dr. Kleinmann disclosed that she is a member of the American Heart Association Get with the Guidelines-Resuscitation Pediatric Research Task Force and the domain lead for International Liaison Committee on Resuscitation. Dr. Sutton’s institution received funding from the National Institutes of Health, and he disclosed that he is the Vice Chair of the Get with the Guidelines Resuscitation Pediatric Research Task Force. Dr. Wolfe received funding from Zoll Medical (speaking honoraria). The remaining authors have disclosed that they do not have any potential conflicts of interest.
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/pccmjournal).
REFERENCES
- 1.Holmberg MJ, Ross CE, Fitzmaurice GM, et al. ; American Heart Association’s Get With The Guidelines–Resuscitation Investigators: Annual incidence of adult and pediatric in-hospital cardiac arrest in the United States. Circ Cardiovasc Qual Outcomes 2019; 12:e005580 [PMC free article] [PubMed] [Google Scholar]
- 2.Girotra S, Spertus JA, Li Y, et al. ; American Heart Association Get With the Guidelines–Resuscitation Investigators: Survival trends in pediatric in-hospital cardiac arrests: An analysis from get with the guidelines-resuscitation. Circ Cardiovasc Qual Outcomes 2013; 6:42–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brady PW, Muething S, Kotagal U, et al. : Improving situation aware- ness to reduce unrecognized clinical deterioration and serious safety events. Pediatrics 2013; 131:e298–e308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aoki Y, Inata Y, Hatachi T, et al. : Outcomes of ‘unrecognised situation awareness failures events’ in intensive care unit transfer of children in a Japanese children’s hospital. J Paediatr Child Health 2019; 55:213–215 [DOI] [PubMed] [Google Scholar]
- 5.McClain Smith M, Chumpia M, Wargo L, et al. : Watcher initiative as- sociated with decrease in failure to rescue events in pediatric population. Hosp Pediatr 2017; 7:710–715 [DOI] [PubMed] [Google Scholar]
- 6.Sandquist M, Tegtmeyer K: No more pediatric code blues on the floor: Evolution of pediatric rapid response teams and situational aware- ness plans. Transl Pediatr 2018; 7:291–298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tibballs J, Kinney S: Reduction of hospital mortality and of prevent- able cardiac arrest and death on introduction of a pediatric medical emergency team. Pediatr Crit Care Med 2009; 10:306–312 [DOI] [PubMed] [Google Scholar]
- 8.Sharek PJ, Parast LM, Leong K, et al. : Effect of a rapid response team on hospital-wide mortality and code rates outside the ICU in a Children’s Hospital. JAMA 2007; 298:2267–2274 [DOI] [PubMed] [Google Scholar]
- 9.Berg RA, Sutton RM, Holubkov R, et al. ; Eunice Kennedy Shriver National Institute of Child Health and Human Development Collaborative Pediatric Critical Care Research Network and for the American Heart Association’s Get With the Guidelines-Resuscitation (formerly the National Registry of Cardiopulmonary Resuscitation) Investigators: Ratio of PICU versus ward cardiopulmonary resuscitation events is increasing. Crit Care Med 2013; 41:2292–2297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.de Mos N, van Litsenburg RR, McCrindle B, et al. : Pediatric in-intensive-care-unit cardiac arrest: Incidence, survival, and predictive factors. Crit Care Med 2006; 34:1209–1215 [DOI] [PubMed] [Google Scholar]
- 11.Wolfe H, Zebuhr C, Topjian AA, et al. : Interdisciplinary ICU cardiac arrest debriefing improves survival outcomes*. Crit Care Med 2014; 42:1688–1695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Phipps AR, Paradis M, Peterson KA, et al. : Reducing serious safety events and priority hospital-acquired conditions in a pediatric hospital with the implementation of a patient safety program. Jt Comm J Qual Patient Saf 2018; 44:334–340 [DOI] [PubMed] [Google Scholar]
- 13.Linstone HA, Turoff M: The Delphi Method: Techniques and Applications. Boston, MA, Addison-Wesley Publishing Company, 1975 [Google Scholar]
- 14.Kerlinger F: Foundations of Behavioral Research. New York, NY, Holt, Rinehart and Winston Inc, 1973 [Google Scholar]
- 15.Green RA: The Delphi technique in educational research [Internet]. SAGE Open 2014; 4:2158244014529773 [Google Scholar]
- 16.Toronto C: Considerations when conducting e-Delphi research: A case study. Nurse Res 2017; 25:10–15 [DOI] [PubMed] [Google Scholar]
- 17.Castle N, Kenward G, Hodgetts T: Avoidable cardiac arrest: Lessons for an A&E department. Accid Emerg Nurs 2003; 11:196–201 [DOI] [PubMed] [Google Scholar]
- 18.Galhotra S, DeVita MA, Simmons RL, et al. ; Members of the Medical Emergency Response Improvement Team (MERIT) Committee: Mature rapid response system and potentially avoidable cardiopulmo- nary arrests in hospital. Qual Saf Health Care 2007; 16:260–265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hodgetts TJ, Kenward G, Vlachonikolis IG, et al. : The identification of risk factors for cardiac arrest and formulation of activation criteria to alert a medical emergency team. Resuscitation 2002; 54:125–131 [DOI] [PubMed] [Google Scholar]
- 20.Moskowitz A, Berg KM, Cocchi MN, et al. : Cardiac arrest in the intensive care unit: An assessment of preventability. Resuscitation 2019; 145:15–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bingham G, Bilgrami I, Sandford M, et al. : Avoiding adult in-hospital cardiac arrest: A retrospective cohort study to determine preventa- bility. Aust Crit Care 2018; 31:219–225 [DOI] [PubMed] [Google Scholar]
- 22.de Caen AR, Maconochie IK, Aickin R, et al. ; Pediatric Basic Life Support and Pediatric Advanced Life Support Chapter Collaborators: Part 6: Pediatric basic life support and pediatric advanced life support: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Circulation 2015; 132:S177–S203 [DOI] [PubMed] [Google Scholar]
- 23.Johnson TP: Snowball sampling: Introduction. Wiley StatsRef: Statistics Reference Online; (Balakrishnan N, Colton T, Everitt B, et al, Eds). 2014 [Google Scholar]
- 24.Ogden SR, Culp WC Jr, Villamaria FJ, et al. : Developing a checklist: Consensus via a modified Delphi technique. J Cardiothorac Vasc Anesth 2016; 30:855–858 [DOI] [PubMed] [Google Scholar]
- 25.Ager A, Stark L, Akesson B, et al. : Defining best practice in care and protection of children in crisis-affected settings: A Delphi study. Child Dev 2010; 81:1271–1286 [DOI] [PubMed] [Google Scholar]
- 26.Kerckhoffs MC, Senekal J, van Dijk D, et al. : Framework to support the process of decision-making on life-sustaining treatments in the ICU: Results of a Delphi study. Crit Care Med 2020; 48:645–653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rickard AC, Vassallo J, Nutbeam T, et al. ; PERUKI (Paediatric Emergency Research in the UK and Ireland): Paediatric traumatic cardiac arrest: A Delphi study to establish consensus on definition and management. Emerg Med J 2018; 35:434–439 [DOI] [PubMed] [Google Scholar]
- 28.Krmpotic K, Van den Bruel A, Lobos AT: A modified Delphi study to identify factors associated with clinical deterioration in hospitalized children. Hosp Pediatr 2016; 6:616–625 [DOI] [PubMed] [Google Scholar]
- 29.Sumsion T: The Delphi technique: An adaptive research tool. Br J Occup Ther 1998; 61:153–156. [Google Scholar]
- 30.Schwartz HP, Bigham MT, Schoettker PJ, et al. ; American Academy of Pediatrics Section on Transport Medicine: Quality metrics in neonatal and pediatric critical care transport: A National Delphi Project. Pediatr Crit Care Med 2015; 16:711–717 [DOI] [PubMed] [Google Scholar]
- 31.Armstrong RA, Kane C, Oglesby F, et al. : The incidence of cardiac arrest in the intensive care unit: A systematic review and meta-analysis. J Intensive Care Soc 2019; 20:144–154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jones J, Hunter D: Consensus methods for medical and health services research. BMJ 1995; 311:376–380 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.