Abstract
The association of smell and taste loss with COVID-19 has been well demonstrated with high prevalence rates. In certain cases, chemosensory loss may be the only symptom of COVID-19 and may linger while other symptoms have resolved. The significance of persistent smell and taste loss and its relationship to ongoing viral shedding has yet to be investigated. In this cross-sectional study, of the 316 laboratory test–confirmed COVID-19 cases at our institution, 46 had subsequent test-based confirmation of viral clearance with 2 consecutive negative RT-PCR test results (reverse transcriptase polymerase chain reaction). Olfactory dysfunction was reported by 50% of the patients (23 of 46), with 78% (18 of 23) having subjective persistent smell loss despite negative RT-PCR test results. These preliminary data demonstrate the persistence of self-reported smell loss despite otherwise clinical resolution and undetectable nasal viral RNA.
Keywords: smell loss, COVID-19, health care workers, SARS-CoV-2, health care policy
Loss of smell and taste has been identified as a distinct clinical feature of COVID-19 and was recently recognized by the Centers for Disease Control and Prevention,1 as well as an increasing number of other national health organizations around the world. We and others have reported a high prevalence of chemosensory dysfunction in patients with SARS-CoV-2 confirmed by reverse transcriptase polymerase chain reaction (RT-PCR).2–7 In certain cases of COVID-19, loss of smell and taste may be the initial or only presenting symptom.5
The time frame for chemosensory recovery needs further evidence-based explication, but preliminary results have suggested that a majority of patients notice an improvement by 2 to 4 weeks postdiagnosis, often trailing the resolution of their other symptoms.2,8 However, for those who do not experience recovery of their smell and taste, there is potential concern that these symptoms may be linked to longer viral loads in the upper aerodigestive tract.9
In particular, the persistent loss of smell and taste as an isolated COVID-19 symptom may be concerning and difficult to interpret for essential personnel trying to return to the work environment, including health care workers. Currently, the Centers for Disease Control and Prevention’s return-to-work criteria for health care workers include resolution of fever, improvement of respiratory symptoms, and, if possible, a test-based strategy with 2 negative consecutive laboratory-confirmed COVID-19 results.10 The significance of other persistent symptoms, such as chemosensory loss, and its relationship to ongoing viral shedding has yet to be investigated. There is much to be elucidated on the pathophysiology of SARS-CoV-2-induced olfactory dysfunction. Understanding the relationship between self-reported chemosensory dysfunction and the presence of SARS-CoV-2 could help formulate recommendations for self-quarantine and return-to-work policies.
Methods
We reviewed the electronic medical records of patients at our institution who were diagnosed between March 9 and April 29, 2020, with SARS-CoV-2 by RT-PCR from nasal cavity samples and subsequently demonstrated clearance of nasal viral RNA by 2 consecutive negative RT-PCR test results. In this patient subset, COVID-19-associated olfactory function was evaluated first through review of electronic medical records and then with confirmation via a phone-based questionnaire. Patients were asked to rate their sense of smell on a 10-point scale (0, complete anosmia; 10, normal smell) at their premorbid baseline, at time of initial COVID-19 testing, and at present survey date. This study was approved by the Institutional Review Board of University of California San Diego Health (200485).
Results
Of the 316 patients who initially tested COVID-19 positive, 46 subsequently had laboratory-confirmed undetectable viral RNA through 2 consecutive negative RT-PCR test results.
Olfactory dysfunction was reported by 23 of these patients (17 reported no loss, 5 were unreachable, 1 had died). The average time between respondents’ initial RT-PCR diagnosis of COVID-19 and their first negative swab result was 16.2 days (interquartile range, 9–22.3). The average time elapsed between their negative diagnosis and survey date was 9.4 days (interquartile range, 3.8–14.8). For the 23 respondents with viral-associated chemosensory loss, mean baseline olfaction score was 9.4, with a nadir of 2.0 (Δ = −7.4) at time of illness and a current score of 7.4 (Δ = −2.0; Figure 1). At the time of the survey following negative RT-PCR test findings, 5 patients reported full recovery of olfaction, while the remaining (18 of 23, 78%) reported continued subjective chemosensory dysfunction. In contrast, 78% of patients reported complete resolution of all other symptoms.
Figure 1.
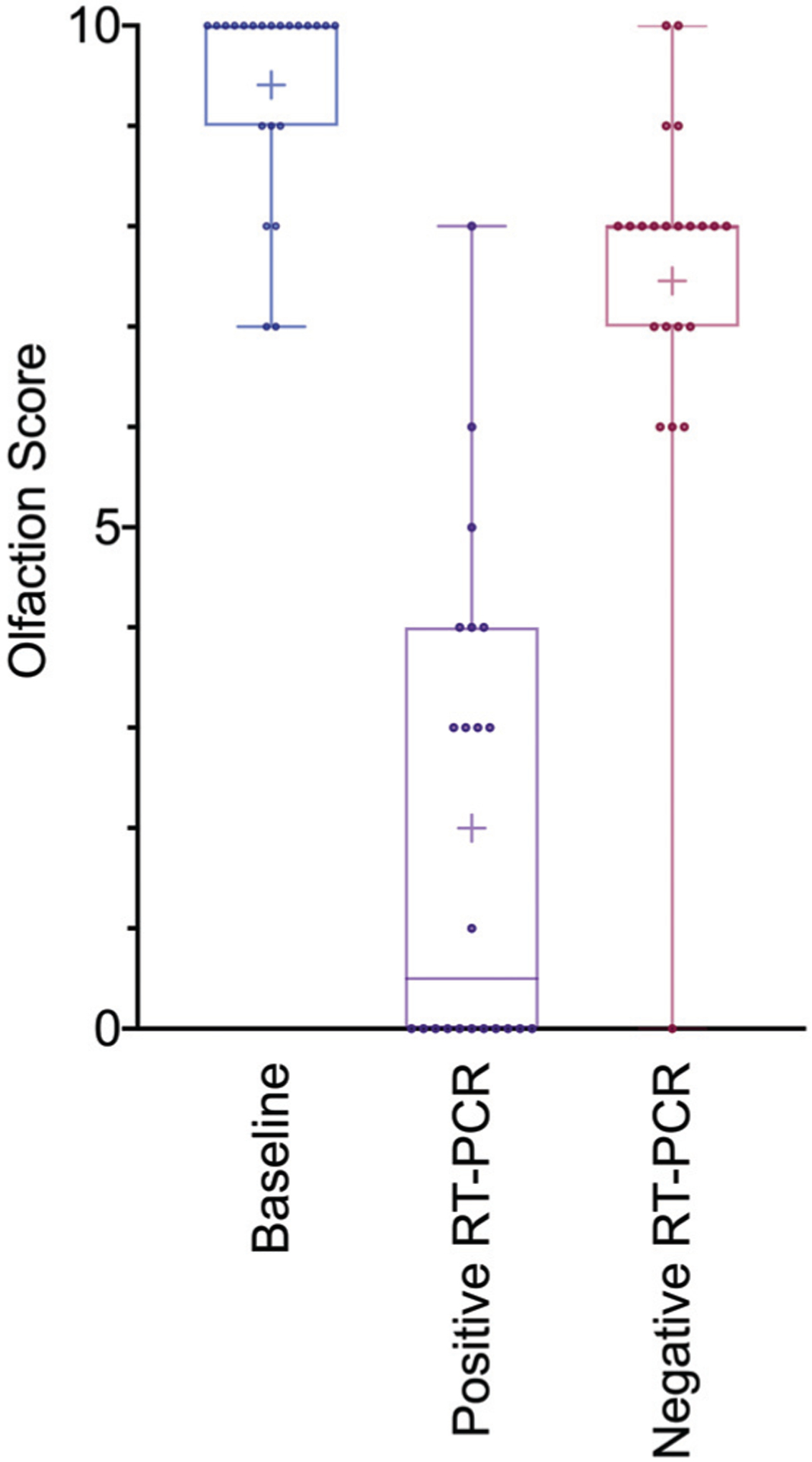
Relationship between olfaction scores and COVID-19 RT-PCR status. Box and whisker plot show olfaction scores at baseline, time of positive RT-PCR testing, and time of survey (following negative RT-PCR results). Whiskers represent minimum and maximum values; boxes indicate interquartile range; and the horizontal line within the box represents the median value. The mean value is denoted by the plus sign, +. RT-PCR, reverse transcriptase polymerase chain reaction.
Discussion
Self-perceived smell loss may persist despite the resolution of viral infection and shedding as determined by serial RT-PCR. Although RT-PCR false-negative rates are well described,11 the patients included in this study underwent 2 consecutive tests separated by >24 hours. This preliminary study sheds lights on an important question whether persistent chemosensory symptoms are linked to persistent viral loads and thus viral transmissibility. These findings may help guide return-to-work policies for essential workers, including health care providers.
This study was limited by its small numbers and delayed follow-up from time of negative diagnosis to time of survey, which may underestimate the severity of persistent olfactory dysfunction. Furthermore, we did not assess for smell loss using quantitative measures, as our primary focus was to evaluate the correlation of symptomatology and viral burden. Here we demonstrate the persistence of self-reported smell loss despite otherwise clinical resolution and undetectable nasal viral RNA. These findings support a safe return to work despite persistent smell loss.
Funding source:
The project described was partially supported by the National Institutes of Health (grant UL1TR001442; Clinical and Translational Science Awards).
Footnotes
Competing interests: Adam S. DeConde, has received consulting fees from Olympus, Stryker Endoscopy, Sanofi, and Optinose (none of which were relevant to this study).
References
- 1.Centers for Disease Control and Prevention. Symptoms of coronavirus. Accessed May 1, 2020. https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html
- 2.Yan CH, Faraji F, Prajapati DP, Boone CE, DeConde AS. Association of chemosensory dysfunction and COVID-19 in patients presenting with influenza-like symptoms. Int Forum Allergy Rhinol. Published online April 15, 2020. doi: 10.1002/alr.22579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kaye R, Chang CWD, Kazahaya K, Brereton J, Denneny JC. COVID-19 anosmia reporting tool: initial findings. Otolaryngol Head Neck Surg. Published online April 28, 2020. doi: 10.1177/0194599820922992 [DOI] [PubMed] [Google Scholar]
- 4.Menni C, Valdes AM, Freidin MB, et al. Real-time tracking of self-reported symptoms to predict potential COVID-19. Nat Med. Published online May 11, 2020. doi: 10.1038/s41591-020-0916-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spinato G, Fabbris C, Polesel J, et al. Alterations in smell or taste in mildly symptomatic outpatients with SARS-CoV-2 infection. JAMA. Published online April 22, 2020. doi: 10.1001/jama.2020.6771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Giacomelli A, Pezzati L, Conti F, et al. Self-reported olfactory and taste disorders in SARS-CoV-2 patients: a cross-sectional study. Clin Infect Dis. Published online March 26, 2020. doi: 10.1093/cid/ciaa330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lechien JR, Chiesa-Estomba CM, De Siati DR, et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Eur Arch Otorhinolaryngol. Published online April 6, 2020. doi: 10.1007/s00405-020-05965-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hopkins C, Surda P, Whitehead E, Kumar BN. Early recovery following new onset anosmia during the COVID-19 pandemic—an observational cohort study. J Otolaryngol Head Neck Surg. 2020;49(1):26. doi: 10.1186/s40463-020-00423-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hopkins C, Vaira LA, De Riu G. Self-reported olfactory loss in COVID-19: is it really a favorable prognostic factor? Int Forum Allergy Rhinol. Published online May 12, 2020. doi: 10.1002/alr.22608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Criteria for return to work for healthcare personnel with suspected or confirmed COVID-19 (interim guidance). Accessed May 1, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/return-to-work.html
- 11.Kim H, Hong H, Yoon SH. Diagnostic performance of CT and reverse transcriptase-polymerase chain reaction for coronavirus disease 2019: a meta-analysis. Radiology. Published online April 17, 2020. doi: 10.1148/radiol.2020201343 [DOI] [PMC free article] [PubMed] [Google Scholar]


