Abstract
Background
The COVID-19 pandemic caused disruptions in the delivery of health services, which may have adversely affected access to substance use disorder (SUD) treatment services. Medicaid expansion has been previously associated with increased access to SUD services for low-income adults. Thus, the pandemic may have differentially impacted overdose mortality depending on expansion status. This study examined trends in overdose mortality nationally and by state Medicaid expansion status from 2013 to 2020.
Methods
State-level data on overdose mortality were obtained from the Centers for Disease Control and Prevention’s WONDER database for 2013–2020 (N = 408 state-years). The primary outcomes were drug and opioid overdose deaths per 100,000 residents. The primary exposure was Medicaid expansion status as of January 1st, 2020. Difference-in-difference (DID) models were used to compare changes in outcomes between expansion and non-expansion states after the onset of the COVID-19 pandemic.
Results
The U.S. experienced 91,799 drug overdose deaths in 2020, a 29.9% relative increase from 2019. Expansion states experienced an adjusted increase of 7.0 drug overdose deaths per 100,000 residents (95% CI 3.3, 10.7) and non-expansion states experienced an increase of 4.3 deaths (95% CI 1.5, 8.2) from 2019 to 2020. Similar trends were observed in opioid overdose deaths. In DID models, Medicaid expansion was not associated with changes in drug (0.9 deaths, 95% CI −2.0, 3.7) or opioid overdose deaths (0.8 deaths, 95% CI −1.8, 3.5).
Conclusions
The increase in drug or opioid overdose deaths experienced during the first year of the COVID-19 pandemic was similar in states with and without Medicaid expansion.
Keywords: Medicaid, Substance use disorder, Opioid use disorder, Overdose mortality, COVID-19
1. Introduction
The U.S. experienced persistently high rates of drug overdose mortality during the last two decades, and the COVID-19 pandemic may have exacerbated this public health crisis. The pandemic caused disruptions in both insurance coverage and the delivery of health services, which may have adversely affected access to substance use disorder (SUD) treatment services (Wakeman et al., 2020). Disruption of SUD treatment services can be particularly harmful for those engaged in treatment for opioid use disorder (OUD). Medication for opioid use disorder (MOUD) (e.g. buprenorphine, methadone) is the recommended treatment for OUD, and its use markedly decreases the risk of opioid-related disease, overdose, and death (National Academies of Sciences, Engineering, 2019). However, access to MOUD is often predicated on in-person visits to a health care provider able to prescribe these life-saving medications (Lagisetty et al., 2017). During the COVID-19 pandemic, regulations that required in-person initiation of buprenorphine/suboxone were lifted and many providers began to offer telehealth to improve access to these medications (Substance Abuse and Mental Health Services Administration, 2020). Regulations for methadone administration were also relaxed, and the number of allowable methadone take-home doses for the treatment of OUD increased in March 2020 (Levander et al., 2021). Despite these changes, many with SUDs reported they were still unable to access needed services (Mellis et al., 2021).
Historically, access to SUD treatment has been generally higher in states that expanded Medicaid compared to those that have not (Abraham et al., 2017, Wen et al., 2017). Beginning in 2014, the Affordable Care Act (ACA) allowed states to expand Medicaid coverage for low-income adults and required Medicaid expansion states to cover substance use disorder services with similar cost-sharing as medical and surgical services (Kravitz-Wirtz et al., 2020). Medicaid insures a disproportionate share of persons with OUD, and Medicaid expansion had facilitated improved access to MOUD compared to non-expansion states prior to the pandemic (Wen et al., 2017). Moreover, Medicaid expansion has previously been associated with greater declines in rates of drug (Venkataramani and Chatterjee, 2019) and opioid overdose deaths (Kravitz-Wirtz et al., 2020). However, it is unclear if the protective effects of Medicaid expansion continued after the onset of the COVID-19 pandemic.
Medicaid served as an important safety-net for many who lost employer-sponsored insurance coverage during the pandemic (Bundorf et al., 2021), as many who experienced pandemic-related job loss were able to maintain health insurance coverage through Medicaid enrollment (Khorrami and Sommers, 2021). Insurance coverage is often an important prerequisite to accessing health services. However, the COVID-19 pandemic interrupted access to health services, including SUD and harm reduction services (Mellis et al., 2021). Moreover, policies that reduce the spread of COVID-19 (e.g., social distancing) can have the unintended consequence of social isolation and despair, both of which can intensify substance use (Wakeman et al., 2020). Taken together, it is possible that the COVID-19 blunted the previously established protective effects of Medicaid expansion. By the beginning of 2020, 36 states and the District of Columbia had elected to expand Medicaid eligibility to low-income adults. While drug overdose deaths increased during the COVID-19 pandemic, no research has examined if drug or opioid overdose mortality differed between Medicaid expansion and non-expansion states during the pandemic. In this cross-sectional study, we examined trends in drug overdose mortality nationally from 2013 to 2020, and if trends changed depending on state Medicaid expansion status after the onset of the COVID-19 pandemic.
2. Methods
We obtained annual, state-level data on drug and opioid overdose deaths from January 1st, 2013 through December 31st, 2020 from the Centers for Disease Control and Prevention’s (CDC) WONDER database (National Center for Health Statistics, 2020). We identified drug overdose deaths using International Classification of Disease (ICD-10), tenth edition underlying cause-of-death codes X40–44, X60–64, X85, and Y10–14. Among deaths with drug overdose as the underlying cause, opioid overdose deaths were identified using ICD-10 multiple cause-of-death codes T40.1 (heroin), T40.2 (other opioids), T40.3 (methadone), T40.4 (other synthetic narcotics), and T40.6 (other and unspecified narcotics). Rates of drug and opioid overdose deaths were calculated as the number of deaths per 100,000 residents. Data on state characteristics were obtained from the Area Health Resource File (Griffith et al., 2021) and lagged two years due to data availability. Data on state Medicaid expansion status was obtained from the Kaiser Family Foundation. States that expanded Medicaid eligibility to low-income adults by January 1st, 2020 were considered as Medicaid expansion states (Kaiser Family Foundation, 2020).
To estimate the association between state Medicaid expansion and trends in drug and opioid overdose mortality, we estimated two types of models using ordinary least squares (OLS) regression. For all models, the pre-period ran from 2013 to 2019 and the post-period was 2020. First, we used interrupted time series (ITS) models to estimate changes in drug and opioid overdose mortality in 2020, controlling for pre-pandemic outcome levels and state characteristics. This allowed us to identify changes that occurred in 2020, the first year of the COVID-19 pandemic.
Next, difference-in-differences (DID) regression models were estimated to contrast changes in drug and opioid overdose deaths between expansion and non-expansion states after the onset of the COVID-19 pandemic. The DID estimate can be interpreted as the differential change in drug and opioid overdose deaths between Medicaid expansion and non-expansion states from 2019 to 2020. Models were adjusted for several covariates that have previously been associated with drug overdose mortality including percent male, percent over 65 years of age, percent unemployed, percent earning less than the federal poverty limit, and physicians per 100,000 residents (Haffajee et al., 2019). Covariates that may be on the causal pathway between the COVID-19 pandemic and overdose mortality during 2020 (e.g. unemployment) were excluded as these variables may bias results (Schisterman et al., 2009). All models included state and year fixed effects, with robust standard errors clustered at the state level. The unit of observation was the state-year, and the analytic sample included all fifty states and the District of Columbia (N = 408 state-years). Analyzes were conducted in STATA/MP version 16.1.
3. Results
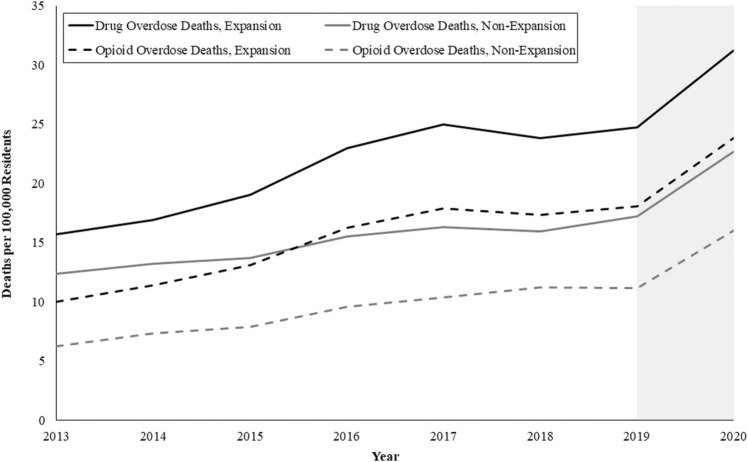
The U.S. experienced 91,799 drug overdose deaths in 2020 – a 29.9% relative increase from 2019 ( Fig. 1). The majority of drug overdose deaths were opioid-related, with 68,630 individuals dying of an opioid overdose in 2020 – a 37.6% increase from 2019 (Fig. 1). Nationally, the rate of drug overdose deaths increased from 22.5 (SD 9.6) to 28.7 (SD 12.7) deaths per 100,000 residents from 2019 to 2020, a difference of 6.1 deaths (95% CI 1.7, 10.6). A concomitant increase occurred in opioid overdose deaths nationally, with opioid overdose deaths increasing from 16.0 (SD 9.6) in 2019–21.5 (SD 12.3) in 2020 – a difference of 5.5 deaths (95% CI 1.1, 9.8).
Fig. 1.
Trends in drug and opioid overdose deaths per 100,000 residents by state Medicaid expansion status from 2013 to 2020. Notes. The figure displays annual drug and opioid overdose death rates from the Centers for Disease Control and Prevention WONDER database. The shaded area indicates the onset of the COVID-19 pandemic (2020).
ITS models revealed that both Medicaid expansion and non-expansion states experienced significant increases in drug and opioid overdose deaths. Expansion states experienced an adjusted increase of 7.0 drug overdose deaths per 100,000 residents (95% CI 3.3, 10.7) and non-expansion states experienced an increase of 4.3 (95% CI 1.5, 8.2) overdose deaths from 2019 to 2020 ( Table 1). Similarly, expansion states experienced an adjusted increase of 6.0 opioid overdose deaths per 100,000 residents (95% CI 2.4, 9.7) and non-expansion states experienced an increase of 3.6 (95% CI 0.6, 6.6) opioid overdose deaths from 2019 to 2020 (Table 1). Parallel trends were observed for both drug and opioid overdose deaths between Medicaid expansion and non-expansion states prior to the COVID-19 pandemic (Fig. 1). In DID models, Medicaid expansion was not associated with changes in drug overdose deaths (0.9 deaths per 100,000, 95% CI −2.0, 3.7) or opioid overdose deaths (0.8 deaths per 100,000 residents, 95% CI −1.8, 3.5).
Table 1.
Changes in Drug and Opioid Overdose Deaths Nationally and Stratified by Medicaid Expansion from 2019 to 2020.
| Rate of Drug Overdose Deathsa |
Change 2019–2020b (95% CI) |
Rate of Opioid Overdose Deathsa |
Change 2019–2020b (95% CI) |
|||
|---|---|---|---|---|---|---|
| 2019 M (SD) |
2020 M (SD) |
2019 M (SD) |
2020 M (SD) |
|||
| Medicaid Expansionc | 24.7 (9.9) | 31.2 (13.3) | 7.0 (3.3, 10.8)*** | 18.1 (10.1) | 23.8 (12.8) | 6.0 (2.4, 9.7)*** |
| Non-Medicaid Expansionc | 17.2 (6.5) | 22.6 (9.8) | 4.8 (1.5, 8.2)** | 11.2 (6.1) | 16.0 (9.2) | 4.6 (0.6, 6.6)* |
Notes: All estimates are expressed as adjusted rates per 100,000 per residents by year.
*p<0.05, ** p <0.01, ***p <0.001.
Unadjusted rates
Results from ordinary least squares (OLS) interrupted time series (ITS) models including state and year fixed effects with robust standard errors clustered at the state level.
Medicaid expansion status was a binary indicator taking on a value of 1 for states which expanded Medicaid income eligibility for childless adults under the Affordable Care Act by January 1, 2020, 0 otherwise.
4. Discussion
This study found that drug and opioid overdose deaths rose markedly in 2020. The U.S. experienced the single largest annual increase in drug overdose mortality in more than two decades, confirming fears the COVID-19 pandemic and related factors may fuel surges in overdose deaths (Wakeman et al., 2020). This is the first known study to examine the association of Medicaid expansion and drug overdose mortality during the first year of the COVID-19 pandemic, and results suggest that Medicaid expansion was not associated with changes in the rate of either drug or opioid overdose deaths. Low-income adults with SUDs face increased barriers to evidence-based care when uninsured. Medicaid expansion does not guarantee access to SUD or harm reduction services, but it can promote access through health insurance coverage (Olfson et al., 2021). Prior to the pandemic, Medicaid expansion improved access to a host of SUD-related services (McCarty et al., 2018, Shover et al., 2019, Wen et al., 2017) that reduce the risk of overdose mortality. However, similar increases in drug overdose deaths in Medicaid expansion and non-expansion states suggests that policies that had previously supported access to SUD and harm reduction services in expansion states were insufficient during the first year of the COVID-19 pandemic.
In the absence of a global pandemic, access to SUD and harm reduction services is limited and often predicated on in-person visits, which can be difficult to impossible for those without the resources (e.g., transportation, housing, childcare, etc.) to present to care. While Medicaid has historically improved access to health services, the COVID-19 pandemic introduced new barriers to care that insurance coverage alone cannot surpass. The intersection of the pandemic and the overdose epidemic in the U.S. likely fueled existing disparities associated with substance use and healthcare access (e.g., housing instability, food insecurity, poverty, comorbidities) (Sharma and Batra, 2021), contributing to similarly increased rates of overdose mortality in expansion and non-expansion states. These results highlight the vulnerability of this population, and demonstrate a critical need to remove barriers and expand the settings where people can access SUD and harm reduction services.
Policies in the U.S. limit the supply of providers who can prescribe MOUD (Auty et al., 2020), the availability of opioid overdose reversing medications (i.e., Narcan, Naloxone) (Davis and Carr, 2017, Sohn et al., 2019), and access to safe injection sites for individuals who inject drugs (Levengood et al., 2021). The administration of all types of MOUD is highly regulated in the U.S. Policy changes that allowed telehealth initiation of buprenorphine and increased the number of methadone take-home doses during the pandemic likely did not increase access substantially enough to meet the demand for these services (Mellis et al., 2021). Increasing access to buprenorphine through emergency medical services (EMS) personnel (Davis et al., 2021) and clinical pharmacists (Peckham et al., 2021) may be a critical step to ensure widespread access for those in need. Policies that support Naloxone access (e.g., standing orders, health plan coverage) reduce the risk of overdose mortality (Sohn et al., 2020, Sohn et al., 2019), yet are inconsistently implemented across the United States. Residents of Medicaid expansion states have historically benefited from improved access to Naloxone (Sohn et al., 2020), but it is unknown if these trends persisted during the COVID-19 pandemic. In light of rising rates of fatal opioid overdose, states should consider implementing Naloxone leave-behind laws that allow EMS personnel to distribute Naloxone after an overdose event to bystanders (Scharf et al., 2021, Wood et al., 2021). Finally, while the majority of fatal overdose events involve opioids, others who use certain drugs (e.g., psychostimulants) are also at risk of overdose death. Safe-injection sites can reduce the risk of death and improve linkage to SUD services, but only one site exists in the U.S. (Levengood et al., 2021). In combination with Medicaid expansion, widespread implementation of harm reduction policies may stem rising rates of overdose mortality.
5. Limitations
This study has several limitations that warrant consideration. First, we were only able to capture drug overdose deaths that occurred in 2020. Trends in drug overdose mortality may differ in 2021 after health systems made changes to support access to care during the pandemic. Second, the CDC WONDER data relies on ICD-10 coding of death certificate data, which may misclassify the substances involved in fatal overdoses and lead to an underestimation of opioid overdose mortality (Kravitz-Wirtz et al., 2020). Third, our study design does not allow us to account for specific state/federal policy changes made during the COVID-19 pandemic that may have impacted drug and opioid overdose mortality. Future research might consider exploring the mechanisms through which these policy changes may have differentially impacted drug overdose mortality in Medicaid expansion and non-expansion states.
6. Conclusions
The COVID-19 pandemic exposed critical gaps in the delivery system of SUD and harm reduction services, which may have contributed to similar increases in the rates of drug and opioid overdose deaths in Medicaid expansion and non-expansion states. To prevent additional and unnecessary loss of human life, the federal government and states should take immediate action to improve access to SUD and harm reduction services.
Funding statement
Ms. Auty’s effort was supported by the National Institute of Drug Abuse [T32-DA041898–03]. Dr. Griffith’s effort was supported by the Agency for Healthcare Research & Quality [K12 HS026395].
CRediT authorship contribution statement
Samantha G. Auty: Conceptualization, Formal analysis, Data curation, Writing – original draft, Writing – review & editing, Visualization. Kevin N. Griffith: Conceptualization, Writing – review & editing, Supervision.
Acknowledgements
None.
Conflicts of interest
The authors have no conflicts of interest to disclose.
Author disclosures
The authors have nothing to disclose.
References
- Abraham A.J., Andrews C.M., Grogan C.M., D’Aunno T., Humphreys K.N., Pollack H.A., Friedmann P.D. The affordable care act transformation of substance use disorder treatment. Am. J. Public Health. 2017 doi: 10.2105/AJPH.2016.303558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auty S.G., Stein M.D., Walley A.Y., Drainoni M.-L. Buprenorphine waiver uptake among nurse practitioners and physician assistants: the role of existing waivered prescriber supply. J. Subst. Abus. Treat. 2020 doi: 10.1016/j.jsat.2020.108032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bundorf, M.K., Gupta, S., Kim, C., 2021. Trends in US Health Insurance Coverage During the COVID-19 Pandemic, in: JAMA Health Forum. American Medical Association, pp. e212487–e212487. [DOI] [PMC free article] [PubMed]
- Davis C., Carr D. State legal innovations to encourage naloxone dispensing. J. Am. Pharm. Assoc. 2017;57:S180–S184. doi: 10.1016/j.japh.2016.11.007. [DOI] [PubMed] [Google Scholar]
- Davis C.S., Carr D.H., Glenn M.J., Samuels E.A. Legal authority for emergency medical services to increase access to buprenorphine treatment for opioid use disorder. Ann. Emerg. Med. 2021 doi: 10.1016/j.annemergmed.2021.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffith K.N., Feyman Y., Auty S.G., Crable E.L., Levengood T.W. County-level data on U.S. opioid distributions, demographics, healthcare supply, and healthcare access. Data Br. 2021;35 doi: 10.1016/j.dib.2021.106779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haffajee R.L., Lin L.A., Bohnert A.S.B., Goldstick J.E. Characteristics of US counties with high opioid overdose mortality and low capacity to deliver medications for opioid use disorder. JAMA Netw. Open. 2019;2 doi: 10.1001/jamanetworkopen.2019.6373. e196373–e196373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser Family Foundation, 2020. Status of State Action on the Medicaid Expansion Decision [WWW Document]. URL 〈https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/〉 (accessed 12.23.20).
- Khorrami P., Sommers B.D. Changes in US medicaid enrollment during the COVID-19 pandemic. JAMA Netw. Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.9463. e219463–e219463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kravitz-Wirtz N., Davis C.S., Ponicki W.R., Rivera-Aguirre A., Marshall B.D.L., Martins S.S., Cerdá M. Association of medicaid expansion with opioid overdose mortality in the United States. JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.2019.19066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lagisetty P., Klasa K., Bush C., Heisler M., Chopra V., Bohnert A. Primary care models for treating opioid use disorders: what actually works? A systematic review. PLoS One. 2017;12 doi: 10.1371/journal.pone.0186315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levander X.A., Pytell J.D., Stoller K.B., Korthuis P.T., Chander G. COVID-19-related policy changes for methadone take-home dosing: a multistate survey of opioid treatment program leadership. Subst. Abus. 2021:1–7. doi: 10.1080/08897077.2021.1986768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levengood T.W., Yoon G.H., Davoust M.J., Ogden S.N., Marshall B.D.L., Cahill S.R., Bazzi A.R. Supervised injection facilities as harm reduction: a systematic review. Am. J. Prev. Med. 2021;61:738–749. doi: 10.1016/j.amepre.2021.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarty D., Gu Y., Renfro S., Baker R., Lind B.K., McConnell K.J. Access to treatment for alcohol use disorders following Oregon’s health care reforms and Medicaid expansion. J. Subst. Abus. Treat. 2018;94:24–28. doi: 10.1016/j.jsat.2018.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mellis A.M., Potenza M.N., Hulsey J.N. COVID-19-related treatment service disruptions among people with single-and polysubstance use concerns. J. Subst. Abus. Treat. 2021;121 doi: 10.1016/j.jsat.2020.108180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and M . Medications for Opioid Use Disorder Save Lives. National Academies Press,; US: 2019. Medications for Opioid Use Disorder Save Lives. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics, 2020. Multiple Cause of Death 1999–2019 on CDC WONDER Online Database.
- Olfson M., Wall M., Barry C.L., Mauro C., Feng T., Mojtabai R. Medicaid expansion and low-income adults with substance use disorders. J. Behav. Health Serv. Res. 2021;48:477–486. doi: 10.1007/s11414-020-09738-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peckham A.M., Ball J., Colvard M.D., Dadiomov D., Hill L.G., Nichols S.D., Tallian K., Ventricelli D.J., Tran T.H. Leveraging pharmacists to maintain and extend buprenorphine supply for opioid use disorder amid COVID-19 pandemic. Am. J. Health Pharm. 2021;78:613–618. doi: 10.1093/ajhp/zxab003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scharf B.M., Sabat D.J., Brothers J.M., Margolis A.M., Levy M.J. Best practices for a novel EMS-based naloxone leave behind program. Prehosp. Emerg. Care. 2021;25:418–426. doi: 10.1080/10903127.2020.1771490. [DOI] [PubMed] [Google Scholar]
- Schisterman E.F., Cole S.R., Platt R.W. Overadjustment bias and unnecessary adjustment in epidemiologic studies. Epidemiology. 2009;20:488–495. doi: 10.1097/EDE.0b013e3181a819a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma M., Batra K. Syndemic of opioid crisis and COVID-19 pandemic: a call to invest in solutions. J. Alcohol Drug Educ. 2021;65:5–12. [Google Scholar]
- Shover C.L., Abraham A., D’Aunno T., Friedmann P.D., Humphreys K. The relationship of Medicaid expansion to psychiatric comorbidity care within substance use disorder treatment programs. J. Subst. Abus. Treat. 2019;105:44–50. doi: 10.1016/j.jsat.2019.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sohn M., Talbert J.C., Delcher C., Hankosky E.R., Lofwall M.R., Freeman P.R. Association between state Medicaid expansion status and naloxone prescription dispensing. Health Serv. Res. 2020;55:239–248. doi: 10.1111/1475-6773.13266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sohn M., Talbert J.C., Huang Z., Lofwall M.R., Freeman P.R. Association of naloxone coprescription laws with naloxone prescription dispensing in the United States. JAMA Netw. Open. 2019;2 doi: 10.1001/jamanetworkopen.2019.6215. e196215–e196215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration, 2020. Provision of methadone and buprenorphine for the treatment of Opioid Use Disorder in the COVID-19 emergency.
- Venkataramani A.S., Chatterjee P. Early Medicaid expansions and drug overdose mortality in the USA: a quasi-experimental analysis. J. Gen. Intern. Med. 2019;34:23–25. doi: 10.1007/s11606-018-4664-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakeman S.E., Green T.C., Rich J. An overdose surge will compound the COVID-19 pandemic if urgent action is not taken. Nat. Med. 2020;26:819–820. doi: 10.1038/s41591-020-0898-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen H.F., Hockenberry J.M., Borders T.F., Druss B.G. Impact of medicaid expansion on medicaid-covered utilization of buprenorphine for opioid use disorder treatment. Med. Care. 2017;55:336–341. doi: 10.1097/MLR.0000000000000703. [DOI] [PubMed] [Google Scholar]
- Wood C.A., Duello A., Horn P., Winograd R., Jackson L., Mayen S., Wallace K. Overdose response training and naloxone distribution among rural first responders. J. Rural Ment. Health. 2021 [Google Scholar]