Abstract
The COVID-19 pandemic has highlighted the importance of work in shaping population health and wellbeing. This Viewpoint applies a multilevel systems framework to assist in understanding the diverse and complex interactions of forces affecting worker health and wellbeing, and how trending changes in employment and working conditions have been accelerated by the pandemic. Government agencies concerned with population health and wellbeing, and economic activity must expand their capacity to monitor, evaluate, and respond to these trends. In addition, integrated enterprise and workplace-based approaches that consider the interactions among these multidimensional drivers will build organisation and worker resilience to navigate the continual changes in work and worker safety, health, and wellbeing in a post-pandemic world.
Introduction
The COVID-19 pandemic is disrupting our economies, public health, and medical-care systems, and is shaping the future of work. The pandemic has accelerated numerous trends in how work is structured, with substantial implications for enterprises, and for worker health and wellbeing. Globally, employers, government regulators, public health agencies, trade unions, and professional associations have grappled with maintaining economic activity while keeping workers safe and healthy.
Work exposures and working conditions can have negative or beneficial effects on the safety, health, and wellbeing of workers.1 For example, workplace air quality can affect respiratory function and transmission of viruses;2 high physical demands and long working hours can result in musculoskeletal pain and disability;3, 4 unpredictable schedules, employee overload, and occupational stress can contribute to burnout, psychological distress, and cardiovascular problems.5 Further, employment, work-associated income, and access to benefits (eg, health-care benefits and sick leave) have the potential to narrow, or widen, health disparities.6 However, working conditions can also have positive effects on workers; for example, workers who have higher autonomy, flexibility, and supportive supervisors and colleagues also have better wellbeing and health.7, 8, 9
The purpose of this Viewpoint is to consider the implications of the COVID-19 pandemic for the future of work, worker health, and wellbeing. We discuss current and anticipated pandemic-related changes in the social–political–economic environment, employment and labour patterns, and enterprise policies and practices.
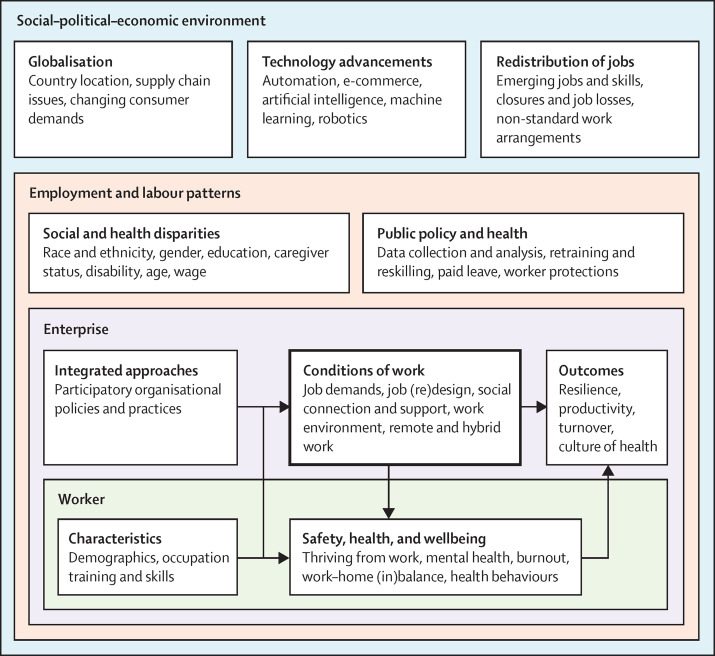
A multilevel evidence-based systems model was used in this Viewpoint to depict the diverse ways the pandemic has affected and will continue to affect work, worker health, and wellbeing (figure ).10 The model highlights the interconnectedness of each system's level, with each level being influenced by the systems within which it resides. The broader social–political–economic environ-ment structures employment and labour patterns, influencing public policy and practice. These levels in turn shape organisational policies, programmes, and practices. Influenced by these systems, enterprises establish working conditions that contribute to worker safety, health, and wellbeing. Applying a systems-level model can help to explain the variability that the pandemic has had on work and workers by country in the context of differences in pre-existing social support, available resources, and existing or new public health and labour protection policies.11
Figure.
The social–political–economic environment during the COVID-19 pandemic and its effects on work and workers
Multilevel, evidenced-based systems model illustrating an example of the contextual forces evident during the COVID-19 pandemic that impacted the future of work and worker safety, health, and wellbeing. We applied a framework from Sorensen and colleagues.10
Based on the model (figure), in the first section of this Viewpoint, we focus on the social–political–economic environment, and employment and labour patterns, that affect enterprises and workers. In the second section, we outline how these factors affect enterprises by influencing implementation of organisational policies, programmes, and practices in relation to COVID-19. We also outline how work is structured, which in turn affects workers, their health, and their wellbeing. We have identified these factors as crucial areas for consideration; however, it is not our intent to provide an exhaustive list of all the possible factors that might affect the future of work and worker health. Many of these factors are focused on high-income countries due to the more expansive literature available on this topic. The factors that affect workers and enterprises are likely to manifest in different ways depending on the social–political–economic context of the country. Therefore, the experiences of low-income and middle-income countries might be different from the experiences described here.
Social–political–economic environment and employment and labour patterns
The pandemic has highlighted and accelerated trends in the social, political, and economic environments that affect employment and labour patterns. For some countries, existing social, political, and economic labour policies enabled jurisdictions to respond to the pandemic swiftly and effectively. In many countries, successful vaccine uptake and acceptance of strict COVID-19 policies to stem the spread of the virus was also related to trust in government and leaders.12, 13, 14, 15 Worker experience varied during the pandemic, depending on where they worked and lived, their age, gender, race, education, level of training, work experience, and home demands, as well as their industry, occupation, and specific job demands. Some jobs are considered essential, such as public-facing positions in health care, supermarkets, and correctional facilities. In these positions, workers have had increasing job demands and faced a high risk of exposure to COVID-19. Other essential jobs, such as working in food production and distribution, manufacturing, and warehouses, might be situated in crowded and inadequately ventilated workplaces where risk of exposure is higher. Individuals employed in service industries such as hospitality, retail businesses with physical premises (ie, bricks-and-mortar retail), and tourism often earn low wages, and have a high risk of unemployment. In contrast, many knowledge and office workers quickly transitioned to working from home. These individuals were more likely to be from urban areas, have higher paying jobs and benefits, and have increased job stability because they had the option of teleworking.16, 17
The rising globalisation of financial markets and disruptions to supply chains have affected many sectors by fuelling increases in shipping costs and delays in delivery, and by creating an impetus to increase productivity in manufacturing and transportation. These forces can result in increased safety and health risks because of increased work pace, longer working hours, and inadequate staffing to meet demands.
The pandemic has accelerated a redistribution of jobs across sectors, affecting labour and employment patterns: an estimated 25% of workers worldwide will choose or need to change occupations by 2030.18 The pandemic is also stimulating technological innovation across physical, digital, and biological spheres. This innovation is resulting in a rapid implementation of emerging technologies in the workplace (eg, automation, e-commerce, robotics, artificial intelligence, machine learning, nanotechnologies, and biotechnologies).19 Over half of global businesses are estimated to have accelerated the automation of tasks because of the pandemic.20 Consumer behaviours have also changed substantially and probably permanently, stimulating substantial growth in the delivery economy.18 The adoption of new technologies is resulting in the need for new job skills and training requirements. Demand for workers is increasing in transportation, distribution centres, and emerging scientific and technological fields. In contrast, demand for workers has decreased in other industries, such as bricks-and-mortar retail, customer services, hospitality, support services, office support, and food services.18 Many of the sectors experiencing a decline in levels of employment, or a slow return to pre-pandemic levels, typically employ economically disadvantaged workers, more women, workers from minority ethnic and racial backgrounds, and immigrant workers.21, 22 Timely and effective upskilling, reskilling, and redeployment will be needed to enable the workforce to respond to these changes. These trends also have longer-term consequences for the stability or precarity of jobs, the quality of work available, and the ability for workers to retire.21
During the pandemic, many countries also observed a steep decline in labour migration.23, 24 The effect of this trend for staffing and diversifying talent, especially in industries that require workers to be physically present such as health care, service industries, and construction, has been substantial.
Globally, the number of workers in non-standard working arrangements (eg, contingent, gig, contract, and agency) has been increasing since the 2008 recession.25, 26, 27 Because non-standard work arrangements provide employers with the flexibility to hire and dismiss workers easily to meet demand and reduce overhead costs, the pandemic has accelerated this trend. For some workers, these non-standard arrangements also provide desirable flexibility (eg, the ability to work around family and community responsibilities). However, workers in non-standard arrangements are also exposed to increased risk of injury, health risks, and income uncertainty. These workers often lack appropriate job protections, a worker voice, and access to affordable health care.27, 28
Existing social and health disparities are being highlighted and widened by the pandemic. Indigenous workers, immigrant workers, and workers from a minority race and ethnic background have been disproportionately affected.29, 30, 31 These workers are often employed in low-wage essential jobs, putting them at higher risk of exposure to SARS-CoV-2. Essential workers are also exposed to other long-standing safety and health hazards, further increasing their risk of injury and illness. Further, in countries such as Canada and the UK, workers with disabilities were found to be more disadvantaged with respect to pandemic-related work accommodations—specific accommodations made by an employer for an individual with a disability or health-related work limitation to enable them to perform their work duties—than workers without a disability.32, 33 In a global survey of individuals with long COVID symptoms lasting more than 28 days, 91% of survey respondents had ongoing symptoms exceeding 7 months. For those individuals still experiencing symptoms, 45% required ongoing work accommodations and 22% remained off work.34 Worldwide, caregivers were disproportionately affected when schools, childcare services, and services providing care to older individuals suspended in-person activities.35 This closure of schools and care facilities led to the need for caregivers to manage caring responsibilities alongside work. Consequently, women—who often do the majority of unpaid care work—exited the workforce at higher rates than men and had higher rates of job and income loss.35 Globally, younger workers have faced high levels of unemployment, reduced access to training, and have had more difficulty recovering from economic shocks due to income uncertainty and job loss.36 Whereas older workers, particularly those in low-skilled positions, who need to change jobs, retrain, or upskill will be disadvantaged.37
Enterprise and worker outcomes
The pandemic has illuminated the interconnected pathways through which broader social–political–economic environments, and employment and labour patterns, have shaped the experiences of enterprises and workers. These experiences have highlighted the need for integrated and adaptable enterprise approaches to ensure worker safety, health, and wellbeing by improving the conditions of work through organisational policies and practices. For example, work environments have been created with conditions and policies that are supportive and health-promoting, that ensure workers are “thriving from work”,38 and that have substantial benefits for worker health, worker wellbeing, and enterprise outcomes.7 These enterprise benefits could include reduced workforce turnover and absenteeism, and higher productivity and employee engagement.8 Implementing supportive practices that dually benefit the organisation and its workers was a priority for some US-based employers at the start of the pandemic.39 However, more recent worker surveys indicate that some practices, such as leadership commitment to wellbeing and workplace communication, are perceived to have declined as the pandemic continues.40
The experiences of employers during the pandemic have been shaped considerably by their industry and the type of work performed by their employees, as well as by public mandates and policies. For example, large, complex, multi-layered, and siloed enterprises have had difficulty implementing changes rapidly in response to an evolving COVID-19 landscape. Many small-sized and medium-sized enterprises have struggled to balance business priorities with worker health and wellbeing, in part due to limited resources and financial constraints. Efficient and integrated structures are expected to enable enterprises to be more resilient in response to the changing landscape of broader social, economic, and political forces. These approaches include streamlining processes to allow rapid responsiveness and aligning goals of the organisation with worker safety, health, and wellbeing needs.
Many workplaces are transitioning to decentralised and remote workspaces connected by technologies. About 25% of workers in high-income countries are expected to continue remote working either part-time or full-time after the pandemic.18 During the pandemic, US remote workers reported being as productive, if not more productive, as they were in the workplace before the pandemic.41, 42 Remote workers might also benefit from an elimination of commuting time, increased autonomy and job control, improved work–life balance, increased participation in the community, and flexible work hours.43 Many of these positive conditions of work have been associated with improved worker health outcomes and wellbeing.7, 8, 9 However, some enterprises with remote workers face potential challenges in implementing new policies, programmes, and practices for remote work. Some work is more effectively conducted online, but other work requires, and benefits from, interpersonal interaction unmediated by technology. The potential to work effectively in a remote setting varies greatly depending on individual circumstances. For example, workers might face difficulty working remotely due to lack of access to private workspaces and technology (from high-speed internet to ergonomic office equipment).44, 45 Similarly, some workers thrive on informal and ongoing interactions in physical workspaces, although others do not. Many remote workers might experience fatigue from high volumes of videoconferencing with few breaks.46 Enterprises will need to establish what hybrid work environments, models of work, and new remote work arrangements will look like for workers.47
Changing work patterns might also influence the physical activity and dietary habits of workers, with associated long-term health effects. Early in the pandemic, many employees who transitioned to working from home reported increased screen time and sedentary behaviours,48 possibly exacerbated by imposed lockdowns. With the expected continuation of remote and hybrid work arrangements, public health strategies that are responsive to these modified work arrangements will be needed to support physical activity, dietary habits, and health in general. For example, remote work arrangements could potentially allow increased flexibility for intermittent exercise throughout the day, increased control over food choices and mealtimes, and improved work–life balance.
The acceleration of automation and digitisation is likely to affect workers in different ways, further increasing existing health disparities.21 For example, employees who can work remotely have benefited from automation and digitisation, enabling them to continue employment and providing flexibility when needed. This flexibility could benefit workers with chronic health conditions and disabilities. Automation and digitisation have increased job precarity for workers in lower-wage occupations such as manufacturing, retail, and service industries, due to jobs being replaced by technological advancements.18, 21 Because employment and income are intrinsically linked to health inequalities, this job precarity can have substantial public health effects for individuals and their families.
As the pandemic continues, many workplaces, especially in health care, education, food service, and retail, have redesigned jobs and modified physical work environments to reduce exposure to SARS-CoV-2. For example, the quality and adequacy of air ventilation and filtration systems are essential for reducing the transmission of COVID-19 and might also generate other health and cognitive benefits.49
Worsening mental health, psychological distress, burnout, and substance use have been accelerated substantially by the pandemic.50, 51, 52, 53, 54 These effects are associated with job uncertainty and loss of income,55 as well as with substantive changes to working conditions. Workers experienced increased stress due to changes in their work organisation and environment. Stressors include exposure to the virus itself, changes in work arrangements and schedules, increased workload and job demands, effects on work–life balance, reduced social support at work, and lack of adequate paid leave policies and health-care benefits.36, 56 Young adults, workers with children, economically disadvantaged workers, workers from minority race and ethnic backgrounds (including Black, and Hispanic and Latinx workers), individuals belonging to Indigenous communities, and workers with long COVID symptoms have been found to be most at risk.36, 54 Increases in working hours and increased job demands often lead to higher incidences of stress and burnout.57, 58 For example, for workers employed in low socioeconomic status occupations, working more than 55 h per week significantly increases risk of stroke and heart disease.59
For remote workers, physical distancing and advice to stay at home contributed to isolation and a lack of distinction between work life and home life. For employers with employees who work remotely or have little social interactions in the workplace, practices that enable communication, increase social interaction and collaboration for work teams, and respect work–life boundaries, are important for alleviating stress and isolation. Supervisors are likely to require additional support and training to transition into new ways of providing leadership that meet the needs of workers under new work arrangements.
The trend in increasing workforce turnover further indicates the extent to which workers are exposed to poor working conditions. These conditions lead to work-related stress, burnout, and other negative health impacts. Workers have been leaving their jobs at a higher rate than was observed before the pandemic.60, 61 As of March, 2021, up to half of the global workforce is actively seeking new employment opportunities.62, 63, 64 These surveys also suggest that workers are seeking employment that would allow them to thrive by supporting their health and wellbeing—eg, jobs with career growth opportunities that provide workers with a sense of meaning and purpose. Workers might also seek employers that treat employees ethically, provide flexibility and autonomy, implement working conditions and arrangements that promote health and wellbeing, and consider employees’ lives outside of work.65
Applying a public health perspective after the pandemic
The COVID-19 pandemic will have long-term impacts on enterprises, workers, and the future of work across the globe. The specifics of these impacts, however, remain uncertain. The pandemic has emphasised the important relationship between work and population health. It has highlighted the importance of worker wellbeing and mental health, thereby expanding the occupational health and safety framework—which previously focused on disease and injury risk—to also focus on the positive impacts that work can have on workers’ ability to thrive in life.
Government agencies concerned with both population health and economic activity must expand their capacity to monitor, evaluate, and respond to these trends. Improved governmental data collection and analysis will enable a greater understanding of work-based social and health disparities. These data can inform public health and occupational health strategies to narrow inequalities at government and enterprise levels. Enhanced monitoring at enterprise and population levels would help to identify and mitigate hazardous exposures. These approaches might include increased monitoring of disease and injuries associated with evolving working conditions in both traditional and non-standard work arrangements; an increased focus by employers and policy makers on how work can affect health and wellbeing in positive ways to supplement traditional injury and disease indicators; and increased attention paid to the ways in which changes in organisation and public policy affect worker safety, health, and wellbeing. These approaches could reduce health risks, facilitate prevention initiatives, and promote worker safety, health, and wellbeing.66
Further research should track the long-term effect of the COVID-19 pandemic on employment patterns, work arrangements, and worker safety, health, and wellbeing. Improvements are needed in the collection, compilation, analysis, and reporting of sociodemographic information for both infection and illness to identify disparities in health and wellbeing. These data need to include industry, occupation, work arrangements, age, sex and gender, income, education, migrant or residency status, and race and ethnicity. Better data (ie, more data, and more reliable data) are needed to inform interventions and improve protections for vulnerable workers. For example, data are needed to further understand how worker protections affect workers across different sociodemographic characteristics, job roles, and work arrangements. Data can also be used to better understand how working conditions, as well as organisational and public policies, widen or narrow health disparities.
To maintain the health and wellbeing of workers, government regulations mandating safer working conditions (eg, improved ventilation, reduced crowding, managing physical and psychosocial risks, and other infection control measures), as well as supportive leave policies, are an important step towards uniform protections across industries and jobs. These mandates need to ensure that workers with high risk of exposure to workplace hazards, and workers in non-standard arrangements, are protected, and should aim to eliminate health disparities. Thereby, employers can play an important role in worker health and wellbeing by implementing health-promoting organisational policies and practices.
The systems-level model (figure) can guide the development of effective strategies that respond to the specific needs of enterprises and workplaces. Approaches and strategies can vary by industry, organisation type, and the needs of the workforce. For enterprises, participatory interventions that engage key stakeholder groups, integrate health protection and health promotion approaches, and consider worker health and wellbeing to be an organisational priority have been found to be most effective at improving worker safety, health, and wellbeing.8 Further, integrated approaches that consider these complex and multidimensional drivers are likely to be most effective at navigating future changes in work and worker safety, health, and wellbeing.10 These approaches would enhance the resilience of organisations to thrive in the post-pandemic world.
During the pandemic and beyond, policy makers and employers need to expand their commitment to improving and sustaining worker wellbeing by considering the factors that ensure workers and enter-prises continue to thrive.38 The International Labour Organization,67 Organisations for Economic Co-operation and Development,68 and other professional labour groups69, 70 have developed specific worker health and wellbeing policy and practice recommendations to facilitate recovery during a pandemic and in the post-pandemic world. These policy recommendations67, 68, 69, 70 were designed to help governments and enterprises navigate changes brought on by COVID-19 in a manner that is beneficial to both enterprises and workers.
Workplaces can be important engines of wellbeing in the communities they support. However, many employers traditionally focus on approaches that target individual worker behaviour (eg, wellness programmes). These narrowly focused approaches promote individual worker behaviour change, and are often ineffective compared to more efficacious upstream changes to workplace conditions and policies that affect groups of workers or all workers.71 Attending to systems-level changes would mitigate the detrimental effects of the pandemic on worker health and wellbeing. These changes could include job or work redesign,72 improvements in physical and psychological work environments, ensuring workers with non-standard work arrangements have access to the same benefits as workers with standard arrangements, and other fair, egalitarian, inclusive, and supportive workplace policies and practices for all workers.
The COVID-19 pandemic has highlighted the importance of specific working conditions, policies, and practices that have helped organisations and workers navigate pandemic-related challenges. These include a commitment to the physical and emotional health, wellbeing, and safety of workers; supportive and flexible supervisors and leadership; frequent and honest communication and dialogue; flexible work provisions; encouragement and support of worker engagement in both identifying and solving problems; and enhanced organisational benefits (eg, financial assistance to establish ergonomic remote offices, childcare assistance, sick leave policies, and caretaker leave policies).73, 74, 75, 76
Adaptations in organisational management systems will be required to support the increase of hybrid and remote workforces. Hybrid and remote work arrangements might also change the sense of cohesion within the organisation, introducing the need for policies and practices to increase connectedness and sense of belonging for workers.77 Workplaces and their working conditions are central to addressing the sociodemographic determinants of health and inequalities, such as determinants related to income, race and ethnicity, and gender.
In response, a collaborative effort involving systemic, integrated approaches at both public policy and enterprise levels can help to ensure the safety, health, and wellbeing of workers, their families, the communities in which they live, and the enterprises where they are employed. The benefits of such approaches are likely to last beyond the pandemic, creating the resilience and adaptability needed for enterprises to meet future public health challenges and those associated with future changes to work.
Declaration of interests
We declare no competing interests.
Acknowledgments
Acknowledgments
This work was supported by a grant from the US National Institute for Occupational Safety and Health, USA, for the Harvard T H Chan School of Public Health Center for Work, Health, and Well-being (U19 OH008861 to GS). GRW is partly supported by the McEllhattan Foundation. The content of this Viewpoint is solely the responsibility of the authors and does not necessarily represent the official views of the Harvard T.H. Chan School of Public Health, the Centers for Disease Control and Prevention, the National Institute for Occupational Safety and Health, or the McElhattan Foundation. We would like to thank Lisa Burke, outreach director at the Harvard T H Chan School of Public Health Center for Work, Health, and Well-being, for proofreading.
Contributors
All authors were involved in conceptualisation, JTD and SEP were responsible for visualisation, SEP wrote the original draft, and JTD, GS, and GRW were responsible for writing, reviewing, and editing the manuscript.
References
- 1.Hudson HL, Nigam JA, Sauter SL, Chosewood L, Schill AL, Howard JE. American Psychological Association; Washington, DC: 2019. Total worker health. [Google Scholar]
- 2.Allen JG, Macomber JD. Harvard University Press; Cambridge, MA: 2020. Healthy buildings: how indoor spaces drive performance and productivity. [Google Scholar]
- 3.Dembe AE, Erickson JB, Delbos RG, Banks SM. The impact of overtime and long work hours on occupational injuries and illnesses: new evidence from the United States. Occup Environ Med. 2005;62:588–597. doi: 10.1136/oem.2004.016667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Niedhammer I, Lesuffleur T, Labarthe G, Chastang J-F. Role of working conditions in the explanation of occupational inequalities in work injury: findings from the national French SUMER survey. BMC Public Health. 2018;18:1–13. doi: 10.1186/s12889-018-5254-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kelly EL, Moen P. Princeton University Press; Princeton, NJ: 2020. Overload: how good jobs went bad and what we can do about it. [Google Scholar]
- 6.Pronk N, Kleinma DV, Goekler SF, Ochiai E, Blakey C, Brewer KH. Promoting health and well-being in healthy people 2030. J Public Health Manag Pract. 2021;27:S242–S248. doi: 10.1097/PHH.0000000000001254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Joyce K, Pabayo R, Critchley JA, Bambra C. Flexible working conditions and their effects on employee health and wellbeing. Cochrane Database Syst Rev. 2010;2010 doi: 10.1002/14651858.CD008009.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fox KE, Johnson ST, Berkman LF, et al. Organisational- and group-level workplace interventions and their effect on multiple domains of worker well-being: a systematic review. Work Stress. 2021 doi: 10.1080/02678373.2021.1969476. published online Aug 26. [DOI] [Google Scholar]
- 9.Adams JM. The value of worker well-being. Public Health Rep. 2019;134:583–586. doi: 10.1177/0033354919878434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sorensen G, Dennerlein JT, Peters SE, Sabbath EL, Kelly EL, Wagner GR. The future of research on work, safety, health and well-being: a guiding conceptual framework. Soc Sci Med. 2021;269 doi: 10.1016/j.socscimed.2020.113593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mendenhall E. The COVID-19 syndemic is not global: context matters. Lancet. 2020;396 doi: 10.1016/S0140-6736(20)32218-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Olagnier D, Mogensen TH. The COVID-19 pandemic in Denmark: big lessons from a small country. Cytokine Growth Factor Rev. 2020;53:10–12. doi: 10.1016/j.cytogfr.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ursin G, Skjesol I, Tritter J. The COVID-19 pandemic in Norway: the dominance of social implications in framing the policy response. Health Policy Technol. 2020;9:663–672. doi: 10.1016/j.hlpt.2020.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tiirinki H, Tynkkynen L-K, Sovala M, et al. COVID-19 pandemic in Finland—preliminary analysis on health system response and economic consequences. Health Policy Technol. 2020;9:649–662. doi: 10.1016/j.hlpt.2020.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jefferies S, French N, Gilkison C, et al. COVID-19 in New Zealand and the impact of the national response: a descriptive epidemiological study. Lancet Public Health. 2020;5:e612–e623. doi: 10.1016/S2468-2667(20)30225-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.European Foundation for the Improvement of Living and Working Conditions COVID-19: implications for employment and working life. March 11, 2021. https://www.eurofound.europa.eu/publications/report/2021/covid-19-implications-for-employment-and-working-life
- 17.Pew Research Center How the coronavirus outbreak has–and hasn't– changed the way Americans work. Dec 9, 2020. https://www.pewresearch.org/social-trends/wp-content/uploads/sites/3/2020/12/PSDT_12.09.20_covid.work_fullreport.pdf
- 18.Lund S, Madgavkar A, Manyika J, et al. The future of work after COVID-19. Feb 18, 2021. https://www.mckinsey.com/featured-insights/future-of-work/the-future-of-work-after-covid-19
- 19.Neto RDCS, Maia JS, de Silva Neiva S, Scalia MD, de Andrade JBSO. The fourth industrial revolution and the coronavirus: a new era catalyzed by a virus. Res Global. 2020;2 [Google Scholar]
- 20.World Economic Forum Resetting the future of work agenda: disruption and renewal in a post-COVID world. Oct, 2020. http://www3.weforum.org/docs/WEF_NES_Resetting_FOW_Agenda_2020.pdf
- 21.Jetha A, Shamaee A, Bonaccio S, et al. Fragmentation in the future of work: a horizon scan examining the impact of the changing nature of work on workers experiencing vulnerability. Am J Ind Med. 2021;64:649–666. doi: 10.1002/ajim.23262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Organization for Economic Co-operation and Development OECD Employment Outlook 2021: navigating the COVID-19 crisis and recovery. 2021. https://www.oecd-ilibrary.org/sites/5a700c4b-en/index.html?itemId=/content/publication/5a700c4b-en
- 23.Asian Development Bank Institute. Organization for Economic Co-operation and Development. International Labour Organization Labor migration in Asia: impacts of the COVID-19 crisis and the post-pandemic future. 2021. https://www.ilo.org/wcmsp5/groups/public/---asia/---ro-bangkok/documents/publication/wcms_784823.pdf
- 24.International Centre for Migration and Policy Development The impact of COVID-19 on talent attraction: an unexpected opportunity for the EU? June 21, 2021. https://www.icmpd.org/news/the-impact-of-covid-19-on-talent-attraction-an-unexpected-opportunity-for-the-eu
- 25.ter Weel B. The rise of temporary work in Europe. De Economist. 2018;166:397–401. [Google Scholar]
- 26.Luo T, Mann A, Hoden RJ. What happened to temps? Changes since the great recession. Feb, 2021. [DOI]
- 27.Organisation for Economic Co-operation and Development OECD policy responses to coronavirus (COVID-19): distributional risks associated with non-standard work: stylised facts and policy considerations. June 12, 2020. https://www.oecd.org/coronavirus/policy-responses/distributional-risks-associated-with-non-standard-work-stylised-facts-and-policy-considerations-68fa7d61/
- 28.Park J, Han B, Park J-S, Park EJ, Kim Y. Nonstandard workers and differential occupational safety and health vulnerabilities. Am J Ind Med. 2019;62:701–715. doi: 10.1002/ajim.22997. [DOI] [PubMed] [Google Scholar]
- 29.Kirby T. Evidence mounts on the disproportionate effect of COVID-19 on ethnic minorities. Lancet Respir Med. 2020;8:547–548. doi: 10.1016/S2213-2600(20)30228-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bhala N, Curry G, Martineau AR, Agyemang C, Bhopal R. Sharpening the global focus on ethnicity and race in the time of COVID-19. Lancet. 2020;395:1673–1676. doi: 10.1016/S0140-6736(20)31102-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Argoty-Pantoja AD, Robles-Rivera K, Rivera-Paredez B, Salmerón J. COVID-19 fatality in Mexico's indigenous populations. Public Health. 2021;193:69–75. doi: 10.1016/j.puhe.2021.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gignac MAM, Shahidi FV, Jetha A, et al. Impacts of the COVID-19 pandemic on health, financial worries, and perceived organizational support among people living with disabilities in Canada. Disabil Health J. 2021;14 doi: 10.1016/j.dhjo.2021.101161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Holland P. Will disabled workers be winners or losers in the post-covid-19 labour market? Disabilities. 2021;1:161–173. [Google Scholar]
- 34.Davis HE, Assaf GS, McCorkell L, et al. Characterizing long covid in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine. 2021;30 doi: 10.1016/j.eclinm.2021.101019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.International Labor Organization Building forward fairer: women's rights to work and at work at the core of the COVID-19 recovery. July, 2021. https://www.ilo.org/wcmsp5/groups/public/---dgreports/---gender/documents/publication/wcms_814499.pdf
- 36.Cotofan M, De Neve JE, Golin M, Kaats M, Ward G. Work and well-being during COVID-19: impact, inequalities, resilience, and the future of work. 2021. http://happiness-report.s3.amazonaws.com/2021/WHR+21_Ch7.pdf
- 37.Kanfer R, Lyndgaard SF, Tatel CE. For whom the pandemic tolls: a person-centric analysis of older workers. Work Aging Retire. 2020;6:238–241. doi: 10.1093/workar/waaa014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Peters SE, Sorensen G, Katz JN, Gundersen DA, Wagner GR. Thriving from work: conceptualization and measurement. Int J Environ Res Public Health. 2021;18 doi: 10.3390/ijerph18137196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Emmet J, Schrar G, Schrimper M, Wood A. COVID-19 and the employee experience: how leaders can seize the moment. June 29, 2020. https://www.mckinsey.com/business-functions/organization/our-insights/covid-19-and-the-employee-experience-how-leaders-can-seize-the-moment
- 40.Maese E, Saad L. How has the pandemic affected U.S. work life? March 17, 2021. https://news.gallup.com/poll/339824/pandemic-affected-work-life.aspx
- 41.Baker M. What is the new employment deal? Oct 13, 2020. https://www.gartner.com/smarterwithgartner/what-is-the-new-employment-deal
- 42.Barrero JM, Bloom N, Davis SJ. Why working from home will stick. April 2021. https://www.nber.org/papers/w28731
- 43.Oakman J, Kinsman N, Stuckey R, Graham M, Weale V. A rapid review of mental and physical health effects of working at home: how do we optimise health? BMC Public Health. 2020;20:1–13. doi: 10.1186/s12889-020-09875-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Boserup B, McKenney M, Elkbuli A. Alarming trends in US domestic violence during the COVID-19 pandemic. Am J Emerg Med. 2020;38:2753–2755. doi: 10.1016/j.ajem.2020.04.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Okuyan CB, Begen MA. Working from home during the COVID-19 pandemic, its effects on health, and recommendations: the pandemic and beyond. Perspect Psychiatr Care. 2021 doi: 10.1111/ppc.12847. published online May 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fauville G, Luo M, Muller Queiroz AC, Bailenson JN, Hancock J. Nonverbal mechanisms predict zoom fatigue and explain why women experience higher levels than men. SSRN. 2021 doi: 10.2139/ssrn.3820035. published online April 5. (preprint). [DOI] [Google Scholar]
- 47.Gartner Press Release: Gartner HR research shows organizations are eroding employee performance and well-being with virtualized office-centric design. https://www.gartner.com/en/newsroom/press-releases/2021-05-03-gartner-hr-research-shows-organizations-are-eroding-employee-performance-and-well-being-with-virtualized-office-centric-design
- 48.Ráthonyi G, Kósa K, Bács Z, et al. Changes in workers' physical activity and sedentary behavior during the COVID-19 pandemic. Sustainability. 2021;13 [Google Scholar]
- 49.Allen JG, Ibrahim AM. Indoor air changes and potential implications for SARS-CoV-2 transmission. JAMA. 2021;325:2112–2113. doi: 10.1001/jama.2021.5053. [DOI] [PubMed] [Google Scholar]
- 50.Abbott A. COVID's mental-health toll: how scientists are tracking a surge in depression. Nature. 2021;590:194–195. doi: 10.1038/d41586-021-00175-z. [DOI] [PubMed] [Google Scholar]
- 51.Varga TV, Bu F, Dissing AS, et al. Loneliness, worries, anxiety, and precautionary behaviours in response to the COVID-19 pandemic: a longitudinal analysis of 200,000 western and northern Europeans. Lancet Reg Health Eur. 2021;2 doi: 10.1016/j.lanepe.2020.100020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pierce M, Hope H, Ford T, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7:883–892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kola L, Kohrt BA, Hanlon C, et al. COVID-19 mental health impact and responses in low-income and middle-income countries: reimagining global mental health. Lancet Psychiatry. 2021;8:535–550. doi: 10.1016/S2215-0366(21)00025-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Perlis RH, Green J, Simonson MD, et al. The COVID States project #54: mental health in the United States. May 21, 2021. https://osf.io/cgfzt/
- 55.Wilson JM, Lee J, Fitzgerald N, Oosterhoff B, Sevi B, Shook NJ. Job insecurity and financial concern during the COVID-19 pandemic are associated with worse mental health. J Occup Environ Med. 2020;62:686–691. doi: 10.1097/JOM.0000000000001962. [DOI] [PubMed] [Google Scholar]
- 56.Ellingrud K, Krishnan M, Krivkovich A, et al. Diverse employees are struggling the most during COVID-19: here's how companies can respond. Nov 17, 2020. https://www.mckinsey.com/featured-insights/diversity-and-inclusion/diverse-employees-are-struggling-the-most-during-covid-19-heres-how-companies-can-respond
- 57.Prasad K, McLoughlin C, Stillman M, et al. Prevalence and correlates of stress and burnout among US healthcare workers during the COVID-19 pandemic: a national cross-sectional survey study. EClinicalMedicine. 2021;35 doi: 10.1016/j.eclinm.2021.100879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wang B, Liu Y, Qian J, Parker SK. Achieving effective remote working during the COVID-19 pandemic: a work design perspective. Appl Psychol. 2021;70:16–59. doi: 10.1111/apps.12290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Li J, Pega F, Ujita Y, et al. The effect of exposure to long working hours on ischaemic heart disease: a systematic review and meta-analysis from the WHO/ILO joint estimates of the work-related burden of disease and injury. Environ Int. 2020;142 doi: 10.1016/j.envint.2020.105739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gandhi V, Robinson J. The ‘great resignation’ is really the ‘great discontent’. July 22, 2021. https://www.gallup.com/workplace/351545/great-resignation-really-great-discontent.aspx
- 61.Cook I. Who is driving the great resignation? Sept 15, 2021. https://hbr.org/2021/09/who-is-driving-the-great-resignation
- 62.Gartner Gartner HR survey shows a quarter of Australian employees are seeking a new job. April 29, 2021. https://www.gartner.com/en/newsroom/press-releases/2021-04-29-gartner-hr-survey-shows-a-quarter-of-australian-emplo
- 63.EY Global More than half of employees globally would quit their jobs if not provided post-pandemic flexibility, EY survey finds. May 12, 2021. https://www.ey.com/en_gl/news/2021/05/more-than-half-of-employees-globally-would-quit-their-jobs-if-not-provided-post-pandemic-flexibility-ey-survey-finds
- 64.De Smet A, Dowling B, Mugayar-Baldocci M, Schaninger B. ‘Great attrition’ or ‘great attraction’? The choice is yours. Sept 8, 2021. https://www.mckinsey.com/business-functions/people-and-organizational-performance/our-insights/great-attrition-or-great-attraction-the-choice-is-yours
- 65.McKinsey & Company The great attrition stems from a great disconnect. Oct 18, 2021. https://www.mckinsey.com/featured-insights/coronavirus-leading-through-the-crisis/charting-the-path-to-the-next-normal/the-great-attrition-stems-from-a-great-disconnect
- 66.Jha AK. Data: the lifeblood of the public health response to COVID-19. Ann Intern Med. 2021 doi: 10.7326/M21-3725. published online Sept 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.International Labour Organization Building forward fairer: women's rights to work and at work at the core of the COVID-19 recovery. 2021. https://www.ilo.org/wcmsp5/groups/public/---dgreports/---gender/documents/publication/wcms_814499.pdf
- 68.Organisation for Economic Co-operation and Development Key policy responses from the OECD. 2021. https://www.oecd.org/coronavirus/en/policy-responses
- 69.Trades Union Congress A better recovery: learning the lessons of the corona crisis to create a stronger, fairer economy. 2020. https://www.tuc.org.uk/sites/default/files/TUC%20Report%20'A%20Better%20Recovery'%20(2).pdf
- 70.American Federation of Labor & Congress of Industrial Organizations Safety first: working people's plan for reopening the economy the right way. 2021. https://aflcio.org/sites/default/files/2020-04/SafetyFirst.pdf
- 71.Baid D, Hayles E, Finkelstein EA. Return on investment of workplace wellness programs for chronic disease prevention: a systematic review. Am J Prev Med. 2021;61:256–266. doi: 10.1016/j.amepre.2021.02.002. [DOI] [PubMed] [Google Scholar]
- 72.Lovejoy M, Kelly EL, Kubzansky LD, Berkman LF. Work redesign for the 21st century: promising strategies for enhancing worker well-being. Am J Public Health. 2021;111:1787–1795. doi: 10.2105/AJPH.2021.306283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Men LR, Qin YS, Jin J. Fostering employee trust via effective supervisory communication during the COVID-19 pandemic: through the lens of motivating language theory. Int J Bus Commun. 2021 https://doi:10.1177/23294884211020491 published online June 6. [Google Scholar]
- 74.Dennerlein JT, Burke L, Sabbath EL, et al. An integrative total worker health framework for keeping workers safe and healthy during the COVID-19 pandemic. Hum Factors. 2020;62:689–696. doi: 10.1177/0018720820932699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Brown CE, Schwatka N, Dexter L, et al. The importance of small business safety and health climates during COVID-19. J Occup Environ Med. 2021;63:81–88. doi: 10.1097/JOM.0000000000002080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Purkayastha D, Vanroelen C, Bircan T, Vantyghem MA, Gantelet Adsera C. Work, health and COVID-19: a literature review. SSRN. 2021 doi: 10.2139/ssrn.3856915. published online June 7. (preprint). [DOI] [Google Scholar]
- 77.Grzegorczyk M, Mariniello M, Nurski L, Schraepen T. Blending the physical and virtual: a hybrid model for the future of work. https://www.bruegel.org/2021/06/hybrid-work/