Abstract
Background & aims
Patients with eating disorders (ED) are known to suffer from various psychological morbidities thus they are expected to be negatively impacted due to the COVID-19 pandemic. Our meta-analysis aims to evaluate the effect of the COVID-19 pandemic on the pooled prevalence of psychological comorbidities in ED patients.
Methods
Pubmed, Scopus, GoogleScholar, and medRxiv were searched using the keywords COVID19 and Eating Disorders and their related MeSH terms. The articles were included if they contained patients with diagnosed EDs and having evaluated their mental health disturbances during the COVID-19 pandemic. The quality of the included studies was assessed using the “assessing risk of bias in prevalence studies” tool. The heterogeneity was assessed using Cochrane Q and I2 heterogeneity statistics.
Results
A total of 13 articles have been included in this meta-analysis with a sample size of 3056. The pooled prevalence of ED patients who experienced worsening of ED symptoms was 57% (95%CI: 36%–76%), anxiety was 64% (95%CI: 39%–78%), and depression was 55% (95%CI: 12%–87%) during the pandemic.
Conclusions
This meta-analysis provides evidence supporting an increase in the pooled prevalence of mental health disorders among patients suffering from EDs during the COVID-19 pandemic.
Keywords: Humans, COVID-19, Eating disorders, Prevalence, Mental health, Meta-analysis
1. Introduction
The COVID-19 pandemic caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has spread around the globe in the past year in an alarming way. It was declared as a pandemic by the World Health Organization (WHO) on March 11th, 2020 [1]. To minimize its transmission, strict measures have been implemented worldwide such as quarantine and social distancing. It has caused panic and fear to build up, posing a global threat on physical and mental health [2]. It has been hypothesised that the COVID-19 pandemic may worsen the risk factors associated with overeating and unhealthy weight gain, especially in vulnerable populations such as children and individuals with obesity as well as eating disorders (ED) [3].
Eating disorders are serious psychiatric disorders characterised by atypical weight-control behaviours or abnormal eating. Disturbed attitudes towards weight, body shape, and eating behaviours play a key role in their origin and maintenance [4]. All eating disorders considerably impair psychosocial functioning and disrupt physical health. Categories of eating disorders as classified by The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition also known as (DSM-5) include anorexia nervosa (AN), bulimia nervosa (BN), binge eating disorder (BED), avoidant-restrictive food intake disorder (ARFID), pica, rumination disorder, other specified feeding or eating disorders (OSFED), and unspecified feeding or eating disorder (UFED) [5]. A systematic review of 94 studies has estimated that the prevalence of lifetime eating disorders was 8.4% for women and 2.2% for men [6]. A recent online international survey studied the impact of COVID-19 pandemic on physical activity and problematic eating behaviors in the general population. Unhealthy eating behaviors were exaggerated and physical activity was shown to have decreased during quarantine [7].
Several articles discussed the relationship between EDs and psychopathology which confirm the complexity of these issues and the difficulties in diagnosis and treatment [8]. The relationship between mental disorders and eating disorders is bidirectional as both affect each other. COVID-19 stay-at-home regulations and major worldwide lockdowns have imposed a global mental health strain [9]. It is well-established that patients with eating disorders are already particularly well-characterized by eating-related concerns and are known to suffer from various psychological comorbidities [10]. It is important to note that patients with mental disorders struggled previously in the past during different pandemics such as Ebola [11]. Thus, the stress of the ongoing pandemic may potentially negatively impact these patients [12]. Several studies have explored the effects of the COVID-19 pandemic on patients with eating disorders. Thus, the aim of this meta-analysis is to investigate the effects of the pandemic on mental health outcomes in patients with eating disorders.
2. Materials & methods
In our study, we have followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines [13]. The following databases; Pubmed, Scopus, GoogleScholar, and medRxiv (preprint server) were searched on the 16th of March, 2021 and updated on 20th of August, 2021, using the following keywords; “COVID-19”, “2019 Novel Coronavirus Disease”, “2019 Novel Coronavirus Infection”, “2019-nCoV Disease”, “2019-nCoV Infection”, “COVID-19 Pandemic”, “COVID-19 Pandemics”, “COVID-19 Virus Disease”, “COVID-19 Virus Infection”, “COVID19”, “Coronavirus Disease 2019, Coronavirus Disease-19, SARS Coronavirus 2 Infection, “SARS-CoV-2 Infection”, “Feeding AND Eating Disorders”, “Appetite Disorders”, “Eating Disorders”, “Eating AND Feeding Disorders”, and “Feeding Disorders”. The authors (BK, AA, DA, and AT) screened retrieved studies by reading the title and abstract and any discrepancy between the authors was solved by discussion. The inclusion criteria were cross-sectional or cohort studies, containing patients with diagnosed eating disorders and who had their mental health disturbances evaluated during the COVID-19 pandemic regardless of the type of eating disorder, age of the patients, or the diagnostic criteria that were used for diagnosis of eating disorders. The exclusion criteria were; studies written in languages other than English, review studies, case reports, and studies that did not include any patient with eating disorders.
The data was extracted by BK, AA, DA, and AT to an electronic spreadsheet table which included the intended variables. The following variables were extracted; country, design, number of participants, age, number of participants who developed worsening of Eating Disorders symptoms, number of participants who developed Depression, number of participants who developed Anxiety and duration of Survey Administration. The quality of the included studies was assessed using the “assessing risk of bias in prevalence studies” tool which has inter-rater agreement of 93% and a kappa value of 0.83; this tool assesses internal and external validity using the following domains; representativeness of the population, adequate sampling frame, random selection of the sample and non-response bias for external validity, as well as collection of data directly from the subjects, acceptable case definition, same method used for data collection was used for all subjects, correct selection of numerator and denominator, the use of validated and reliable tool and appropriate prevalence period for the disease of interest for internal validity [14]. Any study that got a score below 4 was excluded from the analysis. In this meta-analysis, the outcomes of interest were the prevalence of worsening of eating disorders symptoms, depression, and anxiety which were evaluated by using the DSM-V criteria, validated tools, and patient's self-perceptions among eating disorders patients during the COVID-19 pandemic.
The analysis was done using Meta-XL, version 5.3 (EpiGear International, Queensland, Australia). The prevalence of the included studies was the metric of effect size and it was pooled using the random effects model with the double arcsine transformation. Moreover, the heterogeneity was assessed across the studies using Cochrane Q and I2 heterogeneity statistics. The detailed analysis electronic sheet is available in the supplementary material.
3. Results
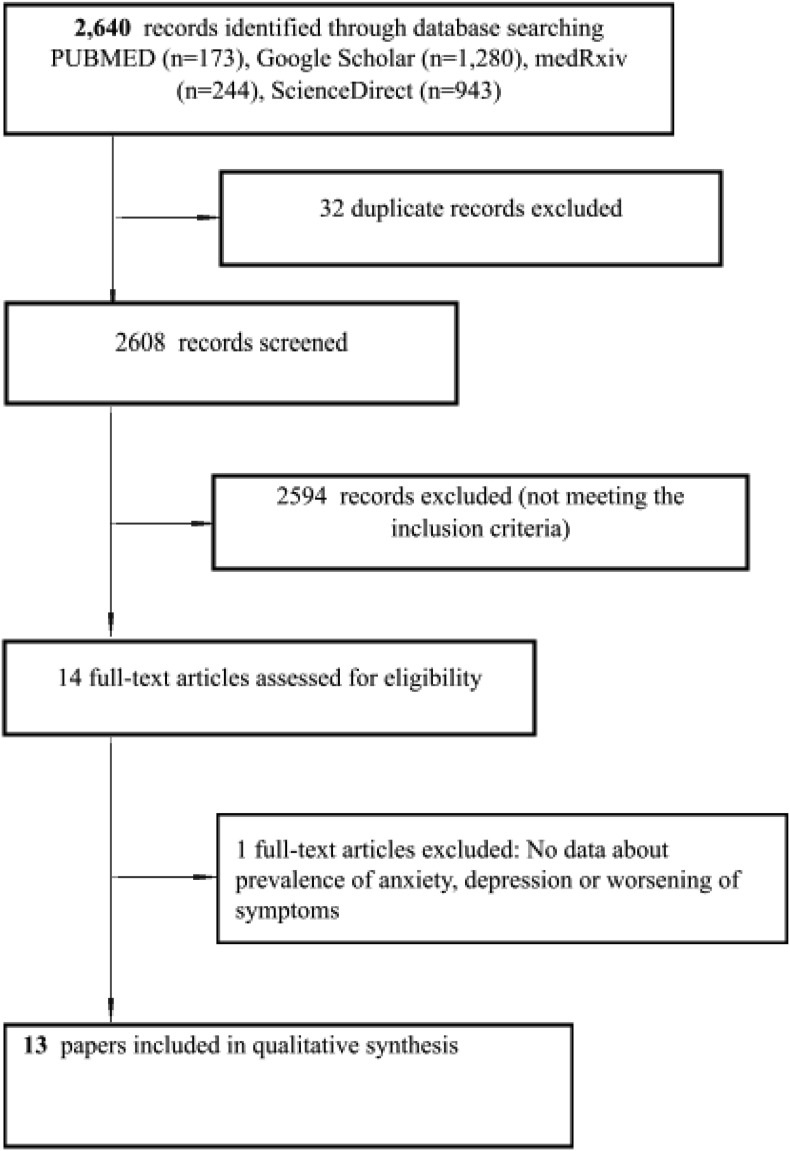
The search yielded 2640 results, after deduplication and applying the inclusion criteria, 13 articles have been included in this meta-analysis (Fig. 1 ) [12,[15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26]] All of the included studies, except one, got a score of 4 [26] or more according to the assessment tool of prevalence studies [14]. None of the studies were excluded based on the score of the quality of assessment.
Fig. 1.
PRISMA Flow Chart: The detailed selection process of the included studies.
The total number of eating disorders patients in this meta-analysis was 3056 participants from 13 different studies (Table 1 ).
Table 1.
The characteristics of the included studies.
| Study | Design | Country | Total Number of Participants | Age (median OR Mean & STDV) | Number of participants who developed worsening of Eating Disorders symptoms (%) | Number of participants who developed Depression (%) | Number of participants who developed Anxiety n (%) | Duration of Survey Administration | Outcomes | Score for External Validity (/4) |
Score for Internal Validity (/6) | Total Score for Assessment Quality (/10) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Schlegl et al. | Cross-sectional | Germany | 159 | 22.4 ± 8.7 | 66/159 (41.5) | N/A | N/A | first week of May 2020 | Eating Disorders Symptoms | 2 | 5 | 7 |
| Phillipou et al. | Cross-sectional | Australia | 180 | N/A | N/A | 140/180 (77.9) | 120/180 (66.7) | April, 2020 | Anxiety and Depression | 3 | 5 | 8 |
| Baenas et al. | cohort | Spain | 74 | 32.12 ± 12.84 | 19/74 (25.7) | 22/74 (29.7) | 31/74 (41.9) | March to May 2020 | Anxiety, Depression and Eating Disorders Symptoms | 3 | 6 | 9 |
| Termorshuizen et al. | Cross-sectional | United States, and Netherlands | 1021 | US: 30.61 ± 9.37 Netherlands: no data | N/A | N/A | USA: 409/511, (80), Netherlands: 332/510 (65) |
April 2020 | Anxiety | 3 | 2 | 5 |
| Richardson et al. | Cross-sectional | Canada | 439 | N/A | N/A | 79/439 (18.0) | 125/439 (28.5) | March to April 2020 | Anxiety and Depression | 2 | 3 | 5 |
| Schlgel et al. 2 | cross-sectional | Germany | 55 | 24.42 ± 6.36 | 27/55 (49.1) | 41/55 (74.5) | N/A | May 2020 | Depression and Eating Disorders Symptoms | 3 | 6 | 9 |
| Bell et al. | cross sectional | UK | 129 | 29.27 ± 8.99 | 110/129 (86.7) | N/A | N/A | April 2020 | Eating Disorders Symptoms | 3 | 3 | 6 |
| QuittKat et al. | Cross sectional | Germany | 62 | Median: 33.2 | 39/62 (63.9) | N/A | N/A | April to May 2020 | Eating Disorders Symptoms | 1 | 3 | 4 |
| Colleluori et al. | Cross-sectional | Italy | 453 | N/A | N/A | N/A | 377/453 (83.3) | March 9th–May18th 2020 | Anxiety | 3 | 4 | 7 |
| Aranda et al. | Pilot cross-sectional study | Spain | 32 | Median: 29.2 | 12/32 (38.0) | N/A | 18/32 (56.2) | N/A | Eating Disorders Symptoms and Anxiety | 2 | 3 | 5 |
| Vuillier et al. | Cross-sectional | United Kingdom | 207 | 30.0± 9.7 |
172/207 (83.1) | N/A | N/A | June to July 2020 | Eating Disorders Symptoms | 3 | 4 | 7 |
| Vitagliano JA et al. | Cohort, Longitudinal | United States | 89 | 18.9 ± 2.9 | 56/89 (63) | 65/89 (73) | 68/89 (77) | July 2020 |
Eating Disorders Symptoms, Depression and Anxiety | 2 | 4 | 6 |
| Birgegård et al. | Cohort, Longitudinal | Sweden | 156 | N/A | 87/156 (56) | N/A | 123/156 (79) | May–July 2020 | Eating Disorders Symptoms and Anxiety | 1 | 4 | 5 |
N/A: Not available.
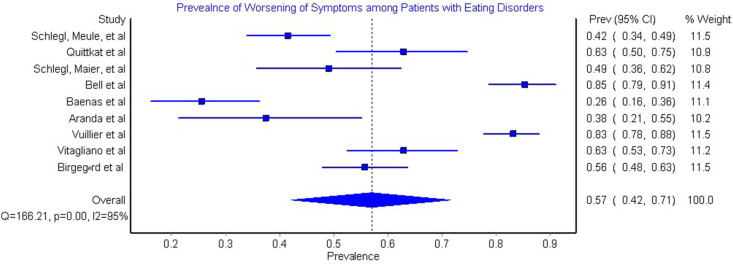
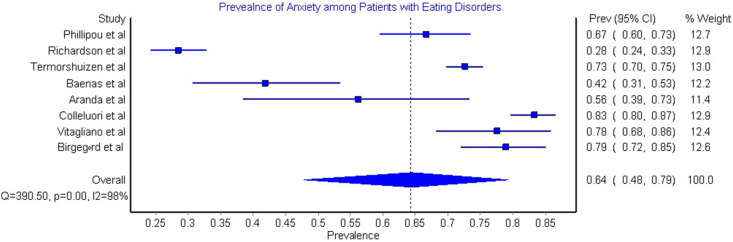
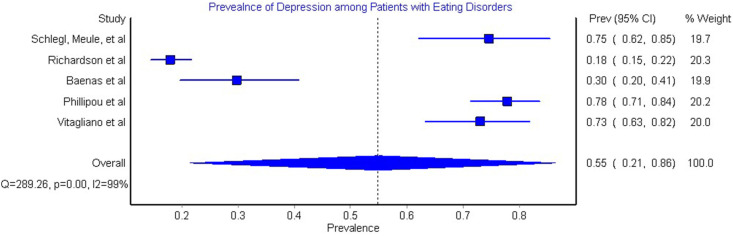
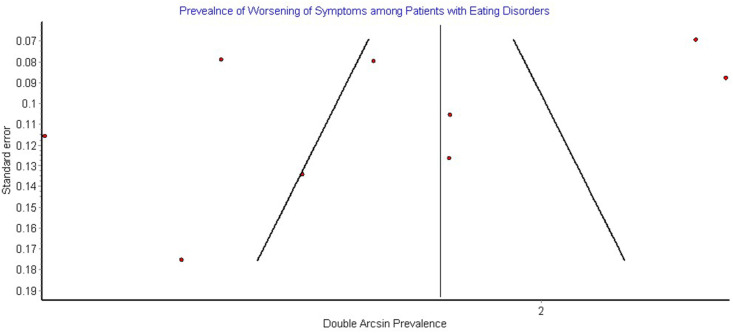
The model that assessed the worsening of ED symptoms, included 963 patients, showed that pooled prevalence of worsening of ED symptoms among ED patients during COVID-19 pandemic was 57% (95%CI: 42%–71%); the heterogeneity of this model was 95% (Q = 166.21, p < 0.001) (Fig. 2 ). In addition, the model that assessed anxiety included 2444 participants and showed that the pooled prevalence of anxiety among eating disorders patients during the COVID-19 pandemic, it was 64% (95%CI: 48%–79%); the heterogeneity in this model was 98% (Q = 390.50, p < 0.001) (Fig. 3 ). Additionally, the model that assessed for depression included 837 patients and showed that 55% (95%CI: 21%–86%) was the pooled prevalence for depression among patients during the COVID-19 pandemic and 99% was the heterogeneity in this model (Q = 289.24, p < 0.001) (Fig. 4 ). The publication bias funnel plot showed significant asymmetry (Fig. 5 ).
Fig. 2.
Prevalence of Worsening of Symptoms among Patients with Eating disorders due to COVID-19: The figure shows that the pooled prevalence of worsening of eating disorders was 57% (95CI: 42%–71%). The heterogeneity in this model was significant.
Fig. 3.
Prevalence of Anxiety among Patients with Eating disorders due to COVID-19: The figure shows that the pooled prevalence of anxiety was 64% (95CI: 48%–79%). The heterogeneity in this model was significant.
Fig. 4.
Prevalence of Depression among Patients with Eating disorders due to COVID-19: The figure shows that the pooled prevalence of depression was 55% (95CI: 21%–86%). The heterogeneity in this model was significant.
Fig. 5.
Publication Bias Funnel Plot: The figure shows asymmetry in the funnel plot indicating significant publication bias.
4. Discussion
Using a verified analytic model, this meta-analysis aims to evaluate the effect of the COVID-19 pandemic on the prevalence rates of depression, anxiety, and worsening of ED symptoms in patients suffering from EDs. Our models showed that the prevalence of worsening of ED symptoms, anxiety, and depression among patients with eating disorders was high.
Our results revealed that the pooled prevalence of anxiety among patients with eating disorders was 64% (95%CI: 48%–79%). Out of the eight studies that evaluated the prevalence of anxiety in eating disorder patients due to the COVID-19 pandemic, two of those studies were conducted in Spain. Those studies showed some variability in terms of prevalence rates for anxiety despite being conducted around the same time, in the same country, and in the same city, resulting in prevalence rates of 56% [12] and 42% [15]. Both studies collected their data using telephone surveys making their results possibly more reliable compared to the other pooled studies in the analysis of anxiety [15]. One study incorporated data from both the Netherlands and the USA which had the highest number of participants included in our meta-analysis [19], with the second highest prevalence rate in anxiety. Another study conducted in the USA reported a prevalence of 77% [20]. On the other hand, the lowest prevalence rate of anxiety was 28% in a study conducted in Canada [16] despite having a high number of participants and a more reliable source of data (National Eating Disorder Information Centre). The highest prevalence rate for anxiety was 83% in a study conducted in Italy [24]. This high rate could be due to the fact that this study was completed upon the experiences of healthcare professionals rather than patients' perception on the matter. Patients tend to downplay their symptoms due to the stigma of mental-health in general. This can also be due to the fact that the data was collected over a longer period of time compared to the other pooled studies in the analysis. In regards to depression, the pooled prevalence of our study was 55% (95%CI: 21%–86%). This prevalence was assessed in five studies with rates of 30%, 78%, 18%, 75%, and 73% in Spain, Australia, Canada, Germany, and USA respectively [15,16,18,20,25]. Previous studies showed that COVID-19 increased the prevalence of depression and anxiety worldwide. Hence, the sequelae of this pandemic will add to the burden of mental health among patients with mental disorders especially eating disorders patients. Reports showed that eating disorders are often underdiagnosed and undertreated [27]; even patients who were under medical care had to receive it via telehealth, which has questionable quality, due to the pandemic's restrictions [19].
The pooled prevalence of worsening of EDs symptoms was 57% (95%CI: 42%–71%). Nine studies were pooled to calculate this prevalence and three of those nine studies were conducted in Germany. Two of those studies conducted in Germany studied a different subtype of eating disorder, in specific anorexia nervosa and bulimia nervosa. Both studies showed similar prevalence rates in regards to worsening of ED symptomatology with rates of 49% for anorexia nervosa patients [18] and 42% in bulimia nervosa patients [17]. In addition, both studies were conducted at the same period. In [18], reasons for worsening of ED symptoms in anorexia patients were due to various maladaptive strategies to help cope with the uncertainty, depression, and anxiety in this case accompanying the pandemic. This relationship between the worsening of ED symptoms and adverse emotions was also portrayed in the results of two other studies [28,29]. On the other hand, a majority of anorexic patients have succeeded in preventing relapse of their symptoms. This could be due to these patients being former inpatients with the knowledge of adaptive coping strategies, receiving therapy throughout the pandemic, having a high BMI, as well as returning back to their families and support groups [18]. In [17] which studied bulimic patients, worsening of overall ED symptomatology because of prolonged lockdown measures, was most likely due to self-induced vomiting, as well as laxative and diuretic abuse. Nonetheless, a majority of these patients had a higher drive for activity during the lockdowns which helped prevent the increase of binge eating. Furthermore, the prevalence of worsening of symptoms in a study conducted in Sweden was 56% and most of the participants explained it by lack of support, lack of structure, and triggering environment [22]. Both studies conducted in Germany [17,18] were compared to two other studies which were also included in our analysis, but were conducted in the U.K [21,25]. There was almost a twofold increase in binging symptoms (83%, 85%) [21,30] in both studies in the U.K. compared to the German studies (42%, 49%). This could be due to the fact that the diagnosis criteria for the studies executed in the U.K. was very broad and patients self-reported their diagnosis of eating disorders. Conversely [17,18], both German studies included former ED inpatients and used ICD-10 data for the diagnosis of eating disorders. Additionally, a Spanish study [12] was the lowest in the prevalence rate of worsening of ED symptoms, with a prevalence rate of 26% which could be attributable to the fact that most patients were already undergoing treatment during the lockdown (98.6%), had social support (94.6%), and only a small percentage (17%) had close people affected by COVID-19.
Eating disorder patients are considered a vulnerable sector of society since they already deal with various psychological stresses due to the nature of their disease. The COVID-19 pandemic has provoked major panic worldwide in general and has also seriously affected those with existing mental health illnesses such as those specifically with eating disorders [31]. The worsening of ED symptoms could be attributed to the general global state of panic accompanying the quarantine and the excessive stocking up of pantries which may have led to severe relapses and purging episodes in ED patients [32]. Moreover, the social isolation and the lockdown measures have left people away from their families and their support networks which has unfortunately led to an increase in ED relapses [30]. Government restrictions such as working from home, the closing of gyms as well as sporting clubs may have also led to an increase in relapse rates in ED patients [33]. The high prevalence rates of anxiety, depression, and relapses among ED patients during a global nationwide pandemic is understandable as such disorder is already long recognized as among the deadliest psychiatric illnesses [34,35]. In addition, the difficulties that patients with EDs face can be conquered by consistent cooperation between the patients and health care providers which might allow patients to maintain their treatment goals [19]. On the other hand, ED patients experienced several positive effects from the pandemic such as connections with family and friends and ability to focus on treatment goals and adapting skills [19].
4.1. Strengths
This meta-analysis has a few strengths. According to our knowledge, it's the first available meta-analysis that examines the detrimental effects of the COVID-19 pandemic on Eating Disorder patients. In addition, our meta-analysis follows the PRISMA guidelines for the standard methods of systematic reviews and meta-analysis. We have also conducted an extensive systematic search throughout various data-bases.
4.2. Limitations
One of the many limitations of this meta-analysis is that not all the pooled studies used universal criteria for the diagnosis of eating disorders such as DSM-5. Moreover, the designs of the included studies were not unified under a single criterion. Although we included preprint repositories (MedRxiv) that contain grey literature, there is a possibility that unpublished data was not included in our study which might affect the results. The heterogeneity and variability were significant ranging from 95% to 99% for all three variables across the studies pooled in the analysis which might affect the results. This is due to the different designs of the included studies, different sample sizes, the inclusion of eating disorder patients, the different diagnostic criteria for ED patients, and the different data collection methods. We were not able to conduct a sensitivity analysis to reduce the heterogeneity as the heterogeneity was equally distributed between the studies. Moreover, the heterogeneity can also be due to the fact that some studies [21,22] assessed patients under certain subtypes of eating disorders (anorexia nervosa and bulimia nervosa) and no other specific subtypes of eating disorders were assessed by any other studies. In addition, the source of the heterogeneity between the included studies was due to the fact that studies used different assessment tools for the adverse effects and complications that arose among ED patients. Furthermore, some of the included studies evaluated these complications using subjective methods which could be of insignificant clinical importance. Consequently, a consensus in the tools used to assess the mental health sequelae among patients with eating disorders is needed. In addition, large well-designed prospective studies are needed to evaluate the effect of the COVID-19 pandemic on EDs patients. Lastly, a significant publication bias was detected in the funnel plot (Fig. 5).
5. Conclusions
In conclusion, this meta-analysis provides evidence that there is an increased prevalence of anxiety, depression, and worsening of eating disorder symptomatology in eating disorder patients during the COVID-19 pandemic. It is vital that we provide unconditional support to ED patients during this period of uncertainty. This could be done through the close monitoring of these patients as well as providing complete support through developing preventive strategies and personalized treatment approaches. We also recommend developing telemedicine interventions and online nutritional support in order to decrease the impact of such psychological distress. In addition, large high-quality randomized controlled trials are needed to evaluate the effectiveness and safety of such interventions in order to be implemented on these patients in future pandemics.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgements
No Acknowledgments.
References
- 1.Listings of WHO's response to COVID-19. https://www.who.int/news/item/29-06-2020-covidtimeline n.d.
- 2.Li J., Yang Z., Qiu H., Wang Y., Jian L., Ji J., et al. Anxiety and depression among general population in China at the peak of the COVID-19 epidemic. World Psychiatr. 2020;19:249–250. doi: 10.1002/wps.20758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rundle A.G., Park Y., Herbstman J.B., Kinsey E.W., Wang Y.C. COVID-19–Related school closings and risk of weight gain among children. Obesity. 2020;28:1008–1009. doi: 10.1002/oby.22813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marcus M.D., Wildes J.E. Obesity: is it a mental disorder? Int J Eat Disord. 2009;42:739–753. doi: 10.1002/eat.20725. [DOI] [PubMed] [Google Scholar]
- 5.Diagnostic and statistical manual of mental disorders (DSM-5®) - American Psychiatric Association - Google Books. https://books.google.jo/books?hl=en&lr=&id=-JivBAAAQBAJ&oi=fnd&pg=PT15&dq=dsm+5&ots=cfOS36KJs9&sig=HmtvmINg7lqMjBf_soVYXMAH5so&redir_esc=y#v=onepage&q=dsm.5&f=true n.d.
- 6.Galmiche M., Déchelotte P., Lambert G., Tavolacci M.P. Prevalence of eating disorders over the 2000-2018 period: a systematic literature review. Am J Clin Nutr. 2019;109:1402–1413. doi: 10.1093/ajcn/nqy342. [DOI] [PubMed] [Google Scholar]
- 7.Ammar A., Brach M., Trabelsi K., Chtourou H., Boukhris O., Masmoudi L., et al. Effects of COVID-19 home confinement on eating behaviour and physical activity: results of the ECLB-COVID19 international online survey. Nutrients. 2020;12:1–14. doi: 10.3390/nu12061583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marucci S., Ragione L.D., De Iaco G., Mococci T., Vicini M., Guastamacchia E., et al. Anorexia nervosa and comorbid psychopathology. Endocr Metab Immune Disord - Drug Targets. 2018;18:316–324. doi: 10.2174/1871530318666180213111637. [DOI] [PubMed] [Google Scholar]
- 9.Shah M., Sachdeva M., Johnston H. Eating disorders in the age of COVID-19. Psychiatr Res. 2020;290:113122. doi: 10.1016/J.PSYCHRES.2020.113122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Citrome L. Binge eating disorder revisited: what's new, what's different, what's next. CNS Spectr. 2019;24:4–12. doi: 10.1017/S1092852919001032. [DOI] [PubMed] [Google Scholar]
- 11.Acharibasam J.W., Chireh B., Menegesha H.G. Assessing anxiety, depression and insomnia symptoms among Ebola survivors in Africa: a meta-analysis. PLoS One. 2021:16. doi: 10.1371/JOURNAL.PONE.0246515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fernández-Aranda F., Casas M., Claes L., Bryan D.C., Favaro A., Granero R., et al. COVID-19 and implications for eating disorders. Eur Eat Disord Rev. 2020;28:239–245. doi: 10.1002/erv.2738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P.A., et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6 doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hoy D., Brooks P., Woolf A., Blyth F., March L., Bain C., et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65:934–939. doi: 10.1016/j.jclinepi.2011.11.014. [DOI] [PubMed] [Google Scholar]
- 15.Baenas I., Caravaca-Sanz E., Granero R., Sánchez I., Riesco N., Testa G., et al. COVID-19 and eating disorders during confinement: analysis of factors associated with resilience and aggravation of symptoms. Eur Eat Disord Rev. 2020;28:855–863. doi: 10.1002/erv.2771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Richardson C., Patton M., Phillips S., Paslakis G. The impact of the COVID-19 pandemic on help-seeking behaviors in individuals suffering from eating disorders and their caregivers. Gen Hosp Psychiatr. 2020;67:136–140. doi: 10.1016/j.genhosppsych.2020.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schlegl S., Meule A., Favreau M., Voderholzer U. Bulimia nervosa in times of the COVID-19 pandemic—results from an online survey of former inpatients. Eur Eat Disord Rev. 2020;28:847–854. doi: 10.1002/erv.2773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schlegl S., Maier J., Meule A., Voderholzer U. Eating disorders in times of the COVID-19 pandemic—results from an online survey of patients with anorexia nervosa. Int J Eat Disord. 2020;53:1791–1800. doi: 10.1002/eat.23374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Termorshuizen J.D., Watson H.J., Thornton L.M., Borg S., Flatt R.E., MacDermod C.M., et al. Early impact of COVID-19 on individuals with self-reported eating disorders: a survey of ∼1,000 individuals in the United States and The Netherlands. Int J Eat Disord. 2020;53:1780–1790. doi: 10.1002/eat.23353. [DOI] [PubMed] [Google Scholar]
- 20.Vitagliano J.A., Jhe G., Milliren C.E., Lin J.A., Spigel R., Freizinger M., et al. COVID-19 and eating disorder and mental health concerns in patients with eating disorders. J Eat Disord. 2021;9 doi: 10.1186/S40337-021-00437-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vuillier L., May L., Greville-Harris M., Surman R., Moseley R.L. The impact of the COVID-19 pandemic on individuals with eating disorders: the role of emotion regulation and exploration of online treatment experiences. J Eat Disord. 2021;9:1–18. doi: 10.1186/s40337-020-00362-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Birgegård A., Abbaspour A., Borg S., Clinton D., Mantilla E.F., Termorshuizen J.D., et al. Longitudinal experiences and impact of the COVID-19 pandemic among people with past or current eating disorders in Sweden. medRxiv. 2021 doi: 10.1101/2021.03.29.21254526. 2021.03.29.21254526. [DOI] [PubMed] [Google Scholar]
- 23.B-B D., CV T. Exploring the impact of the COVID-19 pandemic and UK lockdown on individuals with experience of eating disorders. J Eat Disord. 2020;8 doi: 10.1186/S40337-020-00319-Y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Colleluori G., Goria I., Zillanti C., Marucci S., Dalla Ragione L. Eating disorders during COVID-19 pandemic: the experience of Italian healthcare providers. Eat Weight Disord. 2021 doi: 10.1007/s40519-021-01116-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Phillipou A., Meyer D., Neill E., Tan E.J., Toh W.L., Van Rheenen T.E., et al. Eating and exercise behaviors in eating disorders and the general population during the COVID-19 pandemic in Australia: initial results from the COLLATE project. Int J Eat Disord. 2020;53:1158–1165. doi: 10.1002/eat.23317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Quittkat H.L., Düsing R., Holtmann F.-J., Buhlmann U., Svaldi J., Vocks S. Perceived impact of covid-19 across different mental disorders: a study on disorder-specific symptoms, psychosocial stress and behavior. Front Psychol. 2020;11 doi: 10.3389/FPSYG.2020.586246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Webb Hooper M., Nápoles A.M., Pérez-Stable E.J. COVID-19 and racial/ethnic disparities. JAMA. 2020;323:2466–2467. doi: 10.1001/JAMA.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Frank G.K.W., Roblek T., Shott M.E., Jappe L.M., Rollin M.D.H., Hagman J.O., et al. Heightened fear of uncertainty in anorexia and bulimia nervosa. Int J Eat Disord. 2012;45:227–232. doi: 10.1002/eat.20929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Naumann E., Tuschen-Caffier B., Voderholzer U., Svaldi J. On the role of sadness in the psychopathology of anorexia nervosa. Psychiatr Res. 2014;215:711–717. doi: 10.1016/j.psychres.2013.12.043. [DOI] [PubMed] [Google Scholar]
- 30.Branley-Bell D., Talbot C. Exploring the impact of the COVID-19 pandemic and UK lockdown on individuals with experience of eating disorders. 2020. pp. 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Power M., Doherty B., Pybus K., Pickett K. How COVID-19 has exposed inequalities in the UK food system: the case of UK food and poverty. Emerald Open Res. 2020;2:11. doi: 10.35241/emeraldopenres.13539.2. [DOI] [Google Scholar]
- 33.Rodgers R.F., Lombardo C., Cerolini S., Franko D.L., Omori M., Fuller-Tyszkiewicz M., et al. The impact of the COVID-19 pandemic on eating disorder risk and symptoms. Int J Eat Disord. 2020;53:1166–1170. doi: 10.1002/eat.23318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fichter M.M., Quadflieg N. Mortality in eating disorders - results of a large prospective clinical longitudinal study. Int J Eat Disord. 2016;49:391–401. doi: 10.1002/eat.22501. [DOI] [PubMed] [Google Scholar]
- 35.Preti A., Rocchi M.B.L., Sisti D., Camboni M.V., Miotto P. A comprehensive meta-analysis of the risk of suicide in eating disorders. Acta Psychiatr Scand. 2011;124:6–17. doi: 10.1111/j.1600-0447.2010.01641.x. [DOI] [PubMed] [Google Scholar]