Abstract
The COVID-19 crisis has fundamentally changed how many businesses operate and connect with their customers. Previously unheard-of government restrictions and sheltering-in-place requirements forced most professional services to transition to remote delivery methods (e.g., email, telephone, video consults, Shopify storefronts). Providers of low-touch services (e.g., lawyers, accountants) naturally lent themselves to remote delivery; however, those that offer high-touch services, particularly those in healthcare (e.g., doctors, chiropractors, physical therapists), experienced a drastic change in working conditions when going virtual. Despite a long history of resistance to virtual delivery, the pandemic created an unprecedented incentive for these high-touch professionals to experiment with underutilized care models such as telehealth: the provision of healthcare services remotely using telecommunications technologies. We examine the rapid adoption of telehealth during COVID-19 through the coming together or convergence of previously unrelated technologies, spaces, and practices. Our analysis reveals opportunities and challenges associated with going hands-off that apply to many other professionals providing high-trust services. Specifically, we offer nine guiding principles for building and protecting cognitive and affective trust in virtual and hybrid delivery models. This is important given the pace of compounding technology convergences that lie ahead for service professionals.
Keywords: Innovation, Telehealth, Virtual work, Remote work, Convergence, Technology, Trust
1. Crisis-inspired innovations
Michael Cimino, who produced the great antiwar movie The Deer Hunter, once opined: “There’s nothing good that comes out of war. It’s simply hell on earth, and people survive, and people don’t” (Abramovitch, 2015). While Cimino’s statement is of course correct, there is evidence that something good can indeed come out of warfare. Many of the innovations that are part of our lives today had their origins in terrible crises and wartime struggles. These include various technology innovations ranging from microwave ovens, drones, and GPS systems to antibiotics such as penicillin (Beecher, 1955; Boot, 2007; Satell, 2015).
Rightly or wrongly, the COVID-19 pandemic has been likened to war (Isaacs & Priesz, 2021), and it has already delivered many innovations. Aside from countless initiatives aimed at discovering effective vaccines and serology tests (NIH, 2020), there have also been innovations in mass-producing more ventilators (Shepardson, 2020), hand sanitizers, and face masks (Dhillon et al., 2020), to name but a few. In a broader business context, the COVID-19 pandemic has accelerated the widespread adoption of alternative technology-mediated practices including working from home and communicating via videoconference, as well as buying and selling goods and services online.
The transitioning of professional services from in-person to remote or virtual delivery has been particularly challenging. During the pandemic, rules governing the behavior of citizens and organizations have changed quickly and often (Hannah et al., 2021). Businesses and customers were often unsure about what the next week, let alone the next day, would bring and often had to alternate between providing online and in-person services or a combination of both. For some, the transition to working virtually was relatively straightforward and did not change the nature of the work being done. Specifically, industries employing low-touch professionals (e.g., accountants), those with lower needs to be physically present with their clients to provide service, naturally lent themselves to remote service delivery methods since extant computer systems supported easy file sharing. But what about high-touch professionals, particularly those in healthcare (e.g., doctors), whose services were always highly dependent on the co-presence and physical interaction between provider and client?
In this article, we examine the adaptive experiences of these high-touch professionals to show that remote service delivery presents an opportunity to rethink and redefine processes and the roles of service providers and their clients. Specifically, we illuminate the important influence of the coming together or convergence of previously unrelated technologies, spaces, and practices (Papacharissi, 2010) on the hands-on to hands-off service paradigm shift. Our analysis of these convergences demonstrates that virtual service delivery requires both providers and clients to embrace new social norms, not only in healthcare delivery but in any service that necessitates a high level of trust. We offer nine guiding principles to establish and maintain trust when going virtual, whether inspired by the COVID-19 pandemic, or as part of a post-pandemic reality characterized by consumers demanding more online offerings.
2. When high-touch professionals go virtual
In describing the heterogeneous effects of the pandemic on various occupations, the Federal Reserve Bank of St. Louis offered a “proximity index” that measures how much physical contact certain jobs require (Leibovici et al., 2020). On the index, 15 occupations were deemed contact-intensive, the majority of which were from healthcare (e.g., occupational/physical therapists, home health/personal care aides, doctors/nurses). Given the contact-intensive nature of their work, performing services from a distance may have once seemed impossible, and most of these professionals would not have attempted it without the pressures associated with COVID-19 (Wosik et al., 2020). Indeed, technologies enabling telehealth emerged more than 30 years ago but were largely underutilized before the pandemic despite sufficient evidence for the efficacy of telehealth for the treatment of a variety of conditions (Cottrell et al., 2017; Dario et al., 2017; Mani et al., 2017).
COVID-19 provided the thrust that telehealth so badly needed as several systemic barriers to its adoption were effectively removed. Insurance companies and other funding providers revised their policies to cover virtual medical consultations, while regulatory bodies relaxed practice boundaries, provided telehealth training, and published updated practice guidelines that included telehealth (Smith et al., 2020). These actions, combined with an increased interest in online health services among the public, added pressure to healthcare businesses to innovate and adopt virtual service solutions (Harpaz, 2020). Seemingly overnight, healthcare providers and patients alike overcame what were thought to be deeply entrenched barriers to telehealth and embraced a fundamentally different service delivery model.
2.1. Telehealth and the convergences of technologies, spaces, and practices
To illuminate key insights from the complex transition from in-person to virtual health service delivery, it is useful to draw on the concept of convergences, defined by Papacharissi (2010, p. 53) as “trends and practices within and beyond technology, which describe how individuals connect with their everyday environments through habits of social, political, economic, and cultural texture.” Said another way, convergences describe previously distinct objects, activities, and physical settings coming together or evolving into one over time. In the case of convergence of technologies, previously unrelated technologies become more closely integrated (Borés et al., 2003; Yoffie, 1996), and in some cases unified. For example, the smartphone becoming an all-in-one device performing the functions of watches, timers, calculators, cameras, music players, video games, and many more.
Building on the concept of convergence of technologies, Papacharissi (2010, p. 68) introduced two new dimensions: convergence of spaces, which refers to “the collapse of public and private boundaries that separate spheres of work, domesticity, leisure, civic life, and other individual activities,” and convergence of practices, which describes the tendency for activities to become separated from physical spaces such as office work being completed from home or a coffee shop (Castells, 2000, 2011). Together, each of these convergences affects and is being affected by the other two, as shown in Figure 1 . The compounding influence of the convergences results in complex changes in social norms that occur as businesses transition from in-person to online service delivery. By analyzing telehealth adoption through the lens of convergences of technologies, spaces, and practices, we can begin to make sense of what were systemic and transformative service delivery changes among high-touch professionals that provide lessons for any business going virtual.
Figure 1.
Interconnected convergences of practices, spaces, and technologies
2.2. Convergence of technologies and webside manner
When transitioning away from in-person delivery and redefining existing roles and relationships in a virtual practice, technology plays a major role. The mediated context of telehealth requires that the originally unrelated technologies of providers (e.g., systems in clinics) and recipients (e.g., laptops, phones) become more closely integrated and even unified. As a result, telehealth practitioners have realized that careful steps need to be taken to ensure that patients feel comfortable interacting with their healthcare providers in a new way via technology. For this to occur, patients and healthcare providers need to learn new social norms that guide online behavior, technical confidence (Konttila et al., 2019), and the soft skills for building relationships virtually. When in a physical setting, practitioners can use their well-honed bedside manners and express their empathy through the physical setup of their office, their conversation, and their body language. But when going virtual, an appropriate webside manner needs to be learned and practiced (Edelson, 2018; Rethorn et al., 2021). At the same time, building the virtual social competency (Baron & Markman, 2003) of patients is also necessary to ensure that they can handle online interactions effectively and participate fully in telehealth visits.
As patients and healthcare providers become more comfortable with and increase their confidence in telehealth, they are more likely to embrace complementary technologies with the potential to improve planning and compliance with health treatments. Following convergence of technologies, many popular consumer technologies such as the iPhone and Apple Watch have integrated the functions of previously unrelated technologies (e.g., telephone and pedometer into one device), making it easy to collect biometric data. Other inventions such as KardiaMobile, a handheld device that allows consumers to produce a medical-grade EKG with their smartphone, facilitate more complex medical tests to be conducted at home.
Such remote monitoring technologies are not only more convenient for patients, but also have the potential to lower the cost barrier for various medical assessments, eliminate issues with the unreliability of self-reported data, and increase the quality and quantity of data used to make medical decisions (Russell, 2007). However, when sharing information online and handling biometric data, health professionals need to address the collection, sharing, and remote monitoring of patient information carefully (Mills et al., 2016). As such, concerns about data privacy, protection and storage, and jurisdictional laws need to be taken into account when selecting appropriate telehealth technologies and remote monitoring apps (Russell, 2007).
2.3. Convergence of spaces and virtual consultations
Not only does telehealth free practitioners and patients from spatial constraints when moving from physical to virtual architectures for service delivery, but it also frees them from temporal requirements across various contextual situations. As people communicate and interact with technology in different scenarios, they need to shift among different contexts (Kakihara & Sørensen, 2004). When using telehealth, a living room becomes a treatment space, and parents—or children or roommates—become medical assistants to help with the assessment and treatment of loved ones (Lerman et al., 2020). As such, telehealth consultations have the potential to disrupt home life, especially when spaces are shared. Depending on the type of treatment, these disruptions range from unobtrusive to obtrusive and from ephemeral to persistent (Ljungberg & Sørensen, 2000). For health practitioners, this has meant that spatial-temporal issues need to be taken into consideration, as the same facilities cannot be guaranteed and assessments and treatments may take longer.
However, in comparison with the clinical atmosphere of a medical treatment center, the home environment can be seen as nonthreatening and, as such, increase communication, honesty, and trust between patient and provider (Pinto et al., 2012). Since telehealth brings about the convergence of clinic and home spaces, it gives medical practitioners a unique opportunity to understand the setting in which patients are living and, ultimately, hurting. Practitioners such as physical therapists can coach patients through the exact logistics of how, where, and with what equipment they can perform their home rehabilitation programs, thus increasing the likelihood of patient compliance (Russell, 2007). The convenience of telehealth may also lead to more frequent, albeit shorter healthcare visits and an uptake in preventative medicine. Looking ahead, this has the potential to decrease costs and even shift pricing standards from fee-for-service to subscription-based models in which providers monitor and manage their patients’ health remotely.
While some healthcare providers operating completely online have emerged (e.g., doctorondemand.com), critics question the feasibility and effectiveness of convergence of spaces and practices into solely remote delivery (Miller, 2007). Despite advances in the technologies that support telehealth and remote patient monitoring, working exclusively online may present a risk that something may be missed or that necessary in-person treatment is delayed. Today, it is not possible for certain essential treatments and assessments such as chemotherapy, radiation therapy, high-risk joint manipulations, and x-ray and MRI imaging to be performed online. While the pandemic has caused everyone to realize that a great deal can be done online— including follow-up appointments, health check-ins, and group rehabilitation programs—healthcare providers operating in a post-COVID world may be more likely to adopt a hybrid model of in-person and remote care (Rutter et al., 2020). In this way, the telehealth revolution spurred by COVID-19 may not cause all spaces to converge. Certain settings will continue to be associated with specific social roles, particularly in cancer treatment and acute care settings. However, as telehealth is used more frequently and patient and practitioner practices, technologies, and spaces converge, the costs and benefits of using remote care models are expected to be weighed through a shared decision-making process that is much more transparent and patient-centered (Ozanne et al., 2020).
2.4. Convergence of practices and therapeutic alliances
Many standardized and widely used healthcare delivery methods are, unsurprisingly, not appropriate during a pandemic that demands physical distancing. Therefore, in adopting telehealth and remote monitoring technologies, a fundamental reconceptualization of the behaviors, roles, and relationships of everyone involved in the healthcare encounter is necessary. In this way, virtual health service delivery challenges deeply entrenched labels—including doctor and patient—that carry important metaphoric meanings in their relationship to each other (McLaughlin, 2009). The label doctor, for instance, describes experts, traditionally from the medical or theological fields, who can deal with and explain matters of the body or soul. A doctor once was seen as an eminent specialist and a teacher of a kind—docēre, in Latin, means to teach—whereas the patient was one who suffers while passively and unwearyingly awaiting the outcome of the treatment of doctors.
With telehealth, the relationship between doctor and patient, a relationship in which power has historically been unevenly distributed, turns into more of a therapeutic alliance with health providers and patients working more closely and communicating more openly (Simpson et al., 2021). Instead of doing something to the patient in person, virtual care models require health professionals to adopt the mindset of doing something with the patient from a distance. By effectively removing the expectation or temptation to use hands-on treatments, telehealth provides more opportunities for practitioners to listen to patients and engage in shared decision-making strategies (Lingely-Pottie & McGrath, 2006). Meanwhile, patients—who were once viewed as passive recipients of care—are required to become more actively involved in their medical interventions; this approach has already been shown to improve clinical outcomes in numerous research studies (Ferreira et al., 2013; Fuentes et al., 2014). In this way, the success of telehealth is driven by a realignment of the roles everyone plays in new technologically mediated relationships despite the labels remaining.
3. Building and protecting trust when going virtual
The challenges and opportunities that high-touch professionals faced when initially transitioning to telehealth reveal many insights for all service professionals. Stepping back to consider these collective lessons reveals that building and protecting trust is at their core. Trust is critical between clients and many service providers including healthcare providers, personal trainers, interior designers, lawyers, accountants, auto mechanics, investment advisors, tailors, barbers, and counselors, among others. Trust—defined as “the willingness of a trustor to be vulnerable to the actions of a trustee based on the expectation that the trustee will perform a particular action” (Colquitt et al., 2007, p. 909)—comprises both cognitive and affective components. As detailed by Johnson and Grayson (2005, p. 501), cognitive trust is “a customer's confidence or willingness to rely on a service provider's competence and reliability, while affective trust is formed “on the basis of feelings generated by the level of care and concern” enacted by the service provider. If cognitive trust and emotional trust are established then trusting behavior will follow (Lewis & Weigert, 2012). This is not unlike trusting behavior in a classroom that happens when professors are perceived as both credible (cognitive trust) and likable (affective trust). One alone is rarely enough.
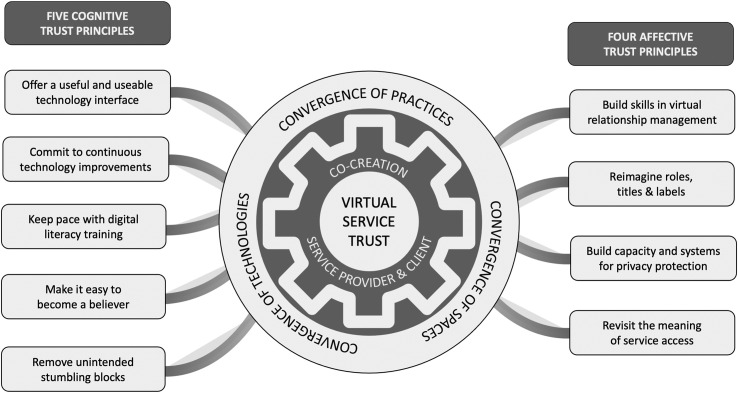
Cognitive trust and affective trust and their relationship to behavior have also been found to hold in virtual settings (Ha et al., 2016; Punyatoya, 2019). Our analysis of the convergence of technologies, spaces, and practices in telehealth (Section 2) provides insights into effectively fostering trust in computer-mediated, or hybrid service delivery models. We propose nine guiding principles for service professionals in various industries to foster cognitive and affective trust when going virtual. These principles are summarized in Figure 2 .
Figure 2.
Nine key principles for building virtual service trust
3.1. Five key principles for building cognitive trust in virtual service delivery
Cognitive trust is knowledge-driven and built significantly through judgments by clients of competency. In reflecting on the lessons learned from telehealth, five guiding principles are revealed for protecting and growing cognitive trust.
3.1.1. Cognitive trust principle #1: Offer a useful and useable technology interface
Service clients make cognitive trust judgments based on the technology-user interface. The overall goal is that the technology is perceived as being useful (i.e., a valuable solution to a problem) and usable (i.e., it is easy to use; Kietzmann, 2008). These two subjective elements shape both clients’ and staffs’ overall attitudes toward technology, the intention to adopt it, and, consequently, the success of remote service delivery. Technical elements like platform stability, network reliability, and speed are important since even perceived failure can decrease cognitive trust in an instant or over time (Raju et al., 2021). Frustrations over wasted time in appointments, meetings, or consultations due to technical problems can erode clients’ competency and reliability assessments. Technological bells and whistles should be eschewed in favor of solid and reliable functionality, as well as a user-friendly interface for all participants that includes considerations for language style and complexity. In addition, consideration needs to be given to the importance of technology standardization across professions or geography. At the outset of the transition to virtual delivery, many service professionals reached for whatever online tools were readily accessible. As a result, many different platforms were adopted. Later down the road, it may be important to step back and consider whether standardization will help build competency and reliability, thus accommodating the convergences of spaces and practices across cities, regions, partners, professional associations, suppliers, and others.
3.1.2. Cognitive trust principle #2: Commit to continuous technology improvements
Competency in practice will only be assured if service professionals commit to keeping pace with hardware and software technology changes that improve not only the efficacy of the services being delivered (e.g., AI developments) but also the practical logistics of the client-practitioner interface (e.g., time-saving appointment booking apps). Such improvements will not only ensure the success of virtual practice but may also build competitive advantage. To realize these benefits, service professionals will need to commit to scanning their boundaries to assess and adopt emerging new technologies in a continuous technology-under-development improvement cycle (Kietzmann, 2008). In doing so, a key consideration should be whether the chosen or developed technology is malleable enough to accommodate future changes.
3.1.3. Cognitive trust principle #3: Keep pace with digital literacy training for staff and clients
Technology improvements will only be beneficial if clients perceive that they are being implemented competently to enhance service delivery. This necessitates an aggressive approach to technical skills training for service professionals and their support staff to keep pace with the evolving convergence of practices. Perception is reality in customer service delivery (Loeffler & Church, 2015). Customers are more likely to make negative competency attributions to the firm than to themselves for any problems that they experience accessing or navigating virtual services (Demoulin & Djelassi, 2013). Therefore, service providers also need to implement technical training for their clients, as appropriate, to ensure that virtual services can be delivered as envisioned.
3.1.4. Cognitive trust principle #4: Make it easy to become a believer
Concerns about service competency can make clients reticent to try virtual delivery models. Helping to lower the perceived risk will help these clients get to yes. Organizations hoping to promote the perception of competency, lower perceptions of riskiness, and build clients’ cognitive trust should consider implementing the following actions:
-
•
Providing opportunities for present and future clients to test drive remote delivery methods as a way to make low-risk assessments of providers’ competencies in virtual practice;
-
•
Creating what-to-expect videos or other supportive learning and promotional tools; and
-
•
Hosting and promoting high-quality and credible reviews of new virtual services (Leung & Ma, 2020).
To forestall fraudulent claims of professional expertise, it should be easy for potential clients to verify licensing, professional college registration, professional designations, and other such competency credentials with accrediting bodies.
3.1.5. Cognitive trust principle #5: Remove unintended stumbling blocks
Service professionals need to review contracts, bylaws, regulations, constitutions, policies, procedures, and agreements to ensure that there are no unintentional barriers in the way of facilitating the convergence of spaces and practices online, both within and outside of their organizations’ boundaries. This review should also extend to key performance indicators, and compensation and reward programs. Virtual delivery means that it is possible to partner with other service professionals anywhere in the world to augment or extend service offerings and enhance the value provided to clients. However, there could be unexpected barriers to such well-intentioned coordination that need to be surfaced and addressed. As well, compensation contracts and service agreements will need to be written that eliminate any unintended friction to virtual practice that builds cognitive trust.
3.2. Four key principles for building affective trust in virtual service delivery
Affective trust is built largely on personal experience and arises from judgments of relationship commitment and quality. In reflecting on the lessons learned from a review of the hands-on to hands-off telehealth transition, four guiding principles are revealed for protecting and growing affective trust pertinent to all service professionals going virtual.
3.2.1. Affective trust principle #1: Build skills in virtual relationship management
Service professionals must be intentional in building and evolving their soft skills, and those of their staff, to create effective digitally mediated client relationships. Training in the equivalent of an effective webside manner will need to be an ongoing project for all types of service providers adapting their offerings to the online space. As the sociocultural environment changes based on the compounding of convergences of technologies, spaces, and practices of society, so too will the expectations and judgments of clients on what constitutes an effective service professional relationship. If evolving expectations are not met, affective trust will erode. In this way, not everyone may be suited to building and maintaining virtual relationships (LaGrandeur & Hughes, 2017). Service professionals will continually need to assess whether an employee is suited to in-person, hybrid, or virtual delivery models as requirements and technologies change. In some cases, it may be effective to designate staff to only face-to-face or virtual delivery instead of adopting jack-of-all-trades expectations.
3.2.2. Affective trust principle #2: Reimagine roles, titles, and labels
The convergences of technologies, spaces, and practices should drive service professionals to recognize the reality of constantly evolving relationship expectations in which affective trust must be fostered. Whether it is with employees, colleagues, or customers, adopting virtual service delivery requires everyone to rethink historically rooted labels, roles, and relationships. As labeling theory suggests, the terms we use to refer to one another are often indicative of conventional in-person service level obligations and service level expectations (Plangger et al., 2013). Service providers should commit to reimagining service roles and customer relationships, and adjust the implicit and explicit expectations, both internally and externally, that are associated with redefined responsibilities. Providers also need to be prepared to relabel these roles if traditional labels prove to get in the way of signaling the expectations of new practices and shared alliance-based responsibilities, central to judgments of affective trust.
3.2.3. Affective trust principle #3: Build capacity and systems for privacy protection
Judgments of affective trust are highly susceptible to perceived breaches in privacy. Service professionals need to establish strong policies, procedures, and technology to guard against any perceived weaknesses in how clients’ personal information collected online is managed (Durnell et al., 2020). This means that priority needs to be given to data safety, security, and storage. Policies and procedures also need to take into account internal and external expectations for data retention and data sharing. As part of these considerations, it will be important to weigh what personal data does and does not need to be collected, and what client data can and should be collected remotely. These considerations become increasingly complex if there are multiple, perhaps international, partners delivering an integrated service to a client.
3.2.4. Affective trust principle #4: Revisit the meaning of service access
Access is likely to be judged by clients as an issue of affective trust (i.e., Do you or do you not empathize with me, as a busy person with a busy life?). Clients’ evolving socio-cultural expectations on access may become a significant competitive point of leverage for businesses that embrace online service delivery. With the convergence of spaces and the convenience of virtual service delivery come new client expectations for greater flexibility in service access. Service professionals who respond by evolving their practice to include early morning, evening, weekend, and holiday options may be viewed as more empathetic and gain a competitive edge. As well, since it is more efficient to do so, there may be heightened expectations among clients for more frequent contact, check-ins, and/or follow-ups, which may impose pressures for providers to adopt subscription-based delivery and other changes in pricing models. Not offering these options, or not providing simplified access to these myriad options, could erode affective trust and result in significant financial losses.
3.3. Co-creation and trust-proofing the future of virtual service delivery
The observant reader will have by now taken note that the convergences of technologies, spaces, and practices are constantly churning. Our analysis of healthcare professionals’ responses to the COVID-19 crisis and adoption of telehealth represents just a snapshot in time, during a health crisis. Clearly, had this pandemic hit in 1960, 1980, or 2000 instead of 2020, our analysis would look very different. The available technology in clinics, offices, and homes greatly shaped effective telehealth implementation. Many of us had partially or fully moved our banking, shopping, advice seeking, and friendships online. These practices were already trusted and deemed socially acceptable and culturally appropriate. Looking forward, the compounding influence of the convergences of technologies, spaces, and practices means that there is effectively no status quo as consumers’ expectations for service delivery constantly evolve.
Many forecasters argue that the hybrid—that is, combined virtual and face-to-face—delivery model recently embraced by many high trust businesses, like telehealth, is here to stay. However, as technology evolves, services that cannot be delivered virtually today, such as chemotherapy treatment or haircuts, may be possible tomorrow. This could shift more and more service delivery to a virtual model. As service professionals migrate more and more of their business practice online, what constitutes an effective provider-client relationship will also evolve. In addition, there are strong incentives to eliminate the expenses of costly commercial office space needed for client meetings and the air pollution that results from commuting long distances in cars. In the future, companies may gravitate back to home-based visits, when necessary, where the service provider comes to the client’s home instead of vice versa. Consider further that, as humans, there may be a threshold beyond which we are unprepared to go in limiting our in-person daily/monthly/annual interactions with others, including our service providers (Kirk & Rifkin, 2020). While much remains unclear, it is certain that change spurred by the convergences of technologies, spaces, and practices, as well as the compounding effects of one on the other, is endemic to our time.
As we outlined above, if the elements in Figure 1 continue converging, it becomes increasingly complex to try to predict and “see” how future service responses to change can erode clients’ cognitive and affective trust. Understanding and responding effectively to client expectations concerning the actual service being performed—and the relationship necessary for its effective performance—will be a constantly moving target. It has been helpful to see and benefit from the lessons learned from the implementation of telehealth, but this has only been possible through the retrospective lens of co-creation.
Co-creation, exemplified here in part through therapeutic alliances, enables service professionals to be prospective. Importantly, co-creation approaches build trust (Sheth & Uslay, 2007). While there are many conceptualizations, co-creation can be understood as customer-focused “collaboration in the creation of value through shared inventiveness, design, and other discretionary behaviors” (Ostrom et al., 2010, p. 24). Co-creation can be understood as comprising two aspects. The first is task performance which represents the “functional, collaborative involvement in the production of services” (Groth, 2005, p. 10), comprising “those processes where the customer undertakes activities and interactions which have traditionally been undertaken by an employee of a firm” (McColl-Kennedy & Cheung, 2018, p. 64). The move to virtual delivery for some service professionals—and certainly all telehealth professionals—has meant that they are effectively engaging in task performance by actively involving clients in performing tasks that were previously accomplished by the service provider.
However, some may be overlooking the second component of co-creation, customer citizenship behavior, which “supports the social and psychological environment in which task performance takes place” (Groth, 2005, p. 9). Understandably, at this time, many service professionals have been focused on getting their services online as soon as possible to survive the pandemic. If these professionals are going to thrive in the online space in the long term, then they will need to consider how they can engage with their clients proactively and create virtual environments that foster both components of co-creation. Service professionals who strategically adopt a co-created delivery model may be better positioned to match and exceed client value expectations that will help trust-proof their businesses in the short and long term. We have signaled this co-creation imperative by locating it as the protective trust buffer to the convergences of technologies, spaces, and practices in Figure 2.
4. Surviving and thriving when going virtual
Healthcare professionals, who were some of the most unlikely adopters of virtual delivery, discovered new ways to provide their services that both overcame challenges and introduced new ways to co-produce value with their patients. Much can be learned from the rapid transition from hands-on, in-person care to hands-off, telehealth service delivery made by an unprecedented number of health professionals during COVID-19. Most importantly, if high-touch professionals can successfully transition their services to remote delivery methods, then so too can almost any business. However, the continued convergences of technologies, spaces, and practices mean that unless service professionals are mindful of the hazards in moving to virtual delivery models, they can inadvertently undermine their clients’ cognitive and affective trust. We have offered nine principles (Figure 2) that will help guide service professionals in protecting and growing this trust. Overall, as the telehealth example shows, businesses that continue to embrace technology-driven changes in service delivery, while mindfully trust-proofing their virtual responses, stand to survive and thrive during COVID-19 and beyond.
References
- Abramovitch M. Hollywood Reporter; 2015, March 2. Michael Cimino: The full, uncensored Hollywood reporter interview.https://www.hollywoodreporter.com/news/michael-cimino-full-uncensored-hollywood-778288 Available at. [Google Scholar]
- Baron R., Markman G. Beyond social capital: The role of entrepreneurs’ social competence in their financial success. Journal of Business Venturing. 2003;18(1):41–60. [Google Scholar]
- Beecher H.K. The powerful placebo. Journal of the American Medical Association. 1955;159(17):1602–1606. doi: 10.1001/jama.1955.02960340022006. [DOI] [PubMed] [Google Scholar]
- Boot M. Gotham Books; New York, NY: 2007. War made new: Weapons, warriors, and the making of the modern world. [Google Scholar]
- Borés C., Saurina C., Torres R. Technological convergence: A strategic perspective. Technovation. 2003;23(1):1–13. [Google Scholar]
- Castells M. Toward a sociology of the network society. Contemporary Sociology. 2000;29(5):693–699. [Google Scholar]
- Castells M. Vol. 12. Edward Elgar; Northampton, MA: 2011. (The rise of the network society). [Google Scholar]
- Colquitt J.A., Scott B.A., LePine J.A. Trust, trustworthiness, and trust propensity: A meta-analytic test of their unique relationships with risk taking and job performance. Journal of Applied Psychology. 2007;92(4):909–927. doi: 10.1037/0021-9010.92.4.909. [DOI] [PubMed] [Google Scholar]
- Cottrell M.A., Galea O.A., O’Leary S.P., Hill A.J., Russell T.G. Real-time telerehabilitation for the treatment of musculoskeletal conditions is effective and comparable to standard practice: A systematic review and meta-analysis. Clinical Rehabilitation. 2017;31(5):625–638. doi: 10.1177/0269215516645148. [DOI] [PubMed] [Google Scholar]
- Dario A.B., Cabral A.M., Almeida L., Ferreira M.L., Refshauge K., Simic M., et al. Effectiveness of telehealth-based interventions in the management of non-specific low back pain: A systematic review with meta-analysis. The Spine Journal. 2017;17(9):1342–1351. doi: 10.1016/j.spinee.2017.04.008. [DOI] [PubMed] [Google Scholar]
- Demoulin N.T.M., Djelassi S. Customer responses to waits for online banking service delivery. International Journal of Retail and Distribution Management. 2013;41(6):442–460. [Google Scholar]
- Dhillon R., Karan A., Beier D., Srikrishna D. We need better masks. Harvard Business Review. 2020, June 18 https://hbr.org/2020/06/we-need-better-masks?ab=hero-subleft-2 Available at. [Google Scholar]
- Durnell E., Okabe-Miyamoto K., Howell R.T., Zizi M. Online privacy breaches, offline consequences: Construction and validation of the concerns with the protection of informational privacy scale. International Journal of Human-Computer Interaction. 2020;36(19):1834–1848. [Google Scholar]
- Edelson C. Physician’s Computer Company; 2018. Virtual bedside manner: Connecting with telemedicine.https://blog.pcc.com/virtual-bedside-manner-connecting-with-telemedicine Available at. [Google Scholar]
- Ferreira P.H., Ferreira M.L., Maher C.G., Refshauge K.M., Latimer J., Adams R.D. The therapeutic alliance between clinicians and patients predicts outcome in chronic low back pain. Physical Therapy. 2013;93(4):470–478. doi: 10.2522/ptj.20120137. [DOI] [PubMed] [Google Scholar]
- Fuentes J., Armijo-Olivo S., Funabashi M., Miciak M., Dick B., Warren S., et al. Enhanced therapeutic alliance modulates pain intensity and muscle pain sensitivity in patients with chronic low back pain: An experimental controlled study. Physical Therapy. 2014;94(4):477–489. doi: 10.2522/ptj.20130118. [DOI] [PubMed] [Google Scholar]
- Groth M. Customers as good soldiers: Examining citizenship behaviors in internet service deliveries. Journal of Management. 2005;31(1):7–27. [Google Scholar]
- Ha H., John J., John J.D., Chung Y. Temporal effects of information from social networks on online behavior: The role of cognitive and affective trust. Internet Research. 2016;26(1):213–235. [Google Scholar]
- Hannah D., Zatzick C., Kietzmann J. Turbulent times demand dynamic rules. Sloan Management Review. 2021;62(4):60–65. [Google Scholar]
- Harpaz J. Forbes; 2020, May 4. 5 reasons why telehealth is here to stay (COVID-19 and beyond)https://www.forbes.com/sites/joeharpaz/2020/05/04/5-reasons-why-telehealth-here-to-stay-covid19/?sh=7b1d80b653fb Available at. [Google Scholar]
- Isaacs D., Priesz A. COVID-19 and the metaphor of war. Journal of Paediatrics and Child Health. 2021;57(1):6–8. doi: 10.1111/jpc.15164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson D., Grayson K. Cognitive and affective trust in service relationships. Journal of Business Research. 2005;58(4):500–507. [Google Scholar]
- Kakihara M., Sørensen C. Practising mobile professional work: Tales of locational, operational, and interactional mobility. Info. 2004;6(3):180–187. [Google Scholar]
- Kietzmann J. Interactive innovation of technology for mobile work. European Journal of Information Systems. 2008;17(3):305–320. [Google Scholar]
- Kirk C.P., Rifkin L.S. I’ll trade you diamonds for toilet paper: Consumer reacting, coping, and adapting behaviors in the COVID-19 pandemic. Journal of Business Research. 2020;117:124–131. doi: 10.1016/j.jbusres.2020.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konttila J., Siira H., Kyngäs H., Lahtinen M., Elo S., Kääriäinen M., et al. Healthcare professionals’ competence in digitalisation: A systematic review. Journal of Clinical Nursing. 2019;28(5/6):745–761. doi: 10.1111/jocn.14710. [DOI] [PubMed] [Google Scholar]
- LaGrandeur K., Hughes J.J. Palgrave Macmillan; London, UK: 2017. Surviving the machine age: Intelligent technology and the transformation of human work. [Google Scholar]
- Leibovici F., Santacreu A.M., Famiglietti M. Federal Reserve Bank of St. Louis; St. Louis, MO: 2020. Social distancing and contact-intensive occupations. [Google Scholar]
- Lerman D.C., O’Brien M.J., Neely L., Call N.A., Tsami L., Schieltz K.M., et al. Remote coaching of caregivers via telehealth: Challenges and potential solutions. Journal of Behavioral Education. 2020;29(2):195–221. doi: 10.1007/s10864-020-09378-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung D., Ma J. Antecedents and consequences of consumers’ trust in hybrid travel websites. Journal of Travel and Tourism Marketing. 2020;37(6):756–772. [Google Scholar]
- Lewis J.D., Weigert A.J. The social dynamics of trust: Theoretical and empirical research, 1985–2012. Social Forces. 2012;91(1):25–31. [Google Scholar]
- Lingely-Pottie P., McGrath P.J. A therapeutic alliance can exist without face-to-face contact. Journal of Telemedicine and Telecare. 2006;12(8):396–399. doi: 10.1258/135763306779378690. [DOI] [PubMed] [Google Scholar]
- Ljungberg F., Sørensen C. In: Planet internet. Braa K., editor. Studentlitteratur; Lund, Sweden: 2000. Overload: From transaction to interaction; pp. 113–136. [Google Scholar]
- Loeffler B., Church B.T. Wiley; Hoboken, NJ: 2015. The experience: The 5 principles of Disney service and relationship excellence. [Google Scholar]
- Mani S., Sharma S., Omar B., Paungmali A., Joseph L. Validity and reliability of internet-based physiotherapy assessment for musculoskeletal disorders: A systematic review. Journal of Telemedicine and Telecare. 2017;23(3):379–391. doi: 10.1177/1357633X16642369. [DOI] [PubMed] [Google Scholar]
- McColl-Kennedy J., Cheung L. In: The Sage handbook of service-dominant logic. Vargo S.L., Lusch R.F., editors. Sage; Thousand Oaks, CA: 2018. Value cocreation: Conceptualizations, origins, and developments; pp. 63–79. [Google Scholar]
- McLaughlin H. What’s in a name: ‘Client’, ‘patient’, ‘customer’, ‘consumer’, ‘expert by experience’, ‘service user’—What’s next? British Journal of Social Work. 2009;39(6):1101–1117. [Google Scholar]
- Miller E.A. Solving the disjuncture between research and practice: Telehealth trends in the 21st century. Health Policy. 2007;82(2):133–141. doi: 10.1016/j.healthpol.2006.09.011. [DOI] [PubMed] [Google Scholar]
- Mills A.J., Watson R.T., Pitt L., Kietzmann J. Wearing safe: Physical and informational security in the age of the wearable device. Business Horizons. 2016;59(6):615–622. [Google Scholar]
- NIH . National Institutes of Health; Washington, DC: 2020. NIH delivering new COVID-19 testing technologies to meet U.S. demand. [Google Scholar]
- Ostrom A.L., Bitner M.J., Brown S.W., Burkhard K.A., Goul M., Smith-Daniels V., et al. Moving forward and making a difference: Research priorities for the science of service. Journal of Service Research. 2010;13(1):4–36. [Google Scholar]
- Ozanne E.M., Noseworthy P.A., Cameron K.A., Schmidt M., Cavanaugh K., Pershing M., et al. Shared decision making in the era of telehealth: Implications for practice and research. MDM Policy and Practice. 2020;5(2):1–4. doi: 10.1177/2381468320976364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papacharissi Z. Polity; Cambridge, UK: 2010. A private sphere: Democracy in a digital age. [Google Scholar]
- Pinto R.Z., Ferreira M.L., Oliveira V.C., Franco M.R., Adams R., Maher C.G., et al. Patient-centred communication is associated with positive therapeutic alliance: A systematic review. Journal of Physiotherapy. 2012;58(2):77–87. doi: 10.1016/S1836-9553(12)70087-5. [DOI] [PubMed] [Google Scholar]
- Plangger K., Kietzmann J.H., Pitt L.F., Berthon P., Hannah D. Nomen est omen: Formalizing customer labeling theory. AMS Review. 2013;3(4):193–204. [Google Scholar]
- Punyatoya P. Effects of cognitive and affective trust on online customer behavior. Marketing Intelligence and Planning. 2019;37(1):80–96. [Google Scholar]
- Raju S., Rajagopal P., Murdock M.R. The moderating effects of prior trust on consumer responses to firm failures. Journal of Business Research. 2021;122:24–37. [Google Scholar]
- Rethorn Z.D., Lee A.C., Rethorn T.J. Connecting at the webside: Rapid telehealth implementation for musculoskeletal clinicians. Journal of Orthopaedic and Sports Physical Therapy. 2021;51(1):8–11. doi: 10.2519/jospt.2021.9902. [DOI] [PubMed] [Google Scholar]
- Russell T.G. Physical rehabilitation using telemedicine. Journal of Telemedicine and Telecare. 2007;13(5):217–220. doi: 10.1258/135763307781458886. [DOI] [PubMed] [Google Scholar]
- Rutter K., Deetjen U., Biesdorf S., Green M. McKinsey & Company; New York, NY: 2020. Living offline and online: The future of hybrid care pathways. [Google Scholar]
- Satell G. Forbes; 2015, March 14. 4 innovation lessons from the history of warfare.https://www.forbes.com/sites/gregsatell/2015/03/14/4-innovation-lessons-from-the-history-of-warfare/?sh=4f63bbc473f3 Available at. [Google Scholar]
- Shepardson D. Reuters; 2020, April 14. GM begins production of ventilators for U.S. government.https://www.reuters.com/article/us-health-coronavirus-gm/gm-begins-mass-production-of-ventilators-for-u-s-government-idUSKCN21W2OK Available at. [Google Scholar]
- Sheth J.N., Uslay C. Implications of the revised definition of marketing: From exchange to value creation. Journal of Public Policy and Marketing. 2007;26(2):302–307. [Google Scholar]
- Simpson S., Richardson L., Pietrabissa G., Castelnuovo G., Reid C. Videotherapy and therapeutic alliance in the age of COVID-19. Clinical Psychology and Psychotherapy. 2021;28(2):409–421. doi: 10.1002/cpp.2521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith A.C., Thomas E., Snoswell C.L., Haydon H., Mehrotra A., Clemensen J., et al. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19) Journal of Telemedicine and Telecare. 2020;26(5):309–313. doi: 10.1177/1357633X20916567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wosik J., Fudim M., Cameron B., Gellad Z.F., Cho A., Phinney D., et al. Telehealth transformation: COVID-19 and the rise of virtual care. Journal of the American Medical Informatics Association. 2020;27(6):957–962. doi: 10.1093/jamia/ocaa067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoffie D.B. Competing in the age of digital convergence. California Management Review. 1996;38(4):31–53. [Google Scholar]