Abstract
Purpose
To determine the integrity of re-attachment in a macula-off detachment repaired with pars plana vitrectomy using perfluorocarbon liquid (PFO) assisted drainage and short-term tamponade with no air-fluid exchange and to discuss a unifying theory on the etiology of retinal malappositions including retinal displacement (stretch), retinal slippage and full-thickness macular folds.
Observations
Significant retinal displacement was observed on fundus autofluorescence imaging following retinal detachment repair using PFO, along with significant metamorphopsia and aniseikonia. The retinal displacement was in the exact direction as the flow of subretinal fluid during the PFO assisted drainage.
Conclusions and importance
Routine use of PFO to assist with drainage and leaving it in as a short-term tamponade for uncomplicated retinal detachment repair may result in inadvertent retinal displacement as a result of the forced flow of subretinal fluid leading to a stretch of the retina. This case supports a unifying theory on the etiology of retinal malappositions including retinal displacement (stretch), retinal slippage and full thickness macular fold. Retinal malappositions occur because of the flow of subretinal fluid either a) induced by the buoyant force of the tamponade and gravity in a direction related to post-operative head position (often towards inferior periphery) in the case of retinal displacement (stretch) or b) from anterior to posterior during air-fluid exchange in the case of full-thickness macular fold with posterior redundancy and anterior stretch or slippage.
Keywords: Retinal displacement, Retinal slippage, Macular fold, Perfluorocarbon liquid
1. Introduction
Anatomic integrity of retinal re-attachment may influence functional outcomes. The occurrence of retinal displacement following rhegmatogenous retinal detachment (RRD) repair with pars plana vitrectomy (PPV) was hypothesized by the presence of retinal vessel printings (RVPs) on fundus autofluorescence (FAF) imaging.1,2 The optimal surgical technique to avoid retinal displacement and achieve a high integrity retinal attachment (HIRA), defined as the absence of RVPs on FAF, remains unknown. A recent study has demonstrated that HIRA is much more likely following successful pneumatic retinopexy (PnR) compared to PPV.3 Some have suggested that intraoperative use of perfluorocarbon liquid (PFO) in PPV may be beneficial and help reduce the occurrence of a low integrity retinal attachment (LIRA), defined as the presence of RVPs on FAF imaging, although the data and results are conflicting and controversial, and more study is required.1,2,4,5 PFO has also been shown to be efficacious as a short-term vitreous substitute in retinal detachment repair.6
We describe the autofluorescence findings following PFO assisted drainage and short-term tamponade with supine positioning for a macula-off RRD repaired with PPV, in an attempt to minimize post-operative retinal displacement. Insights gained form this case also support a potential unifying theory on the etiology of retinal malappositions, which include retinal slippage, full thickness macular folds and retinal displacement.
2. Case report and surgical technique
A 61-year-old pseudophakic male who had PnR 7 days prior for a macula-off RRD presented with counting fingers vision and a total RRD with temporal and inferior retinal breaks and no proliferative vitreoretinopathy. The PnR was initially working well with closure of a superior temporal break but then failed because of a retinal break inferior temporal that was not clearly discernible on presentation. After obtaining informed consent, he underwent a 23-gauge PPV including core and 360° peripheral vitrectomy. Subretinal fluid (SRF) drainage was assisted using PFO that was very slowly injected over approximately 2 minutes into the vitreous cavity until a complete fill was obtained. While PFO was injected, it was noted that SRF was displaced inferiorly and temporally before exiting through the retinal breaks. 360° laser retinopexy was performed with no air-fluid exchange. 23-gauge cannulas were removed and all sclerotomies were sutured. The patient was kept in the supine position for one week. Video 1 shows the slow injection of PFO and drainage of subretinal fluid inferiorly and temporally, followed by laser retinopexy and closure of wounds with no air-fluid exchange.
Supplementary video related to this article can be found at https://doi.org/10.1016/j.ajoc.2022.101337
The following is the supplementary data related to this article:
At the 7th post-operative day, the retina was attached under PFO and FAF imaging showed multiple RVPs suggesting significant retinal displacement (see reference for images).7 PFO removal and air-fluid exchange was performed on the following day, as planned. The retina remained attached and no new retinal breaks were noted. 20% SF6 was then injected.
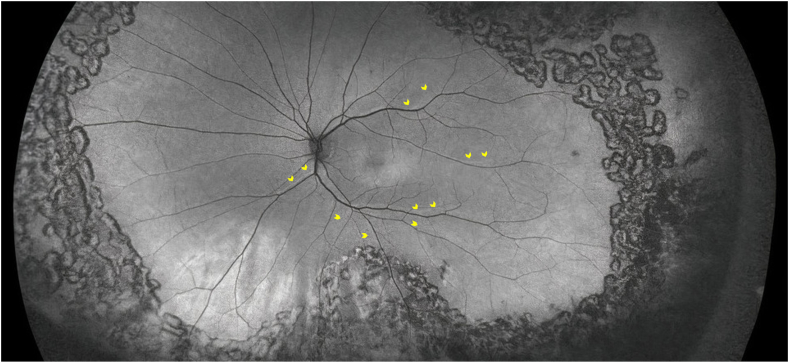
One month following PFO removal, Snellen best-corrected visual acuity was 20/30. The patient complained of significant distortion, and vertical and horizontal metamorphopsia scores were 0.6 and 0.5, respectively, as assessed using the M-chart (M-CHARTS™, Inami & Co,Ltd, 135 Japan). Aniseikonia test (Awaya New Aniseikonia Tests, Handaya Co Ltd, 136 Tokyo, Japan) demonstrated an aniseikonia score of 2. Optos Wide-field FAF (Optos Inc., Malborough, MA, USA) was repeated and confirmed the presence of unchanged RVPs at 1 month (Fig. 1).
Fig. 1.
Wide-field autofluorescence imaging at postoperative month 1 with yellow arrowheads indicating the direction of retinal displacement/stretch inferior and temporally in the same direction as the induced flow of subretinal fluid by the perfluorocarbon liquid. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
3. Discussion
PFO has been a valuable intraoperative adjunct to PPV for the management of complex RRD for the past several decades.8 If PFO reduces the occurrence of post-operative retinal displacement following PPV, then its routine use may be justified.
A combination of multiple surgical factors, including amount of residual SRF at the end of surgery, the buoyant force of the intraocular gas tamponade applied to the retina, the movement of the subretinal fluid post-operatively or intra-operatively, and post-operative positioning, play a role in the occurrence of retinal displacement.3 The small amount of residual SRF that remains at the completion of surgery along with the use of an intraocular gas tamponade likely result in a displacement of fluid under the influence of the buoyant force of the gas bubble and gravity in a direction related to post-operative positioning. It has been hypothesized that this movement of subretinal fluid under the thin and elastic retina leads to a stretch of the retina and LIRA, which is often in the inferior direction related to the direction of fluid flow.
At the outset of this case, we hypothesized that by using PFO to assist with subretinal fluid drainage and as a short term tamponade, while avoiding the air-fluid exchange and gas tamponade we may potentially minimize retinal displacement as there would be relatively little fluid under the retina at the end of surgery, and the large buoyant force of a full gas fill would be avoided. Paradoxically, our patient experienced very prominent and severe retinal displacement mainly downward and temporal. The direction of retinal displacement in this case is particularly instructive because it is in the exact direction in which subretinal fluid was expressed from the retinal breaks, specifically from posterior to anterior in the inferior and temporal direction. This supports the theory that in standard vitrectomy, displacement of subretinal fluid under the thin elastic retina induced by the buoyant force of the tamponade and gravity in a direction related to head position (often towards inferior periphery) leads to a stretch of the retina (often visualized more posteriorly) and retinal displacement or LIRA (see Animation Video 2 demonstrating PFO causing displacement of subretinal fluid from posterior to anterior which results in a corresponding stretch of the retina in the same direction). This contrasts with full thickness macular folds or slippage in which residual subretinal fluid is displaced intra-operatively during air-fluid exchange from anterior to posterior. In full thickness macular folds because the retina is tethered at the ora serrata, it leads to stretch of the retina anteriorly and folds/redundancy/compression posteriorly. In retinal slippage, often in the context of giant retinal tears, the lack of anterior anchoring of the retina eliminates the possibility of anterior stretch and is characterized only with posterior folds/redundancy/compression (see Animation Video 3 demonstrating slippage or full-thickness macular fold which occurs as a result of subretinal fluid being displaced from anterior to posterior intraoperatively during air-fluid exchange). In other words, retinal displacement and full-thickness macular folds share a common pathophysiology relating to the induced flow of subretinal fluid. What varies is the direction of that flow, the time when it occurs during or after the surgery and the resulting anatomic abnormality that is visualized posteriorly (displacement/stretch vs folds/redundancy).
Supplementary video related to this article can be found at https://doi.org/10.1016/j.ajoc.2022.101337
The following are the supplementary data related to this article:
Retinal displacement remains a significant issue following PPV for RRD and has been associated with worse functional outcomes.3,9 Recent studies have demonstrated that retinal displacement can be minimized with the use of PnR3 and if performing vitrectomy, with immediate face down positioning at the completion of surgery.10 Archimedes principle determines that the maximum buoyant force at the apex of a bubble varies linearly with the bubble height11 with a larger force applied to the retina with a full gas fill compared to a much smaller force from a small expansile gas bubble injection and therefore it is also likely that using a smaller gas fill or the injection of a small expansile gas bubble in certain appropriate cases of PPV for RRD could reduce the risk of retinal displacement.12,13 The current literature is uncertain regarding the impact of intraoperative PFO assisted drainage of subretinal fluid on retinal displacement, and a properly designed randomized trial is required. This case demonstrates that PFO used to assist with subretinal fluid drainage and simultaneously as a short-term tamponade may be harmful and increase the risk of post-operative retinal displacement, and in the authors' opinion should be used with caution or avoided in routine primary RRD repair. Whether there would have been less displacement, had the PFO been removed immediately following the subretinal fluid drainage is unknown, but is certainly likely. However, in this circumstance, there likely would have been some residual subretinal fluid left at the end of surgery, and with a large gas tamponade, the patient would have had the usual risks of retinal displacement following PPV that have been demonstrated in the literature.
4. Conclusion
This case has helped to inform the discussion regarding the etiology of retinal displacement/stretch and other types of retinal malappositions such as full thickness macular folds and retinal slippage following retinal detachment repair. Recognizing the importance and etiology of retinal malappositions such as retinal displacement (stretch) may lead to modifications in vitreoretinal surgical techniques to minimize these complications and improve functional outcomes.
Patient consent
The patient consented to publication of the case in writing. This report does not contain any personal information that could lead to the identification of the patient.
Disclosures
No funding or grant support
Authorship
All authors attest that they meet the current ICMJE criteria for authorship.
Declaration of competing interest
Dr. Rajeev H. Muni is a consultant and has participated in advisory boards and receives research funding from Novartis, Bayer, Allergan and Roche, none of which are relevant to this study. The following authors have no financial disclosures: SBM, VRJ.
Acknowledgements
None.
References
- 1.Dell'Omo R., Mura M., Lesnik Oberstein S.Y., Bijl H., Tan H.S. Early simultaneous fundus autofluorescence and optical coherence tomography features after pars plana vitrectomy for primary rhegmatogenous retinal detachment. Retina. 2012;32(4):719–728. doi: 10.1097/IAE.0b013e31822c293e. [DOI] [PubMed] [Google Scholar]
- 2.Shiragami C., Shiraga F., Yamaji H., et al. Unintentional displacement of the retina after standard vitrectomy for rhegmatogenous retinal detachment. Ophthalmology. 2010;117(1):86–92. doi: 10.1016/j.ophtha.2009.06.025. e1. [DOI] [PubMed] [Google Scholar]
- 3.Brosh K., Francisconi C.L.M., Qian J., et al. Retinal displacement following pneumatic retinopexy vs pars plana vitrectomy for rhegmatogenous retinal detachment. JAMA Ophthalmol. 2020;138(6):652. doi: 10.1001/jamaophthalmol.2020.1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guber J., Schawkat M., Lang C., Scholl H.P.N., Valmaggia C. How to prevent retinal shift after rhegmatogenous retinal detachment repair. Ophthalmol Retin. 2019;3(5):417–421. doi: 10.1016/j.oret.2019.01.010. [DOI] [PubMed] [Google Scholar]
- 5.Muni R.H., Figueiredo N., Hillier R.J. Re: guber et al: how to Prevent Retinal Shift after Rhegmatogenous Retinal Detachment Repair. Ophthalmol Retin. 2020;4:7e6. doi: 10.1016/j.oret.2020.02.004. [DOI] [PubMed] [Google Scholar]
- 6.Rush R., Sheth S., Surka S., Ho I., Gregory-Roberts J. Postoperative perfluoro-n-octane tamponade for primary retinal detachment repair. Retina. 2012;32(6):1114–1120. doi: 10.1097/IAE.0b013e31822f56f6. [DOI] [PubMed] [Google Scholar]
- 7.Marafon S.B., Juncal V.R., Muni R.H. Retinal shift with perfluorocarbon liquid without air-fluid exchange. Ophthalmology. 2020;127(5):598. doi: 10.1016/j.ophtha.2020.01.053. [DOI] [PubMed] [Google Scholar]
- 8.Scott I.U., Murray T.G., Flynn H.W., Feuer W.J., Schiffman J.C. Outcomes and complications associated with giant retinal tear management using perfluoro-n-octane. Ophthalmology. 2002;109(10):1828–1833. doi: 10.1016/s0161-6420(02)01184-3. [DOI] [PubMed] [Google Scholar]
- 9.Lee E., Williamson T.H., Hysi P., et al. Macular displacement following rhegmatogenous retinal detachment repair. Br J Ophthalmol. 2013;97(10):1297–1302. doi: 10.1136/bjophthalmol-2013-303637. [DOI] [PubMed] [Google Scholar]
- 10.Casswell E.J., Yorston D., Lee E., et al. Effect of face-down positioning vs support-the-break positioning after macula-involving retinal detachment repair. JAMA Ophthalmol. 2020:1–9. doi: 10.1001/jamaophthalmol.2020.0997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Berger J.W., Brucker A.J. The magnitude of the bubble buoyant pressure: implications for macular hole surgery. Retina. 1998;18(1):84–86. doi: 10.1097/00006982-199801000-00020. [DOI] [PubMed] [Google Scholar]
- 12.Muni R.H., Felfeli T., Figueiredo N., Marafon S.B., Escaf L.S., Juncal V.R. Minimal gas vitrectomy technique for reducing risk of retinal displacement following rhegmatogenous retinal detachment repair. Retin Cases Brief Rep. 2020 Nov 6 doi: 10.1097/ICB.0000000000001076. [DOI] [PubMed] [Google Scholar]
- 13.Muni R.H., Bansal A., Lee W.W., Escaf L.C. Minimal gas vitrectomy with scleral buckle to minimize retinal displacement in rhegmatogenous retinal detachment with inferior breaks. Retin Cases Brief Rep. 2021 Jun 14 doi: 10.1097/ICB.0000000000001174. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.