Abstract
Introduction
The coronavirus disease 2019 pandemic has profoundly impacted surgical education. We assessed resident perceptions of our virtual academic program, which consists of daily lectures or case conferences held via a videoconferencing platform.
Methods
A survey evaluating attitudes and practices for virtual academics was administered to general surgery residents. A focus group was conducted to identify benefits, barriers to engagement, and opportunities for improvement for virtual education. A total of 19 residents completed the education survey, and seven residents participated in the focus group.
Results
While expressing preference toward in-person academics (84.2%), residents felt the virtual academics were of good quality (median rating 4/5) and preferred virtual academics to no academic sessions (94.7%). Of respondents, 57.9% believe that the coronavirus pandemic negatively impacted their surgical education. They believe their American Board of Surgery In-Training Examination preparation was not impacted. Residents preferred using a computer over a phone for academics (79% versus 16%). The focus group identified the benefits of virtual academics, including the ability to participate while away and having recordings available. Areas for improvement included reinforcement of protected time for academics, requiring cameras be on, increasing in-lecture polls, and creation of an online repository of recordings for review. Residents hoped a virtual component of academics and recordings would continue past the pandemic.
Conclusions
Although virtual academics are not the preferred mode of learning in our residency, there are multiple unintended benefits. We recommend a hybrid academic model with in-person didactics and recorded video for later review.
Keywords: COVID-19, Pandemic, Virtual education, Hybrid education
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has forced dramatic changes in daily life of people across the world, compelling much of education to transition to virtual options. Graduate medical education was no exception to this rule, forced from face-to-face into synchronous online platforms. The COVID-19 Delta variant again affected hospital operations that may have been returning to normal in the mid-summer of 2021, forshadowing that virtual programming would remain for the foreseeable future.1
Changes to surgical team structure and didactics in response to the pandemic have been well described, as has the impact of the pandemic on resident wellness and perceived clinical experience during this time frame.2, 3, 4, 5, 6, 7 Many programs converted meetings to teleconferences and/or webinars for morning report, Morbidity & Mortality conference (M & M), and journal club, among others.8 Our institution was one of the first to describe a strategic plan for continued surgical resident education in response to the pandemic, including videoconferencing, social media for daily American Board of Surgery In-Training Examination (ABSITE) review, and faculty-guided surgical videos as a surrogate for learning in the operating room.2 Other institutions have described their adjustment, such as a lecture series at Virginia Commonwealth University that garnered participation from more than 50 surgery resident programs until its conclusion in spring 2020.9
Many studies have made general or anecdotal commentary on e-learning, but few have assessed resident response to the change to a virtual educational platform to determine strengths or weaknesses.7 Here, we present a mixed model assessment of virtual academic practices at our institution. Our goal was to identify the strengths of virtual learning for improvement of existing programming and eventual integration into face-to-face resident education.
Material and Methods
This study was exempt from institutional review board approval. Our institution has a weekly 3-h period of protected academic time encompassing M & M, as well as a 30-min patient care conference every weekday for resident-focused learning. Before the pandemic, this was conducted in person but shifted to a virtual format in March 2020. Synchronous virtual academics were hosted initially using GoToMeeting (LogMeIn Inc, Boston, MA) and then transitioned to Zoom (Zoom Video Communications, San Jose, CA). Residents logged in on the device of their choice from wherever they were assigned that day, which could include their clinical site or home depending on rotation schedules, which were restructured in response to the pandemic. All sessions were recorded, and recordings were then gathered into a repository available to all residents for asynchronous education.
An anonymous 24-question survey assessing attitudes and practices for virtual academics was sent to all members of our general surgery residency in October of 2020 (Supplementary Table 1). Completion of the survey implied consent, which was explicitly stated. Residents were reminded weekly for one month to complete the survey, after which the survey closed. In addition, residents from our program were invited to participate in a focus group conducted during the same month to identify benefits of virtual education, barriers to engagement, and opportunities for improvement. All volunteers were included. A resident and faculty study moderator facilitated the group by asking a series of open-ended questions (Table 1 ). Notes and the discussion recording were reviewed to identify themes.
Table 1.
Virtual learning focus group questions.
| 1. What are some unforeseen benefits of virtual academics? |
| 2. What are the shortcomings of virtual academics? |
| 3. How can we improve engagement in virtual academics? |
| 4. How can we improve attendance for virtual academics? |
| 5. What other ways do you think we could improve quality of virtual academics? |
| 8. Do you think the transition to virtual academics will impact your ABSITE score? |
| 9. How has the COVID-19 pandemic impacted your surgical education, both positively and negatively? |
| 10. Are there any elements of virtual academics you would want to keep after transitioning back to in-person academics? |
Results
Nineteen of 30 residents (63%) completed the survey. Seven residents participated in the focus group discussion. Each postgraduate year (PGY) cohort was represented in both formats.
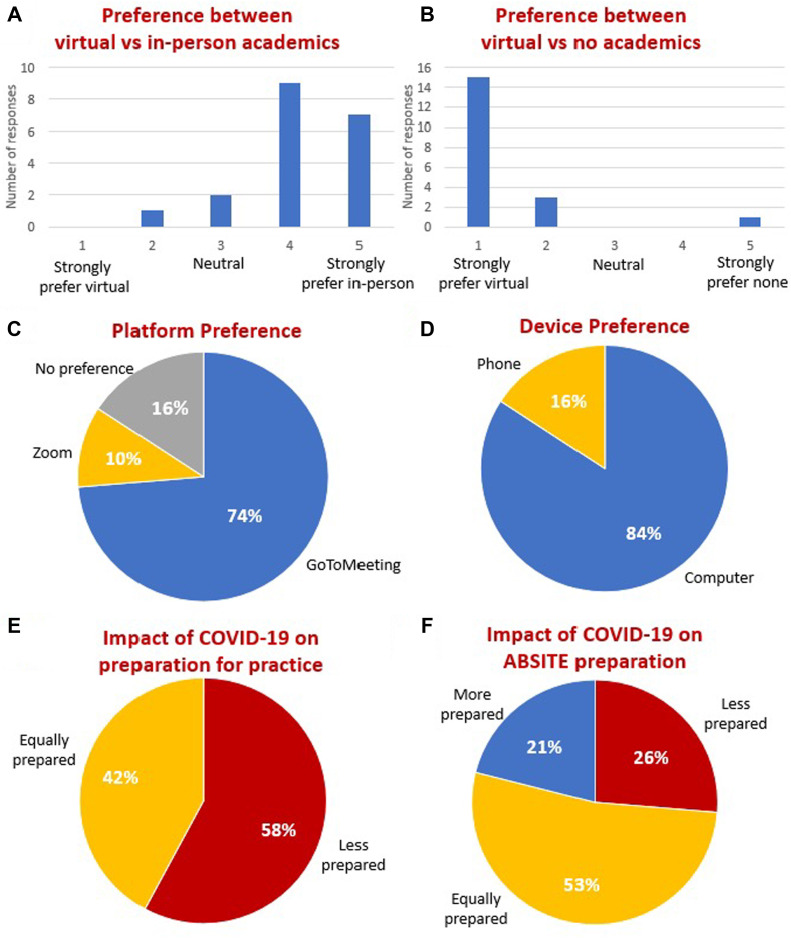
While expressing preference toward in-person academics (84.2% preferred or strongly preferred), residents felt the virtual academics were of good quality (median 4/5, IQR 1) and preferred virtual academics to no academics (94.7%). Of respondents, 57.9% believed that COVID-19 negatively impacted their surgical education, and 58% reported feeling less prepared to be a practicing surgeon, which was answered similarly by junior (PGY 1-3) and senior (PGY 4-6) residents. Most reported ABSITE preparation was not impacted (53%), whereas a minority reported being more prepared (21%) or less prepared (26%). Residents preferred using a computer to log in over a phone (79% versus 16%) for better viewing of slide details, such as tables/graphs but reported using a phone more frequently for convenience. Most residents reported a preference for our program's original platform used for virtual academics, GoToMeeting (74%), whereas fewer preferred Zoom (10%) or had no preference (16%). Results are reported below (Figure).
Fig.
Summary of the survey results. (A) Participant preference for virtual versus in-person academics. (B) Participant preference for virtual versus no academics. (C) Participant preference for virtual programming platform. (D) Participant preference for device used for logging in to virtual academics. (E) Participant response to the impact of COVID-19 and preparation for practice. (F) Participant response to the impact of COVID-19 and ABSITE preparation.
Participants reported several limitations to engagement. These included perceived loss of protected time during academics and multiple distractions. Focus group ideas to address these included reinforcing protected time for academics, requiring cameras be on, increasing use of in-presentation polling, reliable recording of lectures, and creating a repository of recordings for later review. The focus group identified benefits to the virtual format, including the ability for residents to participate while off-site, whether on away rotations or during research year(s). Most participants appreciated the recorded didactics available for independent study. They additionally liked the chat functions of the virtual platform, which they reported lowered the barrier to asking presenters questions. Residents expressed continued support of hybrid options. These recommendations are summarized in Table 2 .
Table 2.
Best practices for virtual learning in graduate medical education.
| 1. Maintain dedicated, protected time for residents. Reinforce this at the start of every didactic session. |
| 2. Emphasize not multitasking during academics. |
| 3. Use computer preferentially for logging in. |
| 4. Require all participants turn on his/her camera. |
| 5. Utilize interactive learning techniques whenever possible. |
| 6. Record all virtual sessions and post to platform of choice for later review or study. |
| 7. Continue virtual (hybrid) options, even when in-person is available. |
Discussion
Our results indicate that residents believe COVID-19 has negatively impacted their education. Although virtual learning is clearly not the preferred modality for academics, remote academics were preferred over no academics at all. Focus groups revealed multiple limitations, but residents appreciated the synchronous and asynchronous accessibility. Residents expressed interest in a hybrid format to continue beyond the pandemic.
When the COVID-19 pandemic made in-person academic activities impractical in the spring of 2020, our group quickly pivoted to the use of technology to compensate for these losses.2 In line with other studies of trainee preferences, our residents showed a clear preference for in-person education, stating decreased attention with an online format.10 Our data do, however, indicate success with virtual lectures, which our trainees believed to be of good quality. The majority of our residents (74%) asserted that ABSITE preparedness was not diminished from prior years, which is corroborated by no meaningful difference in our program's ABSITE scores from 2019 (median 80), 2020 (median 78), and 2021 (median 80). While the virtual format is not ideal, it also offers the chance to learn from and collaborate with multiple institutions and disciplines.9 , 11
A surrogate for learning in the operating room is far more challenging. Our institution created didactic sessions focused on operative technique, in which a faculty member would talk through critical or challenging portions of cases using surgical videos. These videos are now widely available as technology needed for recording and editing has improved and become more accessible. Simulation was difficult, given social distancing regulations and requirements to minimize the time in the hospital, where our simulation laboratory is located. Resident feelings of lack of preparedness for clinical practice are consistent with prior reports, although interestingly, there was no difference in survey response between junior or senior residents who may be impacted differently by reduced case volume.7 , 12 As we struggle to return to a normal case volume secondary to institutional limits that is also reflected on a national scale, we believe that utilization of faculty-led operative video review can augment the learning of operative techniques.13 In addition, in times when another COVID-19 variant or virus may manifest, this tactic offers a reasonable alternative if case volumes decrease.
Virtual learning has many challenges, multiple of which were identified in our focus group. Our residents perceived a loss of protected time for academics and cited multiple distractions. Residents in our program largely participate in virtual academics at their desks, which incites the temptation to multitask. Learners may engage in nearly twice as many nonconference-related activities (e.g., email) per hour during online conference.4 , 10 Potential means of mitigating these factors include requirements for cameras to remain on for visual facial feedback and accountability. Intermittent polling and questions increase engagement. Other studies have suggested “gamification” of lectures with a gameshow format to maintain attention.10 While our residents reported a preference for GoToMeeting over Zoom in their responses, the authors feel this is likely because of the relatively recent transition during the time of the survey and lack of comfort with a new platform. Zoom offers a variety of unique opportunities for in-presentation polling and participant interaction which program leadership believed would be beneficial to lectures, particularly the ability to have in-platform quizzes. Participants had an improved experience when using computers over phones, which may minimize additional distractions such as text alerts, and allow better visualization of slide material.14 , 15 Finally, required and tracked attendance has been suggested.4 Using these methods, our program has anecdotally seen improved engagement since the current study was completed.
An additional benefit to virtual programming is recordings of lectures. Our institution created a lecture share drive and YouTube (YouTube LLC, Mountainview, CA) channel (“Surgery Time”) for easy access. Virtual access to academics allows residents away from our home institution to continue to participate. We plan to continue in a hybrid format on our private Zoom account so all residents can log in even after a return to face-to-face academics, with a video repository so that residents have asynchronous resources available. Given the relative ease of this addition and positive response of residents, we highly recommend that all programs adopt this practice.
This study has multiple limitations. The focus group was moderated by a general surgery resident and staff member, which may have biased residents' responses. Responses were not correlated to conference attendance, which may also have impacted perceptions. The study was limited by sample size, and participants were from a single institution, limiting generalizability to other academic programs. However, the very nature of a focused single-institution survey allowed for acquisition of granular detail about the advantages and disadvantages of virtual academics that facilitated an in-depth understanding of our residents’ preferences. In addition, the study is a worthwhile first step to understand unrecognized advantages to virtual learning that can be either maintained in the current status quo or used in a hybrid format when returning to traditional face-to-face didactics.
In conclusion, we report results of a resident survey and dedicated focus group investigating the impact of COVID-19 on resident perceptions of their education and preparedness for practice, as well as successes and limitations of a virtual platform. With the rise of new COVID-19 variants and the possibility of future outbreaks, we must recognize that virtual programming is an essential aspect of surgery resident education that is likely to endure. We propose the implementation of lessons learned since mid-2020 to improve existing didactics and augment future learning in a hybrid format.
Author Contributions
A.M.A., G.T.C., and T.J.V. all contributed to the design of the study. A.M.A. and T.J.V. conducted the focus group and drafted the survey. E.L.C., A.M.A., and T.J.V. primarily interpreted the results. E.L.C. and A.M.A. collaborated in drafting the article, with primary drafting and revisions from E.L.C. Remaining authors contributed substantially with editing of the article for content, clarity, and brevity; they additionally provided thoughts for inclusion of practical recommendations for virtual learning. All authors gave final approval for publication.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.jss.2022.01.020.
Disclosure
None declared.
Funding
No funding was used to conduct the above study.
Supplementary Data
References
- 1.Chia P.Y., Xiang Ong S.W., Chiew C.J., et al. Virological and serological kinetics of SARS-CoV-2 Delta variant vaccine-breakthrough infections: a multi-center cohort study. medRxiv. 2021;2007 doi: 10.1016/j.cmi.2021.11.010. 2028.21261295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chick R.C., Clifton G.T., Peace K.M., et al. Using technology to maintain the education of residents during the COVID-19 pandemic. J Surg Educ. 2020;77:729–732. doi: 10.1016/j.jsurg.2020.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kogan M., Klein S.E., Hannon C.P., Nolte M.T. Orthopaedic education during the COVID-19 pandemic. J Am Acad Orthop Surg. 2020;28:e456–e464. doi: 10.5435/JAAOS-D-20-00292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abdelsattar J.M., Coleman J.R., Nagler A., et al. Lived experiences of surgical residents during the COVID-19 pandemic: a qualitative assessment. J Surg Educ. 2021;78:1851–1862. doi: 10.1016/j.jsurg.2021.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lund S., Hinduja P., Stulak J., et al. Impact of elective case postponement secondary to COVID-19 on general surgery residents' experience: operative cases logged at three academic teaching hospitals. J Surg Educ. 2021;78:1863–1867. doi: 10.1016/j.jsurg.2021.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Collins C., Mahuron K., Bongiovanni T., et al. Stress and the surgical resident in the COVID-19 pandemic. J Surg Educ. 2021;78:422–430. doi: 10.1016/j.jsurg.2020.07.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Coleman J.R., Abdelsattar J.M., Glocker R.J. COVID-19 pandemic and the lived experience of surgical residents, fellows, and early-career surgeons in the American College of Surgeons. J Am Coll Surg. 2021;232:119–135.e120. doi: 10.1016/j.jamcollsurg.2020.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dedeilia A., Sotiropoulos M.G., Hanrahan J.G., et al. Medical and surgical education challenges and innovations in the COVID-19 era: a systematic review. In Vivo. 2020;34:1603–1611. doi: 10.21873/invivo.11950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Metchik A., Boyd S., Kons Z., et al. How we do it: implementing a virtual, multi-institutional collaborative education model for the COVID-19 pandemic and beyond. J Surg Educ. 2021;78:1041–1045. doi: 10.1016/j.jsurg.2020.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weber W., Ahn J. COVID-19 conferences: resident perceptions of online synchronous learning environments. West J Emerg Med. 2020;22:115–118. doi: 10.5811/westjem.2020.11.49125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smigelski M., Movassaghi M. Small A urology virtual education programs during the COVID-19 pandemic. Curr Urol Rep. 2020;21:50. doi: 10.1007/s11934-020-01004-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aziz H., James T., Remulla D., et al. Effect of COVID-19 on surgical training across the United States: a national survey of general surgery residents. J Surg Educ. 2021;78:431–439. doi: 10.1016/j.jsurg.2020.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.2021 Hardship modifications to general surgery training requirements. The American Board of Surgery; Philadelphia, PA: 2021. [Google Scholar]
- 14.Walsh K. Mobile learning in medical education: review. Ethiop J Health Sci. 2015;25:363–366. doi: 10.4314/ejhs.v25i4.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rozgonjuk D., Saal K., Täht K. Problematic smartphone use, deep and surface approaches to learning, and social media use in lectures. Int J Environ Res Public Health. 2018;15:92. doi: 10.3390/ijerph15010092. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.