Abstract
Background:
Lower socioeconomic position usually portends worse health outcomes, but multiple studies have found that atopic dermatitis is associated with higher socioeconomic position, but the nature of this relationship remains unclear.
Objective:
To systematically review the literature on socioeconomic position and atopic dermatitis and determine if the association varies by patient or study characteristics.
Methods:
A literature search was conducted in the PubMed and Embase databases. Individual-level studies addressing the association between all measures of socioeconomic position and the prevalence or incidence of atopic dermatitis were eligible for inclusion. Two independent reviewers screened all texts and extracted all data for qualitative synthesis.
Results:
88 studies met inclusion criteria. Overall, 42% (37/88) of studies found atopic dermatitis to be positively associated with socioeconomic position, 15% (13/88) found a negative association, and 43% (38/88) found a null or inconsistent association. Studies conducted in Europe, among children, and based on self-report of eczema were more likely to find a positive association with socioeconomic position.
Limitations:
Studies varied both in terms of measurement of socioeconomic position and definition of atopic dermatitis, limiting quantitative synthesis.
Conclusion:
There is not consistent evidence of a positive association between atopic dermatitis and socioeconomic position.
Keywords: atopic, dermatitis, eczema, socioeconomic position, socioeconomic status
Capsule summary
A number of studies and a prior systematic review reported a positive association between atopic dermatitis and socioeconomic position, but the reason for this relationship remains unclear
This updated systematic review found that a majority (58%) of studies did not find a positive association between atopic dermatitis and socioeconomic position
Introduction
Atopic dermatitis (also known as atopic eczema, or eczema) is the most common chronic inflammatory skin condition, affecting up to 15–30% of children and 10–15% of adults worldwide, conferring a significant burden of disease (1)(2)(3)(4). Lower socioeconomic position (SEP), based on estimates of income, educational attainment, occupational prestige, or subjective perceptions of social class and social status, is associated with poorer health outcomes for almost every disease studied (5). In contrast, numerous studies suggest that SEP may be positively associated with atopic dermatitis and other atopic diseases, possibly due to differences in the exposure to microorganisms important to immune system development and function (6)(7).
A 2015 systematic review examining the relationship between SEP and allergic diseases concluded that there was a positive association between SEP and atopic dermatitis, with pooled estimates for the odds ratio of disease for the lowest compared with the highest SEP of 0.72, 95% CI 0.61–0.83 (8). However, results from individual studies varied, with only ten of the nineteen studies on atopic dermatitis finding prevalence to be positively associated with SEP. The review had a broad focus on allergic disease and did not differentiate between participant characteristics or measures of SEP. These factors are important, however, because they could indicate different underlying mechanisms among different patient populations. For example, the relationship between parental educational attainment and childhood atopic dermatitis likely reflects a different set of factors than an individual’s own educational attainment and atopic dermatitis during adulthood.
Multiple studies have found that social and environmental factors are strong predictors of atopic dermatitis, even in comparison to genetic factors (9)(10). A closer inspection of the relationship between SEP and atopic dermatitis is warranted due to the wide spectrum of SEP measures and the heterogenous nature of atopic dermatitis, which varies in severity and chronicity in both children and adults (11). In addition, a re-examination of the relationship is necessitated due to increasing atopic dermatitis research in recent years, with new data highlighting increased prevalence in the adult patient population and in non-Europeans (4)(9).
Studying the relationship between SEP and atopic dermatitis is important for health policy planning and may help to elucidate a better understanding of the mechanisms driving atopic dermatitis presentation and persistence across the lifespan (5). The objective of this study was to systematically examine the published literature on the association between SEP and atopic dermatitis, and to assess whether the association differs by study characteristics, age category of participants, or the measure of SEP used.
Methods
We conducted a systematic review in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) and MOOSE (Meta-analysis Of Observational Studies in Epidemiology) recommendations (12)(13). The review protocol can be accessed at PROSPERO (www.crd.york.ac.uk/PROSPERO, reference number #161081).
Eligibility criteria
Published, full-text studies of individual-level epidemiologic design addressing the association between SEP and the prevalence or incidence of atopic dermatitis were eligible for inclusion, with no restrictions on participant age, sex, or race/ethnicity. Given the nature of the exposure (SEP), all studies were observational. Studies assessing only participants with atopic dermatitis and lacking designated comparison group were excluded. Studies of localized eczema, such as hand eczema, or studies focused on other types of dermatitis, such as seborrheic or contact dermatitis, were not eligible for inclusion.
Information sources and search strategy
We searched the literature using the PubMed and Embase databases for articles published through July 4, 2021. The search strategy was developed in collaboration with a medical librarian and included MeSH (Medical Subject Headings) terms for both SEP and atopic dermatitis. The MeSH term “Socioeconomic Factors” includes terms related to education, social class, income, and occupation, as well as terms on family characteristics, social conditions, and social change. Sample search strategies can be found in the supplemental files folder at https://data.mendeley.com/datasets/syk2bcz8jg/2.
We did not restrict the search by language or timeframe. A cross-check through the bibliography of previous reviews was completed to ensure our search strategy included all relevant studies. We used Google Translate to review non-English language texts; none met final eligibility criteria requiring data extraction.
Study selection, data extraction, and quality assessment
Titles and abstracts were screened by two co-authors (HB and MB) independently using the web-based systematic review management platform Covidence (14). Full texts of the remaining articles were also assessed for final inclusion in Covidence by two independent reviewers. All conflicts were resolved by a third co-author (KA).
Extraction of study design, publication date, sample size, study population, measure of SEP, atopic dermatitis diagnosis method, and effect estimates by socioeconomic group was completed by two independent reviewers. Any discrepancies in extracted data were discussed and resolved through group consensus with a third co-author (KA).
Synthesis methods
To synthesize the results for the association between SEP and atopic dermatitis, we categorized each study into one of four mutually exclusive categories: atopic dermatitis positively associated with SEP, atopic dermatitis negatively associated with SEP, atopic dermatitis not significantly associated with SEP, or inconclusive results on the association between SEP and atopic dermatitis. Studies categorized as inconclusive reported multiple SEP-atopic dermatitis associations, one for each method of SEP assessment, that were not consistent.
Results
A total of 519 studies met inclusion criteria after removal of duplicates, 151 passed title/abstract screening, and 88 were included after full text review (Figure 1).
Figure 1:
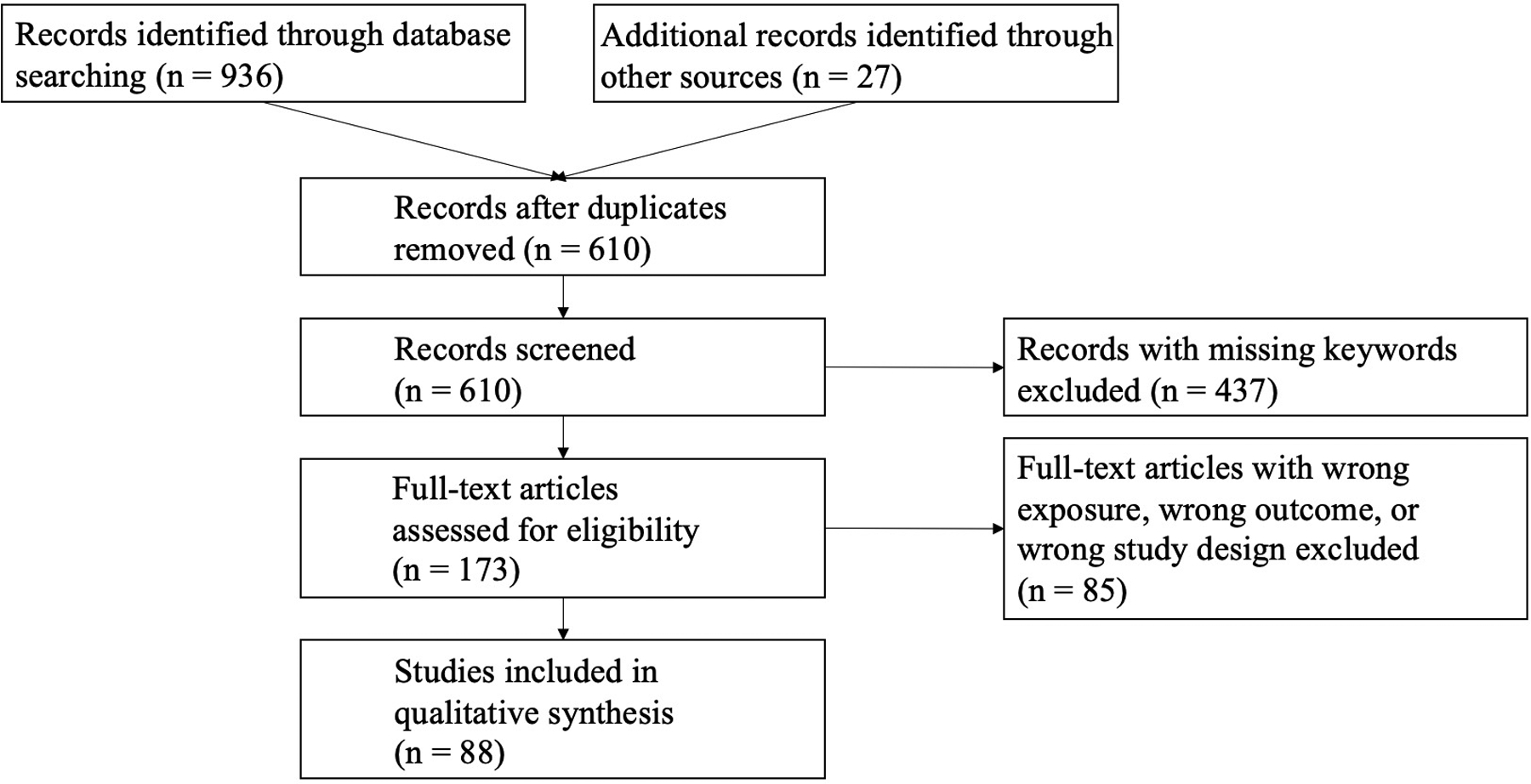
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart
Overview of included studies
The majority of included studies focused on children (78%, 68/88) (Table 1). Europe and Asia were well-represented (74%, 65/88) while the Americas, Africa and the Middle East, and Oceania were less represented. Out of 22 studies from Asia, 21 were from East Asia (China, Taiwan, Korea, Japan). Only three studies originated from Africa (Nigeria, South Africa). Most studies were relatively large in size, ranging from 105 participants to 4,000,739 participants. 29 studies had less than 2500 participants, 30 studies had between 2500 and 20000 participants, and 29 studies had more than 20000 participants.
Table 1:
Characteristics of included studies (total n = 88)
| Percent of Studies | ||
|---|---|---|
| Region | ||
| Africa and the Middle East | 12 | 14% |
| Asia | 22 | 25% |
| Europe | 43 | 49% |
| The Americas | 10 | 11% |
| Oceania | 1 | 1% |
| Study Design | ||
| Case-control | 7 | 8% |
| Cohort | 22 | 25% |
| Cross-sectional | 59 | 67% |
| Age Group | ||
| Adults | 10 | 11% |
| Both | 10 | 11% |
| Children | 68 | 78% |
| Method of Atopic Dermatitis Assessment | ||
| Exam | 9 | 10% |
| Self-report | 67 | 76% |
| Medical records | 12 | 14% |
| Study Size | ||
| n < 2500 | 29 | 33% |
| 2499 < n < 20000 | 30 | 34% |
| 19999 < n | 29 | 33% |
| Publication Date | ||
| 1975–1989 | 7 | 8% |
| 1990–1999 | 8 | 9% |
| 2000–2009 | 24 | 27% |
| 2010–2021 | 49 | 56% |
Most studies were cross-sectional in design (67%, 59/88) and utilized self-reported outcome data (76%, 67/88), predominantly based on the ISAAC (The International Study of Asthma and Allergies in Children) questionnaire (15). SEP was based on self-reported information for all studies, however some studies treated SEP as a continuous variable while others treated it as categorical. For the studies that created SEP categories, many reported binary comparisons, with fewer reporting three, four, or five categories. As shown in Table 3, the most common measures of SEP were income and education. Social class was the next most commonly used SEP proxy variable, with the majority of studies defining it as a measure of occupational skill (16). Eight studies created a composite SEP metric which varied between studies, all of which consisted of some combination of income, education, occupation, and social class. Housing characteristics, which was defined as place of residency (e.g. apartment, house, or shanty) was the least frequently used measure of SEP (n = 3 studies).
Table 3:
Evidence on the associations between SEP and atopic dermatitis by measure of SEP
| Children | ||||
|---|---|---|---|---|
| Positive Association | Negative Association | No association | Total | |
| Measure of SEP | ||||
| Class/Occupation | 6 (40%) | 1 (7%) | 8 (53%) | 15 |
| Income | 13 (33%) | 7 (18%) | 19 (49%) | 39 |
| Family Size | 1 (20%) | 2 (40%) | 2 (40%) | 5 |
| Housing Characteristics | 1 (50%) | 1 (50%) | 2 | |
| Parental* Education | 27 (61%) | 3 (7%) | 14 (32%) | 44 |
| Adults | ||||
| Positive Association | Negative Association | No association | Total | |
| Measure of SEP | ||||
| Class/Occupation | 4 (100%) | 4 | ||
| Income | 2 (23%) | 4 (44%) | 3 (33%) | 9 |
| Family Size | 1 (50%) | 1 (50%) | 2 | |
| Housing Characteristics | 1 (100%) | 1 | ||
| Participant Education | 6 (86%) | 1 (14%) | 7 | |
| Parental* Education | 1 (100%) | 1** | ||
Maternal or paternal
Study population of university students
Association between Socioeconomic Position and Atopic Dermatitis
Study conclusions were inconsistent: 42% (37/88) of studies found atopic dermatitis to be positively associated with SEP, 15% (13/88) found a negative association, and 43% (38/88) found a null or inconclusive association (Table 2). Differences were observed through comparison of studies with varying characteristics: studies of children and those based in Europe were most likely to find positive associations between SEP and atopic dermatitis, while smaller studies and studies using dedicated participant skin examinations or review of participant medical records were more likely to report no association between SEP and atopic dermatitis compared to studies that relied on patient self-reporting of atopic dermatitis.
Table 2:
SEP-atopic dermatitis associations by study characteristic
| Total | |||||
|---|---|---|---|---|---|
| 37 (42%) | 13 (15%) | 23 (26%) | 15 (17%) | 88 | |
| Region | |||||
| Africa/Middle East | 3 (25%) | 2 (17%) | 3 (25%) | 4 (33%) | 12 |
| Asia | 10 (45%) | 5 (23%) | 4 (18%) | 3 (14%) | 22 |
| Europe | 22 (51%) | 2 (5%) | 14 (32%) | 5 (12%) | 43 |
| Americas | 2 (20%) | 4 (40%) | 1 (10%) | 3 (30%) | 10 |
| Oceania | 0 | 0 | 1 (100%) | 0 | 1 |
| Study Design | |||||
| Case-Control | 3 (43%) | 1 (14%) | 2 (29%) | 1 (14%) | 7 |
| Cohort | 9 (41%) | 3 (14%) | 8 (36%) | 2 (9%) | 22 |
| Cross-Sectional | 25 (43%) | 9 (15%) | 13 (22%) | 12 (20%) | 59 |
| Age Group | |||||
| Adults | 3 (30%) | 1 (10%) | 3 (30%) | 3 (30%) | 10 |
| Both | 3 (30%) | 3 (30%) | 3 (30%) | 1 (10%) | 10 |
| Children | 31 (46%) | 9 (13%) | 17 (25%) | 11 (16%) | 68 |
| Method of Atopic Dermatitis Assessment | |||||
| Exam | 2 (22%) | 1 (11%) | 4 (45%) | 2 (22%) | 9 |
| Self-Report | 31 (46%) | 9 (14%) | 15 (22%) | 12 (18%) | 67 |
| Medical Record | 4 (33%) | 3 (25%) | 4 (33%) | 1 (9%) | 12 |
| Sample Size | |||||
| 20000+ | 14 (46%) | 6 (19%) | 3 (12%) | 6 (23%) | 29 |
| 2500–19999 | 15 (50%) | 2 (7%) | 9 (30%) | 4 (13%) | 30 |
| 105–2499 | 8 (28%) | 5 (17%) | 11 (38%) | 5 (17%) | 29 |
| Publication Date | |||||
| 1975–1989 | 3 (43%) | 0 | 0 | 4 (57%) | 7 |
| 1990–1999 | 7 (88%) | 0 | 0 | 1 (12%) | 8 |
| 2000–2009 | 11 (46%) | 2 (8%) | 4 (17%) | 7 (29%) | 24 |
| 2010–2019 | 16 (33%) | 14 (29%) | 10 (20%) | 9 (18%) | 49 |
The most commonly used measure of SEP for adult studies was income, followed by education (Table 3). Seven out of the nine studies on adults that used income as a measure of SEP found no association with atopic dermatitis or that lower income was associated with higher rates of atopic dermatitis. In contrast, six out of the seven studies on adults that used education as a measure of SEP found a positive association. All four studies involving adults that used class/occupation as a measure of SEP found no association with atopic dermatitis.
For studies that included children, the most commonly used measure of SEP was parental education, followed by household income and class (Table 3). The educational categories and cut-offs (i.e. graduate/professional school vs high school education) varied by study. The majority of studies using parental education (61%, 27/44) found a positive association between SEP and atopic dermatitis. In contrast, a minority of studies using household income (33%, 13/39) and class (40%, 6/15) found a positive association.
Discussion
In contrast to prior reports, our systematic review of the literature on SEP and atopic dermatitis found that a minority of studies (42%, 37/88) reported a positive association between high SEP and atopic dermatitis. The majority of studies found either no association between SEP and atopic dermatitis, an inconclusive association between SEP and atopic dermatitis based on multiple measures of SEP used in a study, or atopic dermatitis associated with low SEP. Studies from Europe and studies of children were most common and were more likely to report a positive association as compared to studies among adults and in other geographic settings. Smaller studies were more likely to report no association between SEP and atopic dermatitis, possibly due to lower statistical power.
A previous systematic review reported a significant positive association between SEP and atopic dermatitis, with pooled crude estimate for the odds ratio of disease for the lowest compared with the highest SEP of 0.72 (95% CI 0.61–0.83) (8). The authors of this study didn’t address how differing measures of socioeconomic position or atopic dermatitis were analyzed, which from a methodologic standpoint warrants consideration. Part of the discrepancy in results with our study may be due to our review containing many more studies (n = 88 versus n = 19). The additional studies in our review were published more recently, included more locations outside of Europe, and included more adults.
The conclusions from individual studies have varied in their explanations for reported associations. Studies finding a positive association between SEP and atopic dermatitis have discussed their results in the context of decreased immune system challenges from early life exposures or increased awareness of disease among higher SEP individuals. Other proposed mechanisms included differential exposure to tobacco smoke, pollutants or toxins.
Our results challenge prior literature suggesting that atopic dermatitis is a unique exception to the typical association between high SEP and better health outcomes (5)(8), and clinicians should be aware that patients from diverse backgrounds may be at equal risk. The decades-old “hygiene hypothesis” posited that individuals of higher SEP may be less likely to have environmental exposures important for reduction of allergic disease (17). More recent research has highlighted the importance of early life microbial exposures for immune system priming (7)(18). Our findings support the need for additional research on how different measures of SEP relate to microbial exposures, immune tolerance, and subsequent allergic disease over time, and atopic dermatitis provides a useful model for studying these dynamics (19).
Limitations of our study warrant discussion: the definition of both exposure (SEP) and outcome (atopic dermatitis) varied across studies, precluding quantitative meta-analysis of all studies. Moreover, both were largely self-reported, though most relied on a standardized questionnaire and self-report of atopic dermatitis has been shown to reasonably approximate physician assessment in both children and adults. (20)(21)(22) We focused on disease prevalence but were unable to analyze how SEP might affect disease severity or activity over time because there were not sufficient numbers of studies with consistent measures. Some data suggest that patients with lower SEP may experience more severe disease, therefore this is an important area for future research (11). This review highlights the importance of clear reporting and standardized measurement of SEP and atopic dermatitis. Because atopic dermatitis waxes and wanes over time and affects individuals of all ages, it is important to differentiate between the lifetime prevalence and period prevalence, and for future studies to examine longitudinal trends.
Conclusion
Many studies have examined the association between SEP and atopic dermatitis, however there is significant heterogeneity between the measures of SEP and measurement of atopic dermatitis, and clear conclusions on the directionality of association did not emerge. Given that atopic dermatitis affects up to one in five children worldwide, these results highlight the importance of additional research into social influences and disparities on atopic dermatitis disease severity and activity across the lifespan.
Supplementary Material
Funding statement:
The authors received no specific funding for this work. SML is supported by a Wellcome senior research fellowship in clinical science (205039/Z/16/Z). For the purpose of Open Access, the author has applied a CC BY public copyright license to any Author Accepted Manuscript (AAM) version arising from this submission.
SML is also supported by Health Data Research UK (grant no. LOND1), which is funded by the UK Medical Research Council, Engineering and Physical Sciences Research Council, Economic and Social Research Council, Department of Health and Social Care (England), Chief Scientist Office of the Scottish Government Health and Social Care Directorates, Health and Social Care Research and Development Division (Welsh Government), Public Health Agency (Northern Ireland), British Heart Foundation and Wellcome Trust. KA receives funding from NIAMS (K23AR073915) and the Robert Wood Johnson Foundation through the Amos Medical Faculty Development Program. The views in this manuscript do not necessarily represent the views of the funders.
Footnotes
Conflicts of interest: The authors have no conflicts of interest to declare.
References
- 1.Overview of Atopic Dermatitis. AJMC. (https://www.ajmc.com/journals/supplement/2017/atopic-dermatitis-focusing-on-the-patient-care-strategy-in-the-managed-care-setting/overview-of-atopic-dermatitis-article). (Accessed February 23, 2020)
- 2.Murray CJL, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2197–2223. [DOI] [PubMed] [Google Scholar]
- 3.Silverberg JI, Hanifin JM. Adult eczema prevalence and associations with asthma and other health and demographic factors: a US population-based study. J. Allergy Clin. Immunol 2013;132(5):1132–1138. [DOI] [PubMed] [Google Scholar]
- 4.Hay RJ, Johns NE, Williams HC, et al. The global burden of skin disease in 2010: an analysis of the prevalence and impact of skin conditions. J. Invest. Dermatol 2014;134(6):1527–1534. [DOI] [PubMed] [Google Scholar]
- 5.Adler NE, Newman K. Socioeconomic Disparities In Health: Pathways And Policies. Health Affairs. 2002;21(2):60–76. [DOI] [PubMed] [Google Scholar]
- 6.Rook GAW. Review series on helminths, immune modulation and the hygiene hypothesis: the broader implications of the hygiene hypothesis. Immunology. 2009;126(1):3–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Flohr C, Yeo L. Atopic dermatitis and the hygiene hypothesis revisited. Curr. Probl. Dermatol 2011;41:1–34. [DOI] [PubMed] [Google Scholar]
- 8.Uphoff E, Cabieses B, Pinart M, et al. A systematic review of socioeconomic position in relation to asthma and allergic diseases. European Respiratory Journal. 2015;46(2):364–374. [DOI] [PubMed] [Google Scholar]
- 9.Abuabara K, You Y, Margolis DJ, et al. Genetic ancestry does not explain increased atopic dermatitis susceptibility or worse disease control among African American subjects in 2 large US cohorts. J. Allergy Clin. Immunol 2020;145(1):192–198.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kantor R, Silverberg JI. Environmental risk factors and their role in the management of atopic dermatitis. Expert Rev Clin Immunol. 2017;13(1):15–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chung J, Simpson EL. The socioeconomics of atopic dermatitis. Ann. Allergy Asthma Immunol 2019;122(4):360–366. [DOI] [PubMed] [Google Scholar]
- 12.PRISMA. (http://www.prisma-statement.org/). (Accessed October 17, 2019)
- 13.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–2012. [DOI] [PubMed] [Google Scholar]
- 14.About Covidence. (https://community.cochrane.org/help/tools-and-software/covidence/about-covidence). (Accessed February 8, 2020)
- 15.Worldwide variation in prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and atopic eczema: ISAAC. The International Study of Asthma and Allergies in Childhood (ISAAC) Steering Committee. Lancet. 1998;351(9111):1225–1232. [PubMed] [Google Scholar]
- 16.Savage M, Devine F, Cunningham N, et al. A New Model of Social Class? Findings from the BBC’s Great British Class Survey Experiment. Sociology. 2013;47(2):219–250. [Google Scholar]
- 17.Okada H, Kuhn C, Feillet H, et al. The ‘hygiene hypothesis’ for autoimmune and allergic diseases: an update. Clin Exp Immunol. 2010;160(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Paller AS, Kong HH, Seed P, et al. The microbiome in patients with atopic dermatitis. Journal of Allergy and Clinical Immunology. 2019;143(1):26–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ding T, Schloss PD. Dynamics and associations of microbial community types across the human body. Nature. 2014;509(7500):357–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Is there a geographical variation in eczema prevalence in the U.K.? Evidence from the 1958 British birth cohort study - McNally - 2000 - British Journal of Dermatology - Wiley Online Library (https://onlinelibrary.wiley.com/doi/abs/10.1046/j.1365-2133.2000.03416.x?sid=nlm%3Apubmed). (Accessed August 25, 2021) [DOI] [PubMed]
- 21.Williams HC, Strachan DP, Hay RJ. Childhood eczema: disease of the advantaged? BMJ. 1994;308(6937):1132–1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Silverberg JI, Patel N, Immaneni S, et al. Assessment of atopic dermatitis using self-report and caregiver report: a multicentre validation study. British Journal of Dermatology. 2015;173(6):1400–1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


