Abstract
Background:
Aircraft noise can affect populations living near airports. Chronic exposure to aircraft noise has been associated with cardiovascular disease, including hypertension. However, previous studies have been limited in their ability to characterize noise exposures over time and to adequately control for confounders.
Objectives:
The aim of this study was to examine the association between aircraft noise and incident hypertension in two cohorts of female nurses, using aircraft noise exposure estimates with high spatial resolution over a 20-year period.
Methods:
We obtained contour maps of modeled aircraft noise levels over time for 90 U.S. airports and linked them with geocoded addresses of participants in the Nurses’ Health Study (NHS) and Nurses’ Health Study II (NHS II) to assign noise exposure for 1994–2014 and 1995–2013, respectively. We used time-varying Cox proportional hazards models to estimate hypertension risk associated with time-varying noise exposure (dichotomized at 45 and 55 dB(A)), adjusting for fixed and time-varying confounders. Results from both cohorts were pooled via random effects meta-analysis.
Results:
In meta-analyses of parsimonious and fully-adjusted models with aircraft noise dichotomized at 45 dB (A), hazard ratios (HR) for hypertension incidence were 1.04 (95% CI: 1.00, 1.07) and 1.03 (95% CI: 0.99, 1.07), respectively. When dichotomized at 55 dB(A), HRs were 1.10 (95% CI: 1.01, 1.19) and 1.07 (95% CI: 0.98, 1.15), respectively. After conducting fully-adjusted sensitivity analyses limited to years in which particulate matter (PM) was obtained, we observed similar findings. In NHS, the PM-unadjusted HR was 1.01 (95% CI: 0.90, 1.14) and PM-adjusted HR was 1.01 (95% CI: 0.89, 1.14); in NHS II, the PM-unadjusted HR was 1.08 (95% CI: 0.96, 1.22) and the PM-adjusted HR was 1.08 (95% CI: 0.95, 1.21). Overall, in these cohorts, we found marginally suggestive evidence of a positive association between aircraft noise exposure and hypertension.
Keywords: Aircraft noise exposure, Aircraft, Hypertension, Noise
1. Introduction
Individuals are exposed to multiple sources of noise every day from occupational and residential exposures. Although individuals can habituate to noise exposures at a certain level (Münzel et al., 2014), chronic noise exposures can still lead to changes in the autonomic nervous system and the endocrine system, resulting in adverse health effects such as increases in blood pressure, blood lipids, and glucose levels (Babisch, 2002; Babisch and van Kamp, 2009; Basner et al., 2014; Hammer et al., 2014; Münzel et al., 2014; Sørensen et al., 2013). Hypertension, in particular, has been examined extensively both because of the biological plausibility of the association and the public-health importance of hypertension (Fu et al., 2017; Ising and Kruppa, 2004; Jarup et al., 2008; Zhang et al., 2016). The biological plausibility of chronic exposure to noise leading to hypertension and cardiovascular effects has often been tested under occupational or experimental settings, although there is growing evidence that environmental noise may be linked to health outcomes (Hansell et al., 2013).
Aircraft noise may be more strongly related to adverse outcomes than many other noise sources. For example, aircraft noise was associated with greater self-reported annoyance and sleep disturbance compared with equivalent noise levels produced by other transportation sources, such as roads and railways (Ising and Kruppa, 2004; Münzel et al., 2014). In addition, adverse health effects, such as increased blood pressure, were shown to be more strongly associated with aircraft noise compared to white noise of the same level (Münzel et al. 2017, 2018). The distinct characteristics associated with aircraft noise exposure, such as its frequency and temporal sound pattern, as well as perception about the usefulness or desirability of the noise source, may drive cardiovascular effects through its impacts on levels of stress, annoyance and sleep (Münzel et al. 2017, 2018; van Kempen et al., 2002). Aircraft noise is also of particular interest due to its chronicity, intensity, and prevalence in certain communities near airports.
The magnitudes and strengths of the association between aircraft noise and hypertension have varied markedly across studies (Babisch and van Kamp, 2009; Huang et al., 2015; van Kempen et al., 2002). Some studies have reported an increased risk (Eriksson et al., 2007; Huang et al., 2015; Pyko et al., 2018), whereas others have found no association (Carugno et al., 2018; Zeeb et al., 2017). A number of factors could contribute to the inconsistency in the literature, including differences in study populations, noise modeling methods, exposure levels and characterization methods, ability to control for potential confounders, and study design (Chang et al., 2013; Huang et al., 2015). In particular, many studies are cross-sectional or case-control, with limited numbers of prospective cohort studies (Dimakopoulou et al., 2017; Eriksson et al., 2010; Evrard et al., 2017; Fuks et al., 2017; Jarup et al., 2008). There are also few studies with extensive longitudinal noise data at high spatial resolution.
In this study, we used noise exposure around multiple airports modeled using consistent software and criteria at high spatial resolution across a 20-year period, and we linked these longitudinal data with two large prospective cohorts. To our knowledge, this is the first multiairport prospective cohort study examining the association of aircraft noise with hypertension in the U.S.
2. Material and methods
2.1. Study populations
The two prospective cohorts included in this study were Nurses’ Health Study (NHS) and Nurses’ Health Study II (NHS II). NHS started in 1976 and is composed of 121,700 female nurses who were born between 1921 and 1946, living in one of 11 states (CA, CT, FL, MD, MA, MI, NJ, NY, OH, PA, and TX) at the time they were invited to participate. NHS II enrolled 116,429 female nurses who were born between 1946 and 1964, living in 14 states (CA, CT, IN, IA, KY, MA, MI, MO, NY, NC, OH, PA, SC, and TX) at baseline in 1989. There are now individuals from each cohort living in all 48 contiguous states and the District of Columbia. Questionnaires are mailed every two years with relatively high response rates (~90%) (Bao et al., 2016; Hart et al., 2018) that include extensive questions on demographic and physical characteristics, health status, lifestyle, and family disease history. Questionnaires also provide a detailed residential address history for each participant throughout our follow-up periods (NHS: 1994–2014, NHS II: 1995–2013). The Institutional Review Board at Brigham and Women’s Hospital approved the study protocol, and participants provided implied consent by virtue of returning the mailed questionnaires.
2.2. Aircraft noise exposure
We collaborated with the U.S. Federal Aviation Administration (FAA) and the John A. Volpe National Transportation Systems Center to obtain modeled noise contours for 1995, 2000, 2005, 2010, and 2015 for 90 U.S. airports (Fig. 1). Aircraft operations data came from the Official Airline Guide (OAG - air travel intelligence) for 1995, and from the Enhanced Traffic Management System (ETMS) for all other years.
Fig. 1.
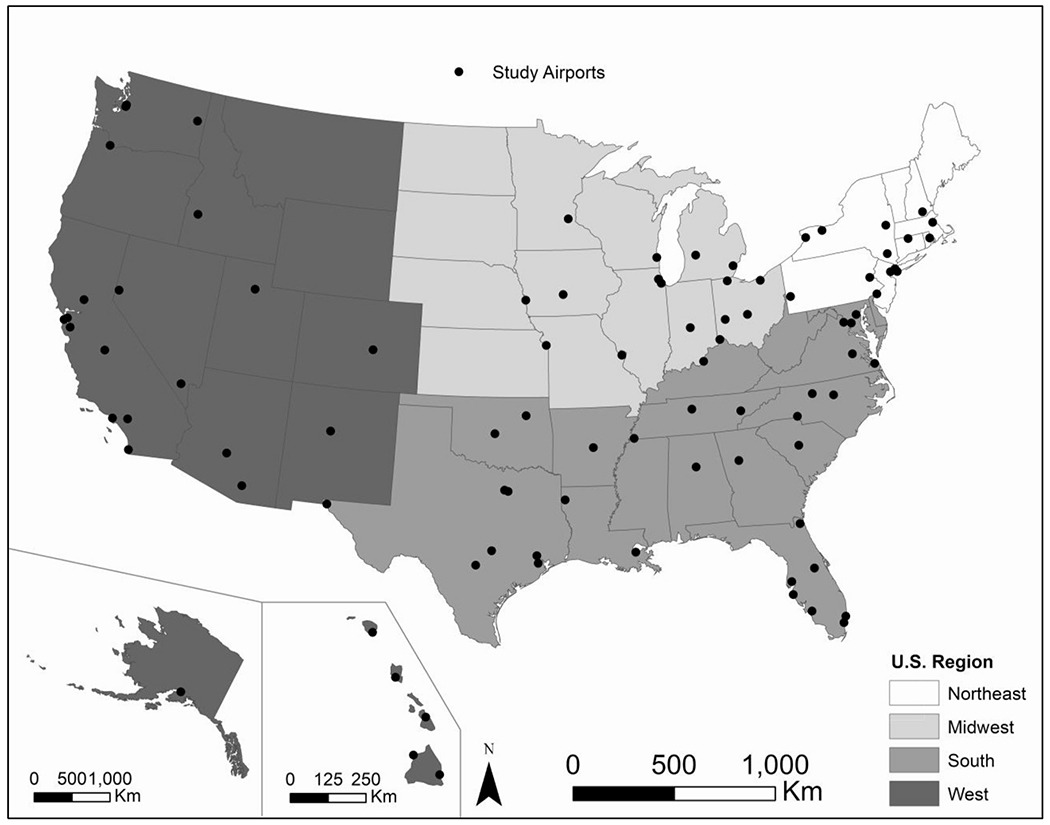
A map of 90 airports included in our study by region.
Based on standard modeling procedure, operations were annualized into a single average annual day using the following data: Aircraft Noise and Performance (ANP) aircraft type, day (07:00 to 22:00 local time) or night (22:00 to 07:00 local time), and operation airport (Federal Aviation Administration, 2014b). In addition, detailed departure and arrival runway, flight path utilization, and stage length data for the 90 airports were used to approximate tracks taken in an annualized year. The Aviation Environmental Design Tool (AEDT) was then employed to compute the noise exposure data using the annualized flight track information (Federal Aviation Administration, 2014b). AEDT simultaneously models both noise and emissions and is the tool used by U.S. regulatory bodies for domestic planning, environmental compliance, and research analyses (Federal Aviation Administration., 2014a). AEDT replaced the Integrated Noise Model (INM), one of the widely used legacy noise modeling tools, and incorporates improved algorithms to better capture aircraft performance and positioning (Federal Aviation Administration., 2014a).
The noise contour maps estimated noise exposure areas at 1 dB (dB) resolution down to a minimum of 45 dB(A) at a 0.1 nautical mile (~607 feet) spatial resolution due to the availability of data at the time. We focused on day-night average sound level (DNL), a 24-h weighted average that applies a 10 A-weighted decibel (dB(A)) penalty for nighttime noise, as it is the primary metric used in U.S. aviation decision-making.
The modeled exposure surfaces were intersected with the participants’ geocoded residential addresses during follow-up and the noise levels were assumed to have remained the same in each of the 5-year time intervals. A very small percentage (less than 1%) of participants lived close to more than one airport. For participants living near multiple airports, the sum of the noise contours was calculated (noting that noise is measured on a log-scale and therefore was summed using the formula ). We assumed that participants who did not live within the modeled noise contours of the 90 airports were exposed to less than DNL 45 dB(A) aircraft noise.
2.3. Hypertension incidence
Participants of each cohort self-reported hypertension diagnoses biennially. Hypertension incidence was defined as a new report of physician-diagnosed high blood pressure since the previous questionnaire. Previous studies have been performed in both NHS and NHS II to confirm the validity of self-report data with medical records (Colditz et al., 1986; Forman et al., 2008). For example, a study conducted on a random subsample of NHS participants from the 1982 questionnaire found that of those reporting hypertension, 100% had a systolic/diastolic blood pressure reading ≥140/≥90 mmHg and 77% had a reading ≥160/≥95 mmHg documented in medical records (Colditz et al., 1986). This study also obtained an age-stratified random sample of NHS participants from the 1980 questionnaire living in the Greater Boston Area and found that of those that did not report hypertension, 6.8% had blood pressure readings of ≥140/≥90 mmHg and none had readings ≥160/≥95 mmHg (Colditz et al., 1986). In NHS II, investigators surveyed a random subsample of respondents from the 2005 questionnaire and found that 94% of those who reported hypertension had medical record documentation, and 85% of those who did not report hypertension did not have documentation (Forman et al., 2008). We excluded women who reported a diagnosis of hypertension at and prior to baseline for this analysis (1994 for NHS and 1995 for NHS II, corresponding to the earliest date noise estimates were available).
2.4. Covariates
We selected a large set of a priori variables identified in the literature as potential predictors of noise or risk factors for hypertension. Fixed covariates, such as race, family history of hypertension, and individual-level socioeconomic status (SES) (partner’s educational attainment), and time-varying covariates, such as age, calendar year, menopausal status, diabetes, body mass index (BMI, kilograms per square meter), smoking status (current versus former/never smokers), physical activity (metabolic equivalent hours per week, MET), and medication use (current statin and nonnarcotic analgesic use) were obtained from questionnaire data. Neighborhood-level SES (nSES; Census tract-level median income and home value) and region of residence (Northeast, Midwest, South, West) were obtained for each 2-year period using data from the 2010 Census tracts. Standard food frequency questionnaires were used to calculate alcohol use (quintiles of grams per day) and diet (quintiles of the Dietary Approaches to Stop Hypertension (DASH) score (Harrington et al., 2013)). Time-varying covariates were updated every two years with the exception of diet and physical activity variables, which were updated every four years. Hearing loss, current night shift work status, and air pollution (fine [PM2.5] and coarse [PM2.5-10] particulate matter) were added to sensitivity models as we had limited data on these characteristics. Information on hearing loss was obtained in 2008 and 2009, and current night shift work status was available only in the NHS II cohort. Air pollution data were obtained from 1994 to 2007 and matched to participants’ geocoded addresses. Detailed methods for air pollution estimates are available elsewhere (Yanosky et al. 2008, 2014).
2.5. Statistical analysis
The final analytic dataset included a total of 162,183 participants, with 63,245 and 98,938 participants from NHS and NHS II, respectively. Our analyses were limited to years 1994–2014 for NHS and 1995–2013 for NHS II, given the availability of our noise data. Participants started contributing person-time from the return date of the baseline questionnaire until they developed hypertension, or were censored at the time of death, loss to follow-up, or end of follow-up. We assessed sociodemographic characteristics of participants of each cohort categorized into two groups using a 55 dB(A) cut-point to determine any exposure status-specific underlying differences.
We used time-varying Cox proportional hazards models, stratified by age in months and 2-year calendar period to adjust for trends over time, to estimate hypertension risk associated with time-varying aircraft noise exposure. In separate models, we used two different cut-points (DNL 45 and 55 dB(A)) to classify noise, with subjects below these cut-points considered as the reference group. We used a 45 dB(A) cut-point in order to assess the impact of modeled aircraft noise exposures above background, and a 55 dB(A) cut-point to further examine the exposure-response relationship. In basic models, we adjusted for age and calendar year. We also conducted parsimonious and fully-adjusted models given that some proposed covariates may be viewed as colliders or intermediates within the causal pathway between aircraft noise and hypertension (Glymour, 2006). In parsimonious models, we adjusted for age, calendar year, race, physical activity, smoking status, alcohol use, DASH, spouse’s education attainment, nSES (Census tract home value and household income), and region of residence. In fully-adjusted models, we additionally adjusted for menopausal status, family history of hypertension, BMI, and medication use (current statin and NSAID use).
The analyses were first conducted separately by cohort, then combined in a meta-analysis. In the meta-analysis, we applied inverse-variance weighting and used the DerSimonian and Laird method (DerSimonian and Laird, 1986) to determine heterogeneity of the two cohorts and if random-effects meta-analysis would be warranted.
We also conducted a series of sensitivity analyses to examine our results using the 55 dB(A) cut-point. First, we restricted our analyses to those participants who lived within the modeled noise contours of one of the 90 airports (those with assigned DNL ≥45 dB(A)) in an effort to address potential exposure error and to minimize the impact of potential differences in populations among those living proximate to airports versus farther away. Second, we excluded observations that had exposure at or above DNL 65 dB(A) (NHS: n ≥ 65 dB(A) = 125; NHS II: n ≥ 65 dB(A) = 288) because this is the eligibility threshold to receive noise abatement measures through the FAA at some individual airports, and therefore there is potential for increased exposure error. Third, we restricted our data to time periods (through 2009) where we were able to adjust our models for air pollution, to confirm the independent impact of noise on hypertension. Lastly, we adjusted our full multivariable models for current night shift work status among participants in the NHS II cohort.
We evaluated effect measure modification by including a multiplicative term of exposure and current smoking status, diabetes status, family history of hypertension, hearing loss, menopausal status, statin use, and race in order to identify potentially sensitive populations in our cohorts.
Statistical Analysis System (SAS) 9.4 (Cary, NC) was used for all analyses.
3. Results
As expected, given the earlier recruitment date for NHS, age distributions and some age-related outcomes (e.g., statin use and menopausal status) differed between NHS and NHS II (Table 1). For other variables, the baseline characteristics were relatively similar between the two cohorts, except for a fairly large difference in family history of hypertension, and small differences in alcohol consumption and current smoking status. A number of baseline characteristics of exposed and unexposed participants were similar in both cohorts such as age and BMI. However, there was some dissimilarity such as higher percentage of non-white, Census tract median home value, and air pollution levels in the groups exposed to ≥55 dB(A) compared to groups exposed to < 55 dB(A) (Table 1).
Table 1.
Age-standardized characteristics of Nurses’ Health Study (1994) and Nurses’ Health Study II (1995) participants at baseline, overall and by aircraft noise exposure.
| NHS |
NHS II |
|||||
|---|---|---|---|---|---|---|
| Overalla,b | DNL <55 dB (A) a,b | DNL ≥55 dB (A) a | Overalla,b | DNL <55 dB (A) a,b | DNL ≥55 dB (A) a | |
| N | 63,245 | 62,668 | 577 | 98,938 | 97,824 | 1,114 |
| Age, yrs c | 59.1 ± 7.1 | 59.1 ± 7.1 | 59.2 ± 6.9 | 40.3 ± 4.8 | 40.3 ± 4.7 | 40.3 ± 4.9 |
| DNL, dB(A) | 49.4 ± 4.1 | 48.3 ± 2.7 | 57.7 ± 2.8 | 49.6 ± 4.3 | 48.3 ± 2.7 | 57.8 ± 3.0 |
| White, % | 94.6 | 94.7 | 88.2 | 93.3 | 93.5 | 82.2 |
| Post-Menopausal, % | 87.8 | 87.8 | 86.8 | 7.2 | 7.2 | 5.4 |
| Partner’ s Education Attainment, % | ||||||
| Less than high school | 5.2 | 5.2 | 5.4 | 0.7 | 0.7 | 0.2 |
| High school | 37.9 | 37.8 | 42.7 | 17.1 | 17.1 | 16.3 |
| More than high school | 56.9 | 57.0 | 51.9 | 82.2 | 82.2 | 83.5 |
| BMI, kg/m2 | 25.5 ± 4.6 | 25.5 ± 4.6 | 25.6 ± 4.7 | 25.3 ± 5.4 | 25.3 ± 5.4 | 25.6 ± 5.6 |
| Family History of Hypertension, % | 36.1 | 36.1 | 36.1 | 49.3 | 49.2 | 51.6 |
| Statin Use, % d | 4.5 | 4.5 | 3.7 | 2.4 | 2.4 | 1.9 |
| Aspirin Use, % | ||||||
| < 1 day/mo | 56.9 | 56.9 | 56.3 | 77.3 | 77.3 | 77.7 |
| 1 day/wk | 12.6 | 12.6 | 15.1 | 14.4 | 14.4 | 13.5 |
| 2–3 days/wk | 9.2 | 9.2 | 8.9 | 4.3 | 4.3 | 4.0 |
| 4–5 days/wk | 6.9 | 7.0 | 5.3 | 1.2 | 1.2 | 1.5 |
| >5 days/wk | 14.4 | 14.4 | 14.4 | 2.9 | 2.9 | 3.3 |
| Ibuprofen Use, % | ||||||
| None | 81.2 | 81.2 | 83.2 | 35.3 | 35.3 | 41.0 |
| 1 day/wk | 5.6 | 5.6 | 5.5 | 39.6 | 39.7 | 36.5 |
| 2–3 days/wk | 4.6 | 4.6 | 5.1 | 16.9 | 16.9 | 14.8 |
| 4–5 days/wk | 2.0 | 2.0 | 1.5 | 3.5 | 3.5 | 4.2 |
| >5 days/wk | 6.6 | 6.6 | 4.7 | 4.7 | 4.7 | 3.4 |
| Acetaminophen Use, % | ||||||
| None | 86.6 | 86.6 | 85.7 | 45.7 | 45.6 | 47.5 |
| 1 day/wk | 4.5 | 4.5 | 4.0 | 40.4 | 40.4 | 41.9 |
| 2–3 days/wk | 4.0 | 4.0 | 4.7 | 10.3 | 10.3 | 8.2 |
| 4–5 days/wk | 1.7 | 1.7 | 1.0 | 2.0 | 2.0 | 1.5 |
| >5 days/wk | 3.3 | 3.2 | 4.6 | 1.7 | 1.7 | 0.9 |
| Current Smoker, % | 15.2 | 15.2 | 16.0 | 11.3 | 11.2 | 13.1 |
| Alcohol Consumption, g/day | 5.1 ± 8.8 | 5.1 ± 8.8 | 4.2 ± 6.9 | 3.5 ± 6.6 | 3.5 ± 6.6 | 3.6 ± 6.4 |
| DASH Score | 23.9 ± 4.6 | 23.9 ± 4.6 | 24.1 ± 4.7 | 23.7 ± 4.9 | 23.7 ± 4.9 | 23.3 ± 4.9 |
| Physical Activity, MET-hr/wk | 20.9 ± 26.0 | 20.9 ± 26.1 | 19.1 ± 22.3 | 18.7 ± 23.0 | 18.7 ± 23.0 | 19.8 ± 25.6 |
| Median Income, per 1,000 USD | 83.1 ± 35.0 | 83.1 ± 35.1 | 81.3 ± 32.0 | 80.4 ± 32.0 | 80.3 ± 32.0 | 83.1 ± 32.0 |
| Median Home Value, per 10,000 USD | 30.3 ± 22.0 | 30.2 ± 22.0 | 37.4 ± 21.6 | 26.7 ± 20.7 | 26.6 ± 20.7 | 37.0 ± 22.4 |
| PM2.5-10, μg/m3 | 9.1 ± 4.0 | 9.1 ± 4.0 | 10.8 ± 3.7 | 9.7 ± 4.1 | 9.7 ± 4.1 | 10.6 ± 3.5 |
| PM2.5, μg/m3 | 14.1 ± 3.1 | 14.0 ± 3.1 | 15.5 ± 2.7 | 14.0 ± 3.0 | 14.0 ± 3.0 | 14.9 ± 2.6 |
| Region of Residence, % | ||||||
| Northeast | 52.5 | 52.4 | 62.0 | 33.9 | 33.7 | 50.8 |
| Midwest | 17.3 | 17.4 | 8.8 | 32.7 | 32.9 | 15.7 |
| South | 16.5 | 16.6 | 15.1 | 18.3 | 18.3 | 19.1 |
| West | 13.6 | 13.6 | 14.2 | 15.1 | 15.2 | 14.3 |
Abbreviations: BMI, Body Mass Index; dB(A), A-Weighted Decibels; DNL, Day-Night average sound Level; DASH, Dietary Approaches to Stop Hypertension; g/day, grams per day; HR, Hazard Ratio; kg/m2, kilograms per square meter; μg/m3, micrograms per cubic meter; NHS, Nurses’ Health Study; NHS II, Nurses’ Health Study II; MET-hr/wk, metabolic equivalent hour per week; mo, month; PM, particulate matter; USD, United States Dollar; wk, week; yrs, years.
Values are means ± standard deviations (SD) for continuous variables; percentages for categorical variables and are standardized to the age distribution of the study population.
Means (SD) were obtained for noise measurements modeled (above 45 dB (A)).
Value is not age adjusted.
In NHS II, statin use was not obtained at baseline (1995); however, statin use was obtained during follow-up (starting in 1999).
The number of participants exposed to different levels of aircraft noise in each cohort at baseline are displayed in Table 2. Less than 10% of the NHS and NHS II participants at baseline were exposed to aircraft noise as a result of living near one of the 90 airports included in our noise exposure assessment (with DNL ≥45 dB(A)). About 1% of the participants were exposed to aircraft-associated DNL ≥55 dB(A). There were 33,190 and 28,256 hypertension cases contributing over 711,429 and 1,267,845 person-years in NHS and NHS II, respectively.
Table 2.
Hazard ratios (95% CIs) for hypertension associated with aircraft noise in NHS, NHS II, and meta-analysis of both cohorts in separate models.
| DNL category (in db(A)) | Cases | Person Years | Basic Modela HR (95% CI) | Parsimonious Modelb HR (95% CI) | Full Modelc HR (95% CI) | |
|---|---|---|---|---|---|---|
| NHS | ||||||
| ≥45 | 2,452 | 48,862 | 1.05 (1.01, 1.10) | 1.05 (1.01, 1.10) | 1.05 (1.00, 1.09) | |
| <45 | 30,738 | 662,567 | Ref. | Ref. | Ref. | |
| ≥55 | 318 | 6,103 | 1.09 (0.97, 1.21) | 1.07 (0.96, 1.20) | 1.05 (0.94, 1.17) | |
| <55 | 32,872 | 705,325 | Ref. | Ref. | Ref. | |
| NHS II | ||||||
| ≥45 | 2,167 | 96,894 | 1.00 (0.95, 1.04) | 1.02 (0.97, 1.07) | 1.01 (0.96, 1.05) | |
| <45 | 26,089 | 1,170,950 | Ref. | Ref. | Ref. | |
| ≥55 | 314 | 12,758 | 1.10 (0.99, 1.23) | 1.12 (1.00, 1.25) | 1.08 (0.97, 1.21) | |
| <55 | 27,942 | 1,255,087 | Ref. | Ref. | Ref. | |
| Meta-analysis | ||||||
| ≥45 | 4,619 | 145,756 | 1.03 (0.97, 1.08) | 1.04 (1.00, 1.07) | 1.03 (0.99, 1.07) | |
| <45 | 56,827 | 1,833,517 | Ref. | Ref. | Ref. | |
| ≥55 | 632 | 18,861 | 1.09 (1.01, 1.18) | 1.10 (1.01, 1.19) | 1.07 (0.98, 1.15) | |
| <55 | 60,814 | 1,960,412 | Ref. | Ref. | Ref. | |
Abbreviations: BMI, Body Mass Index; DASH, Dietary Approaches to Stop Hypertension; dB(A), A-Weighted Decibels; DNL, Day-Night Average Sound Level; HR, Hazard Ratio; NSAID, Non-Steroidal Analgesic Intake Drug; NHS, Nurses’ Health Study; NHS II, Nurses’ Health Study II; MET, Metabolic Equivalent; nSES, Neighborhood Level Socio-Economic Status.
Adjusted for age and calendar year.
Adjusted for age, calendar year, race, physical activity, smoking status, alcohol use, DASH, spouse’s education attainment, nSES (Census tract home value and household income), and region of residence.
Adjusted for age, calendar year, race, physical activity, smoking status, alcohol use, DASH, spouse’s education attainment, nSES (Census tract home value and household income), region of residence, menopausal status, family history of hypertension, and BMI.
Results from time-varying Cox proportional hazards models are also shown in Table 2. When comparing exposures to DNL at the 45 dB(A) cut-point, we observed similar estimates across basic, parsimonious, and fully-adjusted models. In our parsimonious models, we observed hazard ratios (HRs) of 1.05 (95% CI: 1.01, 1.10) and 1.02 (95% CI: 0.97, 1.07) in NHS and NHS II, respectively. In fully-adjusted models, we observed HRs of 1.05 (95% CI: 1.00, 1.09) in NHS I and 1.01 (95% CI: 0.96, 1.05) in NHS II. When examining exposures to DNL at the 55 dB(A) cut-point in parsimonious models, we observed similar findings, with HRs of 1.07 (95% CI: 0.96, 1.20) and 1.12 (95% CI: 1.00, 1.25) in NHS and NHS II, respectively. Fully-adjusted models yielded similar yet not statistically significant effect estimates, with HRs of 1.05 (95% CI: 0.94, 1.17) in NHS I and 1.08 (95% CI: 0.97, 1.21) in NHS II. In the meta-analysis of the two cohorts, we observed multivariable HRs in parsimonious models of 1.04 (95% CI: 1.00, 1.07) and 1.10 (95% CI: 1.01, 1.19) using the 45 dB(A) and 55 dB(A) cut-points, respectively. Similar yet attenuated estimates were observed in fully-adjusted models. No heterogeneity was observed between the two cohorts in all models.
We did not observe any evidence of effect modification by diabetes status, family history of hypertension, hearing problem, menopausal status, or statin use (Table 3). However, we did observe effect modification between smoking status and aircraft noise on hypertension in NHS (for smokers, HR: 0.68, 95% CI: 0.44, 1.03; for non-smokers, HR: 1.12, 95% CI: 0.99, 1.26) yet not in NHS II (for smokers, HR: 0.98, 95% CI: 0.67, 1.45; for non-smokers, HR: 1.10, 95% CI: 0.98, 1.24).
Table 3.
Effect modification of the association of exposure to DNL ≥55 dB(A) versus DNL <55 dB(A) on the risk of hypertension.
| NHS |
NHS II |
|||||
|---|---|---|---|---|---|---|
| Effect Modifier | Cases | Person-Years | Hazard Ratio (95% CI) | Cases | Person-Years | Hazard Ratio (95% CI) |
| Race | ||||||
| White | 31,327 | 675,735 | 1.03 (0.91, 1.16) | 26,304 | 1,197,244 | 1.12 (0.99, 1.27) |
| Non-White | 1,863 | 35,693 | 1.01 (0.68, 1.49) | 1,952 | 70,601 | 0.79 (0.58, 1.09) |
| p-for-interaction a | 0.40 | 0.21 | ||||
| Menopausal Status | ||||||
| Pre-menopausal | 963 | 28,087 | 1.09 (0.58, 2.06) | 15,415 | 805,691 | 1.04 (0.90, 1.21) |
| Post-menopausal | 32,166 | 681,611 | 1.04 (0.93, 1.17) | 10,319 | 380,334 | 1.08 (0.88, 1.32) |
| p-for-interaction a | 0.39 | 0.90 | ||||
| Hearing Loss | ||||||
| Yes | 3,820 | 74,773 | 0.93 (0.62, 1.41) | 887 | 31,172 | 1.36 (0.68, 2.72) |
| No | 22,700 | 499,621 | 1.03 (0.90, 1.19) | 21,955 | 983,268 | 1.03 (0.90, 1.17) |
| p-for-interaction a | 0.47 | 0.03 | ||||
| Diabetes | ||||||
| Yes | 1,921 | 28,016 | 1.15 (0.71, 1.85) | 1,099 | 20,481 | 0.95 (0.53, 1.71) |
| No | 31,269 | 683,413 | 1.04 (0.92, 1.17) | 27,157 | 1,247,364 | 1.08 (0.96, 1.21) |
| p-for-interaction a | 0.43 | 0.93 | ||||
| Family History of Hypertension | ||||||
| Yes | 13,622 | 254,140 | 1.01 (0.84, 1.21) | 16,930 | 594,914 | 1.08 (0.93, 1.25) |
| No | 19,568 | 457,289 | 1.07 (0.93, 1.24) | 11,326 | 672,931 | 1.09 (0.91, 1.31) |
| p-for-interaction a | 0.45 | 0.93 | ||||
| Statin Use | ||||||
| Yes | 6,407 | 112,069 | 1.13 (0.87, 1.46) | 3,260 | 83,325 | 0.96 (0.65, 1.41) |
| No | 26,783 | 599,359 | 1.05 (0.92, 1.19) | 24,996 | 1,184,520 | 1.10 (0.98, 1.24) |
| p-for-interaction a | 0.86 | 0.53 | ||||
| Smoking Status | ||||||
| Smoker | 3,544 | 77,687 | 0.68 (0.44, 1.03) | 2,634 | 108,976 | 0.98 (0.67, 1.45) |
| Non-Smoker | 29,586 | 632,391 | 1.12 (0.99, 1.26) | 25,580 | 1,157,273 | 1.10 (0.98, 1.24) |
| p-for-interaction a | <0.01 | 0.40 | ||||
| Region | ||||||
| Northeast | 16,895 | 358,947 | 1.04 (0.90, 1.21) | 9182 | 419,274 | 1.12 (0.94, 1.34) |
| Midwest | 5,621 | 122,043 | 0.97 (0.65, 1.43) | 9192 | 413,082 | 1.03 (0.79, 1.34) |
| South | 6,207 | 129,824 | 1.05 (0.78, 1.41) | 5824 | 234,354 | 1.15 (0.91, 1.45) |
| West | 4,466 | 100,518 | 1.25 (0.93, 1.69) | 4053 | 200,775 | 1.00 (0.72, 1.39) |
| p-for-interaction a | 0.77 | 0.90 | ||||
p-for-interaction for the multiplicative term of potential effect modifier by noise category.
The results from our sensitivity analyses using the 55 dB(A) cut-point broadly demonstrated the consistency of our findings as shown in Fig. 2. Restricting the analyses to participants who lived within the modeled noise contours for one of the 90 airports (DNL ≥45 dB(A)) resulted in a major reduction in sample size in both cohorts. Although we observed a HR above one for the relationship between aircraft noise and hypertension in NHS II, the HR changed to below one in NHS. Excluding participants who may have had noise abatement due to close proximity to an airport (DNL ≥65 dB(A)) had little influence given the small number of participants excluded from the model. When restricting the dataset for NHS to 2008 and NHS II to 2009 in order to adjust for air pollution, numbers of cases and person time were reduced to 28,641 cases with 602,374 person-years in NHS and 23,773 cases with 1,071,673 person-years in NHS II. When examining fully-adjusted multivariable associations between DNL at the 55 dB(A) cut-point and risk of hypertension in the truncated cohorts, we observed similar but attenuated results as the full cohorts (in NHS, HR: 1.01, 95% CI: 0.90, 1.14; in NHS II, HR: 1.08, 95% CI: 0.96, 1.22). After adding air pollution measurements into the models, results were similar, with an HR of 1.01 (95% CI: 0.89, 1.14) in NHS and HR of 1.08 (95% CI: 0.95, 1.21) in NHS II. Lastly, when we further adjusted our fully-adjusted multivariable model for current night shift status in the NHS II cohort, we found no change in effect estimate, with an HR of 1.08 (95% CI: 0.97, 1.21).
Fig. 2.
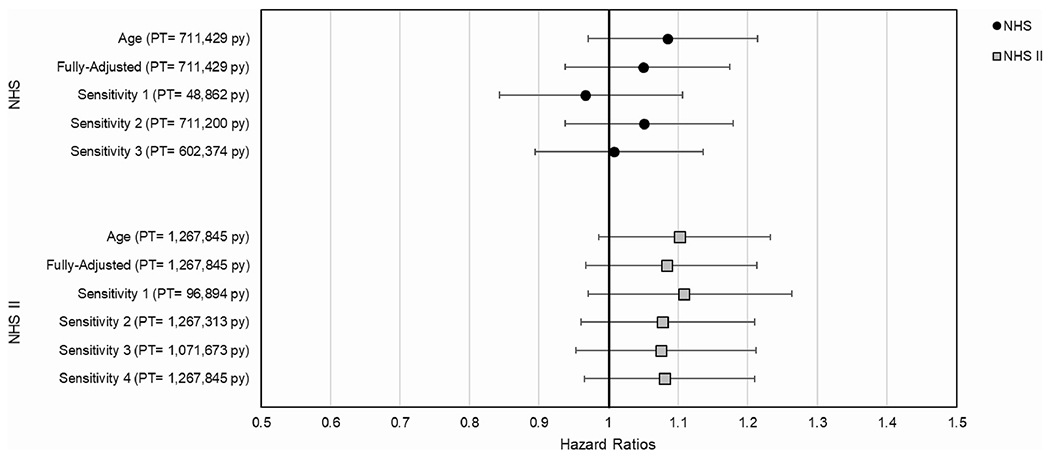
Hazard ratios (95% CIs) for associations between aircraft noise (DNL ≥55 dB(A) vs. <55 dB(A)) and hypertension in NHS and NHS II in basic (age), fully-adjusted, and sensitivity models (noting person-years). Fully Adjusted Model: Adjusted for age, calendar year, race, menopausal status, family history of hypertension, BMI, physical activity, smoking status, alcohol use, DASH, medication use (current statin and NSAID use), spouse’s education attainment, nSES (Census tract home value and household income), and region of residence. Sensitivity 1: Excluding observations under 45 dB(A). Sensitivity 2: Excluding observations greater than or equal to 65 dB(A). Sensitivity 3: Further adjustment for PM2.5 and PM2.5-10 (NHS: 1994-2008, NHS II: 1995-2009). Sensitivity 4: Further adjustment of fully-adjusted model for current night shift work in NHS II only. Abbreviations:BMI, Body Mass Index; DASH, Dietary Approaches to Stop Hypertension; dB(A), A-Weighted Decibels; DNL, Day-Night Average Sound Level; HR, Hazard Ratio; NSAID, Non-Steroidal Analgesic Intake Drug; NHS, Nurses’ Health Study; NHS II, Nurses’ Health Study II; MET, Metabolic Equivalent; PT, person-time contributed; PY, person-years; nSES, Neighborhood Level Socio-Economic Status.
4. Discussion
Our study, which to our knowledge is the first to examine the association between aircraft noise and hypertension in a large U.S. nationwide prospective cohort, found a marginally suggestive association between aircraft noise and risk of hypertension, with and without adjustment for other risk factors. Exposure to DNL ≥55 dB(A) was similarly weakly suggestive of an increased hypertension risk.
Although previous studies have used different exposure metrics and reflect multiple epidemiological study designs that complicate direct comparison of our quantitative estimates, our findings are broadly consistent with the literature investigating the association between aircraft noise and hypertension. Of note, Carugno et al., (2018) did not find consistent dose-dependence with exclusive categorical exposure groups compared to the referent group (<60 dB(A)), differing with choice of hypertension definition (Carugno et al., 2018). For example, the study reported a prevalence ratio of 0.94 (90% CI: 0.60, 1.50) for exposure estimates of 60–64 dB(A) and of 0.74 (90% CI: 0.36, 1.51) for 65–75 dB(A) using the World Health Organization (WHO) hypertension definition (Carugno et al., 2018). Additionally, a case-control study conducted by Zeeb and colleagues observed odds ratios (ORs) of 1.01 (95% CI: 0.99, 1.03) for 24-h noise estimates of 45–50 dB(A), 1.01 (95% CI: 0.98, 1.04) for 50–55 dB(A), and 0.97 (95% CI: 0.92, 1.02) for 55–60 dB(A) using hospital diagnosed hypertension (Zeeb et al., 2017). Another study found strong associations between day-evening-night average sound level (DENL or LDEN a 24-h weighted average similar to DNL, and hypertension in a cross-sectional analysis among male participants; however, they did not find associations among female participants (Evrard et al., 2017). In the HYENA study, investigators observed similar associations between LDEN and hypertension, with an OR of 1.04 (95% CI: 0.96, 1.12) for every 10 dB(A) (Babisch et al., 2013). Conversely, Pyko and colleagues found stronger positive associations between aircraft noise and hypertension (HR: 1.24, 95% CI: 1.06, 1.45) when dichotomizing LDEN into ≥45 vs. <45 dB(A) (Pyko et al., 2018).
Several studies reported that nighttime aircraft noise was more important than daytime noise (Dimakopoulou et al., 2017; Evrard et al., 2017; Jarup et al., 2008), consistent with associations of aircraft noise with sleep disturbance (Perron et al., 2012) or reflective of less misclassification related to exposure estimations at residential address due to time-activity patterns (Babisch and van Kamp, 2009). A cohort study conducted in Athens, Greece found relationships between aircraft noise exposure and hypertension, with an HR of 1.34 (95% CI: 0.57, 3.16) for every 10 dB (A) of daytime noise (07:00 to 23:00) and an HR of 3.39 (95% CI: 0.87, 13.3) for every 10 dB of nighttime noise (23:00 to 07:00) (Dimakopoulou et al., 2017). Of note, this study sampled percentages of participants living near the airport, within exposure contours <50, 50–60 and >60 dB(A) at 15%, 50% and 35%, respectively.
Our findings were relatively stable across multiple sensitivity analyses and were similar yet attenuated after controlling for a number of confounders. Excluding participants who did not live close to one of the 90 airports included in our noise modeling had a relatively large impact on the HR in NHS, but not in NHS II. Given that the effect estimate observed in NHS was smaller compared with NHS II, the reduction in sample size associated with this exclusion criterion may have led to less stable estimates and reduced power to detect the associations of interest. Excluding participants with DNL larger than 65 dB(A) resulted in a very small increase in relative risk for hypertension associated with aircraft noise in NHS, which may be related to the effect of the noise abatement programs, although given the small number of participants excluded, it is difficult to make definitive conclusions. The relationship between aircraft noise and hypertension was not confounded by particulate matter air pollution in NHS or NHS II, similar to the findings from other studies (Héritier et al., 2019; Stansfeld, 2015). Additionally, although we were unable to account for shiftwork in both cohorts, adjusting our model for night shift work status among participants in NHS II showed no change in our estimate.
When examining effect modification, we found a weaker relationship between aircraft noise and hypertension in smokers compared to non-smokers in NHS, similar to previous studies (Eriksson et al., 2007; Huang et al., 2015; Pyko et al., 2018). These results may indicate that noise does not contribute as much to cardiovascular outcomes when compared to smoking. Other studies also found effect modification by age group, sex, glucose tolerance and self-reported annoyance to aircraft noise, with higher associations among older individuals, men, non-smokers, those with normal glucose tolerance, and those who self-reported a high degree of annoyance (Eriksson et al. 2007, 2010; Evrard et al., 2017).
This study had a few limitations. Hypertension status was self-reported, however; validation studies showed very good correlation between the self-report and medical records (Colditz et al., 1986; Forman et al., 2008). Unfortunately, direct blood pressure measurements were not available in our cohorts, limiting our ability to detect associations with aircraft noise. Our results may underestimate true associations given that we were unable to incorporate access to care measures; because hypertension is often asymptomatic, it is commonly under-detected unless individuals have routine medical care. The study participants were primarily White female nurses; therefore, there may be limited generalizability to the general U.S. population.
Understanding the association between DNL and hypertension is important, as DNL is the specific metric used for policy purposes. However, DNL may not be the most sensitive measure of the impact of aircraft noise on hypertension, especially if sleep disturbance is considered a key pathway. In previous studies, nighttime noise has been shown to be more relevant (Dimakopoulou et al., 2017; Evrard et al., 2017; Jarup et al., 2008; Schmidt et al., 2015; Torjesen, 2017). That said, by applying a penalty to nighttime noise, DNL potentially captures some concerns about sleep disturbance. Although only DNL was available at the time of this analysis, analysis using nighttime noise or other noise metrics may be valuable to aid in establishing the mechanism by which noise is associated with hypertension. Additionally, DNL measurements were only available in 5-year increments and thus assumed to be consistent over each 5-year time-period, and data for earlier years and lower decibels were less precise. These may have led to some level of exposure measurement error.
Our study populations were not highly exposed to aircraft noise, which is to be expected for a nationwide cohort not recruited specifically for aircraft noise epidemiology. This makes identifying the association or determining the shape of the exposure-response function more challenging, especially if the association happens at a higher exposure level and/or the magnitude of the association is very small. In addition to lack of power due to the small number of participants exposed to a high level of aircraft noise, the noise estimates developed based on the residential addresses may not represent the true exposure levels of the participants as a result of time spent at home versus at work and home-specific factors, such as window opening behavior or the level of soundproofing (Lercher et al., 2000). Time spent at home versus at work is less of a concern for NHS, where many participants likely had retired by the time of this follow-up and were more likely to spend time at home. Home-specific factors can affect the individual noise exposure levels since people spend more time indoors than outdoors (Klepeis et al., 2001). However, it is unclear whether the exposure misclassification related to indoor and outdoor activity patterns and home-specific factors could be differential. In theory, those with higher ambient noise could take actions such as window closing to reduce their personal exposures. This would have resulted in biasing the results towards the null. But overall, the probability of substantial differential exposure misclassification is likely small, as most individuals spend a significant amount of time indoors at home, these populations have comparable workplace characteristics, and there is only a very small percentage of participants exposed to high levels of aircraft noise. Given the small magnitude of the observed health effect estimates of aircraft noise on hypertension in this study, it is important to consider the impact of these challenges.
Another potential source of exposure misclassification arises due to the fact that the noise estimates were only developed for 90 airports in the U.S.; therefore, participants who lived close to an airport that was not one of the 90 airports selected for assessment with our noise models would have been incorrectly assigned a lower DNL and included in the reference group. In an effort to address this limitation as well as the concern that populations not living near airports may differ in multiple ways from those who live near airports, we conducted a sensitivity analysis only including individuals within the noise contours around the selected 90 airports. While our findings were broadly consistent, this exclusion criterion led to dramatically reduced power to detect the effect of aviation noise on hypertension in NHS (Fig. 2).
Lastly, we were unable to adjust for other sources of noise exposure, such as road traffic, that may also be associated with hypertension. Several studies have found associations between road traffic noise exposure and incident hypertension (Banerjee et al., 2014; Bluhm et al., 2007; Jarup et al., 2008); yet when examined together studies have found stronger associations with aircraft noise (Dimakopoulou et al., 2017; Jarup et al., 2008). Additionally, studies have shown that annoyance from aircraft noise is greater than from road traffic noise (Miedema and Oudshoorn, 2001).
Our study also had several strengths. The prospective cohort study design provided a wide range of time-varying exposure, outcome, and covariate information over two decades of follow-up. The combination of extensive cohort data and motivated participants (all medical professionals) contributed to strong internal validity with potentially small residual confounding. We were also able to assess the impact of an array of potential confounders using high quality self-reported data. Another strength is the consistency of how aircraft noise estimates were developed, where the same protocol was used for developing noise contours for all 90 airports. This addresses one of the limitations often mentioned for meta-analyses investigating potential noise-hypertension associations that use noise and outcome data developed under different protocols and models.
5. Conclusions
In conclusion, we found a marginally suggestive relationship between aircraft noise exposure and hypertension in the NHS and NHS II cohorts. Given that the FAA uses a 65 dB(A) DNL threshold for sound mitigation, based on older evidence related to annoyance rather than health outcomes, our study results warrant further investigation regarding the health effects of aircraft noise exposure and more precise exposure assessment below the regulatory threshold.
Acknowledgements
This study was funded by Federal Aviation Administration (FAA) 13-C-AJFE-BU-016, under the Aviation Sustainability Center (ASCENT). Any opinions, findings, conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the FAA. Chloe Kim, Stephanie Grady, and Daniel Nguyen were also supported by the National Institute of Environmental Health Sciences (NIEHS) T32 training grant T32ES014562. Junenette Peters, Jonathan Levy, and Daniel Nguyen were additionally supported on R01ES025791-01A1, and Jaime Hart and Francine Laden were additionally supported on P30 ES000002. We acknowledge the contribution made by the John A. Volpe National Transportation Systems Center in developing the noise contours. The Nurses’ Health Studies are supported by UM1 CA186107, R01 HL150119, R01 HL034594, U01 CA176726, R01 HL35464, U01 HL145386.
Funding
This study was funded by Federal Aviation Administration (FAA) 13-C-AJFE-BU-016, under the Aviation Sustainability Center (ASCENT). Any opinions, findings, conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the FAA. Chloe Kim, Stephanie Grady, and Daniel Nguyen were also supported by the National Institute of Environmental Health Sciences (NIEHS) T32 training grant T32ES014562. Junenette Peters, Jonathan Levy, and Daniel Nguyen were additionally supported on R01ES025791-01A1, and Jaime Hart and Francine Laden were additionally supported on P30 ES000002. The Nurses’ Health Studies are supported by UM1 CA186107, R01 HL150119, R01 HL034594, U01 CA176726, R01 HL35464, U01 HL145386.
Footnotes
Human studies approval
This study involves human subjects, in which we have verified consent from subjects participating in this study was received prior to conducting the study. We also provide written assurance that the study has been reviewed and approved by the accredited committee, the Institutional Review Board at Brigham and Women’s Hospital.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Babisch W, 2002. The noise/stress concept, risk assessment and research needs. Noise Health 4, 1–11. [PubMed] [Google Scholar]
- Babisch W, Pershagen G, Selander J, Houthuijs D, Breugelmans O, Cadum E, et al. , 2013. Noise annoyance–a modifier of the association between noise level and cardiovascular health? Sci. Total Environ 452–453. 10.1016/j.scitotenv.2013.02.034, 50–57. [DOI] [PubMed] [Google Scholar]
- Babisch W, van Kamp I, 2009. Exposure-response relationship of the association between aircraft noise and the risk of hypertension. Noise Health 11, 161–168. 10.4103/1463-1741.53363. [DOI] [PubMed] [Google Scholar]
- Banerjee D, Das P, Fouzdar A, 2014. Urban residential road traffic noise and hypertension: a cross-sectional study of adult population. J. Urban Health 91, 1144–1157. 10.1007/sll524-014-9916-l. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bao Y, Bertoia M, Lenart E, Stampfer M, Willett W, Speizer F, et al. , 2016. Origin, methods, and evolution of the three nurses’ health studies. Am. J. Publ. Health 106, 1573–1581. 10.2105/AJPH.2016.303338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basner M, Babisch W, Davis A, Brink M, Clark C, Janssen S, et al. , 2014. Auditory and non-auditory effects of noise on health. Lancet 383, 1325–1332. 10.1016/S0140-6736(13)61613-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bluhm G, Berglind N, Nordling E, Rosenlund M, 2007. Road traffic noise and hypertension. Occup. Environ. Med 64, 122–126. 10.1136/oem.2005.025866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carugno M, Imbrogno P, Zucchi A, Ciampichini R, Tereanu C, Sampietro G, et al. , 2018. Effects of aircraft noise on annoyance, sleep disorders, and blood pressure among adult residents near the Orio al Serio International Airport (BGY), Italy. Med. Lav 109, 253–263. 10.23749/mdl.vl09i4.7271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang T, Hwang B, Liu C, Chen R, Wang V, Bao B, et al. , 2013. Occupational noise exposure and incident hypertension in men: a prospective cohort study. Am. J. Epidemiol 177, 818–825. 10.1093/aje/kws300. [DOI] [PubMed] [Google Scholar]
- Colditz G, Martin P, Stampfer M, Willett W, Sampson L, Rosner B, et al. , 1986. Validation of questionnaire information on risk factors and disease outcomes in a prospective cohort study of women. Am. J. Epidemiol 123, 894–900. 10.1093/oxfordjournals.aje.al14319. [DOI] [PubMed] [Google Scholar]
- DerSimonian R, Laird N, 1986. Meta-analysis in clinical trials. Contr. Clin. Trials 7, 177–188. 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- Dimakopoulou K, Koutentakis K, Papageorgiou I, Kasdagli M, Haralabidis A, Sourtzi P, et al. , 2017. Is aircraft noise exposure associated with cardiovascular disease and hypertension? Results from a cohort study in Athens, Greece. Occup. Environ. Med 74, 830–837. 10.1136/oemed-2016-104180. [DOI] [PubMed] [Google Scholar]
- Eriksson C, Bluhm G, Hilding A, Ostenson C, Pershagen G, 2010. Aircraft noise and incidence of hypertension–gender specific effects. Environ. Res 110, 764–772. 10.1016/j.envres.2010.09.001. [DOI] [PubMed] [Google Scholar]
- Eriksson C, Rosenlund M, Pershagen G, Hilding A, Ostenson C, Bluhm G, 2007. Aircraft noise and incidence of hypertension. Epidemiology 18, 716–721. 10.1097/EDE.0b013e3181567e77. [DOI] [PubMed] [Google Scholar]
- Evrard A, Lefèvre M, Champelovier P, Lambert J, Laumon B, 2017. Does aircraft noise exposure increase the risk of hypertension in the population living near airports in France? Occup. Environ. Med 74, 123–129. 10.1136/oemed-2016-103648. [DOI] [PubMed] [Google Scholar]
- Federal Aviation Administration, 2014a. AEDT: Product Information. Available: https://aedt.faa.gov/productreleases.aspx. (Accessed 18 September 2019).
- Federal Aviation Administration, 2014b. Aviation Environmental Design Tool (AEDT). Available: https://www.faa.gov/about/office_org/headquarters_offices/apl/research/models/aedt/. (Accessed 4 April 2017).
- Forman J, Curhan G, Taylor E, 2008. Plasma 25-hydroxyvitamin D levels and risk of incident hypertension among young women. Hypertension 52, 828–832. 10.1161/hypertensionaha.l08.117630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu W, Wang C, Zou L, Liu Q, Gan Y, Yan S, et al. , 2017. Association between exposure to noise and risk of hypertension: a meta-analysis of observational epidemiological studies. J. Hypertens 35, 2358–2366. 10.1097/HJH.0000000000001504. [DOI] [PubMed] [Google Scholar]
- Fuks K, Weinmayr G, Basagaña X, Gruzieva O, Hampel R, Oftedal B, et al. , 2017. Long-term exposure to ambient air pollution and traffic noise and incident hypertension in seven cohorts of the European study of cohorts for air pollution effects (ESCAPE). Eur. Heart J 38, 983–990. 10.1093/eurheartj/ehw413 [DOI] [PubMed] [Google Scholar]
- Glymour M, 2006. Using causal diagrams to understand common problems in social epidemiology. In: Methods in Social Epidemiology. Jossey-Bass/Wiley, Hoboken, NJ, US, pp. 393–428. [Google Scholar]
- Hammer M, Swinburn T, Neitzel R, 2014. Environmental noise pollution in the United States: developing an effective public health response. Environ. Health Perspect 122, 115–119. 10.1289/ehp.1307272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansell A, Blangiardo M, Fortunato L, Floud S, de Hoogh K, Fecht D, et al. , 2013. Aircraft noise and cardiovascular disease near Heathrow airport in London: small area study. BMJ 347, f5432. 10.1136/bmj.f5432. [DOI] [PubMed] [Google Scholar]
- Harrington J, Fitzgerald A, Kearney P, McCarthy V, Madden J, Browne G, et al. , 2013. DASH diet score and distribution of blood pressure in middle-aged men and women. Am. J. Hypertens 26, 1311–1320. 10.1093/ajh/hptl06. [DOI] [PubMed] [Google Scholar]
- Hart J, Bertrand K, DuPre N, James P, Vieira V, VoPham T, et al. , 2018. Exposure to hazardous air pollutants and risk of incident breast cancer in the Nurses’ Health Study II. Environ. Health 17, 28. 10.1186/sl2940-018-0372-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Héritier H, Vienneau D, Foraster M, Eze I, Schaffner E, de Hoogh K, et al. , 2019. A systematic analysis of mutual effects of transportation noise and air pollution exposure on myocardial infarction mortality: a nationwide cohort study in Switzerland. Eur. Heart J 40, 598–603. 10.1093/eurheartj/ehy650. [DOI] [PubMed] [Google Scholar]
- Huang D, Song X, Cui Q, Tian J, Wang Q, Yang K, 2015. Is there an association between aircraft noise exposure and the incidence of hypertension? A meta-analysis of 16784 participants. Noise Health 17, 93–97. 10.4103/1463-1741.153400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ising H, Kruppa B, 2004. Health effects caused by noise: evidence in the literature from the past 25 years. Noise Health 6, 5–13. [PubMed] [Google Scholar]
- Jarup L, Babisch W, Houthuijs D, Pershagen G, Katsouyanni K, Cadum E, et al. , 2008. Hypertension and exposure to noise near airports: the HYENA study. Environ. Health Perspect 116, 329–333. 10.1289/ehp.10775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klepeis N, Nelson W, Ott W, Robinson J, Tsang A, Switzer P, et al. , 2001. The National Human Activity Pattern Survey (NHAPS): a resource for assessing exposure to environmental pollutants. J. Expo. Anal. Environ. Epidemiol 11, 231–252. 10.1038/sj.jea.7500165. [DOI] [PubMed] [Google Scholar]
- Lercher P, Widmann U, Kofler W, 2000. Transportation noise and blood pressure: the importance of modifying factors. Internoise 4, 2302–2307, 2000. [Google Scholar]
- Miedema HM, Oudshoorn CG, 2001. Annoyance from transportation noise: relationships with exposure metrics DNL and DENL and their confidence intervals. Environ. Health Perspect 109, 409–416. 10.1289/ehp.01109409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Münzel T, Daiber A, Steven S, Tran L, Ullmann E, Kossmann S, et al. , 2017. Effects of noise on vascular function, oxidative stress, and inflammation: mechanistic insight from studies in mice. Eur. Heart J 38, 2838–2849. 10.1093/eurheartj/ehx081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Münzel T, Gori T, Babisch W, Basner M, 2014. Cardiovascular effects of environmental noise exposure. Eur. Heart J 35, 829–836. 10.1093/eurheartj/ehu030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Münzel T, Schmidt FP, Steven S, Herzog J, Daiber A, Sørensen M, 2018. Environmental noise and the cardiovascular system. J. Am. Coll. Cardiol 71, 688–697. 10.1016/j.jacc.2017.12.015. [DOI] [PubMed] [Google Scholar]
- Perron S, Tétreault L, King N, Plante C, Smargiassi A, 2012. Review of the effect of aircraft noise on sleep disturbance in adults. Noise Health 14, 58–67. 10.4103/1463-1741.95133. [DOI] [PubMed] [Google Scholar]
- Pyko A, Lind T, Mitkovskaya N, Ögren M, Östenson C, Wallas A, et al. , 2018. Transportation noise and incidence of hypertension. Int. J. Hyg Environ. Health 221, 1133–1141. 10.1016/j.ijheh.2018.06.005. [DOI] [PubMed] [Google Scholar]
- Schmidt F, Kolle K, Kreuder K, Schnorbus B, Wild P, Hechtner M, et al. , 2015. Nighttime aircraft noise impairs endothelial function and increases blood pressure in patients with or at high risk for coronary artery disease. Clin. Res. Cardiol 104, 23–30. 10.1007/s00392-014-0751-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sørensen M, Andersen Z, Nordsborg R, Becker T, Tjønneland A, Overvad K, et al. , 2013. Long-term exposure to road traffic noise and incident diabetes: a cohort study. Environ. Health Perspect 121, 217–222. 10.1289/ehp.1205503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stansfeld S, 2015. Noise effects on health in the context of air pollution exposure. Int. J. Environ. Res. Publ. Health 12, 12735–12760. 10.3390/ijerphl21012735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torjesen I, 2017. Long term aircraft noise is linked to incidence of high blood pressure. BMJ 357, j2872. 10.1136/bmj.j2872. [DOI] [Google Scholar]
- van Kempen E, Kruize H, Boshuizen H, Ameling C, Staatsen B, de Hollander A, 2002. The association between noise exposure and blood pressure and ischemic heart disease: a meta-analysis. Environ. Health Perspect 110, 307–317. 10.1289/ehp.02110307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yanosky J, Paciorek C, Laden F, Hart J, Puett R, Liao D, et al. , 2014. Spatiotemporal modeling of particulate air pollution in the conterminous United States using geographic and meteorological predictors. Environ. Health 13, 63. 10.1186/1476-069X13-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yanosky J, Paciorek C, Schwartz J, Laden F, Puett R, Suh H, 2008. Spatiotemporal modeling of chronic PM10 exposure for the nurses’ health study. Atmospheric Environ Oxf Engl 1994 42, 4047–4062. 10.1016/j.atmosenv.2008.01.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeeb H, Hegewald J, Schubert M, Wagner M, Dröge P, Swart E, et al. , 2017. Traffic noise and hypertension - results from a large case-control study. Environ. Res 157, 110–117. 10.1016/j.envres.2017.05.019. [DOI] [PubMed] [Google Scholar]
- Zhang Z, Laden F, Forman J, Hart J, 2016. Long-term exposure to particulate matter and self-reported hypertension: a prospective analysis in the Nurses’ Health Study. Environ. Health Perspect 124, 1414–1420. 10.1289/EHP163. [DOI] [PMC free article] [PubMed] [Google Scholar]


