Abstract
Background
Proximal humerus fractures are the third most common fracture in older adults. Because of the aging population, the incidence of these fractures and their impact will continue to grow. With advancement in treatment options for proximal humeral fractures, the aim of this study was to evaluate the trends in acute management of proximal humerus fractures to determine how definitive treatment has changed over the past decade in patients older than 65 years.
Methods
Using a commercially available database, patient records were queried from 2010 to 2019 for the incidence of proximal humerus fractures. For each individual year, data were queried to identify the incidence of closed reduction percutaneous pinning (CRPP), hemiarthroplasty (HA), intramedullary nailing (IMN), open reduction internal fixation (ORIF), total shoulder arthroplasty (TSA), reverse total shoulder arthroplasty (RSA), or nonoperative treatment for acute proximal humeral fractures. A Cochran-Armitage trend test was used to determine significant changes in the trends of proximal humerus fracture management. Logistic regression analyses were performed to generate odds ratios (OR) with associated 95% confidence intervals comparing each individual procedure performed in 2019 to 2010.
Results
A total of 160,836 patients at least 65 years of age and older were diagnosed with a proximal humerus fracture. Of this total, 28,503 (17.72%) patients received operative treatment and 132,333 (82.28%) received nonoperative treatment. From 2010 to 2019, operative treatment trends of proximal humerus fractures changed such that CRPP decreased by 60.0%, HA decreased by 81.4%, IMN decreased by 81.9%, ORIF decreased by 25.7%, TSA decreased by 80.5%, and RSA increased by 1841.4% (all P < .0001). Overall, nonsurgical management increased from 80% to 85% during the examined study period (P < .0001). Patients in 2019 were significantly more likely to receive an RSA (OR 22.65) and were significantly less likely to receive CRPP (OR 0.45), HA (OR 0.20), IMN (OR 0.20), ORIF (OR 0.82), and TSA (OR 0.22) than patients in 2010. In addition, patients in 2019 were significantly more likely to receive nonoperative treatment than patients in 2010 (OR 1.10).
Conclusion
Over the past decade, most of older adults who sustain proximal humerus fractures continue to receive nonoperative treatment. Although CRPP, IMN, HA, ORIF, and TSA have decreased, RSA has recently become more widely utilized, which is consistent with what has been noted in other countries. Continued examination of the mid- and long-term outcomes of the increasing percentages in RSA should be performed in this population.
Keywords: Proximal humerus fracture, Hemiarthroplasty, Reverse shoulder arthroplasty, Total shoulder arthroplasty, Internal fixation, Elderly
Accounting for 5%-6% of all adult fractures, proximal humerus fractures occur in the United States at an annual incidence of 600 cases per 1,000,000 people.5,13 These fractures have a bimodal distribution and typically involve young patients with high-energy trauma or older patients who experience low-energy falls. Proximal humerus fracture treatments vary based on myriad factors including fracture displacement, activity level, concurrent injuries, age, fracture type, and bone quality.26 Although proximal humerus fracture management in patients older than 65 years is debated, most of these fractures have historically been treated nonoperatively.16,17 When indicated, operative treatment options include open reduction internal fixation (ORIF), closed reduction percutaneous pinning (CRPP), intramedullary nailing (IMN), hemiarthroplasty (HA), total shoulder arthroplasty (TSA), and reverse total shoulder arthroplasty (RSA).7
As the third most common fracture type in the elderly following hip fractures and distal radius fractures, proximal humerus fracture cases are expected to rise with the aging U.S. population.2,12 With perceived increasing popularity of RSA and increasing prevalence of proximal humerus fractures in older adults, this study aimed to evaluate the trends in acute management of proximal humerus fractures to determine how treatment selection has changed over the last decade. It was hypothesized that RSA has increased relative to other surgical treatment options.
Materials and methods
Data source
A large nationwide commercially available administrative claims database, PearlDiver (PearlDiver, Inc, Fort Wayne, IN, USA), was utilized to retrospectively review deidentified patient records. This study used the “MUExtr” data set, a sub–data set of the 144 million patients within PearlDiver. Specifically, this data set contains patient records pertaining to procedures or diagnoses of the upper extremity from multiple insurance providers across U.S. territories and states including commercial insurance groups, Medicare, and Medicaid from 2010 to Q1 of 2020. Codes used from this data set included Current Procedural Technology (CPT) and International Classification of Diseases (ICD), Ninth Revision and Tenth Revision (ICD-9/ICD 10). Institutional review board exemption was granted through the Tulane University Human Research and Protection Program as the provided data were deidentified and compliant with the Health Insurance Portability and Accountability Act.
Patient selection
Using both ICD-9 and ICD-10 diagnostic codes, patient data consisting of a diagnosis of proximal humerus fracture were first queried. Patients who received either operative or nonoperative treatment of the proximal humerus fracture within 1 month of initial trauma were included in this study to best represent acute decision-making management. These data were queried each year from 2010 through 2019. Only patients aged 65 years and older were included. Patients with prior history of malignancy and infection were excluded. Records regarding fractures of the isolated greater tuberosity, shaft, or distal humerus were not included. Patients who passed away during the examined study period or did not have active follow-up during this time were also excluded. Given that both RSA and TSA are coded using the same CPT code (CPT-23472), these operations were identified with ICD-9 and ICD-10 procedural codes as these codes allow for specificity. Similar to previous studies, the use of ICD procedural codes for the procedures instead of CPT-23472 allowed accuracy in identifying TSA versus RSA during the studied time period.8,21,22 A comprehensive list of all ICD and CPT codes used in this study are included in Supplementary Table S1.
Outcomes
For each individual year of this study, data were queried for patients undergoing operative or nonoperative treatment within 1 month of their initial proximal humerus fracture. The procedures analyzed included CRPP, HA, ORIF, IMN, TSA, and RSA. Patients who received nonoperative treatment were identified if they did not have any surgical procedures or procedures requiring anesthesia within 1 month after initial proximal humerus fracture. One month was chosen for the operative cohort to define a period of acute treatment such that fractures fixed after this time period would be considered due to failure of nonoperative management.20
Statistical analysis
All data analyses were performed using the R statistical software (R Project for Statistical Computing, Vienna, Austria) integrated within PearlDiver and Microsoft Excel (Microsoft Corp., Redmond, WA, USA) with the XLStat statistical package add-on (Addinsoft Inc., New York, NY, USA) with an α level set to 0.05. A Cochran-Armitage trend test was performed to analyze operative management trends by evaluating the two-tailed null hypothesis that each treatment remained constant over the decade. Logistic regression analyses were conducted to generate odds ratios (ORs) with associated 95% confidence intervals (CIs) that compared each individual procedure in 2019 versus 2010.
Results
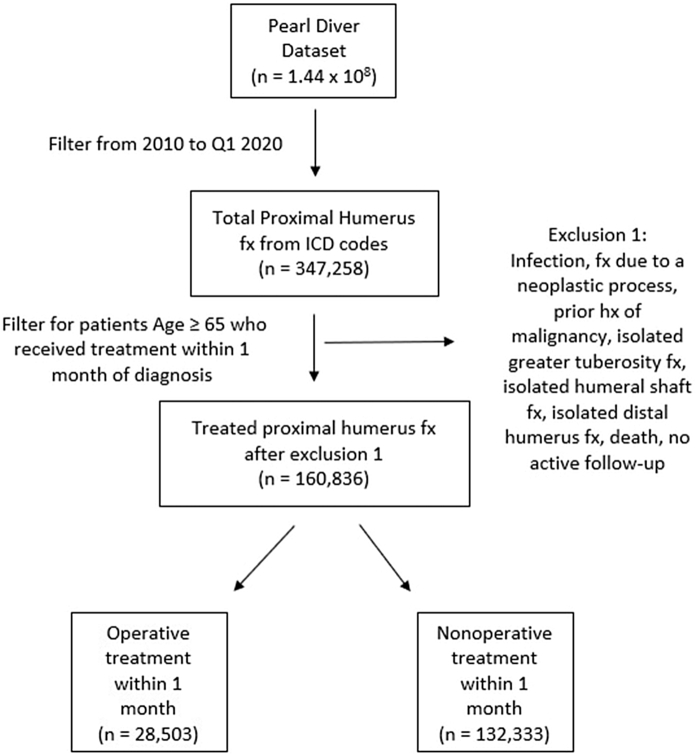
From 2010 to 2019, a total of 160,836 patients aged 65 years and older were diagnosed with a proximal humerus fracture, and of this total, 28,503 (17.72%) patients received operative treatment and 132,333 (82.28%) received nonoperative treatment (Fig. 1). The comprehensive breakdown of individual treatments provided to patients with a proximal humerus fracture by year is listed in Table I.
Figure 1.
The flow diagram of patients included in the study. Fx, fracture; Hx, history.
Table I.
Comprehensive breakdown of treatments provided to patients with proximal humerus fractures by year.
| Procedure | Number of patients | % |
|---|---|---|
| 2010 (n = 16,961) | ||
| CRPP | 225 | 1.33% |
| Hemiarthroplasty | 483 | 2.85% |
| Intramedullary nailing | 816 | 4.81% |
| ORIF | 1784 | 10.52% |
| Total shoulder arthroplasty | 77 | 0.45% |
| Reverse total shoulder arthroplasty | 29 | 0.17% |
| Nonoperative management | 13,547 | 79.87% |
| 2011 (n = 16,301) | ||
| CRPP | 186 | 1.14% |
| Hemiarthroplasty | 434 | 2.66% |
| Intramedullary nailing | 733 | 4.50% |
| ORIF | 1792 | 10.99% |
| Total shoulder arthroplasty | 11 | 0.07% |
| Reverse total shoulder arthroplasty | 112 | 0.69% |
| Nonoperative management | 13,033 | 79.95% |
| 2012 (n = 16,656) | ||
| CRPP | 170 | 1.02% |
| Hemiarthroplasty | 371 | 2.23% |
| Intramedullary nailing | 757 | 4.54% |
| ORIF | 1841 | 11.05% |
| Total shoulder arthroplasty | 8 | 0.05% |
| Reverse total shoulder arthroplasty | 155 | 0.93% |
| Nonoperative management | 13,354 | 80.18% |
| 2013 (n = 18,110) | ||
| CRPP | 237 | 1.31% |
| Hemiarthroplasty | 363 | 2.00% |
| Intramedullary nailing | 808 | 4.46% |
| ORIF | 2068 | 11.42% |
| Total shoulder arthroplasty | 21 | 0.12% |
| Reverse total shoulder arthroplasty | 220 | 1.21% |
| Nonoperative management | 14,393 | 79.48% |
| 2014 (n = 18,492) | ||
| CRPP | 203 | 1.10% |
| Hemiarthroplasty | 330 | 1.78% |
| Intramedullary nailing | 724 | 3.92% |
| ORIF | 2051 | 11.09% |
| Total shoulder arthroplasty | 16 | 0.09% |
| Reverse total shoulder arthroplasty | 357 | 1.93% |
| Nonoperative management | 14,811 | 80.09% |
| 2015 (n = 16,335) | ||
| CRPP | 151 | 0.92% |
| Hemiarthroplasty | 226 | 1.38% |
| Intramedullary nailing | 536 | 3.28% |
| ORIF | 1638 | 10.03% |
| Total shoulder arthroplasty | 15 | 0.09% |
| Reverse total shoulder arthroplasty | 329 | 2.01% |
| Nonoperative management | 13,440 | 82.29% |
| 2016 (n = 14,420) | ||
| CRPP | 122 | 0.85% |
| Hemiarthroplasty | 162 | 1.12% |
| Intramedullary nailing | 152 | 1.05% |
| ORIF | 1223 | 8.48% |
| Total shoulder arthroplasty | 11 | 0.08% |
| Reverse total shoulder arthroplasty | 351 | 2.43% |
| Nonoperative management | 12,399 | 85.99% |
| 2017 (n = 14,042) | ||
| CRPP | 90 | 0.64% |
| Hemiarthroplasty | 93 | 0.66% |
| Intramedullary nailing | 119 | 0.85% |
| ORIF | 1237 | 8.81% |
| Total shoulder arthroplasty | 11 | 0.08% |
| Reverse total shoulder arthroplasty | 405 | 2.88% |
| Nonoperative management | 12,087 | 86.08% |
| 2018 (n = 14,441) | ||
| CRPP | 75 | 0.52% |
| Hemiarthroplasty | 89 | 0.62% |
| Intramedullary nailing | 158 | 1.09% |
| ORIF | 1239 | 8.58% |
| Total shoulder arthroplasty | 13 | 0.09% |
| Reverse total shoulder arthroplasty | 444 | 3.07% |
| Nonoperative management | 12,423 | 86.03% |
| 2019 (n = 15,078) | ||
| CRPP | 90 | 0.60% |
| Hemiarthroplasty | 90 | 0.60% |
| Intramedullary nailing | 148 | 0.98% |
| ORIF | 1326 | 8.79% |
| Total shoulder arthroplasty | 15 | 0.10% |
| Reverse total shoulder arthroplasty | 563 | 3.73% |
| Nonoperative management | 12,846 | 85.20% |
CRPP, closed reduction percutaneous pinning; ORIF, open reduction internal fixation.
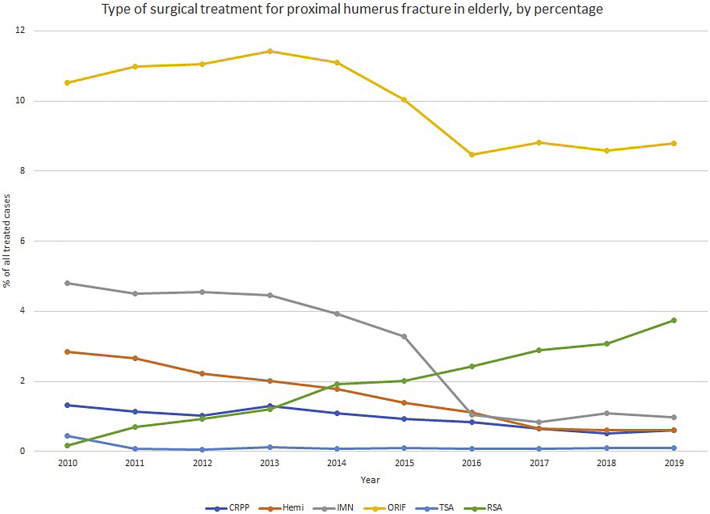
When evaluating the decade trends for each individual treatment utilizing the Cochran-Armitage trend test, the rates of CRPP decreased by 60.0%, HA decreased by 81.4%, IMN decreased by 81.9%, ORIF decreased by 25.7%, and TSA decreased by 80.5%, whereas the rate of RSA increased by 1841.4% (all P < .0001) as seen in Table II. The rate of nonoperative management increased during the study period from 80% to 85% (P < .0001). When the rates of operative procedures for proximal humerus fractures were compared between 2010 and 2019, patients in 2019 were more likely to receive an RSA than those in 2010 (OR 22.65, 95% CI: 15.58-32.91). Conversely, patients in 2019 were less likely to receive CRPP, HA, IMN, ORIF, and TSA than those in 2010 (CRPP, OR 0.45, 95% CI: 0.35-0.57; HA, OR 0.20, 95% CI: 0.16-0.26; IMN, OR 0.20, 95% CI: 0.16-0.23; ORIF, OR 0.82, 95% CI: 0.76-0.88; TSA, OR 0.22, 95% CI 0.13-0.38). Patients in 2019 were also more likely to receive nonoperative treatment than patients in 2010 (OR 1.10, 95% CI 1.06-1.15) (Table III).
Table II.
Operative treatment trends for 65-year-old patients and older over the decade.
| Treatment trends from 2010 to 2019 for patients aged 65 years and older | Total % change | P value |
|---|---|---|
| CRPP | –60.0 | <.0001 |
| Hemiarthroplasty | –81.4 | <.0001 |
| Intramedullary nailing | –81.9 | <.0001 |
| ORIF | –25.7 | <.0001 |
| Total shoulder arthroplasty | –80.5 | <.0001 |
| Reverse total shoulder arthroplasty | 1841.4 | <.0001 |
CRPP, closed reduction percutaneous pinning; ORIF, open reduction internal fixation.
Table III.
An odds ratio comparison of proximal humerus treatments in 2019 versus 2010.
| 2019 versus 2010 treatments | ORs (95% CI) |
|---|---|
| CRPP | 0.45 (0.35-0.57) |
| Hemiarthroplasty | 0.20 (0.16-0.26) |
| Intramedullary nailing | 0.20 (0.16-0.23) |
| ORIF | 0.82 (0.76-0.88) |
| Total shoulder arthroplasty | 0.22 (0.13-0.38) |
| Reverse total shoulder arthroplasty | 22.65 (15.58-32.91) |
| Nonoperative treatment | 1.10 (1.06-1.15) |
OR, odds ratio; CI, confidence interval; CRPP, closed reduction percutaneous pinning; ORIF, open reduction internal fixation.
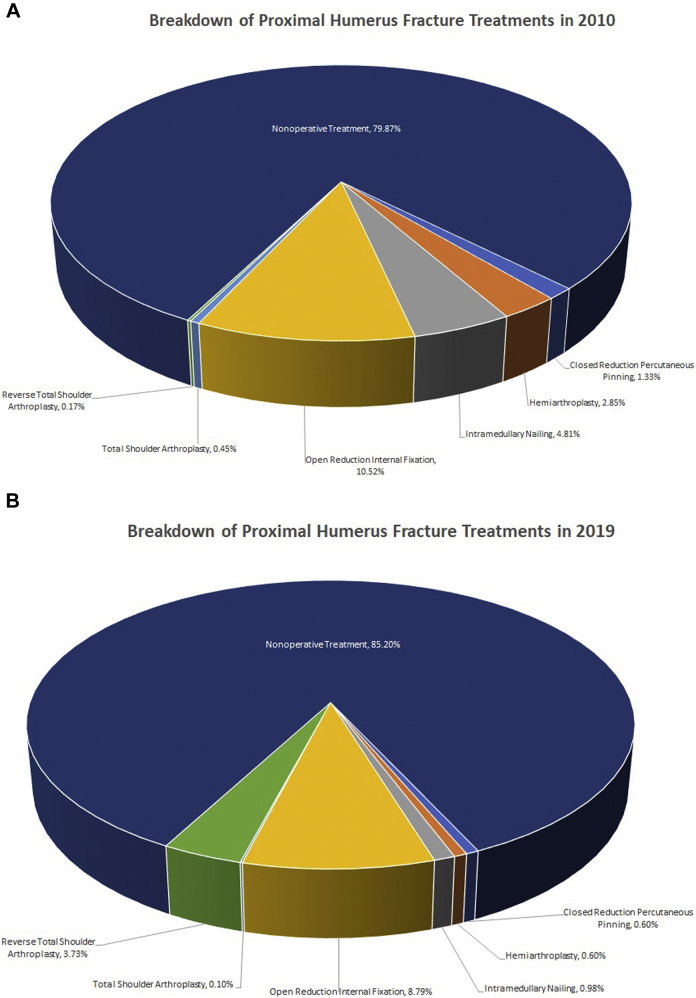
The number of surgeries performed for proximal humerus fractures over the past decade by percentage of all treated proximal humerus fractures can be seen in Figure 2. Graphic representation of the relative treatment proportions of 2010 versus 2019 can be seen in Figure 3.
Figure 2.
The proportional trend of acute operative treatments given to elderly patients in 2010-2019 after sustaining a proximal humerus fracture. CRPP, closed reduction percutaneous pinning; Hemi, hemiarthroplasty; IMN, intramedullary nailing; ORIF, open reduction internal fixation; TSA, total shoulder arthroplasty; RSA, reverse total shoulder arthroplasty.
Figure 3.
Proportional changes in treatments from 2010 to 2019. (A) Breakdown of treatments in 2010. (B) Breakdown of treatments in 2019.
Discussion
With improvements in health care, life expectancy in the United States has increased from 69.9 to 78.9 years from 1959 to 2016.28 In addition, Khatib et al reported a 28% increase in population-adjusted incidence of proximal humerus fractures from 1990 to 2010 in patients aged 65 years and older and attributed this overall increase to the aging population as patients younger than 65 years had no significant increase in proximal humerus fracture incidence.14 Although cases of proximal humerus fractures in the elderly increase, there is still no consensus in selecting between different treatment options.24
In a 2016 study of U.S. epidemiological trends, Han et al reported nonoperative treatment to be the mainstay proximal humerus fracture management in the elderly with an increasing rate of RSA despite ORIF being the most common operative procedure over an 8-year span.8 Hasty et al in 2017 demonstrated nonoperative treatment to similarly be the treatment of choice for proximal humerus fractures over an 8-year span in the United States despite rates of operative management rising with ORIF as the most common procedure performed and a decreasing rate of HA while RSA increased.9 In 2016, when examining only operative treatments for proximal humerus fractures, Rosas et al determined HA to be the most common operative treatment in the United States despite a decreasing trend in use over a 3-year span with RSA rates increasing and ORIF rates remaining constant.21
When examining international treatment trends, Klug et al tracked proximal humerus management from 2007 to 2016 in a national German registry and reported ORIF to be the most common operative treatment method, although RSA had the greatest proportional increase in utility over that period supporting its growing popularity.15 Evaluating the 9-year surgical trend of the South Korean population from 2008 to 2016, Jo et al documented ORIF rates increasing in this cohort.11 However, this study did highlight a proportionate increase in the overall rate of RSA over this time period, accounting for greater than 50% of all arthroplasty procedures in the final year of the study period.11 Sumrein et al reported a rise in ORIF treatment of proximal humerus fractures for the Swedish population from 2001 to 2012 with the rate of arthroplasty doubling.27 While studying the 23-year long-term trends of surgical treatment for proximal humerus fractures in the Finnish population, Huttunen et al documented a similar rise in ORIF treatment as the most common operative procedure, whereas there was a 6-fold increase in arthroplasty rates from 1987 to 2009.10 Data in the present study are aligned with other global population treatment trends such that there continues to be an increase in RSA performed in this cohort.
After initial approval by the Food and Drug Administration in 2003, RSA has gained popularity as a treatment option in the United States for elderly patients with severe proximal humerus fractures.23 When used for treatment of proximal humerus fractures, RSA prosthesis survival has been reported to be as high as 91% after 20 years with satisfactory functional outcomes.6 As poor functional outcomes have been reported with HA in the setting of rotator cuff deficiencies, Mata-Fink et al demonstrated RSA to have superior functional outcomes in a 2013 systematic review of proximal humerus management in older adults.18 Because of ORIF and HA having the potential for complications including nonunion and poor tuberosity healing, RSA may be a viable option in the aging population for patients with complex multiple-part proximal humerus fracture patterns as it allows for greater tolerance in tuberosity positioning and healing.1,3,4 If ORIF fails in the elderly, salvage RSA may remain as an option for proximal humerus fractures. However, RSA after failed ORIF has been reported to have higher complication rates than acute RSA treatment after a proximal humerus fracture with primary RSA having significantly better range of motion, better patient-reported outcomes, and fewer complications than patients with RSA performed as a revision salvage procedure and may also contribute to surgeons choosing primary RSA over ORIF.19,25
This study has several limitations inherent to database studies. Both ICD-9 and ICD-10 codes were manually examined and queried for this study. As code descriptions differ between ICD-9 and ICD-10 for given diagnoses and procedures, there is a possibility of coding discrepancies. To reduce this potential limitation, a coding translator was used to ensure that relevant ICD-9 and ICD-10 codes were used and that chosen ICD-9 codes corresponded with chosen ICD-10 codes. Given this study only reported on trends of proximal humerus fractures and rates of operative versus nonoperative management using retrospective data, outcome and complication information cannot be attained. In addition, this study was inclusive of all proximal humerus fractures to show an overview of the last decade’s trends as a whole. Therefore, diverse fracture patterns ranging from nondisplaced to 4-part fractures were examined together, and analysis did not evaluate differing treatments for each pattern. An inherent limitation of a claims study is human error created from errors in medical billing code input. However, a study from the Centers for Medicare and Medicaid Services reported such instances make up only 1.0% of overall payments and thus would have minimal impact on the outcomes seen.29 These data are from a U.S. database, so the trends may not accurately reflect global trends in proximal humerus fracture management. Additionally, the decision to use only ICD procedural codes in identifying procedures such as TSA and RSA may have undercounted the procedures performed. However, this decision was necessary, given TSA and RSA have the same CPT code (CPT-23472). In addition, certain CPT codes aggregate multiple procedures under the same code such as HA, TSA, and RSA for prosthetic replacement (CPT-23616). This CPT code was therefore excluded to maintain specificity; however, the total number of patients with this CPT was comparable with the total number of patients identified through ICD procedural codes. By solely using ICD codes to identify these operations, this study was able to more accurately distinguish procedures such as TSA and RSA as there are specific ICD codes for each. Finally, the switch from ICD-9 to ICD-10 in October of 2015 likely accounts for the drop in total proximal humerus fracture patients seen in the following data. However, any coding issues due to the transition would be expected in all treatment groups and would be unlikely to affect percentages.
Conclusion
Over the past decade, most of older adults who sustain proximal humerus fractures are treated nonoperatively at an increasing rate. RSA has continued to increase in comparison with CRPP, HA, IMN, ORIF, and TSA as the first-line surgical treatment option consistent with what has been seen in other countries. Continued examination of the mid- and long-term outcomes of RSA should be performed in this population.
Disclaimers
Funding: No funding was disclosed by the authors.
Conflicts of interest: F.H.S. has received royalties from Smith and Nephew, Exactech, CONMED, and Zimmer Biomet and is affiliated with and currently serves as the 1st Vice President of the American Academy of Orthopaedic Surgery. These royalties and affiliation are not related to the subject of this work. M.J.O.B. has received consultant payments from Smith and Nephew, Exactech, Wright Medical, and Aevumed. These payments are not related to the subject of this work. The other authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Institutional review board exemption was granted by Tulane University Biomedical IRB (study #: 2021-632).
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jseint.2021.08.006.
Supplementary data
References
- 1.Adeyemo A., Bertha N., Perry K.J., Updegrove G. Implant selection for proximal humerus fractures. Orthop Clin North Am. 2021;52:167–175. doi: 10.1016/j.ocl.2020.12.008. [DOI] [PubMed] [Google Scholar]
- 2.Baron J.A., Barrett J.A., Karagas M.R. The epidemiology of peripheral fractures. Bone. 1996;18:S209–S213. doi: 10.1016/8756-3282(95)00504-8. [DOI] [PubMed] [Google Scholar]
- 3.Boileau P., Alta T.D., Decroocq L., Sirveaux F., Clavert P., Favard L., et al. Reverse shoulder arthroplasty for acute fractures in the elderly: is it worth reattaching the tuberosities? J Shoulder Elbow Surg. 2019;28:437–444. doi: 10.1016/j.jse.2018.08.025. [DOI] [PubMed] [Google Scholar]
- 4.Boileau P., Krishnan S.G., Tinsi L., Walch G., Coste J.S., Molé D. Tuberosity malposition and migration: Reasons for poor outcomes after hemiarthroplasty for displaced fractures of the proximal humerus. J Shoulder Elbow Surg. 2002;11:401–412. doi: 10.1067/mse.2002.124527. [DOI] [PubMed] [Google Scholar]
- 5.Court-Brown C.M., Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37:691–697. doi: 10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 6.Gallinet D., Cazeneuve J.F., Boyer E., Menu G., Obert L., Ohl X., et al. Reverse shoulder arthroplasty for recent proximal humerus fractures: outcomes in 422 cases. Orthop Traumatol Surg Res. 2019;105:805–811. doi: 10.1016/j.otsr.2019.03.019. [DOI] [PubMed] [Google Scholar]
- 7.Gupta A.K., Harris J.D., Erickson B.J., Abrams G.D., Bruce B., McCormick F., et al. Surgical management of complex proximal humerus fractures-a systematic review of 92 studies including 4500 patients. J Orthop Trauma. 2015;29:54–59. doi: 10.1097/BOT.0000000000000229. [DOI] [PubMed] [Google Scholar]
- 8.Han R.J., Sing D.C., Feeley B.T., Ma C.B., Zhang A.L. Proximal humerus fragility fractures: recent trends in nonoperative and operative treatment in the Medicare population. J Shoulder Elbow Surg. 2016;25:256–261. doi: 10.1016/j.jse.2015.07.015. [DOI] [PubMed] [Google Scholar]
- 9.Hasty E.K., Jernigan E.W., Soo A., Varkey D.T., Kamath G.V. Trends in surgical management and costs for operative treatment of proximal humerus fractures in the elderly. Orthopedics. 2017;40:e641–e647. doi: 10.3928/01477447-20170411-03. [DOI] [PubMed] [Google Scholar]
- 10.Huttunen T.T., Launonen A.P., Pihlajamäki H., Kannus P., Mattila V.M. Trends in the surgical treatment of proximal humeral fractures - a nationwide 23-year study in Finland. BMC Musculoskelet Disord. 2012;13:261. doi: 10.1186/1471-2474-13-261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jo Y.H., Lee K.H., Lee B.G. Surgical trends in elderly patients with proximal humeral fractures in South Korea: a population-based study. BMC Musculoskelet Disord. 2019;20:136. doi: 10.1186/s12891-019-2515-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kannus P., Palvanen M., Niemi S., Parkkari J., Järvinen M., Vuori I. Increasing number and incidence of osteoporotic fractures of the proximal humerus in elderly people. Br Med J. 1996;313:1051–1052. doi: 10.1136/bmj.313.7064.1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Karl J.W., Olson P.R., Rosenwasser M.P. The epidemiology of upper extremity fractures in the United States, 2009. J Orthop Trauma. 2015;29:e242–e244. doi: 10.1097/BOT.0000000000000312. [DOI] [PubMed] [Google Scholar]
- 14.Khatib O., Onyekwelu I., Zuckerman J.D. The incidence of proximal humeral fractures in New York State from 1990 through 2010 with an emphasis on operative management in patients aged 65 years or older. J Shoulder Elbow Surg. 2014;23:1356–1362. doi: 10.1016/j.jse.2013.12.034. [DOI] [PubMed] [Google Scholar]
- 15.Klug A., Gramlich Y., Wincheringer D., Schmidt-Horlohé K., Hoffmann R. Trends in surgical management of proximal humeral fractures in adults: a nationwide study of records in Germany from 2007 to 2016. Arch Orthop Trauma Surg. 2019;139:1713–1721. doi: 10.1007/s00402-019-03252-1. [DOI] [PubMed] [Google Scholar]
- 16.Koval K.J., Gallagher M.A., Marsicano J.G., Cuomo F., McShinawy A., Zuckerman J.D. Functional outcome after minimally displaced fractures of the proximal part of the humerus. J Bone Jt Surg - Ser A. 1997;79:203–207. doi: 10.2106/00004623-199702000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Kruithof R.N., Formijne Jonkers H.A., van der Ven D.J.C., van Olden G.D.J., Timmers T.K. Functional and quality of life outcome after non-operatively managed proximal humeral fractures. J Orthop Traumatol. 2017;18:423–430. doi: 10.1007/s10195-017-0468-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mata-Fink A., Meinke M., Jones C., Kim B., Bell J.-E. Reverse shoulder arthroplasty for treatment of proximal humeral fractures in older adults: a systematic review. J Shoulder Elbow Surg. 2013;22:1737–1748. doi: 10.1016/j.jse.2013.08.021. [DOI] [PubMed] [Google Scholar]
- 19.Nelson P.A., Kwan C.C., Tjong V.K., Terry M.A., Sheth U. Primary versus salvage reverse total shoulder arthroplasty for displaced proximal humerus fractures in the elderly: a systematic review and Meta-analysis. J Shoulder Elbow Arthroplast. 2020;4 doi: 10.1177/2471549220949731. :247154922094973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Patel A.H., Lee O.C., O’Brien M.J., Savoie F.H., Sherman W.F. Short-term reoperation risk after surgical and nonsurgical management of isolated greater tuberosity fractures. JSES Int. 2021;5:532–539. doi: 10.1016/j.jseint.2020.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rosas S., Law T.Y., Kurowicki J., Formaini N., Kalandiak S.P., Levy J.C. Trends in surgical management of proximal humeral fractures in the Medicare population: a nationwide study of records from 2009 to 2012. J Shoulder Elbow Surg. 2016;25:608–613. doi: 10.1016/j.jse.2015.08.011. [DOI] [PubMed] [Google Scholar]
- 22.Ross B.J., Wu V.J., McCluskey L.C., O’Brien M.J., Sherman W.F., Savoie F.H. Postoperative complication rates following total shoulder arthroplasty (TSA) vs. reverse shoulder arthroplasty (RSA): a nationwide analysis. Semin Arthroplasty. 2020;30:83–88. doi: 10.1053/j.sart.2020.05.006. [DOI] [Google Scholar]
- 23.Rugg C.M., Coughlan M.J., Lansdown D.A. Reverse total shoulder arthroplasty: Biomechanics and Indications. Curr Rev Musculoskelet Med. 2019;12:542–553. doi: 10.1007/s12178-019-09586-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schliemann B., Siemoneit J., Theisen C., Kösters C., Weimann A., Raschke M.J. Complex fractures of the proximal humerus in the elderly--outcome and complications after locking plate fixation. Musculoskelet Surg. 2012;96:S3–S11. doi: 10.1007/s12306-012-0181-8. [DOI] [PubMed] [Google Scholar]
- 25.Shannon S.F., Wagner E.R., Houdek M.T., Cross W.W., Sánchez-Sotelo J. Reverse shoulder arthroplasty for proximal humeral fractures: outcomes comparing primary reverse arthroplasty for fracture versus reverse arthroplasty after failed osteosynthesis. J Shoulder Elbow Surg. 2016;25:1655–1660. doi: 10.1016/j.jse.2016.02.012. [DOI] [PubMed] [Google Scholar]
- 26.Spross C., Meester J., Mazzucchelli R.A., Puskás G.J., Zdravkovic V., Jost B. Evidence-based algorithm to treat patients with proximal humerus fractures—a prospective study with early clinical and overall performance results. J Shoulder Elbow Surg. 2019;28:1022–1032. doi: 10.1016/j.jse.2019.02.015. [DOI] [PubMed] [Google Scholar]
- 27.Sumrein B.O., Huttunen T.T., Launonen A.P., Berg H.E., Felländer-Tsai L., Mattila V.M. Proximal humeral fractures in Sweden—a registry-based study. Osteoporos Int. 2017;28:901–907. doi: 10.1007/s00198-016-3808-z. [DOI] [PubMed] [Google Scholar]
- 28.Woolf S.H., Schoomaker H. Life expectancy and Mortality rates in the United States, 1959-2017. JAMA. 2019;322:1996–2016. doi: 10.1001/jama.2019.16932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.2019 Medicare fee-for-service supplemental improper payment data. CMS; 2019. https://www.cms.gov/research-statistics-data-and-systemsmonitoring-programsmedicare-ffs-compliance-programscertcert/2019-medicare-fee-service-supplemental-improper-payment-data Available at: Accessed August 17, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.