Abstract
Background
Four-dimensional computed tomography (4D CT) is rapidly emerging as a diagnostic tool for the investigation of dynamic upper limb disorders. Dynamic elbow pathologies are challenging to diagnose, and at present, limitations exist in current imaging modalities
Objective
We aimed to assess the clinical utility of 4D CT in detecting potential dynamic elbow disorders.
Methods
Twenty-eight elbow joints from 26 patients with symptoms of dynamic elbow pathology were included in this study. They were first assessed by a senior orthopedic surgeon with subsequent qualitative data obtained via a Siemens Force Dual Source CT scanner (Erlangen, Germany), producing two- and three-dimensional “static” images and 4D dynamic “movie” images for assessment in each clinical scenario. Clinical assessment before and after scan was compared.
Results
Use of 4D CT scan resulted in a change of diagnosis in 16 cases (57.14%). This included a change in primary diagnosis in 2 cases (7.14%) and secondary diagnosis in 14 cases (50%). In 25 cases (89.29%), the 4D CT scan allowed us to understand the pathological anatomy in greater detail which led to a change in the management plan of 15 cases (53.57%).
Conclusion
4D CT is a promising diagnostic tool in the management of dynamic elbow disorders and may be considered in clinical practice. Future studies need to compare it with other diagnostic modalities such as three-dimensional CT.
Keywords: 4D CT, Four-dimensional computed tomography, Dynamic CT, Dynamic elbow disorders, Elbow instability
Dynamic elbow pathologies are diagnosed clinically and can be challenging to manage. Diagnosis requires a thorough history and detailed clinical examination of the affected joints. Further imaging with plain radiographs and a computed tomography (CT) help delineate bony anatomical deficiencies and may show indirect signs of ligament injuries like calcifications of the ligaments. Magnetic resonance imaging helps detect ligament tears, tendon pathology, and cartilage damage and assist with surgical planning.8,25 However, at present, limitations exist in current imaging techniques as images produced are static. Subtle dynamic pathologies are potentially missed, and this may result in inadequate management of dynamic elbow conditions, resulting in poor outcomes after surgery.16 In an increasingly challenging medical environment where meeting patients’ expectations is paramount, combined with pathology in a complex joint where a diagnosis can be difficult, the availability of a dynamic imaging modality can be useful in treating dynamic elbow disorders.14,23
The emergence and refinement of four-dimensional CT (4D CT) in the past two decades, where three-dimensional (3D) images of a moving object are recorded over time (fourth dimension), have led to its increasing use in both research and clinical practice.10,11,26 Its initial use was largely confined to the management of parathyroid, cardiac, thoracic, and gastrointestinal pathologies.13 In recent times, its use has been extended in the diagnosis and understanding of dynamic joint disorders, specifically of the upper limb. A great promise has been shown using 4D CT in diagnosing and treating coracoacromial disorders, snapping scapula syndrome, and carpal bone disorders.1,4,11 A recent study also indicated that the use of 4D CT significantly influenced interpretation, clinical diagnosis, and the surgical treatment of dynamic wrist conditions.6 Recent advances have enabled the processing of these large-volume data sets into two-dimensional, 3D, and 4D formats, producing both static images and dynamic ‘movie’ series. Images are of high quality with good spatial and temporal resolution. Most importantly, this was performed without the need for increased radiation exposure to the patient.7
This study is an extension of our work using 4D CT in wrist conditions, where it was noted to be significantly beneficial in assisting us in understanding pathology and in directing appropriate treatment. We conducted a retrospective analysis of our use of 4D CT in aiding our management of dynamic elbow conditions. Here, we present a summary of the cases of which 4D CT was used and how it influenced our decision-making with regard to the final diagnosis and surgical treatment.
Materials and methods
This study is a retrospective analysis of patients who have undergone 4D CT scans of the elbow joint for various pathologies between 2015 and 2019. The indication for the 4D CT scan was to assess patients who had dynamic conditions of the elbow. This included patients with pain on specific joint motion, clicking and locking symptoms, congenital disorders with instability, suspected impingement, and dynamic instability. Ethics committee approval was obtained to review the scans performed on adults, ≥18 years.
Technique
The scanner used was a Siemens Force Dual Source CT (Erlangen, Germany). The patient practiced the elbow motions before starting the CT scan and was also later guided verbally during the scanning process. The patient was first positioned lying prone or decubitus with the affected arm extended and the elbow joint centered in the gantry. The elbow was supported by sandbags to reduce motion artifact. The table was centered to the elbow joint, identified via a preliminary topogram, with the volume range set to 5.8 cm to ensure that no table movement was required. Slice thickness and interval were set to 0.6 mm and 0.5 mm, respectively (Fig. 1).
Figure 1.
Patient position on the scanner table for 4D CT of the elbow. (A) Elbow position on the scanner table to correspond to the triangle imprint. (B) Position of the elbow through the scanner. (C) Position of the elbow from the side view. 4D CT, four-dimensional computed tomography.
After completion of the topogram, the radiographer stood behind a lead glass window, wearing a lead apron and thyroid shield and verbally guided the patient through the movements during dynamic image acquisition. The scanning protocol included flexion-extension, pronation supination in extension, and pronation supination at flexion 45°. The settings were 80 kV tube voltage, 0.25 s gantry rotation time, 90 mA current, and continuous x-ray. The total scan time for each full motion cycle was set at a mean of 15 seconds. We performed one full motion cycle in each case to reduce radiation exposure. The radiographer monitoring the patient movements allowed the scan to be stopped and started on demand as each movement was completed. Data were reconstructed for each dynamic image at 0.25-second intervals, which resulted in 40 to 72 data volumes per movement.
Volume data were reconstructed using Siemens software with 0.6-mm thickness and 0.5-mm interval between images, using both bone and soft tissue algorithms. Soft tissue reconstructions were used to produce the 4D dynamic 3D images. Bone reconstructions were used to produce 4D dynamic thick and thin multiplanar reformat images. A musculoskeletal consultant radiologist reviewed the images and produced a radiological report.
Patient details including age, gender, and clinical diagnosis were recorded. A senior orthopedic surgeon and a musculoskeletal radiologist reviewed the findings from the 4D CT scans, and a diagnosis was made. Images were assessed in various views such as anterior, medial or lateral, posterior, oblique, and axial to ensure subtle movements in any direction were not missed. Prescan and postscan diagnoses were then compared. This included the primary diagnosis (eg osteoarthritis [OA], posterolateral rotatory instability) and secondary diagnosis (eg impinging coronoid osteophytes and loose bodies). We also analyzed if the 4D CT scan findings changed the interpretation and management plan. Radiation doses were collected and monitored.
Radiation exposure is calculated by using the recorded dose length product and multiplying this with the organ-specific conversion factor. In the case of the wrist, a conversion factor of 0.0008 is used. This product is then termed the effective dose (mSv). This corresponds with an effective radiation exposure of 1.13 mSv per scan, which compares with the 0.06 mSv for the effective radiation dose of a 3D CT scan of the wrist. For reference, environmental background radiation is 2 mSv annually, and so a patient undergoing a 4D CT receives the equivalent of less than a year of background radiation. This dose is lesser than many diagnostic x-ray and nuclear medicine procedures. No harmful effects of radiation have been demonstrated at this dose level because any effect is too small to be measured and the risk is believed to be low
Results
There were 28 elbows in 26 patients included in this study. Majority of the patients were male (n = 18/26, 69.2%). Elbow pathologies and clinical indications identified include OA and its specific impinging loose body or osteophyte, radial tuberosity impingement and instability, implant impingement leading to loss of range of movement (ROM), hemimelia with global instability, and osteochondritis dissecans. Table I highlights the individual cases in which 4D CT was used and how it affected the diagnosis, interpretation, and management of each condition.
Table I.
Clinical findings on 4D CT of the elbow.
| Elbow |
Diagnosis |
Value of 4D CT scan |
||||
|---|---|---|---|---|---|---|
| Age, sex | Before 4D CT | After 4D CT | Diagnosis | Interpretation | Management | |
| 1 | 75, M | Post capitellum ORIF. ?PLRI | Healed fracture with PLRI | + | + | + |
| 2 | 42, M | Subacute coronoid + radial head#. ?Fragment mobility | Healing fractures. No mobility | + | + | + |
| 3 | 44, M | Recent dislocation. ?PLRI | Stable elbow | + | + | + |
| 4 | 29, M | ?PLRI | Stable elbow | + | + | + |
| 5 | 19, M | OCD + loose body | OCD + loose body | - | - | - |
| 6 | 28, F | ?PLRI | Stable elbow | + | + | + |
| 7 | 48, M | Pain and clicking. Malunited radial head fracture | Clicking from loose body | ++ | + | + |
| 8 | 42, F | ORIF radial head. ?Implant impingement | Implant impingement confirmed | + | + | + |
| 9 | 20, M | Hemimelia +/- PLRI | Hemimelia + global instability | ++ | + | + |
| 10 | 48, M | Early OA | Normal joint | + | + | + |
| 11 | 47, F | Post radial head excision. ?Bony impingement | Radial tuberosity impingement and scar tissue | + | + | + |
| 12 | 68, F | Bicipital tendinitis vs. impingement | Bicipital tendinitis. Early OA. | + | + | + |
| 13 | 62, M | ? Radial head instability. Previous distal biceps repair | Stable joint | + | + | + |
| 14 | 57, M | Bicipital impingement | Biceps tendinitis | + | + | + |
| 15 | 57, F | Bicipital impingement | Bicipital impingement, osteophyte | + | + | - |
| 16 | 84, M | Bicipital impingement | No impingement. Partial biceps tear | + | + | + |
| 17 | 57, M | Bicipital tendinitis. ?impingement | Bicipital tendinitis, partial tear. No impingement | + | + | + |
| 18 | 69, M | Pain. ?OA | Bicipital tendinitis | ++ | + | + |
| 19 | 77, F | Bicipital tendinitis + radial tuberosity impingement | Bicipital tendinitis, partial tear + radial tuberosity impingement | + | + | + |
| 20 | 57, M | Bicipital impingement | Biceps tendinitis | + | + | + |
| 21 | 48, M | Pain after distal biceps repair. ?Tuberosity impingement | Biceps tendinitis | + | + | + |
| 22 | 69, M | Pain. ?OA | Bicipital tendinitis | ++ | + | + |
| 23 | 71, M | OA + radial head implant loosening | OA + radial head implant loosening | - | + | - |
| 24 | 56, M | OA + loose bodies | OA + loose bodies | - | - | - |
| 25 | 48, M | OA + ulnar neuritis + stiffness | OA + impinging osteophytes | - | + | - |
| 26 | 72, M | OA + loose bodies | OA + loose bodies, osteophytes | - | + | - |
| 27 | 77, M | OA | OA + RC instability | + | + | + |
| 28 | 25, M | OA + stiffness | OA + impinging osteophytes | - | + | - |
| 29 | 55, M | OA + loose body | OA + impinging osteophyte | + | + | + |
| 30 | 77, M | OA | OA + RC instability | + | + | + |
| 31 | 72, F | OA | OA | - | - | - |
| 32 | 55, M | OA + clicking + loose bodies | OA. Loose bodies not engaging | + | + | + |
| 33 | 44, F | OA + instability. | OA + instability | - | + | - |
| 34 | 74, M | OA + ulna neuritis | OA + instability + ulna neuritis | + | + | + |
| 35 | 71, F | OA + instability, | OA + instability | - | + | - |
4D CT, four-dimensional computed tomography; PLRI, posterolateral rotatory instability; OA, osteoarthritis; RC, radiocapitellar; OCD, osteochondritis dessicans.
Note: Changes in the primary (++) and secondary (+) diagnosis.
Use of 4D CT scan resulted in a change of diagnosis in 16 cases (57.14%). This included a change in primary diagnosis in 2 cases (7.14%) and secondary diagnosis in 14 cases (50%). In 25 cases (89.29%), the 4D CT scan allowed us to understand the pathological anatomy in greater detail which led to a change in the management plan of 15 cases (53.57%).
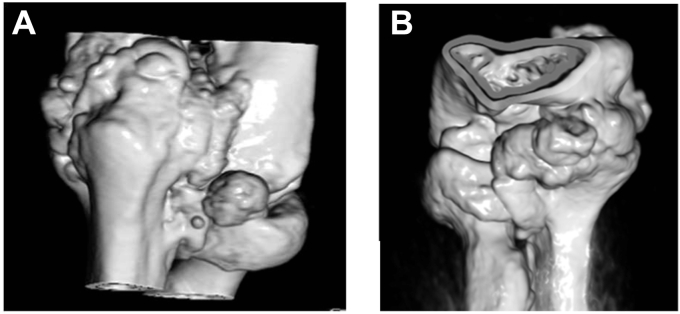
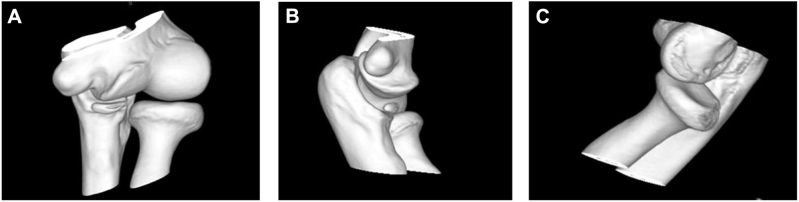
In a subgroup analysis, we noticed that in patients with distal biceps pathology (Fig. 2 and Video 1) and primary elbow OA (Fig. 3 and Video 2), 4D CT was of value. In most cases of distal biceps pathology, there was a change in the management plan after the 4D CT. There were 3 of 9 elbows (33.3%) with primary OA which had radio capitellar OA with loss of joint space. This was associated with anterior subluxation of the radial head, accentuated in pronation in all 3 cases.
Figure 2.
The patient presents with anterior elbow pain and clicking. 4D CT showed radial tuberosity impingement when the forearm moves from (A) supination to (B) pronation. 4D CT, four-dimensional computed tomography.
Figure 3.
The patient with osteoarthritis showing (A) osteophyte impingement and (B) loose body impingement.
The mean effective radiation dose was 1.54 mSev (range: 1.0-2.3).
Discussion
Management of dynamic elbow pathologies is challenging, and this is not aided by limitations present in current modalities of imaging, which produce mainly static images. Our study has shown that current methods of obtaining a diagnosis may be inadequate, especially if the changes are subtle. 4D CT enabled us to have a better understanding of how the proximal radius, ulna, and distal humerus interact in each clinical pathology, by analyzing the multiple static and dynamic images obtained as the joint moved throughout its range of motion. The types of cases that we found 4D CT to be useful included the following: (1) post–elbow dislocation in the young active patient who had some residual instability symptoms at four weeks, (2) distal biceps pathology with suspected dynamic instability and radial tuberosity impingement, (3) OA with loose bodies and impinging osteophytes, (4) complex elbow disorders like hemimelia, and (5) suspected implant impingement in patients with a decreased ROM after surgery. 4D CT aided our clinical decision-making, with regard to both final diagnoses, primary and/or secondary, and subsequent surgical management.
Elbow dislocations are common, with simple elbow dislocations comprising up to 75% of cases. These are usually managed conservatively with good outcomes although a small group may develop chronic instability. Conservative management varies with individual surgeons, but most allow early mobilization with some limitation of activities for 6 weeks.25 This is accepted by most patients, but in those with high functional demand, such as athletes and manual laborers, earlier decision-making with regard to potential surgery may be required.21 A 4D CT can help with this decision-making because of its ability to detect small bony displacements during a normal ROM and with provocation. In our patient who was an avid rugby player and sustained a simple dislocation of the elbow, we performed a 4D CT at 4 weeks as he still reported mild instability symptoms. A normal 4D CT, with the addition of provocation, allowed us to discharge him from follow-up with just clinical advice and reassurance, minimizing loss of work hours.
Distal biceps tendinosis, impingement, and partial tears are uncommon clinical conditions that are inter-related but with different approaches to management, reinforcing the need for an accurate diagnosis of the pathology. Distal biceps tendinosis tends to be managed nonsurgically with good outcomes, whereas tears are managed surgically to good effect.2,3 Distal biceps impingement is usually managed surgically if symptoms are persistent and osteophytes engage and block the ROM. There may be a benefit in the early surgical management of these patients as osteophytes at the radial tuberosity potentially contribute to tendon rupture or instability, especially if they engage the proximal ulna.22 Current imaging modalities may be inadequate as they are unable to objectively identify the point of osteophyte engagement in a full joint motion cycle in real time and if any instability results from this impingement. Using a 4D CT in 10 cases of distal biceps pathology, we were able to clearly differentiate between pathologies and adjust management to good effect. A 4D CT allowed us to identify osteophyte location, presence of impingement, which position of the forearm resulted in impingement, and if corresponding radial head subluxation occurred. In one case with stiffness after distal biceps repair, we were able to rule out confidently that implant placement was not responsible for stiffness post-op and the patient was managed with physiotherapy with a good subsequent outcome.
This dynamic scan has also assisted us in understanding pathologies that are not well understood. Primary elbow OA is uncommon, and some patients occasionally report symptoms of clicking and mild instability.20 All nine elbow joints with OA analyzed had radio capitellar osteophytes at the radial head, capitellum, or both in varying extents. However, only three of these elbow joints had advanced radio capitellar OA with loss of joint space. These three joints also exhibited an anterior subluxation of the radial head, accentuated with pronation. These observations are consistent with the findings of Miyake et al which showed a significant change in joint kinematics in elbows with radio capitellar OA compared with those without.18 This change in joint kinematics and radial head subluxation noted on a 4D CT could potentially be an additional cause of a patient’s symptoms of clicking and/or instability. In these patients, an isolated joint débridement, arthroscopic or open, may not be sufficient in relieving their symptoms, and it may explain why some patients remain dissatisfied after débridement surgery.16
A comprehensive débridement of the offending osteophytes and loose bodies in elbow OA has been shown to improve patient outcomes. This is only possible with an accurate preoperative imaging and surgical planning, of which 4D images can assist in. Yamamoto et al combined 3D CT images with computational software to create preoperative 4D simulation ‘movies’ for surgical planning and noted a significant improvement in pain, range of motion, and patient satisfaction postoperatively.27 In a patient with a malunited distal humerus, resulting in a block to both extension and flexion, Goh et al reported the benefits of using 4D CT preoperatively for surgical planning.9
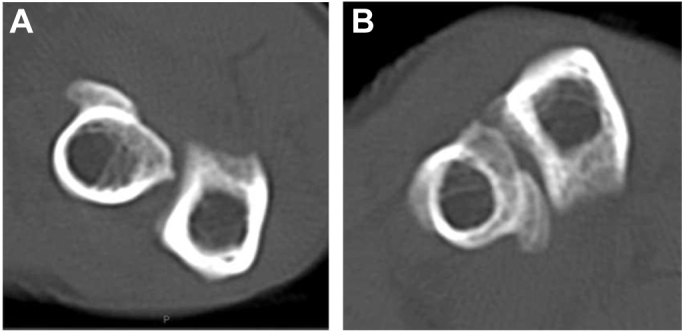
In complex congenital disorders like hemimelia, pathology can be multifactorial. 4D CT was performed in a single patient with this condition (Fig. 4). The information acquired from the 4D CT, combined with our detailed history and examination, allowed us to have a comprehensive discussion of the pathology with the patient, allowing him to make an informed decision with regard to management. This is increasingly important in today’s modern practice as patients have a wealth of information available to them on the internet, are more educated, and have higher expectations with regard to personal involvement in their care.23
Figure 4.
The patient with hemimelia with (A) hypoplastic trochlear and proximal una. (B) Ulnohumeral instability on extension. (C) Radial head subluxation on supination.
The 3D CT and 4D CT are catch-all terms with complex definitions. These are synthetic and selective representations of morphological and functional information obtained from one or more data acquisitions and sourced from one or more imaging modalities from the whole of a studied volume.5 These imaging techniques aim to simplify and improve the analysis of complex information for diagnostic or therapeutic purposes.24 The 3D can correspond to time or to a parameter in 3D Euclidean space, whereas 4D corresponds to the evolution of a volume of interest over time.19 Determination of the anatomical affected area that causes symptoms may guide the surgeon to the location for arthroscopic management. The current imaging methods to evaluate this include ultrasound, plain radiographs, magnetic resonance imaging, CT, and 3D CT scans. These imaging modalities are typically unable to accurately quantify the dynamic affected area although the 3D CT scan can accurately determine the anatomical abnormalities.17 With the recent development of the 4D CT, producing 3D CT images that demonstrate movement in real time (4D CT) is now possible.4 A 4D CT scan is a promising technique because it not only determines the dynamic aspects but also provides static images in two-dimensional, and 3D, of the underlying anatomy. However, future studies need to compare it with other diagnostic modalities such as 3D CT to confirm its accuracy.
The use of 4D CT had its challenges during the scanning process. Concerns are present about the radiation dose, but accurate 3D kinematics can be calculated using dynamic CT using a conventional CT with a limited radiation dose.12,15 When performing elbow maneuvers, patients had to be briefed before the scan. They were also required to practice following commands before the scan was performed to ensure it could be performed in a single setting. The speed of motion was also crucial as movements that were too quick or slow would result in motion artifacts or a loss of images, respectively. Loss of images would occur as the movements exceeded the scanner acquisition time. This was time-consuming, and fewer patients could undergo imaging at any period. Co-ordination of scans with the radiology staff and donning of radiation protection gowns also resulted in delays. Performing provocative maneuvers was also a challenge because of a confined space and discomfort experienced by patients. Finally, access to experienced radiologists is also a limitation as most are not familiar with this imaging modality.
Conclusion
Despite the challenges encountered, 4D CT has been shown to be a useful adjunct in the diagnosis and assessment of dynamic elbow disorders. It can provide important information with regard to functional anatomy and its resultant disease progression, and its use in routine clinical practice may be considered. Future studies need to conduct a cost analysis and compare it with other diagnostic modalities such as 3D CT.
Disclaimers
Funding: No funding was disclosed by the authors.
Conflicts of interest: The authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Ethics approval was received from the Southern Adelaide Clinical Human Research Ethics Committee.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jseint.2021.09.013.
Supplementary data
4D CT showing radial tuberosity impingement as the patient moves from supination to pronation.
4D CT showing anterior radial head subluxation, accentuated with pronation in a patient with osteoarthritis and radio-capitellar joint space loss.
References
- 1.Alta T.D., Bell S.N., Troupis J.M., Coghlan J.A., Miller D. The new 4-dimensional computed tomographic scanner allows dynamic visualization and measurement of normal acromioclavicular joint motion in an unloaded and loaded condition. J Comput Assisted Tomogr. 2012;36:749–754. doi: 10.1097/RCT.0b013e31826dbc50. [DOI] [PubMed] [Google Scholar]
- 2.Bain G.I., Johnson L.J., Turner P.C. Treatment of partial distal biceps tendon tears. Sports Med Arth Rev. 2008;16:154–161. doi: 10.1097/JSA.0b013e318183eb60. [DOI] [PubMed] [Google Scholar]
- 3.Barker S.L., Bell S.N., Connell D., Coghlan J.A. Ultrasound-guided platelet-rich plasma injection for distal biceps tendinopathy. Shoulder & Elbow. 2015;7:110–114. doi: 10.1177/1758573214567558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bell S.N., Troupis J.M., Miller D., Alta T.D., Coghlan J.A., Wijeratna M.D. Four-dimensional computed tomography scans facilitate preoperative planning in snapping scapula syndrome. J Shoulder Elbow Surg. 2015;24:e83–e90. doi: 10.1016/j.jse.2014.09.020. [DOI] [PubMed] [Google Scholar]
- 5.Calhoun P.S., Kuszyk B.S., Heath D.G., Carley J.C., Fishman E.K. Three-dimensional volume rendering of spiral CT data: theory and method. Radiographics. 1999;19:745–764. doi: 10.1148/radiographics.19.3.g99ma14745. [DOI] [PubMed] [Google Scholar]
- 6.Carr R., MacLean S., Slavotinek J., Bain G.I. Four-dimensional computed tomography scanning for dynamic wrist disorders: prospective analysis and recommendations for clinical utility. J Wrist Surg. 2019;8:161. doi: 10.1055/s-0038-1675564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Choi Y.S., Lee Y.H., Kim S., Cho H.W., Song H.-T., Suh J.-S. Four-dimensional real-time cine images of wrist joint kinematics using dual source CT with minimal time increment scanning. Yonsei Med J. 2013;54:1026–1032. doi: 10.3349/ymj.2013.54.4.1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Conti Mica M., Caekebeke P., van Riet R. Lateral collateral ligament injuries of the elbow–chronic posterolateral rotatory instability (PLRI) EFORT Open Rev. 2016;1:461–468. doi: 10.1302/2058-5241.160033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goh Y.P., Lau K.K. Using the 320-multidetector computed tomography scanner for four-dimensional functional assessment of the elbow joint. Am J Orthop. 2012;41:E20–E24. [PubMed] [Google Scholar]
- 10.Gondim Teixeira P.A., Formery A.-S., Jacquot A., Lux G., Loiret I., Perez M., et al. Quantitative analysis of subtalar joint motion with 4D CT: proof of concept with cadaveric and healthy subject evaluation. Am J Roentgenol. 2017;208:150–158. doi: 10.2214/AJR.16.16434. [DOI] [PubMed] [Google Scholar]
- 11.Kakar S., Breighner R.E., Leng S., McCollough C.H., Moran S.L., Berger R.A., et al. The role of dynamic (4D) CT in the detection of scapholunate ligament injury. J wrist Surg. 2016;5:306. doi: 10.1055/s-0035-1570463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kerkhof F., Brugman E., D’Agostino P., Dourthe B., van Lenthe G., Stockmans F., et al. Quantifying thumb opposition kinematics using dynamic computed tomography. J Biomech. 2016;49:1994–1999. doi: 10.1016/j.jbiomech.2016.05.008. [DOI] [PubMed] [Google Scholar]
- 13.Kwong Y., Mel A.O., Wheeler G., Troupis J.M. F our-dimensional computed tomography (4DCT): a review of the current status and applications. J Med Imaging Radiat Oncol. 2015;59:545–554. doi: 10.1111/1754-9485.12326. [DOI] [PubMed] [Google Scholar]
- 14.Lalone E., Giles J., Alolabi B., Peters T., Johnson J., King G. Utility of an image-based technique to detect changes in joint congruency following simulated joint injury and repair: an in vitro study of the elbow. J Biomech. 2013;46:677–682. doi: 10.1016/j.jbiomech.2012.11.047. [DOI] [PubMed] [Google Scholar]
- 15.Leng S., Zhao K., Qu M., An K.N., Berger R., McCollough C.H. Dynamic CT technique for assessment of wrist joint instabilities. Med Phys. 2011;38:S50–S56. doi: 10.1118/1.3577759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lim T.K., Koh K.H., Lee H.I., Shim J.W., Park M.J. Arthroscopic débridement for primary osteoarthritis of the elbow: analysis of preoperative factors affecting outcome. J Shoulder Elbow Surg. 2014;23:1381–1387. doi: 10.1016/j.jse.2014.01.009. [DOI] [PubMed] [Google Scholar]
- 17.Milch H. Snapping scapula. Clin Orthopaedics Relat Res. 1961;20:140–150. [PubMed] [Google Scholar]
- 18.Miyake J., Shimada K., Moritomo H., Kataoka T., Murase T., Sugamoto K. Kinematic changes in elbow osteoarthritis: in vivo and 3-dimensional analysis using computed tomographic data. J Hand Surg. 2013;38:957–964. doi: 10.1016/j.jhsa.2013.02.006. [DOI] [PubMed] [Google Scholar]
- 19.Rauch A., Arab W.A., Dap F., Dautel G., Blum A., Gondim Teixeira P.A. Four-dimensional CT analysis of wrist kinematics during radioulnar deviation. Radiology. 2018;289:750–758. doi: 10.1148/radiol.2018180640. [DOI] [PubMed] [Google Scholar]
- 20.Ravalli S., Pulici C., Binetti S., Aglieco A., Vecchio M., Musumeci G. An overview of the pathogenesis and treatment of elbow osteoarthritis. J Funct Morphol Kinesiol. 2019;4:30. doi: 10.3390/jfmk4020030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Savoie F.H., III, Trenhaile S.W., Roberts J., Field L.D., Ramsey J.R. Primary repair of ulnar collateral ligament injuries of the elbow in young athletes: a case series of injuries to the proximal and distal ends of the ligament. Am J Sports Med. 2008;36:1066–1072. doi: 10.1177/0363546508315201. [DOI] [PubMed] [Google Scholar]
- 22.Seiler J.G., III, Parker L.M., Chamberland P.D., Sherbourne G.M., Carpenter W.A. The distal biceps tendon: two potential mechanisms involved in its rupture: arterial supply and mechanical impingement. J Shoulder Elbow Surg. 1995;4:149–156. doi: 10.1016/s1058-2746(05)80044-8. [DOI] [PubMed] [Google Scholar]
- 23.Skär L., Söderberg S. Patients’ complaints regarding healthcare encounters and communication. Nurs open. 2018;5:224–232. doi: 10.1002/nop2.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Teixeira P.A.G., Gervaise A., Louis M., Raymond A., Formery A.-S., Lecocq S., et al. Musculoskeletal wide-detector CT kinematic evaluation: from motion to image. Semin Musculoskelet Radiol. 2015;19:456–462. doi: 10.1055/s-0035-1569257. [DOI] [PubMed] [Google Scholar]
- 25.van Riet R.P. Assessment and decision making in the unstable elbow: management of simple dislocations. Shoulder & Elbow. 2017;9:136–143. doi: 10.1177/1758573216686533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wassilew G.I., Janz V., Heller M.O., Tohtz S., Rogalla P., Hein P., et al. Real time visualization of femoroacetabular impingement and subluxation using 320-slice computed tomography. J Orth Res. 2013;31:275–281. doi: 10.1002/jor.22224. [DOI] [PubMed] [Google Scholar]
- 27.Yamamoto M., Murakami Y., Iwatsuki K., Kurimoto S., Hirata H. Feasibility of four-dimensional preoperative simulation for elbow debridement arthroplasty. BMC Musculoskel Disord. 2016;17:1–7. doi: 10.1186/s12891-016-0996-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
4D CT showing radial tuberosity impingement as the patient moves from supination to pronation.
4D CT showing anterior radial head subluxation, accentuated with pronation in a patient with osteoarthritis and radio-capitellar joint space loss.