Abstract
This study was performed to describe a rare case of granulomatous lobular mastitis (GLM) that was successfully treated with bromocriptine in a male patient with gynecomastia and hyperprolactinemia. A 20-year-old man presented with a 1-year history of breast enlargement and galactorrhea. Physical examination revealed bilateral breast enlargement, porous discharge, and a 3-cm left breast lump in the 10-o’clock quadrant. Magnetic resonance imaging of the brain showed a 1.2-mm pituitary tumor. Laboratory analysis revealed hyperprolactinemia with low serum testosterone and elevated prolactin and estradiol levels. The lump in the left breast was examined by ultrasonography and mammography, and a core needle biopsy revealed chronic inflammation. The patient’s galactorrhea and breast lump disappeared after 3 months of treatment with bromocriptine at 2.5 mg once a day. His serum prolactin level also normalized. Following a review of this case, the patient was diagnosed with gynecomastia with hyperprolactinemia complicated by rare GLM. To the best of our knowledge, this is the first reported case of concurrent gynecomastia and GLM.
Keywords: Gynecomastia, hyperprolactinemia, granulomatous lobular mastitis, bromocriptine, case report, literature review
Introduction
Gynecomastia is a benign proliferation of glandular breast tissue in men. Among men with gynecomastia, approximately 70% develop pubertal gynecomastia and two-thirds develop palpable breast tissue.1,2 Gynecomastia is idiopathic in most adolescents and resolves spontaneously over 1 to 3 years in 75% to 90% of affected individuals. 3 The exact pathogenesis of gynecomastia is unknown, but it is thought to be caused by a relative or absolute lack of androgen action in breast tissue. 4 Chronic conditions such as cirrhosis, hypogonadism, and renal insufficiency; the use of supplements, medications, or dangerous drugs; and, in rare cases, tumors can all cause nonphysiologic gynecomastia. 5 Gynecomastia and secondary hypogonadism may be exacerbated by hyperprolactinemia. Granulomatous lobular mastitis (GLM) is a rare and benign inflammatory disease of the breast characterized by non-necrotizing granulomatous inflammation in the breast lobules and parenchyma. 6
This study was performed to report the first known case of gynecomastia and rare GLM caused by hyperprolactinemia. The patient’s symptoms disappeared after treatment with oral bromocriptine.
Case report
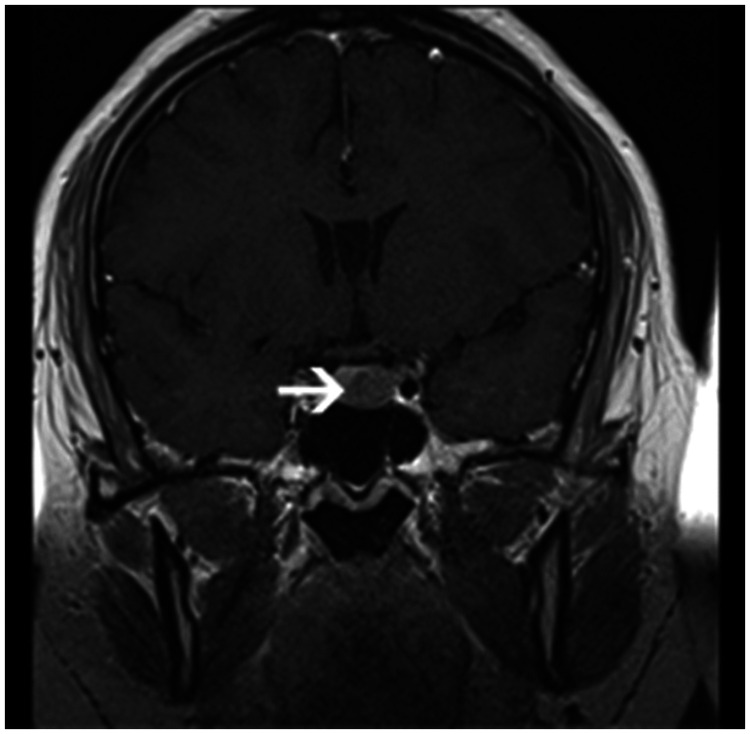
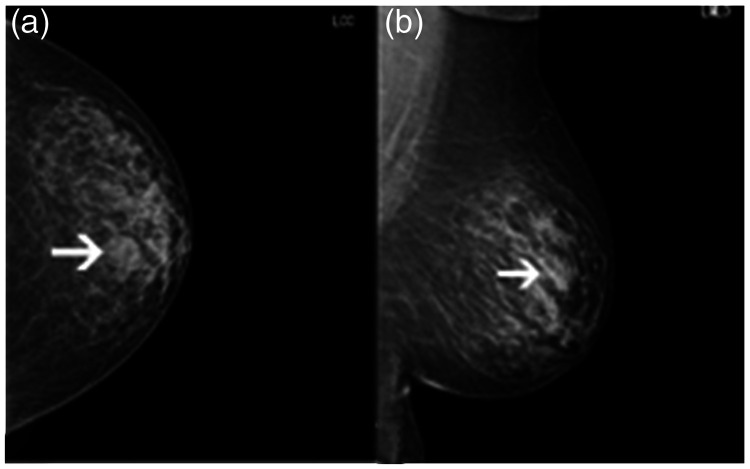
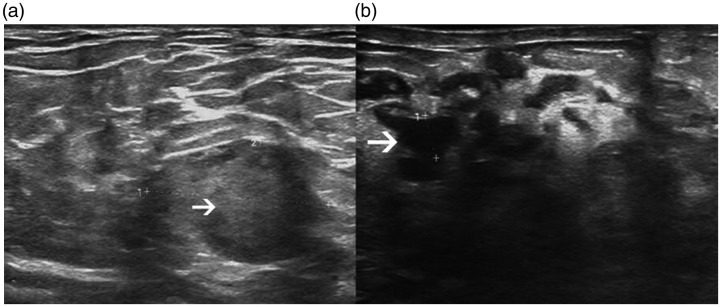
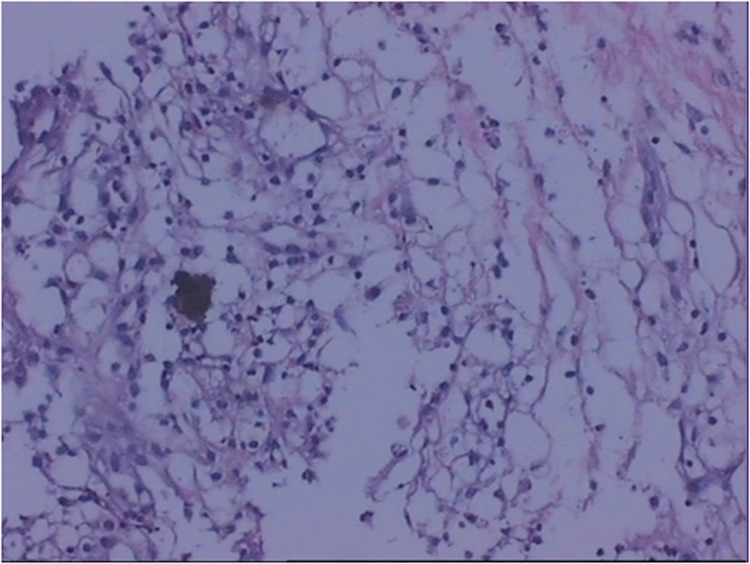
A 20-year-old man presented with a 1-year history of bilateral breast enlargement and galactorrhea. A general physical examination revealed bilateral breast enlargement with nipple discharge (Figure 1). A 3-cm-diameter left breast lump was present in the 10-o’clock quadrant. Magnetic resonance imaging revealed a left pituitary tumor measuring 12 × 10 mm with a low T1 and T2 signal. The tumor was well-enhanced after administration of contrast agent (Figure 2). Mammography revealed a round mass measuring approximately 26 × 20 mm in the upper quadrant of the left breast with a clear boundary and gynecomastia (Figure 3). Ultrasonography revealed a 26- × 17-mm hypoechoic mass with irregular borders in the left breast, as well as dilated bilateral breast ducts filled with cloudy fluid (Figure 4). Following a core needle biopsy, the left breast mass was diagnosed as GLM with partial acinar reaction (Figure 5). The patient had no relevant medical or psychiatric history.
Figure 1.
Bilateral breast enlargement with nipple discharge.
Figure 2.
Magnetic resonance image of a 12- × 10-mm left pituitary tumor with low T1 and T2 signal.
Figure 3.
Left mammography of a 26-mm-diameter clearly defined mass and gynecomastia. (a) Craniocaudal view. (b) Mediolateral oblique view.
Figure 4.
Ultrasound image of the breast. (a) Hypoechoic mass with irregular borders. (b) Breast duct dilation with cloudy fluid.
Figure 5.
Granulomatous structure consisting of lymphocytes and histiocytes accompanied by partial acinar reaction (200× magnification).
Hormone analysis revealed a high prolactin level, a high estradiol level, and a low testosterone level upon admission (Table 1). Thyroid function was normal. Both the bromocriptine inhibition test and metoclopramide excitation test were positive. The C-peptide release test suggested hyperinsulinemia. Color ultrasound examination of the thyroid, abdomen, and urinary tract showed no obvious abnormality. The patient was treated with bromocriptine at 2.5 mg once a day for 3 months. His serum prolactin level gradually decreased. After 3 months of follow-up, the patient’s left breast lump had disappeared, his other hormonal assays had returned to normal, and his serum prolactin level was 9.25 ng/mL. The reporting of this study follows the CARE guidelines. 7
Table 1.
Hormone levels in the present case.
| Hormone | Level | Reference range for men |
|---|---|---|
| Testosterone | 0.82 ng/mL↓ | 1.75–7.81 ng/mL |
| Progesterone | 0.24 | 0.10–0.84 ng/mL |
| Cortisol | 10.5 µg/dL | Morning: 6.7–22.6 µg/dLAfternoon: 58–403 µg/dL |
| Estradiol | 50.00 pg/mL | 20.00–47.00 pg/mL |
| Follicle-stimulating hormone | 0.20 mIU/mL | 1.27–12.96 mIU/mL |
| Luteinizing hormone | 0.20 mIU/mL | 1.24–8.62 mIU/mL |
| Prolactin | 165.60 ng/mL | 2.64–13.13 ng/mL |
Discussion
Gynecomastia is a common condition in the general population. In the vast majority of cases, gynecomastia is cosmetic and benign in nature and has no clinical significance. However, affected individuals may experience localized soreness and pain. Gynecomastia can be caused by a serious underlying illness or a medication, or it can be inherited.4,8 Glandular breast tissue proliferates when the estrogen-to-testosterone ratio in men is disrupted.
Gynecomastia is a physiologic or nonphysiologic condition that occurs when the estrogen-to-testosterone ratio in men is disrupted. 9 Gynecomastia is most likely caused by hyperprolactinemia, which suppresses gonadotropin-releasing hormone secretion, resulting in an imbalance of androgenic and estrogenic influences on breast tissue. 10 However, the patient described in the present report had a unique case of gynecomastia and hyperprolactinemia complicated by rare GLM. GLM is a rare, chronic inflammatory disease of the breast in women caused by a variety of infectious and noninfectious factors. GLM is frequently misdiagnosed as an inflammatory or malignant condition, necessitating a pathologic diagnosis to rule out cancer and other conditions such as an abscess, periductal mastitis, tuberculosis, and sarcoidosis. Histologically, GLM is distinguished by necrotizing chronic granulomatous lobulitis and abscess formation. 11 GLM is extremely rare in men; only 13 cases have been reported in the literature to date. 12
Gynecomastia was initially diagnosed in our patient. A lump was discovered in his left breast during the physical examination. Ultrasound examination suggested that the patient had breast cancer, and a core needle biopsy revealed chronic inflammation. Left pituitary tumor-induced hyperprolactinemia may be the cause of gynecomastia, resulting in hormone imbalance. No reports to date have described gynecomastia associated with GLM. With respect to the pathogenesis of this condition, the chronic inflammation around the duct lobules is thought to be caused by milk stasis. Because the clinical manifestations and imaging findings of gynecomastia and GLM are similar to those of breast cancer, a pathological biopsy is required to differentiate gynecomastia from breast cancer.
Ultrasound examination is occasionally requested to rule out a mass or to distinguish cancer from pseudogynecomastia or lipomastia, which is a focal accumulation of adipose tissue that is always bilateral and occurs in overweight adolescents.13,14 Lipomastia is defined as diffuse adipose tissue proliferation without the presence of fibroglandular tissue on ultrasound. 15 Unlike gynecomastia, no discrete mass is present and no distinct borders are visible. Physiological pubertal gynecomastia resolves spontaneously in most cases, so treatment is rarely required. However, if the gynecomastia is severe and persistent, pharmacological treatment or surgery may be required. 16
The primary treatment goal for this disease is resolution of the hyperprolactinemia. Bromocriptine is used to reduce the serum prolactin level, which aids in normalization of the sex hormone imbalance and milk stasis. After 3 months of follow-up, our patient’s serum prolactin level was normal, and the breast milk and breast lump had disappeared.
In summary, we have herein described the first known case of gynecomastia with hyperprolactinemia complicated by rare GLM, which usually affects women. This is the first report of this condition in a man.
Footnotes
Ethics and informed consent: The patient provided written permission for publication of this case report. The study was approved by the ethics committee of Jiangsu University Affiliated People’s Hospital (approval number: K-20210175-w).
Declaration of conflicting interest: The authors declare that there is no conflict of interest.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by a grant from the National Natural Science Foundation of China (81971629) and Research Project of Jiangsu Maternal and Child Health Association (FYX202004).
ORCID iD: Liang Yin https://orcid.org/0000-0003-3601-0983
References
- 1.Acharya SV. Clinical features, presentation and hormonal parameters in patients with pubertal gynecomastia. J Family Med Prim Care 2021; 10: 648–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carlson HE. Gynecomastia. N Engl J Med 1980; 303: 795–799. [DOI] [PubMed] [Google Scholar]
- 3.Fiorini A, Sepich M, Pontrelli M, et al. Adolescent gynecomastia due to minimal androgen resistance syndrome: a case report and literature review. Sex Dev 2020; 14: 21–26. [DOI] [PubMed] [Google Scholar]
- 4.Narula HS, Carlson HE. Gynaecomastia–pathophysiology, diagnosis and treatment. Nat Rev Endocrinol 2014; 10: 684–698. [DOI] [PubMed] [Google Scholar]
- 5.Dickson G. Gynecomastia. Am Fam Physician 2012; 85: 716–722. [PubMed] [Google Scholar]
- 6.Grover H, Grover SB, Goyal P, et al. Clinical and imaging features of idiopathic granulomatous mastitis – the diagnostic challenges and a brief review. Clin Imaging 2021; 69: 126–132. [DOI] [PubMed] [Google Scholar]
- 7.Gagnier JJ, Kienle G, Altman DG, et al. The CARE guidelines: consensus-based clinical case reporting guideline development. Headache 2013; 53: 1541–1547. [DOI] [PubMed] [Google Scholar]
- 8.Koch T, Bräuner EV, Busch AS, et al. Marked increase in incident gynecomastia: a 20-year national registry study, 1998 to 2017. J Clin Endocrinol Metab 2020; 105: dgaa440. [DOI] [PubMed] [Google Scholar]
- 9.Todorova ZP, Stefanova EM, Todorov IP. Causes and psychological impact of gynecomastia in boys and adolescents. Endokrynol Pol 2021; 72: 670–671. [DOI] [PubMed] [Google Scholar]
- 10.Galdiero M, Pivonello R, Grasso LFS, et al. Growth hormone, prolactin, and sexuality. J Endocrinol Invest 2012; 35: 782–794. [DOI] [PubMed] [Google Scholar]
- 11.Tang A, Dominguez DA, Edquilang JK, et al. Granulomatous mastitis: comparison of novel treatment of steroid injection and current management. J Surg Res 2020; 254: 300–305. [DOI] [PubMed] [Google Scholar]
- 12.Yaghan RJ, Ayoub NM, Shenawi HM, et al. Idiopathic granulomatous mastitis in the male population: a clinical analysis of 13 reported cases. Breast J 2020; 26: 1481–1482. [DOI] [PubMed] [Google Scholar]
- 13.Önder Ö, Azizova A, Durhan G, et al. Imaging findings and classification of the common and uncommon male breast diseases. Insights Imaging 2020; 11: 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leung AKC, Leung AAC. Gynecomastia in infants, children, and adolescents. Recent Pat Endocr Metab Immune Drug Discov 2017; 10: 127–137. [DOI] [PubMed] [Google Scholar]
- 15.Colucci PG, Cohen SA, Baad M, et al. Pediatric chest wall masses: spectrum of benign findings on ultrasound. Pediatr Radiol 2021. [DOI] [PubMed] [Google Scholar]
- 16.Lemaine V, Cayci C, Simmons PS, et al. Gynecomastia in adolescent males. Semin Plast Surg 2013; 27: 56–61. [DOI] [PMC free article] [PubMed] [Google Scholar]