Abstract
The purpose of this article is to identify gold standards of care for return to sport following athletic injury, investigate overlooked aspects of return to sport rehabilitation, and provide expert opinion regarding current practices. The article was written by performing a literature review, then providing editorial expert opinion regarding current standards of return to sport. We concluded, through literature review and expert consensus, that a three-pronged approach to return to sport is recommended for therapists. These three prongs are ROM, strength, and hop testing. Cardiovascular readiness and psychological readiness for return to sport must also be assessed.”
Introduction
There are many stages that an individual must pass through when contemplating return to sport. Return to sport should be viewed as a continuum through recovery with the aim of returning to peak performance.1 The individual must be able to complete a progression of categorical components of rehabilitation before being considered ready to return to their respective sport.
Early-Stage Rehabilitation
This includes areas such as range of motion (ROM), strength, and isokinetic testing. All of these components are quantitative in nature and should be comparable to the contralateral limb. Additionally, in some cases, when the contralateral limb cannot be used as a control (e.g., previous injury to that limb as well), normative values for the specific joint or muscle involved may be considered.
The first rehabilitative evaluation a clinician should consider is range of motion. Range of motion involves restoring the joint and associated musculoskeletal structures to their preinjury range of tolerable movement. The gold standard for measuring ROM is radiographic imaging; however, hand-held goniometry has also been reported to obtain measurements very close to that of radiography.2 There are published normative values for the majority of joints, and these values have been established with acceptable intraobserver and interobserver reliability.3 A common practical application of returning range of motion is for the patient to be at or above 85% of their range compared to the unaffected limb, or normative published values, prior to initiating a progressive resistance program. Figure 1 displays normative values for clinical reference.4
Fig 1.
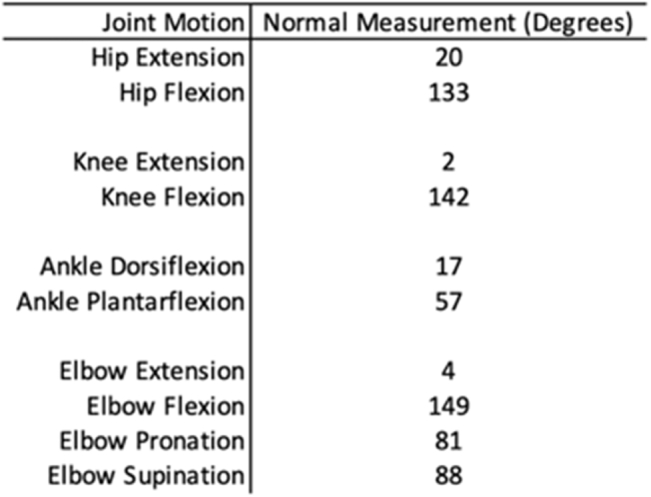
Normative values for clinical reference.
Strength is the next component of the rehabilitative process and is monitored through strength testing. Järvinen et al. reported that rehabilitation should begin with the immobilization of an injured muscle sufficient to build enough scar to minimize the chance of rerupture or injury. Following this period of immobilization, mobilization (strength) should be started gradually within the limits of pain. Early mobilization is needed to optimize recovery and strength of the injured skeletal muscle to preinjury levels.5
Finally, isokinetic testing is the third objective component of the rehabilitative process that a clinician should consider. Hickey et al. remarked that the addition of isokinetic testing as return to play (RTP) criteria may result in a more desirable balance between RTP times and rates of reinjury.6 Furthermore, isokinetic intervention can detect strength imbalances. Restoring a normal strength profile decreases the incidence of muscle reinjury.7 A major limiting factor to this component of rehabilitation is the lack of availability of isokinetic machines. In lieu of isokinetics, regular strength testing is widely accepted as a surrogate to track progress. Strength testing can be compared to baseline scores or unaffected limb scores (if available).
The single-leg hop test is a commonly used lower extremity return to play test and carries a large body of anecdotal support from clinicians around the world. Webster and Hewett8 noted that passing a RTS test battery (including single leg hop testing) significantly reduced the risk for subsequent graft rupture. However, recent literature has suggested that this test may not be the most effective in determining musculoskeletal readiness. In a 2019 study, no association was found between the single-leg hop test and knee extensor strength.9 This suggests the test should not be used in isolation to determine readiness to return.
Cardiovascular Fitness
Rehabilitation specialists should also evaluate cardiovascular fitness following a comprehensive mobility, strength, and movement screen as part of a well-coordinated program for athletes to return to sport (RTS). The demands of competitive sport entail that several criteria be met to return to sport safely while integrating stresses on the body without a breakdown in form. Although not specifically studied, evidence does support that an improvement in cardiovascular and metabolic capacity can lead to reduction in injury.10
Commonly administered test protocols should also be employed in determining return to play criteria. For example, the single-leg hop test is frequently used as part of clearance examinations for athletes to RTP following anterior cruciate ligament reconstruction (ACLR). Prior studies by Augustsson et al. show that the risk for injury in the lower extremities increases with muscular fatigue.11 Inferences can be made for risk of reinjury due to a breakdown in form and function of movement based on single-leg hop testing under fatigued states. Although there is limited research on the benefits of high-intensity interval training (HIIT) compared to alternative training protocols, research does show that training variables related to endurance, such as VO2max and oxygen consumption, improved to a greater extent than did other protocols.12 From these findings, we can infer HIIT helps to improve endurance for the athlete, which is important when considering injury is more likely to occur in a fatigued state. A positive benefit in favor of including HIIT training is that it leaves more time for training sport-specific drills.12
In 2010, Creighton et al. developed a three-step decision-based RTP model for an injury or illness that is specific to the individual practitioner making the RTP decision, called the Strategic Assessment of Risk and Risk Tolerance (StARRT) framework. This updated model breaks down the decision-making process into three parts: 1) the assessment of health risk, 2) the assessment of activity risk, and 3) the assessment of risk tolerance. Morrison et al. proposed this model to account for workload, as it is required in reconditioning and development of the energy systems required by individuals to RTS safely.13
Over the past decade, an increased focus has been placed on the implementation of high-intensity interval training (HIIT) as a component of athletic preparation or training. Interest in HIIT may have stemmed from its parallels to repeated-sprint ability (RSA) in team sports, whereby longer duration is spent in low-intensity bouts with short bursts of maximal efforts. Along with transferability of tasks, the benefits of HIIT include improved strength, power, and cardiovascular adaptation with decreased time spent training. This does, however, come at the expense of having increased injury rates when not properly integrated by coaches, trainers, or medical professionals.14
On the basis of the evidence, the authors of this article propose that HIIT be combined with sport-specific drills to improve endurance while decreasing fear of reinjury that will allow for a safer transition to play. We recommend the adoption of 1-to-3-minute bouts of all-out activity followed by 30-second to 1-minute recovery periods for a total of 20 to 30 minutes for the HIIT component. This may be integrated with sport-specific tasks to further minimize time and improve cardiovascular fitness. Further research is needed to understand workload and fatigue that is appropriate with testing and training to safely clear athletes for RTS.
Psychological Readiness
The third category of rehabilitation specialists should test and review in RTS following injury is psychological readiness for return to sport. Confidence, fear of movement, fear of reinjury, and fear of inferior performance can all play a role in increasing risk of injury. We believe that both being too fearful of reinjury, as well as overconfident can cause increased risk of reinjury. The prevailing thought process that we recommend is to ensure that athletes are building both physical and psychological resilience throughout the rehabilitation process to reduce fear-avoidance beliefs at discharge. As therapists, we must be aware of possible iatrogenic effects that create fear in our patients by overemphasizing risk of reinjury during the rehabilitation process.
The current literature emphasizes fear avoidance as a more likely and more deleterious problem than overconfidence, but it is important to keep in mind the “gladiator effect” when building up athlete resiliency. There are athletes that present with very low fear-avoidance or concern for their injury, and these athletes should be counseled differently than those that have high levels of fear avoidance. For those athletes with extremely low levels of fear, it is recommended that we ensure that they still respect the fact that they have undergone a surgical procedure or sustained an injury that needs rehabilitation. For those with high levels of fear, the focus should be more on reducing fear of movement/injury and, thus, an individualized approach is necessary.
Outcome measures to evaluate psychological readiness for RTS include, but are not limited to, the FABQ (fear avoidance belief questionnaire), the Tampa Scale for Kinesiophobia, KOOS (Knee Osteoarthritis Outcome Score) sport questionnaire, and the IKDC (International Knee Documentation Committee) questionnaire. Hart et al. used some of these outcome measures in a 2020 study regarding level of function after 1 year following ACLR.15 Their findings indicate that higher scores on the Tampa Scale (>37), higher KOOS-pain scale, and worse task-specific confidence were associated with poorer performance when returning to sport following ACLR. They also found that those with greater psychological readiness performed better on the hop-testing cluster tests. These results indicate the utility of using these outcome measures prior to hop testing. A case-control study found that a lower IKDC score, and higher Tampa-11 score (elevated fear) were associated with the delay or inability to return to sport 6 and 12 months after ACLR.16
Paterno et al. performed a prospective cohort study in 2018 examining outcomes following ACLR and the association between fear on functional testing and second ACL injury rates.17 The study found those that suffered a second ipsilateral ACL injury had a higher TSK-11 score and those with a TSK-11 score of 19 or greater were 13 times more likely to have a second ACL tear within 24 months of RTS. Additionally, odds ratios found that patients with higher TSK-11 (Tampa Scale) scores were 4 times more likely to report lower levels of activity, 7 times more likely to have <95% limb symmetry on hop testing, and 6 times more likely to have less than 90% quadriceps strength ratio. More studies have had similar results with Baez et al. finding in 2019 those with self-reported kinesiophobia were 17% less likely to return to sport.
In addition to studying return to play after ACL injury, other injuries have been studied as well. Fear of reinjury has been associated with reduced self-reported function and lower levels of physical activity after elbow injuries.18 Karlsson et al. in 2014 also found a significant negative correlation between kinesiophobia and all patient-reported outcomes, as well as activity level following Achilles' tendon rupture. While most RTS research has been focused and centered around the ACLR population, there is some emerging evidence on various injuries, which supports examining psychological readiness for RTS for all injuries.
Both kinesiophobia and pain catastrophizing have been shown to be effectively reduced while patients undergo physical therapy following ACLR.19 What we say and do with our patients can clearly have a positive effect on this realm of recovery. Kinesiophobia is a modifiable risk factor that physical therapists can both positively and negatively affect depending on how we communicate and care for our patients. We recommend using phrasing and terminology with patients that improves their self-efficacy, confidence, and resilience. Examples include: “let’s get your leg so strong it's bulletproof”, “involved leg”, or “I want you to feel confident enough that you don’t need my help anymore”. Terms or phrases that invoke fear, harm, or immobility should be avoided. Examples include: “massive tear”, “bad leg”, or “your shoulder will never be the same again”. We also recommend screening for and referring patients to psychotherapy, as needed, if it is determined that there is psychological intervention needed beyond our scope. It is important to remember to work as an interdisciplinary team that treats the injured athlete with physical therapy and athletic training, and refers providers to ensure patients are well cared for. Patients see their therapist more frequently and for longer time periods postinjury than they see their referring doctors, so providing consistent and effective feedback with referring providers ensures continuity of care and improves outcomes.
Summary
Current postoperative protocols focus on resolving physical impairments, specifically strength and AROM. There has been improvement over the past 10-15 years by including power and proprioception as variables of interest by doing hop-testing clusters and UE RTS testing prior to RTS, although even these areas are still sometimes overlooked by rehabilitation specialists. Most often overlooked, though, are fear of reinjury and psychological readiness for RTS. Psychologically informed practice has been used in the treatment of low back pain successfully20 and should be integrated into the athletic population as well. This entails education to reduce fear-avoidance, quota-based exercises, and graded exposure to stimuli to build confidence/resilience. Other interventions may include goal setting, imagery, self-talk, relaxation, and enhancement of social support. A summary of our items to consider in rehabilitation is included in Table 1. Although many studies have used these techniques within the chronic pain population, future research would be pertinent to examine their effectiveness in athletic and RTS populations. Additionally, we found a paucity of research regarding cardiovascular and anaerobic readiness for return to sport following injury. Future research is warranted to investigate whether a lack of cardiovascular fitness may predispose athletes for reinjury following rehabilitation. This would aid in guiding our RTS treatment paradigms and ensuring that therapists are accurately optimizing treatment strategies in the clinic.
Table 1.
Items to Consider in Rehabilitation
| Quantitative Tests/Measures | Cardiovascular Readiness | Psychological Readiness |
|---|---|---|
| Range of motion (ROM) | Aerobic capacity | Confidence |
| Strength (MMT) | Anaerobic capacity | Kinesiophobia |
| Isokinetics | VO2max | Fear of reinjury |
| Hop testing | Sport-specific capacity | FABQ |
| UE return to sports testing | Tampa Scale (TSK-11) | |
| KOOS |
MMT, manual muscle testing; FABQ, fear avoidance belief questionnaire; KOOS, Knee Osteoarthritis Outcome Score; UE, upper extremity.
Although there may be an abundance of published literature and recommendations on what clinicians should be wary of at given stages of the RTS progression (such as referenced above), it is widely accepted that every patient is unique, and variations do occur more often than we would like to admit. Each patient should be treated as an individual. And although the clinician can use normative values and specific markers to monitor progress, the individual patient should be the driving factor behind progressions and progress in their RTS.
Footnotes
Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
References
- 1.Davies W.T., Myer G.D., Read P.J. Is it time we better understood the tests we are using for return to sport decision making following ACL reconstruction? A critical review of the hop tests. Sports Med. 2020;50:485–495. doi: 10.1007/s40279-019-01221-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lavernia C., D’Apuzzo M., Rossi M.D., Lee D. Accuracy of knee range of motion assessment after total knee arthroplasty. J Arthroplasty. 2008;23:85–91. doi: 10.1016/j.arth.2008.05.019. (6 Suppl). doi: 10.1016/j.arth.2008.05.019. [DOI] [PubMed] [Google Scholar]
- 3.Sankar W.N., Laird C.T., Baldwin K.D. Hip range of motion in children: What is the norm? J Ped Orthop. 2012;32:399–405. doi: 10.1097/BPO.0b013e3182519683. [DOI] [PubMed] [Google Scholar]
- 4.Soucie J.M., Wang C., Forsyth A., et al. Range of motion measurements: Reference values and a database for comparison studies. Haemophilia. 2011;17:500–507. doi: 10.1111/j.1365-2516.2010.02399.x. [DOI] [PubMed] [Google Scholar]
- 5.Järvinen T.A.H., Järvinen T.L.N., Kääriäinen M., et al. Muscle injuries: Optimising recovery. Best Pract Res Clin Rheumatol. 2007;21:317–331. doi: 10.1016/j.berh.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 6.Hickey J.T., Timmins R.G., Maniar N., Williams M.D., Opar D.A. Criteria for progressing rehabilitation and determining return-to-play clearance following hamstring strain injury: A systematic review. Sports Med. 2017;47:1375–1387. doi: 10.1007/s40279-016-0667-x. [DOI] [PubMed] [Google Scholar]
- 7.Croisier J.L., Ganteaume S., Binet J., Genty M., Ferret J.M. Strength imbalances and prevention of hamstring injury in professional soccer players: A prospective study. Am J Sports Med. 2008;36:1469–1475. doi: 10.1177/0363546508316764. [DOI] [PubMed] [Google Scholar]
- 8.Webster K.E., Hewett T.E. What is the evidence for and validity of return-to-sport testing after anterior cruciate ligament reconstruction surgery? A systematic review and meta-analysis. Sports Med. 2019;49:917–929. doi: 10.1007/s40279-019-01093-x. [DOI] [PubMed] [Google Scholar]
- 9.Barfod K.W., Feller J.A., Hartwig T., Devitt B.M., Webster K.E. Knee extensor strength and hop test performance following anterior cruciate ligament reconstruction. Knee. 2019;26:149–154. doi: 10.1016/j.knee.2018.11.004. [DOI] [PubMed] [Google Scholar]
- 10.Hulin B.T., Gabbett T.J., Lawson D.W., Caputi P., Sampson J.A. The acute:chronic workload ratio predicts injury: high chronic workload may decrease injury risk in elite rugby league players. Br J Sports Med. 2016;50:231. doi: 10.1136/bjsports-2015-094817. [DOI] [PubMed] [Google Scholar]
- 11.Augustsson J., Thomeé R., Lindén C., Folkesson M., Tranberg R., Karlsson J. Single-leg hop testing following fatiguing exercise: reliability and biomechanical analysis. Scan J Med Sci Sports. 2006;16:111–120. doi: 10.1111/j.1600-0838.2005.00446.x. [DOI] [PubMed] [Google Scholar]
- 12.Engel F.A., Ackermann A., Chtourou H., Sperlich B. High-intensity interval training performed by young athletes: A systematic review and meta-analysis. Front Physiol. 2018;9:1012. doi: 10.3389/fphys.2018.01012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morrison S., Ward P., duManoir G.R. Energy system development and load management through the rehabilitation and return to play process. Int J Sports Phys Ther. 2017;12:697–710. https://pubmed.ncbi.nlm.nih.gov/28900575. [PMC free article] [PubMed] [Google Scholar]
- 14.Rynecki N.D., Siracuse B.L., Ippolito J.A., Beebe K.S. Injuries sustained during high-intensity interval training: Are modern fitness trends contributing to increased injury rates? J Sports Med Phys Fitness. 2019;59:1206–1212. doi: 10.23736/S0022-4707.19.09407-6. [DOI] [PubMed] [Google Scholar]
- 15.Hart H.F., Culvenor A.G., Guermazi A., Crossley K.M. Worse knee confidence, fear of movement, psychological readiness to return-to-sport and pain are associated with worse function after ACL reconstruction. Phys Ther Sport. 2020;41:1–8. doi: 10.1016/j.ptsp.2019.10.006. [DOI] [PubMed] [Google Scholar]
- 16.Lentz T.A., Zeppieri G., George S.Z., et al. Comparison of physical impairment, functional, and psychosocial measures based on fear of reinjury/lack of confidence and return-to-sport status after ACL reconstruction. Am J Sports Med. 2015;43:345–353. doi: 10.1177/0363546514559707. [DOI] [PubMed] [Google Scholar]
- 17.Paterno M.V., Flynn K., Thomas S., Schmitt L.C. Self-reported fear predicts functional performance and second ACL injury after ACL reconstruction and return to sport: A pilot study. Sports Health. 2018;10:228–233. doi: 10.1177/1941738117745806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Prugh J., Zeppieri G., George S.Z. Impact of psychosocial factors, pain, and functional limitations on throwing athletes who return to sport following elbow injuries: A case series. Physiother Theory Pract. 2012;28:633–640. doi: 10.3109/09593985.2012.666632. [DOI] [PubMed] [Google Scholar]
- 19.Tichonova A., Rimdeikienė I., Petruševičienė D., Lendraitienė E. The relationship between pain catastrophizing, kinesiophobia and subjective knee function during rehabilitation following anterior cruciate ligament reconstruction and meniscectomy: A pilot study. Medicina (Kaunas) 2016;52:229–237. doi: 10.1016/j.medici.2016.07.005. [DOI] [PubMed] [Google Scholar]
- 20.Vibe Fersum K., O’Sullivan P., Skouen J.S., Smith A., Kvåle A. Efficacy of classification-based cognitive functional therapy in patients with non-specific chronic low back pain: A randomized controlled trial. Eur J Pain. 2013;17:916–928. doi: 10.1002/j.1532-2149.2012.00252.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


