Abstract
Background:
Recommended personal protective equipment (PPE) is routinely limited or unavailable in low-income countries, but there is limited research as to how clinicians adapt to that scarcity, despite its implications for patients and workers.
Methods:
This is a qualitative secondary analysis of case study data collected in Liberia in 2019. Data from the parent study were included in this analysis if it addressed availability and use of PPE in the clinical setting. Conventional content analysis was used on data including: field notes documenting nurse practice, semi-structured interview transcripts, and photographs.
Findings:
Data from the majority of participants (32/37) and all facilities (12/12) in the parent studies were included. 83% of facilities reported limited PPE. Five management strategies for coping with limited PPE supplies were observed, reported, or both: rationing PPE, self-purchasing PPE, asking patients to purchase PPE, substituting PPE, and working without PPE. Approaches to rationing PPE included using PPE only for symptomatic patients or not performing physical exams. Substitutions for PPE were based on supply availability.
Conclusions:
Strategies developed by clinicians to manage low PPE likely have negative consequences for both workers and patients; further research into the topic is important, as is better PPE provision in low-income countries.
Background
While epidemics and pandemics can cause acute shortages of personal protective equipment (PPE) for health care workers, in many countries PPE is often limited or unavailable under normal working conditions. This chronic shortage of PPE results in routine exposures of both patients and workers to infectious disease. A 2017 survey of healthcare workers (HCWs) found that in low-income countries (countries with a per capita gross national income of $1005 or less) only 11% of respondents had access to respirators appropriate for working with patients with TB; 12% had access to isolation gowns.1 A scarcity of PPE is strongly associated with decreased adherence to standard precautions and infection prevention and control (IPC) protocols.2 Following IPC protocols is critical to preventing the spread of healthcare-acquired infections for both workers and patients.3
Nurses, as the largest cadre of HCWs in the world,4 are particularly vulnerable to these dynamics. Nurses adopt work-around strategies to address low or absent PPE in an effort to mitigate the associated risks.5 These strategies are based on nurses’ and other clinicians’ individual risk assessments and facility-level ad hoc approaches.6,7 What these strategies are, how clinicians select them, and how often they are utilized, however, is not well understood.
In the case of Liberia, a low-income country that suffered an Ebola outbreak from 2014–2015, the epidemic resulted in a significant investment in IPC training for nurses. Consequently, there is a high level of awareness around IPC practices among Liberian nurses,8,9 and Liberia has national IPC guidelines for how PPE should be used in clinical settings.10 Nonetheless, there is also a persistent scarcity of PPE, making following guidelines in the clinical settings at times difficult or impossible.11 How nurses manage this conundrum, and the implications of their approaches for patient and worker safety, is not well understood.
In an effort to better understand the strategies used by nurses working in low-income countries who have limited access to PPE during routine practice, this study examines the strategies used by nurses in Liberia as an exemplar case. The current study sought to answer the research question, “How do Liberian nurses manage limited PPE?”.
Methods
This study is a secondary analysis of data from a qualitative case study originally conducted to study the impact of two Liberian government policies, the Basic and Essential Packages of Health Service (BPHS and the EPHS), on Liberian nursing practice. The data from the parent study was appropriate to studying PPE use as they included both participants’ descriptions of their approach to PPE use, as well as field notes documenting that use in a variety of clinical settings. Conventional content analysis was selected as a preferred method of analysis when describing phenomena for which pre-existing data is limited.12
Description of the Parent Study
The parent study was a case study of the impact of the BPHS and EPHS on nurse practice in Liberia. Thirty-seven nurses and nursing administrators at 12 facilities (seven private, five public; six inpatient, six outpatient) were included in the parent study. Participants had to have worked at their facilities a minimum of six months to be included. Data for the parent study was collected from February-June, 2019 in two counties in Liberia, Montserrado and Nimba. Monrovia, Liberia’s capital, is located in Montserrado county. These counties were selected for their size; approximately one-third of Liberians lived in one of the other at the time of data collection.
Data collection for the parent study included direct observation of nurse practice, semi-structured interviews of participants, and photographs of items relevant to nurse practice in clinical settings. Nurse practice was observed over the course of a shift of the participant’s choosing. The data analyzed for the parent study included: field notes (37), interview transcripts (36), and photographs (214). Data were de-identified prior to being loaded into Atlas.ti v8.3.1 (Scientific Software Development GmbH, Berlin, Germany) for the primary analysis and for this secondary analysis. These de-identified data were used for this secondary analysis. Many of these documents discussed the presence or absence of PPE in the clinical setting and how the nurses used it, indicating these data would be well suited to this analysis.
Methods for the Current Study
Data from the parent study were included in this analysis if it addressed PPE availability in a participant’s current clinical setting (i.e., the setting they were working in at the time of data collection) or strategies developed by participants to use PPE effectively. Conventional content analysis was used for this study because it is well suited to describing and categorizing new aspects of phenomena for which there is limited literature and we wanted to capture the widest possible set of strategies.12 When appropriate, summative content analysis helped to quantify key findings to illustrate the scope of certain issues. Analysis for this study was conducted in January 2021, about eighteen months after primary data collection was completed. LJR [first author] conducted the analysis for both this study and the parent study. APS [last author] was the auditor of the parent study analysis. An audit trail was created by recording the name of every document included in this analysis, as well as the theme extracted, in the order in which it was reviewed. To ensure rigor, we have followed the recommendations of Ruggiano and Perry13 by including a clear explanation of the relationship between the parent study and the secondary analysis, discussing Institutional Review Board (IRB) approval of the secondary analysis, identifying the secondary analysis’ limitations, and using an audit trail.
Approval from the author’s university IRB was obtained for this secondary analysis.
Results
We included 52 documents (28 interview transcripts, four photographs, and 20 field notes), pertaining to 32 of the 37 participants in the parent study, in this analysis. Of these thirty-two participants, 20 worked in Montserrado county and 12 worked in Nimba county. All 12 facilities in the parent study had at least one participant from that facility included in this analysis. This included all four Directors of Nursing included in the parent study because all four discussed limited PPE at their facilities when interviewed. Of the five nurses included in the parent study but not included in this study, four worked at two private facilities (one faith-based and one for-profit), and one worked at a public facility. See Table 1 for a summary of nurses and facilities included in this analysis.
Table 1.
Participant and Facility Characteristics
| Montserrado | Nimba | Total | |
|---|---|---|---|
| Participant Characteristics | |||
| Participants included in secondary analysis | 20 | 12 | 32 |
| Participants from public facilities | 7 | 6 | 13 |
| Participants from private facilities | |||
| For-profit | 5 | 1 | 6 |
| Faith based | 8 | 5 | 13 |
| Facility Characteristics | |||
| Total facilities | 7 | 5 | 12 |
| Public facilities | 2 | 2 | 4 |
| Private facilities | |||
| For-profit | 2 | 1 | 4 |
| Faith based | 3 | 1 | 4 |
Scope of PPE Shortages
Participants reported limited or absent PPE in ten of the twelve facilities (83%). Gloves and surgical masks were the PPE most often reported limited or unavailable. Five of the facilities with limited PPE were public, and five were private. Four of these facilities were inpatient and six were outpatient. Both of the facilities in which PPE was not reported to be limited or absent were private.
The scope of shortages varied by facility type and were described as more severe in public facilities than private ones. The Director of Nursing at one private, faith-based facility in Montserrado described the PPE supply as “depleting” but still had many boxes of gloves in her office. Nurses at the same facility described being able to obtain PPE as needed. By contrast, the Director of Nursing at a public facility in Nimba described the PPE supply there by saying simply, “We don’t have enough.” A nurse at her facility was observed purchasing gloves for her colleagues from her own funds.
Work-around or Rationing Strategies to Mitigate Supply Issues
Five main types of management strategies to address limited or absent PPE were represented in these data. These strategies included: 1) Rationing PPE; 2) Purchasing for PPE themselves; 3) Asking patients to purchase PPE; 4) Working with substituted PPE; and 5) Working without PPE. Table 2 summarizes examples of three of these strategies from both transcripts and field notes.
Rationing PPE took several forms: reserving PPE for known or suspected infectious patients, re-using PPE, and, possibly, deferring physical exams in favor of patient history and labs. Reserving PPE for known or suspected infectious patients was described by a participant working in a private, faith-based facility in Nimba: “What is the essence of wearing PPE? Wearing gowns and masks. No, we don’t do that. Except in the case where the patient is coughing.” One nurse who worked in a private, faith-based facility in Montserrado said that she would re-use one pair of gloves for multiple patients during a day’s work and explained why: “We are trying to be moderate also with the use of material.” One nurse who worked with patients with TB reported that she saved masks for early in the week, when clinics were more crowded; she was observed on a Friday working without a mask.
Deferring physical exams in favor of a patient history and labs was a strategy described by one public facility nurse: “So you are not…going to do examination [when] there is no glove.” Further, eight of the thirty-two participants included in this analysis, at both public and private facilities, were observed taking a very thorough patient medical history and ordering labs without performing any physical examinations during their shift.
Patients or workers purchasing PPE themselves were observed or reported at multiple facilities. The Director of Nursing at a public hospital in Montserrado said, “So if you buy your gloves, then we will treat you.” One participant who worked in a different public facility in Monsterrado said, “You got to get your own gloves because you want to be healthy.” Another participant in Nimba county was observed giving her own money to a clinical assistant so the assistant could purchase gloves.
A number of nurses were observed substituting available PPE for the PPE recommended in Liberia’s IPC guidelines. On one general pediatric ward in a public hospital in Montserrado, elbow-length, plastic gloves from the obstetric ward were used because the regular, wrist-length gloves were unavailable. In a private hospital, a nurse was observed using clean (as opposed to sterile) gloves for a catheter insertion. Last, a nurse was observed seeing a patient who was positive for TB while wearing a surgical mask. Another example, though it was not, strictly speaking, substituted PPE, seems relevant: the regular use of an isopropyl alcohol 50% solution in lieu of hand sanitizer at facilities in Nimba county (See Figure 1). WHO (2010) recommendations indicate isopropyl alcohol-based hand sanitizer should be 75% isopropyl alcohol.
Figure 1.
Isopropyl Alcohol
The final strategy, working without PPE, was also observed as a participant took care of patients infected with TB. This nurse was observed taking care of TB patients both outdoors and indoors with no mask at all. She was aware of the importance of ventilation to keep safe: “That’s the reason why we sit in the open space” but she was directly observed performing a dressing change on a patient indoors.
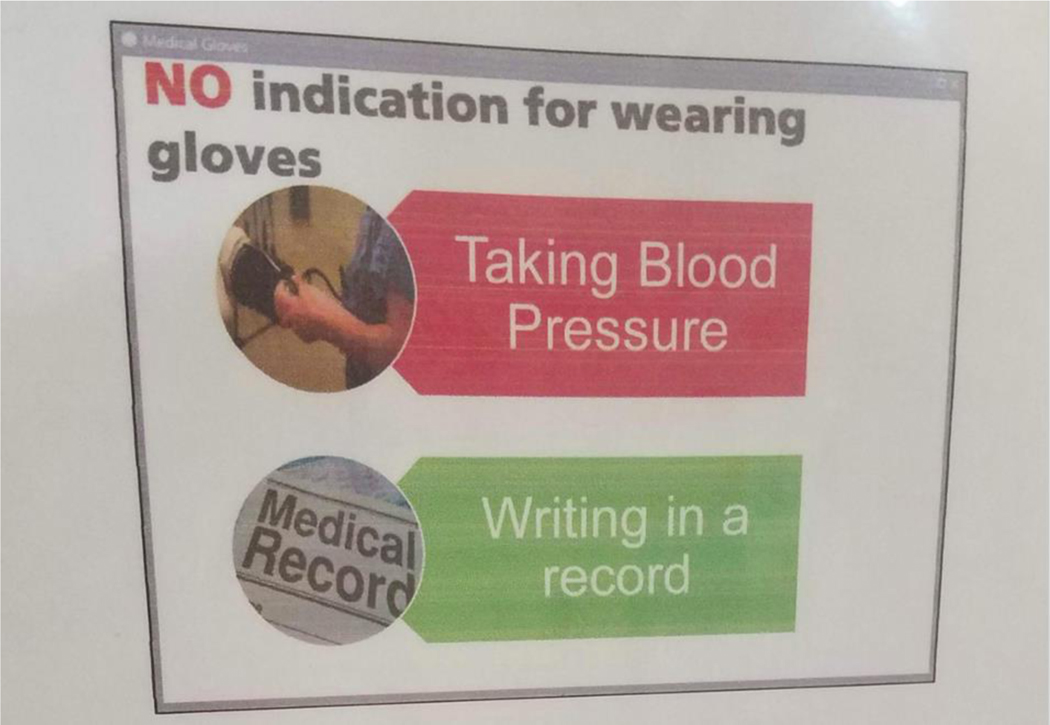
Overuse of PPE
There is some evidence that PPE in Liberia, at times, is overused. One participant, who worked at a private facility in Nimba county, was observed advising her student to “double glove” when examining the intact skin of a patient’s abdomen. Another nurse stated that she should have worn an apron when she was handling a urine specimen, which is not indicated in Liberia’s national IPC guidelines. Last, a sign at a private facility indicated that nurses often wore gloves when documenting or taking patients’ blood pressure by discouraging the practice (See Figure 2).
Figure 2.
Poster Displayed at a Nurses’ Station at a Private Facility in Nimba County
Discussion
These findings suggest that PPE, particularly gloves and masks, is routinely limited or absent at healthcare facilities in Liberia. As a result, nurses must employ a variety of strategies not recommended in Liberia’s national IPC guidelines to protect themselves and their patients from infection. These strategies were often informed by the nurses’ awareness of the importance of PPE in protecting themselves and their patients.
These strategies were not unique. Limited availability of face masks has been documented in Vietnam among nurses who worked with patients with TB 15; the strategies these nurses reported using to manage their limited supplies included sanitizing masks themselves and purchasing masks for themselves. While nurses in this study did not report sanitizing their own PPE, self-purchase of PPE was an important approach. Further, the ad hoc nature of the approaches described in this study mirrors the Drevin et al.’s 6 findings in Sierra Leone, where safety procedures at obstetric facilities changed repeatedly due to a lack of available PPE during the Ebola epidemic.
For clinicians, the fact that these strategies need to be developed and applied by individuals likely adds to the difficulty of their job. Clinicians who have limited access to PPE report increased stress at work6,16 and greater rates of job dissatisfaction.17 This could be due largely to fear of infection, but also a consequence of the additional cognitive load of identifying and implementing new strategies based on shifting PPE availability. Each facility included in both this analysis and the parent study had an IPC Focal Person (i.e., a person whose is responsible for encouraging appropriate IPC practices). This is a highly active role in Liberia,9,11 but Focal People cannot enforce adherence to PPE guidelines when materials are not available.
Further examination of PPE rationing, with an eye towards creating guidelines that would be useful in situations of PPE scarcity, would likely lighten this load. While healthcare workers in high-income countries are known to use PPE selectively based on the infectious organism,7 in Liberia nurses reported making decisions based on symptoms such as coughing, as did clinicians in Vietnam.15 Further investigation into how nurses make these decisions could identify some clinician preferences that are more protective than others, and suggest opportunities for training and evidence-based guidance. Decision analysis techniques may prove useful for studying that phenomenon.
For patients, the net effect of re-using PPE on their exposure to infectious disease is not well understood. Further research on this phenomenon is particularly warranted due to the growing body of evidence that PPE is routinely absent in many settings. The re-use of PPE that comes into direct contact with patients, such as gloves, likely presents a different set of risks than the re-use of masks and respirator, but stronger data, including studies that examine microorganisms on re-used PPE, would be very useful in stratifying risk.
Another potential effect of absent PPE on patients may result from HCW’s unwillingness to perform physical exams in the absence of PPE. Only one participant explicitly identified deferring exams as a PPE management strategy, but several HCWs were observed providing care without performing an exam, and it is possible many did so for the same reason. Unfortunately, follow-up questions were not feasible in this secondary analysis; further research into this possibility would be valuable. Further, how physical exams can be effectively performed using only inspection has been explored in more detail due to the rise of telemedicine during COVID-19 18,19; those studies may have interesting implications for PPE-limited contexts and provide suggestions for relevant clinician trainings.
Lastly, the financial consequences of PPE scarcity fall on both clinicians and patients. Clinicians purchasing PPE themselves or asking patients to purchase it before receiving treatment was probably effective at preventing infection, but it shifts costs from the healthcare system to individuals. This is unfortunate; out-of-pocket costs paid by Liberians already constitute roughly 42% of total health expenditure in Liberia.20 If this strategy is used routinely, it almost certainly constitutes a barrier to care that many patients cannot overcome. Further, nurses in Liberia earn between $250 and $300 USD per month, and many nurses do not receive their pay regularly.21 At the time of data collection, a box of gloves cost about $4 USD, meaning that regular purchasing for individual protection would quickly become a challenge.
Ongoing research into these different strategies should not be viewed as a substitute for the provision of required PPE for the HCWs and patients. Organizations, within Liberia and beyond, working to improve health outcomes in Liberia should consider the probable clinical consequences of missing PPE as a threat to their goals of better healthcare for all and include PPE provision in their budgets. Last, these data indicate some clinicians in Liberia were overusing PPE. Additional training about appropriate use, perhaps from these same organizations, might preserve limited stocks for longer period of time.
Limitations
Limitations of the study center on those associated with qualitative secondary data analyses and how the parent study data were collected. First, data were collected in two of Liberia’s 15 counties. These two counties, Nimba and Montserrado, are two of the most urban and accessible counties in Liberia (Monrovia is connected to Nimba county by a paved road); thus, it is likely the availability of PPE in these facilities was a best-case scenario. Observation time at each facility varied according to the number of participants at that facility. One facility in Nimba had only one participant and thus only one day of observation. Since much of these data came from direct observation and interviews, they are vulnerable to both the Hawthorne effect and social desirability bias. Last, since this was a secondary data analysis, it was not possible to follow up with participants about some of the questions raised in this study.13 Follow-up would have been particularly useful in investigating possible exposures related to these PPE management strategies, and whether nurses were deferring physical exams due to limited PPE.
Conclusions
These findings substantiate regular low supply of basic PPE in one low-income country and how said lack of resource impacts frontline healthcare delivery by nurses. Nurses applied a variety of management strategies; these strategies varied in their potential impact on patient and worker health. Further investigation into the nature, frequency, and consequences of low PPE management strategies may improve worker and patient health and have potential transferability to other clinicians who routinely do not have access to adequate PPE.
Highlights.
Personal protective equipment is often absent in low- and middle-income countries
Healthcare workers adopt workarounds to cope with missing equipment
These workarounds are poorly understood despite their importance to safety
This study identifies multiple workarounds used consistently by nurses in Liberia
These strategies have different implications for both workers and patients
Acknowledgement.
The authors would like to acknowledge Dr. Robyn d’Avignon for her contributions to this manuscript.
Funding. Funding for the parent study was provided by Grant Number, T42OH008422, funded by the Centers for Disease Control and Prevention. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention or the Department of Health and Human Services. The parent study was also supported by the 2018 AAOHN Medique Research Grant. This secondary analysis was funded by Postdoctoral Fellowship Training Grant (T32 NR016914. Program Director: Titler) Complexity: Innovations in Promoting Health and Safety.
Footnotes
No conflicts of interest
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Desai AN, Ramatowski JW, Lassmann B, Holmes A, Mehtar S, Bearman G. Global infection prevention gaps, needs, and utilization of educational resources: A cross-sectional assessment by the International Society for Infectious Diseases. Int J Infect Dis. 2019;82:54–60. doi: 10.1016/j.ijid.2019.02.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beyamo A, Dodicho T, Facha W. Compliance with standard precaution practices and associated factors among health care workers in Dawuro Zone, South West Ethiopia, cross sectional study. BMC Health Serv Res. 2019;19(1):381. doi: 10.1186/s12913-019-4172-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Health Care without Avoidable Infections: The Critical Role of Infection Prevention and Control; 2016. Accessed January 12, 2021. https://www.who.int/infection-prevention/publications/ipc-role/en/
- 4.World Health Organization. Reprot of the Policy Dialogue Meeting on the Nursing Workforce; 2017. https://www.who.int/hrh/news/2017/NursingApril2017-2.pdf
- 5.Buxton H, Flynn E, Oluyinka O, et al. Barriers and opportunities experienced by staff when implementing infection prevention and control guidelines during labour and delivery in healthcare facilities in Nigeria. J Hosp Infect. 2019;103(4):428–434. doi: 10.1016/j.jhin.2019.07.018 [DOI] [PubMed] [Google Scholar]
- 6.Drevin G, Mölsted Alvesson H, van Duinen A, Bolkan HA, Koroma AP, Von Schreeb J. “For this one, let me take the risk”: why surgical staff continued to perform caesarean sections during the 2014–2016 Ebola epidemic in Sierra Leone. BMJ Glob Health. 2019;4(4):e001361. doi: 10.1136/bmjgh-2018-001361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harrod M, Weston LE, Gregory L, et al. A qualitative study of factors affecting personal protective equipment use among health care personnel. Am J Infect Control. 2020;48(4):410–415. doi: 10.1016/j.ajic.2019.08.031 [DOI] [PubMed] [Google Scholar]
- 8.Cooper C, Fisher D, Gupta N, MaCauley R, Pessoa-Silva CL. Infection prevention and control of the Ebola outbreak in Liberia, 2014–2015: key challenges and successes. BMC Med. 2016;14:2. doi: 10.1186/s12916-015-0548-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tremblay N, Musa E, Cooper C, et al. Infection prevention and control in health facilities in post-Ebola Liberia: don’t forget the private sector! Public Health Action. 2017;7(Suppl 1):S94–S99. doi: 10.5588/pha.16.0098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ministry of Health. National Infection Prevention and Control Guidelines.; 2018. Accessed February 7, 2021. https://www.washinhcf.org/wpcontent/uploads/2018/05/Liberia-National-IPC-Guidelines-2018.pdf
- 11.Ridge LJ, Stimpfel AW, Klar RT, Dickson VV, Squires AP. Infection Prevention and Control in Liberia 5 Years After Ebola: A Case Study. Workplace Health Saf. Published online April 13, 2021:2165079921998076. doi: 10.1177/2165079921998076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hsieh H-F, Shannon SE. Three Approaches to Qualitative Content Analysis. Qualitative Health Research. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- 13.Ruggiano N, Perry TE. Conducting secondary analysis of qualitative data: Should we, can we, and how? Qual Soc Work. 2019;18(1):81–97. doi: 10.1177/1473325017700701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization. Guide to Local Production: WHO-Recommended Handrub Formulations; 2010. https://www.who.int/gpsc/5may/Guide_to_Local_Production.pdf
- 15.Chughtai AA, Seale H, Chi Dung T, Maher L, Nga PT, MacIntyre CR. Current practices and barriers to the use of facemasks and respirators among hospital-based health care workers in Vietnam. American Journal of Infection Control. 2015;43(1):72–77. doi: 10.1016/j.ajic.2014.10.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fadare RI, Akpor OA, Ifechukwude IG, Richard D A, Bello CB. Nurses’ Safety in Caring for Tuberculosis Patients at a Teaching Hospital in South West Nigeria. J Environ Public Health. 2020;2020:3402527. doi: 10.1155/2020/3402527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Naburi H, Mujinja P, Kilewo C, et al. Job satisfaction and turnover intentions among health care staff providing services for prevention of mother-to-child transmission of HIV in Dar es Salaam, Tanzania. Hum Resour Health. 2017;15(1):61. doi: 10.1186/s12960-017-0235-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Laskowski ER, Johnson SE, Shelerud RA, et al. The Telemedicine Musculoskeletal Examination. Mayo Clin Proc. 2020;95(8):1715–1731. doi: 10.1016/j.mayocp.2020.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wahezi SE, Duarte RA, Yerra S, et al. Telemedicine During COVID-19 and Beyond: A Practical Guide and Best Practices Multidisciplinary Approach for the Orthopedic and Neurologic Pain Physical Examination. Pain Physician. 2020;23(4S):S205–S238. [PubMed] [Google Scholar]
- 20.World Health Organization. Out-of-Pocket Expenditure as Percentage of Current Health Expenditure (CHE) (%) Data by Country.; 2021. Accessed February 18, 2021. https://apps.who.int/gho/data/node.main.GHEDOOPSCHESHA2011?lang=en
- 21.Ballah Zeze. Health Workers End Strike, Return to Work Today. The Bush Chicken. https://bushchicken.com/health-workers-end-strike-return-to-work-today/. Published September 20, 2019. Accessed February 16, 2021. [Google Scholar]