Abstract
Rationale
COVID-19 vaccine hesitancy presents significant challenges for public health.
Objective
Vaccine hesitancy among middle-aged and older adults has been a significant barrier in Singapore's battle against COVID-19. We hypothesize that the trust middle-aged and older adults place in various sources of information influences vaccine hesitancy, and that distinct typologies of trust can be identified to better inform targeted health communication efforts.
Method
Data from a nationally representative panel survey of Singaporeans aged 56–75 (N = 6094) was utilized. Modules fielded in August and November 2020, and June 2021 were analyzed, assessing social networks, trust in sources of information, and vaccination status respectively. Predictors of vaccination status were first examined. Latent class analysis was then used to identify typologies of trust in various sources of information.
Results
Trust in formal sources of information (e.g government sources) is found to predict vaccination status among respondents. Contrary to expectations, trust in social media and informal sources (family and friends), and perceived social support did not predict vaccination status. Latent class analysis identified 4 typologies of respondents based on their patterns of trust in these sources. Significantly, it is found that a portion of respondents with low trust in formal sources of information have high trust in informal sources. The four distinct typologies of trust in sources of information are also found to predict vaccination status.
Conclusions
Because trust in formal sources of information influences vaccination status, authorities should build trust in such sources to encourage vaccination against COVID-19. However, health communication strategies with middle-aged and older adults who have low levels of trust in the formal sources may be more effective if authorities leveraged alternative channels such as informal sources, including the social networks of such individuals. Overall, the findings suggest the need for targeted communication strategies to encourage vaccination.
1. Introduction
As the COVID-19 pandemic proceeds and governments race to vaccinate their populations against new variants, much attention has now shifted to the barriers preventing effective levels of immunization that would grant countries herd immunity and allow the resumption of normal life (Machingaidze and Wiysonge, 2021; Ullah et al., 2021). While these barriers have included structural issues such as limited vaccine supplies (Bollyky, 2021), significant attitudinal barriers have resulted in vaccine hesitancy (Paul et al., 2020). Such barriers have been identified in various countries including Singapore (Tan et al., 2021), where the current study is based.
Given this, the current research examines whether the sources of information that middle-aged and older adults in Singapore trust for information on COVID-19 influences vaccine hesitancy. In particular, in addition to sources that existing studies have examined such as social media and the government, the current study also examines the level of trust that individuals place in other informal sources more relevant to middle aged and older adults, specifically their friends and family. Further, the current study hypothesizes that the level of trust placed in a single source, for instance government sources, may be correlated with other sources such as trust in local television.
In Singapore, vaccine hesitancy has been particularly prevalent among middle-aged and older adults. While vaccinations for those aged 70 and above started in February 2021 and in March 2021 for those 60 and above, about 25% of adults above the age of 60 remained unvaccinated and had not booked appointments to vaccinate as of July 2021 (Kurohi, 2021). This is compared to 86% of individuals aged 40–59 who had received at least one dose of the vaccine or booked their appointments to do so at that point in time, despite vaccinations for this group starting later (Lim, 2021). The poor vaccination rates among older adults, coupled with the arrival of the Delta variant, has subsequently resulted in the re-institution of restrictions in Singapore to curb the virus (Teo, 2021a). Thus, to facilitate the success of vaccination regimes, it is imperative to identify the attitudinal barriers that lead to vaccine hesitancy and to design effective interventions to address them.
Preliminary studies have identified several attitudinal barriers that lead to vaccine hesitancy including misinformation and misconceptions about vaccines (Fisk, 2021). A significant factor contributing to such barriers is the use of particular sources of information, especially social media, that has been shown to be associated with vaccine hesitancy (Jennings et al., 2021; Kumari et al., 2021; Malik et al., 2020). Closely intertwined with the use of non-reliable sources such as social media, or in the case of the US certain news outlets, is the belief in conspiracy theories that create false perceptions of COVID-19 vaccines (Romer and Jamieson, 2020; Ullah et al., 2021). Additional to the use of such sources of information is the importance of the level of trust that individuals place in the government or authorities in predicting vaccine hesitancy in general (Casiday et al., 2006; Larson et al., 2018). Specific to COVID-19 this relationship has also been observed as well - it has been found that individuals with greater levels of trust in the government and other health institutions are more likely to vaccinate against COVID-19 (Daly et al., 2021; Trent et al., 2021).
While these studies have shed important light on the factors and barriers influencing vaccine hesitancy, much is still needed to be understood specific to vaccine hesitancy among middle-aged and older adults. This is because the influence of social media on vaccine hesitancy may be less applicable to middle-aged and older adults who have been shown to be less likely to use social media in general (Holt et al., 2013; Perrin, 2015). Instead, prior studies on the effect of social support on health behavior have illustrated that non-institutional actors, for instance informal social networks such as friends and family, are important sources of health information for middle-aged and older adults (Auslander and Howard, 1990; Harvey and Alexander, 2012; Penning, 1995). It has been argued that for certain populations, such sources are more respected and trusted as a result of the greater intimacy individuals share with these sources (Straughan and Adeline, 2000). The influence of such sources on middle-aged and older adult vaccine hesitancy may thus be significant and should be better studied. Hence, in order to account for the influence that these non-institutional actors may have on the COVID-19 vaccine willingness of middle-aged and older adults, the current study examines trust in sources of information rather than trust in institutions as other studies have paid attention to, such as trust in government (Prickett and Simon, 2021) or in science (Merkley and Loewen, 2021). Previous research has illustrated the importance of trust in sources of information in shaping health literacy (Chen et al., 2018) and behaviors (Brown-Johnson et al., 2018) as the level of trust that individuals place in specific sources influences the perceived validity of a particular piece of information that they come across (Brewer and Ley, 2013), giving reason to believe that it is a relevant concept to study in understanding vaccine hesitancy.
Additionally, doing so would potentially enable policymakers to identify alternative channels through which middle-aged and older adults with low trust in formal sources (such as government sources) can be encouraged to vaccinate. This would facilitate the development of short-term strategies to increase COVID-19 vaccination rates, as policy recommendations to build trust in formal sources (Lazarus et al., 2021) may not be feasible within the critical timeframe needed to achieve herd immunity against current variants of COVID-19.
Hence, our research aims for this paper are twofold – to identify middle-aged and older adult subgroups that are not forthcoming to receive the COVID-19 vaccination based on their patterns of trust in sources of information, and to explore the avenues of communication which may be more effective in reaching out to these subgroups in terms of the likelihood that such older adults would trust these avenues.
1.1. COVID-19 in Singapore
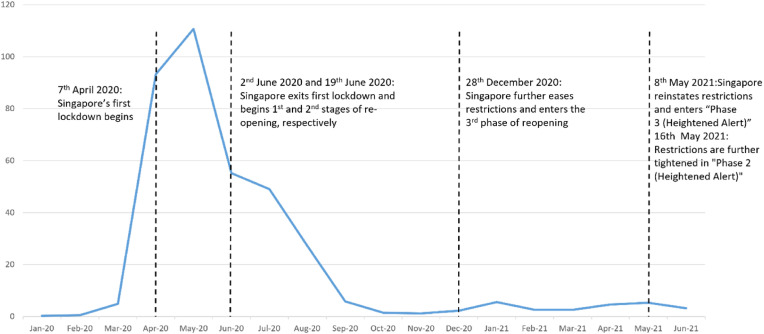
Singapore's first case of COVID-19 was identified on January 23, 2020 and by April 1, 2020, 1000 cases had been detected in the country. This prompted local authorities to implement a lockdown from April 7, 2020 to June 1, 2020, barring all residents from leaving their homes for non-essential activities (see Fig. 1). Following the lockdown, restrictions were gradually eased through a series of phases. Phase 1 and 2 of Singapore's reopening started on 2 June and 19 June respectively. During Phase 2, individuals were allowed to gather in groups of 5 and various social activities were permitted to resume. At the end of November 2020, Singapore's COVID-19 cases were largely confined to single digit figures (Ritchie et al., 2020). With the improving COVID-19 situation, local restrictions were eased further, and the country transitioned to Phase 3 of its reopening on December 28, 2020. In this phase, individuals were allowed to gather in groups of 8 and various social activities were permitted to be held in larger groups. However, following the local transmission of the Delta COVID-19 variant in the community and resulting rise in community cases, Singapore returned to stricter measures on May 8, 2021, with social gatherings capped at 5 persons. Measures were tightened once again on May 16, 2021, limiting social groups to a maximum of 2 persons.
Fig. 1.
Timeline of Singapore's monthly average of new cases per million residents per day from January 2020 to June 2021, and the different stages of Singapore's efforts to contain the virus.
Concurrent with Singapore's re-opening in Phase 3, Singapore's vaccination campaign started on December 30, 2020 with priority given to high-risk groups including frontline workers, the elderly, and persons with comorbidities (Ministry of Health, 2020). Vaccinations were made available to all Singapore residents for free and were progressively rolled out to residents by age group - those aged 70 and above could vaccinate from February 22, 2021, those aged 60–69 years from March 8, 2021, and those aged 45–59 years from March 24, 2021 (Channel News Asia, 2021a). As mentioned, the vaccination drive has been met with resistance, especially from middle-aged and older adults. In light of this authorities have implemented various initiatives to encourage vaccination among older adults, for instance launching home vaccination services to allow homebound older adults to get vaccinated (Lim and Kwee, 2021). However, despite such measures, vaccination rates among middle-aged and older adults remain significantly lower than that of younger groups at the time of writing.
1.2. Media landscape in Singapore during COVID-19
Within Singapore, trust in the government has been shown to be generally high (Wong and Jensen, 2020). However, the COVID-19 pandemic brought much uncertainty resulting in inconsistencies in the government's public health messaging. For instance, at the start of the pandemic, the Singapore government had initially recommended that individuals should not wear masks as they were deemed ineffective but later reversed their recommendation and made masks mandatory in public spaces (Reuters, 2020). This, coupled with spread of COVID-19 misinformation (Long and Liu, 2021) and the increasing pervasiveness of conspiracy theories and false information in Singapore (Channel News Asia, 2021b) especially among older adults (IPS Exchange Series, 2021), has generated much ‘noise’ in the information landscape in Singapore. To address this the government has utilized the law to police sources of information and prevent the spread of false information. Authorities have made use of the Protection from Online Falsehoods and Manipulation Act (2019) (POFMA) which gives authorities powers to censor information sources that are deemed by authorities to be spreading falsehoods. POFMA has been used on various information outlets to censor alleged COVID-19 misinformation multiple times during the pandemic so far (Teo, 2021b). The existence of POFMA illustrates the tight control that the Singapore government maintains over most media outlets in the country (Lee and Willnat, 2009) which results in a media landscape that is more subdued in terms of the proliferation of narratives counter to the government's in the mainstream media, as compared to other countries such as the United States where political polarization has shaped the media landscape (Wilson et al., 2020).
Nevertheless, with the aforementioned inconsistencies in the government's messaging early in the pandemic, existing criticisms of POFMA as a tool for the government to exert political control casting doubt on the legitimacy of its usage (Teo, 2021b), and the flood of misinformation on social media beyond the government's ability to filter, the onus has still largely been placed on the individual to exercise discretion in their consumption of information about the pandemic. This gives reason to believe that the level of trust that middle-aged and older adults in Singapore place in various sources of information may be important in influencing COVID-19 vaccination hesitancy.
2. Methods
2.1. Study design and participants
This study utilizes data from the Singapore Life Panel (SLP), a population representative monthly survey of Singaporeans aged 56–75. The SLP is a monthly online panel survey that has been ongoing since 2015. Respondents were recruited through a random sample of 25,000 households in Singapore, obtained from the Department of Statistics in 2015 (see Vaithianathan et al., 2018). From this sample, 11,500 respondents were successfully recruited onto the panel at the baseline in 2015. Over the course of 5 years, attrition and the removal of non-active panel members (defined as those who have not participated in any survey for 12 consecutive months) resulted in a sample of 8,386 active respondents in June 2021. Monthly survey responses are collected through an online survey platform. Respondents are given the option to complete the self-administered surveys on the web or to do so via a telephone interview. All survey instruments are available in English, Mandarin, Malay and Tamil - the four most common languages spoken in Singapore. Respondents’ informed consent for their participation in the panel was first collected in 2015 during recruitment for a period of 5 years which was the original intended duration of the panel. In July 2020 informed consent was collected once again through the online survey platform due to the panel being extended for another 5 years. Respondents are compensated with grocery vouchers that are mailed to their address for every survey they complete, with amounts varying based on the length of the survey being fielded for the month.
This paper uses data collected in June 2021 on COVID-19 vaccination rates, November 2020 on the trust that respondents have in various sources of information for information on COVID-19, and August 2020 on respondents' social networks. The survey platform yielded 6,861 responses in June 2021, 7,210 responses in November 2020, and 7,394 responses in August 2020, corresponding to initial response rates of 81.8%, 86.0%, and 88.2% respectively. After restricting the sample to respondents who had participated in both the November 2020 (when the trust in different sources of information for COVID-19 information question was fielded) and June 2021 (when respondents were asked of their vaccination statuses) surveys, as well as accounting for missing data, an initial sample of 6,094 respondents was derived (Sample I). This was the sample on which the latent class analysis (LCA) was carried out as the LCA did not require additional variables. However, further restricting the analytical sample to respondents who had also participated in August 2020 (when the social networks data was collected) resulted in a second sample of 5,738 respondents. To better reflect vaccine willingness based on respondents’ vaccination status, a further 61 responses who cited being ineligible as a reason for not vaccinating were excluded from the analysis. This was done to account for respondents who were not vaccinated at this point in time due to medical conditions such as anaphylaxis rather than a lack of willingness. This resulted in a final sample of 5,677 respondents (Sample II). This results in a final valid response rate of 67.7% which is argued to be an acceptable response rate for social research (Baruch, 1999). This final sample was used to carry out the various regression analyses that required the use of these additional variables. Due to the use of two different samples, the number of observations used in each analysis is presented in the title of every table presenting the results.
2.2. Measures
2.2.1. Vaccination status
This study examined vaccination hesitancy by studying respondents' vaccination status. This was determined by asking respondents if they had been vaccinated against COVID-19 in June 2021. Respondents were given four options to describe their vaccination status; that they were fully vaccinated (completed 2 doses or had 1 dose and does not require a second), partially vaccinated (only had 1 dose), intending to vaccinate but yet to register, and not planning to vaccinate. Due to the government's vaccination drive outlined above, non-vaccination in June 2021 would unlikely be due to lack of access and more likely due to vaccine hesitancy. In order to better identify trends, respondents who were either partially or fully vaccinated were merged as “Vaccinated” (coded as 1), and respondents who were planning to vaccinate but had not, and respondents who did not plan to vaccinate were merged as “Not vaccinated” (coded as 0).
2.2.2. Trust in sources of information
Participants were asked to rate their level of trust in several news sources (government sources, local news on television, local radio channels, social media, family, and friends), specific to news and information on COVID-19. The types of sources included in the question were identified based on the local context in Singapore. Since the beginning of the pandemic, the Singapore government has made significant efforts to communicate information on COVID-19 to the public through channels directly managed by government ministries or agencies. For instance, daily case updates were communicated through Whatsapp and other messaging platforms such as Telegram, as well as Singapore's Ministry of Health website. As such, “government sources”, referring to sources of information coming directly from government ministries or agencies, were deemed to be of interest. Local television and radio are also popular sources of information among the public in Singapore. While such sources of information are tightly monitored by the government they remain privately managed, distinguishing such sources from “government sources”. Based on the literature cited above, the current study was also interested in examining trust in social media platforms, such as Twitter, Facebook, and Instagram, as well as family and friends for information on COVID-19. Respondents rated their trust in each source on a 6-point Likert scale ranging from “Strongly Mistrust” to “Strongly Trust”. For ease of interpretation and analysis, the variables were dichotomized during the latent class modelling, but were treated as ordinal in other analysis. For dichotomization, “Strongly Mistrust”, “Somewhat Mistrust”, and “Slightly Mistrust” responses were merged into “Mistrust”, and “Strongly Trust”, “Somewhat Trust”, and “Slightly Trust” responses were merged into a “Trust” category.
In order to account for multicollinearity between trust variables for our first logistic regression model predicting vaccination status (see Table 3 ), trust scores between ‘formal sources’ (government sources, local television, and local radio), and trust scores between ‘informal sources’ (friends and family) were separately averaged to create indexes, and these indexes were used to represent the level of trust respondents place in formal and informal sources in the model.
Table 3.
Odds ratios of correlatives predicting vaccination status (N = 5,677).
| Variable | Odds Ratio |
|---|---|
| Trust in Formal Sources | 1.28*** |
| Trust in Informal Sources | 0.92 |
| Trust in Social Media | 0.93t |
| Gender | |
| Male | REF |
| Female | 0.82* |
| Race/Ethnicity | |
| Chinese | REF |
| Malay | 1.14 |
| Indian | 0.66* |
| Other | 1.15 |
| House type | |
| 1–3 Room HDB Flat | REF |
| 4–5 Room HDB Flat or Executive Condominium | 1.27* |
| Private apartment/condominium/landed property | 1.06 |
| Highest Education Achieved | |
| Primary or No Formal Education | REF |
| Secondary | 1.11 |
| Post-Secondary without University Degree | 0.82 |
| Post-Secondary with University Degree | 0.86 |
| Subjective Health Status | 1.26*** |
| Age | 0.99 |
| Social Support | 0.99 |
| Monthly Income | 1.00*** |
| Network Density | 1.18 |
| Cragg-Uhler/Nagelkerke R2 | 0.044 |
Note: The results are based on logistic regression models with “Not Vaccinated” as the reference group to “Vaccinated”.
tp < .10. *p < .05. **p < .01. ***p < .001.
2.2.3. Social support
To assess social support, several items were adopted from the Medical Outcome Study Social Support Survey (Sherbourne and Stewart, 1991). Participants were asked how often various forms of support were available to them when they needed it. These included “Someone you can count on to listen to when you need to talk”, “Someone to confide in or talk to about yourself or your problems”, “Someone who you can count on for help in a time of need”, “Someone to show you love and affection”, “Someone to help you if you were confined to bed”, “Someone to prepare your meals if you were unable to do it” and “Someone to help with daily chores if you were sick”. Items were rated on a 5-point Likert scale ranging from “None of the time” to “All of the time”. Participants’ scores were subsequently summed to generate an overall social support score (minimum 4 – maximum 20). As the instrument is fielded monthly, this study uses data from the June 2021 wave.
2.2.4. Network density
To account for differences in the social structures of respondents, network density, referring to the proportion of possible ties existing within a social network, was included as a covariate in the analysis. This was measured using a name generator drawn from the General Social Survey. Respondents were first asked to list the names of up to 5 of their closest contacts and then subsequently asked to rate, on a scale ranging from 1 – Not at all close to 4 – Very close, the extent to which each of their 5 social contacts (or alters) listed knew each other for a total of ten maximum ties that could occur between all 5 alters. Ties were determined to be present between two alters if they were at least “Not very close”, excluding cases where two alters were “Not at all close”. Network density was then calculated by dividing the number of ties existing by the total number of possible ties in the ego's network, excluding the ties between the ego and their alters as has been done in previous studies on egocentric networks (for example, Walker, 2015).
Network density was a variable of particular interest as the density of one's network has been argued to influence the spread of information within the network, while at the same time also influencing one's behavior due to the establishment of particular norms within the network (Granovetter, 1992). While some studies have shown that the social networks of older adults become smaller as they age (Fuller-Iglesias at al. 2015; Huxhold et al., 2013), other studies have illustrated that social networks among older adults tend to be stable (van Tilburg, 1998) – given that the social networks module was fielded less than a year before vaccination status was enquired, the authors thus saw it fit to utilize the social networks data collected in August 2020.
2.2.5. Self-reported health
As the present study focused on older adults who are in general more likely to be in poorer health and existing studies had identified the fear of the side effects as a key reason for not taking the vaccine (Nguyen et al., 2021), respondents’ self-reported health or subjective health status was also included as a covariate in the analysis. Respondents were asked to rate their health on a five-point scale ranging from 1 – Poor to 5 – Excellent. The question on self-reported health is fielded monthly.
2.2.6. Statistical analysis
Using Stata 17.0, logistic regression models were applied to examine the effect of the aforementioned correlatives on vaccination status (Table 3 ). LCA was subsequently applied to identify patterns in the trust that respondents place in sources of information (Table 4 ). LCA was selected as an appropriate analytical method due to its ability to inform practice in developing strategic, targeted interventions (Weller et al., 2020), the key purpose of the current research. LCA was thus used to identify typologies based on the pattern of trust that respondents placed in the 6 different sources of information, and the analysis was conducted using MPlus 8.5. With reference to the model fit statistics (see Table 7 in appendix), 4 groups were defined with each group displaying distinct patterns of trust in the different sources. Additional reliability checks were also conducted by calculating the latent class probabilities for each class (average latent class probabilities were at least .95 for all classes).
Table 4.
Latent class analysis on sources of information on COVID-19 (N = 6,094).
| Source of Information | Rating | Group 1 (7.81%) | Group 2 (85.83%) | Group 3 (3.59%) | Group 4 (2.77%) |
|---|---|---|---|---|---|
| Government Sources (%) | Don't Trust | 0.09 | 0.01 | 1.00 | 0.83 |
| Trust | 0.91 | 0.99 | 0.00 | 0.17 | |
| Local news on television (%) | Don't Trust | 0.01 | 0.00 | 1.00 | 0.92 |
| Trust | 0.99 | 1.00 | 0.00 | 0.09 | |
| Local radio channels (%) | Don't Trust | 0.05 | 0.01 | 0.99 | 0.78 |
| Trust | 0.95 | 0.99 | 0.01 | 0.22 | |
| Social Media (%) | Don't Trust | 0.91 | 0.32 | 0.93 | 0.67 |
| Trust | 0.10 | 0.68 | 0.07 | 0.34 | |
| Family (%) | Don't Trust | 0.53 | 0.00 | 0.95 | 0.09 |
| Trust | 0.47 | 1.00 | 0.05 | 0.91 | |
| Friends (%) | Don't Trust | 0.97 | 0.01 | 1.00 | 0.06 |
| Trust | 0.03 | 0.99 | 0.00 | 0.94 |
A final logistic regression model was then applied to assess the value of the latent groups identified in predicting respondents’ vaccination status (Table 6 ).
Table 6.
Odds ratios of correlatives for vaccination status with latent groups (N = 5,677).
| Variable | Odds Ratio |
|---|---|
| Latent Group | |
| Group 1: Pro-formal Selective | REF |
| Group 2: Broad Trust | 0.73t |
| Group 3: Broad Distrust | 0.43*** |
| Group 4: Pro-informal Selective | 0.41** |
| Gender | |
| Male | REF |
| Female | 0.83* |
| Ethnicity | |
| Chinese | REF |
| Malay | 1.13 |
| Indian | 0.66* |
| Other | 1.15 |
| House Type | |
| 1–3 Room HDB Flat | REF |
| 4–5 Room HDB Flat or Executive Condominium | 1.28* |
| Private apartment/condominium/landed property | 1.08 |
| Highest Education Achieved | |
| Primary or No Formal Education | REF |
| Secondary | 1.13 |
| Post-Secondary without University Degree | 0.85 |
| Post-Secondary with University Degree | 0.89 |
| Subjective Health Status | 1.26*** |
| Age | 1.00 |
| Social Support | 1.00 |
| Monthly Income | 1.00*** |
| Network Density | 1.17 |
| Cragg-Uhler/Nagelkerke R2 | 0.04 |
3. Findings
Table 1 describes the sample characteristics for both samples. A large majority (about 86%) of older adults in both samples had received at least one dose of COVID-19 vaccines. The mean age for both samples was about 64 years, and about 53% and 52% of respondents in the first and second samples were women, respectively. Ethnic distribution in both samples was similar, with about 89% Chinese, 5% Malay, 5% Indian, and 2% Others. In both samples, about 19% of respondents lived in 1–3 Room HDB flats, about 63% lived in 4–5 Room HDB flats or Executive Condominiums, and about 18% lived in Private apartments, condominiums, or landed properties. A majority (64%) of respondents in both samples reported their health as being Excellent, Very good, or Good. Respondents in the second sample had a mean Social Support score of about 14, and a mean network density score of 0.7.
Table 1.
Sample descriptions.
| Variables | Sample I (N = 6,094) | Sample II (N = 5,677) |
|---|---|---|
| Vaccinated with at least 1 dose (%) | 85.58 | 86.84 |
| Mean of Age (SD) | 64.28 (5.42) | 64.27 (5.41) |
| Female (%) | 52.35 | 52.51 |
| Ethnicity (%) | ||
| Chinese | 88.97 | 89.13 |
| Malay | 4.78 | 4.65 |
| Indian | 4.53 | 4.56 |
| Others | 1.72 | 1.66 |
| House Type (%) | ||
| HDB 1–3 Room | 19.45 | 18.67 |
| HDB 4–5 Room or Executive Condo | 62.6 | 62.76 |
| Private apartment/condominium/landed property | 17.95 | 18.57 |
| Education (%) | ||
| Primary or lower | 21.86 | 21.16 |
| Secondary | 41.35 | 40.94 |
| Post-secondary without University Degree | 21.04 | 21.58 |
| Post-secondary with University Degree | 15.75 | 16.33 |
| Mean of Monthly Income (SD) | 3969.63 (5030.88) | 4047.96 (5030.88) |
| Self-reported health as Excellent, Very good, or Good (%) | 63.70 | 64.22 |
| Mean of Social Support (SD) | – | 14.46 (3.97) |
| Mean of Network Density (SD) | – | 0.70 (0.33) |
Table 2 reports the proportion of respondents who trusted (“Strongly Trust”, “Somewhat Trust”, or “Slightly Trust”) each source of information. Government sources, local television, and local radio are often seen as ‘formal’ sources of information in Singapore that are regulated by authorities (Lee and Willnat, 2009). These sources were the most trusted among the 6 sources. Social media was the least trusted source, although most respondents still reported trusting in social media for information on COVID-19. Most respondents also trusted informal sources from their social networks, with about 92% trusting their family, and slightly less (88%) trusting their friends.
Table 2.
Sources of information for COVID-19 (N = 6,094).
| Source of Information for COVID-19 | Trust (%) |
|---|---|
| Government Sources | 92.32 |
| Local Television | 93.63 |
| Local Radio | 93.14 |
| Social Media | 60.63 |
| Family | 92.04 |
| Friends | 88.14 |
Table 3 presents the odds ratios of a logistic regression model predicting vaccination status. The results show that respondents who placed greater levels of trust in formal sources of information (government sources, local news on television, and local news on the radio) were significantly more likely to have received at least 1 dose of the COVID-19 vaccine in June 2021. On the other hand, contrary to the idea that informal social networks may influence vaccine willingness among middle-aged and older adults to a greater extent, trust in informal sources (friends and family) did not predict the likelihood of being vaccinated. Social media only slightly predicted vaccination status (p = .09), with those who placed greater trust in social media being less likely to have received at least 1 dose of the vaccine. Respondents who are female (relative to male) and are of Indian ethnicity (relative to being Chinese) are also found to be less likely to have been vaccinated in June 2021, while respondents who lived in wealthier house types (relative to less wealthy house types) and those who rated their own health status more positively were also more likely to have received at least 1 dose of the vaccine. As the odds ratio for monthly income was about 1.00, it was not found to predict vaccination status.
To further explore the hypothesis that trust in different sources of information would be correlated, latent class analysis was subsequently applied to identify typologies according to the different patterns of trust that respondents placed in the sources of information (Table 4). Table 5 presents a simplified categorization of the 4 typologies identified. Based on these categorizations, the following labels were given to the groups based on their patterns of trust for clarity in discussion – Group 1 was labelled ‘Pro-formal Selective’, Group 2 was labelled ‘Broad Trust’, Group 3 was labelled ‘Broad Distrust’, and Group 4 was labelled ‘Pro-informal Selective’.
Table 5.
Simplified categorization of latent class typologies according to level of trust.
| Latent Class | Formal Sources | Social Media | Friends | Family |
|---|---|---|---|---|
| Group 1 | High | Low | Moderate – low | Low |
| Group 2 | High | Moderate – high | High | High |
| Group 3 | Low | Low | Low | Low |
| Group 4 | Low | Moderate – low | High | High |
Note: Trust in each category was classified by the estimated probabilities of trusting each category (p). High: p > .75, Moderate – high: 0.75 > p > .5, Moderate – low: 0.5 > p > .25, Low: p < .25.
Respondents exhibiting ‘Pro-formal Selective’ patterns of trust (Group 1), about 8% of respondents, were likely to trust formal sources (government sources, local news on television, local radio channels) and moderately likely to trust their friends, but did not trust social media and had comparatively low trust in their family. Respondents exhibiting ‘Broad Trust’ patterns of trust (Group 2) had a majority of respondents (86%) and were very likely to trust all sources except for social media. Respondents exhibiting ‘Broad Distrust’ patterns of trust (Group 3), about 4% of respondents, were very unlikely to trust any source of information. Finally, respondents exhibiting ‘Pro-informal Selective’ patterns of trust (Group 4), about 3% of respondents, were unlikely to trust formal sources, but were relatively more likely to trust social media, and were very likely to trust their friends and family. Between typologies, trust in social media as a source ranged from moderate to low and did not vary between groups to the extent that trust in formal sources, and trust in informal sources (friends and family) did. Within each typology, trust in the different formal sources was largely consistent and did not vary much.
The value of the latent groups identified in predicting respondents' vaccination status was then tested through a logistic regression model (Table 6). Results indicate that the latent classes significantly predicted respondents' vaccination status in June 2021 with respondents exhibiting ‘Pro-formal Selective’ trust patterns most likely to have been vaccinated with at least 1 dose, followed firstly by respondents exhibiting ‘Broad trust’ trust patterns, and finally by respondents exhibiting ‘Broad Distrust’ and ‘Pro-informal Selective’ trust patterns with little difference in the effect of these final two patterns of trust. These findings expand on those of the first model (Table 3) by illustrating that the patterns of trust that our respondents exhibited across both formal and informal sources of information also predicts the vaccination status of our respondents in June 2021. In particular, we find that while trust in formal sources of information on its own positively predicts vaccination status, respondents with high trust in formal sources of information while at the same time having lower levels of trust in informal sources of information are more likely to have been vaccinated as compared to respondents who had high levels of trust in both formal and informal sources of information.
Additionally, as with the previous model, respondents who are female, Indian, and who reported lower levels of health were less likely to be vaccinated. Housing type was again found to significantly predict vaccination status, with individuals living in 4–5 Room HDB Flats or Executive Condominiums more likely to be vaccinated than those living in 1–3 Room HDB Flats in June 2021.
4. Discussion
While existing studies on the influence of the sources of information on the willingness to vaccinate have focused predominantly on the usage of such sources, the current study finds evidence that the level of trust that middle-aged and older adults place in sources of information is also important. In particular, greater trust in formal sources of information is found to be associated with being vaccinated. This is congruent with prior studies that have similarly illustrated the importance of trust in sources of information in shaping other health factors, such as smoking behavior (Brown-Johnson et al., 2018) or health literacy (Chen et al., 2018). Specific to COVID-19 vaccination willingness, the belief in conspiracy theories and misinformation about the vaccine has been identified as a significant factor preventing COVID-19 vaccine willingness (Fisk, 2021; Loomba et al., 2021). Higher levels of trust in formal sources that disseminate reliable information are thus likely to prevent the subscription to misinformation, therefore circumventing the barrier of misinformation and the belief in conspiracy theories.
The findings also imply that, contrary to prior studies that have found that the use of social media predicted the willingness to vaccinate (Benis et al., 2021; Jennings et al., 2021; Kumari et al., 2021), trust in social media for information on COVID-19 only slightly predicted the vaccination status of middle-aged and older adults in Singapore. This is possibly because previous studies examined the general population, while the present study focuses on middle-aged and older adults. Middle-aged and older adults have been found to use social media less and significant barriers to using social media which discourage the adoption of such platforms among older populations have also been identified (Charness and Boot, 2009; Leist, 2013). Thus, while the use of social media may be an important factor determining vaccination willingness in other populations, this may not hold true for middle-aged and older adults who may utilize such platforms less. Future research should further explore these preliminary findings and examine the differential influence of social media use amongst middle-aged and older adults on vaccine hesitancy in comparison to other demographic groups.
The results of the latent class analysis also indicate that distinct typologies of trust patterns across different sources of information can be found among middle-aged and older adults, and that these typologies predict the willingness to vaccinate against COVID-19. These findings have several implications. Firstly, selectivity of trust in sources of information – in particular, only placing trust in formal sources and not in informal sources – is found to be associated with a greater willingness to vaccinate, relative to a broad trust in all sources. This is congruent with existing literature on critical health literacy (Nutbeam, 2000, 2008) which argues that the ability to discern reliable from unreliable information is important in shaping health consequences such as health behavior (Chen et al., 2018) which may have been even more critical during the pandemic due to the greater uncertainty in health communication as has been discussed.
Secondly and more specific to the development of interventions, prior studies have suggested the need to use formal sources such as health officials and healthcare professionals as channels for the dissemination of information on COVID-19 vaccines to counter misinformation due to the greater levels of trust that individuals place in these sources (Latkin et al., 2021; Malik et al., 2020). The current findings support such assertions and illustrate that these recommendations would be effective for a large majority of middle-aged and older adults in Singapore as it has been demonstrated that Singaporeans in general have high levels of trust in such sources (Blendon et al., 2006). However, the current findings also illustrate that there are other groups for whom such methods may be less effective - particularly middle-aged and older adults with low trust in formal sources who are also found to be less willing to vaccinate. Thus, while the proportion of middle-aged and older adults in these groups may be small, given the critical need to achieve high rates of vaccination amongst older adults attention should nevertheless be paid to these individuals who may ‘fall through the cracks’ of mainstream strategies.
For such individuals, the findings imply a need for targeted interventions that cater to the specific patterns of trust exhibited to encourage vaccinations. For middle-aged and older adults in the pro-informal selective typology, the findings indicate that a more effective means to encouraging vaccinations would be through the alternative channels such individuals place greater trust in, particularly their informal sources of information such as their friends and family. This supports existing literature on the importance of informal social networks in influencing health behavior (Sentell et al., 2020; Straughan and Adeline, 2000) and the importance of recognizing that formal sources are only a single ‘node’ out of many others in the health decision making process for individuals (Nimmon and Regehr, 2018). Such efforts should supplement strategies to build trust in formal sources which may not be feasible in the short term but are nevertheless important for long-term health policy efforts. As for respondents who were unlikely to trust any source of information (broad distrust typology), the current findings support recommendations that authorities should attempt to build trust through consistent messaging (Lazarus et al., 2021; Machingaidze and Wiysonge, 2021).
The current research faces several limitations. In particular, as mentioned, the media landscape in Singapore is unique due to the government's media censorship laws. As such, specific findings may not be directly translatable to other social and cultural contexts. The analytical methods employed were also cross sectional in nature and prevented any inference of causality between trust in sources of information and vaccination status. Additionally, the authors acknowledge that trust in a particular source of information does not equate to the use of the particular source which was not explored in this paper. Thus, to better inform policymakers and interventions, future research should examine how trust in sources of information may relate to the use of such sources of information within the context of the willingness to vaccinate. Further research should also examine trust in sources at a more granular level, for instance by specifying trust in specific social media platforms, as previous research has elucidated useful insights by examining the usage of social media platforms at this level of specificity (Jennings et al., 2021). Due to the panel nature of the data, the current study also uses variables measured at different time points for the current analysis, most importantly measuring trust in sources of information in November 2020 while measuring vaccination status in June 2021. While the COVID-19 situation was relatively stable and improving in Singapore during this period which may have made it unlikely that public trust in sources of information would not have changed, we acknowledge that sentiments may have changed nevertheless and highlight this as a limitation of the current research. Finally, the current analysis utilizes vaccination status as a proxy for vaccine hesitancy, rather than directly measuring the willingness to vaccinate. While we refine the measure by excluding non-vaccinated respondents who cite being ineligible as a reason for not being vaccinated, this may nevertheless be less accurate in capturing vaccine hesitancy.
To conclude, the COVID-19 pandemic has proven to be unpredictable with the onset of new variants hindering efforts to exit the pandemic (Rubin, 2021). While vaccinations have been largely effective in controlling the virus, it is likely that the vaccination regime against COVID-19 will be prolonged as additional ‘booster’ shots are needed to combat new variants (Erman and Steenhuysen, 2021). It is thus important for policymakers to be equipped with insights that would enable them to effectively roll out vaccines, especially to vulnerable groups such as middle-aged and older adults. While the factors behind vaccine hesitancy remain complex, this paper illustrates a need for targeted interventions with regards to the effective communication of information regarding COVID-19 vaccines to specific groups of older adults.
Authorship
Micah Tan: Conceptualization, Methodology, Formal analysis, Writing – original draft; Paulin Tay Straughan: Supervision, Conceptualization, Writing – review & editing; Grace Cheong: Validation, Data curation, Writing – review & editing.
Declaration of interest
The authors have no known conflict of interest to disclose.
Acknowledgments
This work was supported by The Ngee Ann Kongsi; and the Ministry of Education, Singapore, under its Academic Research Fund Tier 3 program award reference number MOE2019-T3-1-006. The authors also thank the anonymous reviewers for their insightful comments that have improved the article greatly.
Appendix.
Table 7.
Model fit statistics for latent class analysis
| LCA Model | DF | Loglikelihood | AIC | BIC | ABIC | Entropy | LMR Adjusted LRT | Bootstrap LRT |
|---|---|---|---|---|---|---|---|---|
| 2 Classes | 50 | −9601.94 | 19229.881 | 19317.187 | 19275.877 | 0.942 | p < .0001 | p < .0001 |
| 3 Classes | 43 | −8931.785 | 17903.569 | 18037.887 | 17974.333 | 0.977 | p < .0001 | p < .0001 |
| 4 Classes | 36 | −8735.85 | 17525.7 | 17707.028 | 17621.23 | 0.977 | p < .0001 | p < .0001 |
| 5 Classes | 29 | −8706.262 | 17480.523 | 17708.863 | 17600.821 | 0.834 | p < .0001 | p < .0001 |
| 6 Classes | 22 | −8701.158 | 17484.316 | 17759.668 | 17629.381 | 0.909 | p = .2886 | p = .6667 |
References
- Auslander Gail K., Howard Litwin. Social support networks and formal help seeking: differences between applicants to social services and a nonapplicant sample. J. Gerontol. 1990;45(3) doi: 10.1093/geronj/45.3.s112. S112-119. [DOI] [PubMed] [Google Scholar]
- Baruch Yehuda. Response rate in academic studies-A comparative analysis. Hum. Relat. 1999;52(4):421–438. doi: 10.1177/001872679905200401. [DOI] [Google Scholar]
- Benis Arriel, Anna Khodos, Ran Sivan, Levner Eugene, Ashkenazi Shai. Social media engagement and influenza vaccination during the COVID-19 pandemic: cross-sectional survey study. J. Med. Internet Res. 2021;23(3):e25977. doi: 10.2196/25977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blendon Robert J., DesRoches Catherine M., Cetron Martin S., Benson John M., Meinhardt Theodore, Pollard William. Attitudes toward the use of quarantine in A public health emergency in four countries. Health Aff. 2006;25(Suppl. 1):W15–W25. doi: 10.1377/hlthaff.25.w15. [DOI] [PubMed] [Google Scholar]
- Bollyky Thomas J. U.S. COVID-19 vaccination challenges go beyond supply. Ann. Intern. Med. 2021;174(4):558–559. doi: 10.7326/M20-8280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer Paul, Ley Barbara. Whose science do you believe? Explaining trust in sources of scientific information about the environment. Sci. Commun. 2013;35(1):115–137. doi: 10.1177/1075547012441691. [DOI] [Google Scholar]
- Brown-Johnson Cati G., Boeckman Lindsay M., White Ashley H., Burbank Andrea D., Paulson Sjonna, Beebe Laura A. Trust in health information sources: survey analysis of variation by sociodemographic and tobacco use status in Oklahoma. JMIR Public Health and Surveillance. 2018;4(1):e6260. doi: 10.2196/publichealth.6260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casiday Rachel, Cresswell Tricia, Wilson Deb, Panter-Brick Catherine. A survey of UK parental attitudes to the MMR vaccine and trust in medical authority. Vaccine. 2006;24(2):177–184. doi: 10.1016/j.vaccine.2005.07.063. [DOI] [PubMed] [Google Scholar]
- Channel News Asia COVID-19 vaccination for people aged 60 to 69 brought forward, invitations to go out in ‘next few days’: moh. CNA. 2021 https://www.channelnewsasia.com/singapore/covid-19-vaccination-seniors-60-69-brought-forward-314136 [Google Scholar]
- Channel News Asia The big read: conspiracy theories, scientific misinterpretations, plain ignorance abound in COVID-19 infodemic. Channel News Asia. 2021 https://www.channelnewsasia.com/singapore/covid-19-information-conspiracy-theories-pofma-experts-1851986 [Google Scholar]
- Charness Neil, Boot Walter R. Aging and information technology use: potential and barriers. Curr. Dir. Psychol. Sci. 2009;18(5):253–258. doi: 10.1111/j.1467-8721.2009.01647.x. [DOI] [Google Scholar]
- Chen Xuewei, Hay Jennifer L., Waters Erika A., Kiviniemi Marc T., Biddle Caitlin, Schofield Elizabeth, Li Yuelin, Kaphingst Kimberly, Orom Heather. Health literacy and use and trust in health information. J. Health Commun. 2018;23(8):724–734. doi: 10.1080/10810730.2018.1511658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly Michael, Jones Andrew, Robinson Eric. Public trust and willingness to vaccinate against COVID-19 in the US from october 14, 2020, to March 29, 2021. JAMA. 2021;325(23):2397–2399. doi: 10.1001/jama.2021.8246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erman Michael, Steenhuysen Julie. Reuters; 2021. Pfizer, BioNTech to Seek Authorization for COVID Booster Shot as Delta Variant Spreads.https://www.reuters.com/business/healthcare-pharmaceuticals/pfizer-ask-fda-authorize-booster-dose-covid-vaccine-delta-variant-spreads-2021-07-08/ [Google Scholar]
- Fisk Rebecca J. Barriers to vaccination for coronavirus disease 2019 (COVID-19) control: experience from the United States. Global Health Journal. 2021;5(1):51–55. doi: 10.1016/j.glohj.2021.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller-Iglesias Heather R., Webster Noah J., Antonucci Toni C. The complex nature of family support across the life span: implications for psychological well-being. Dev. Psychol. 2015;51(3):277–288. doi: 10.1037/a0038665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granovetter Mark. In: Networks And Organizations: Structure, Form, and Action. Nohria N., Eccles R.G., editors. Harvard Business School Press; Boston, MA: 1992. Problems of explanation in economic sociology; pp. 25–56. [Google Scholar]
- Harvey Idethia S., Alexander Kezia. Perceived social support and preventive health behavioral outcomes among older women. J. Cross Cult. Gerontol. 2012;27(3):275–290. doi: 10.1007/s10823-012-9172-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt Kristoffer, Adam Shehata, Strömbäck Jesper, Ljungberg Elisabet. Age and the effects of news media attention and social media use on political interest and participation: do social media function as leveller? Eur. J. Commun. 2013;28(1):19–34. doi: 10.1177/0267323112465369. [DOI] [Google Scholar]
- Huxhold Oliver, Fiori Katherine L., Windsor Tim D. The dynamic interplay of social network characteristics, subjective well-being, and health: the costs and benefits of socio-emotional selectivity. Psychol. Aging. 2013;28(1):3–16. doi: 10.1037/a0030170. [DOI] [PubMed] [Google Scholar]
- IPS Exchange Series . Institute of Policy Studies, National University Singapore; Singapore: 2021. Singaporean's Susceptibility To False Information. 19. [Google Scholar]
- Jennings Will, Stoker Gerry, Bunting Hannah, Valgarðsson Viktor Orri, Gaskell Jennifer, Devine Daniel, McKay Lawrence, Mills Melinda C. Lack of trust, conspiracy beliefs, and social media use predict COVID-19 vaccine hesitancy. Vaccines. 2021;9(6):593. doi: 10.3390/vaccines9060593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumari Archana, Ranjan Piyush, Chopra Sakshi, Kaur Divjyot, Kaur Tanveer, Datt Upadhyay Ashish, Abraham Isaac Joshua, Kasiraj Rhytha, Prakash Bindu, Kumar Parmeshwar, Dwivedi Sada Nand, Naval K., Vikram Knowledge, barriers and facilitators regarding COVID-19 vaccine and vaccination programme among the general population: a cross-sectional survey from one thousand two hundred and forty-nine participants. Diabetes & Metabolic Syndrome. 2021;15(3):987–992. doi: 10.1016/j.dsx.2021.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurohi Rei. The Straits Times; 2021. Ministers Urge More Seniors to Get Vaccinated against Covid-19 Ahead of Singapore's Further Reopening.https://www.straitstimes.com/singapore/ministers-urge-more-seniors-to-get-vaccinated-ahead-of-further-reopening [Google Scholar]
- Larson Heidi J., Clarke Richard M., Jarrett Caitlin, Eckersberger Elisabeth, Levine Zachary, Schulz Will S., Paterson Pauline. Measuring trust in vaccination: a systematic review. Hum. Vaccines Immunother. 2018;14(7):1599–1609. doi: 10.1080/21645515.2018.1459252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latkin Carl A., Dayton Lauren, Miller Jacob R., Yi Grace, Jaleel Afareen, Nwosu Chikaodinaka C., Cui Yang, Falade-Nwulia Oluwaseun. Behavioral and attitudinal correlates of trusted sources of COVID-19 vaccine information in the US. Behav. Sci. 2021;11(4):56. doi: 10.3390/bs11040056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus Jeffrey V., Ratzan Scott C., Adam Palayew, Gostin Lawrence O., Larson Heidi J., Rabin Kenneth, Spencer Kimball, El-Mohandes Ayman. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2021;27(2):225–228. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Terence, Willnat Lars. In: 101–19 in Political Communication In Asia. Lee T., Aw A., editors. Routledge; 2009. Media management and political communication in Singapore. [Google Scholar]
- Leist Anja K. Social media use of older adults: a mini-review. Gerontology. 2013;59(4):378–384. doi: 10.1159/000346818. [DOI] [PubMed] [Google Scholar]
- Lim Jessie, Kwee Ivan. The Straits Times; 2021. 24 People Get Covid-19 Vaccination at Home under Ongoing Pilot Project.https://www.straitstimes.com/singapore/24-people-vaccinated-at-home-under-ongoing-pilot-project [Google Scholar]
- Lim Min Zhang. The Straits Times; 2021. “Bigger Push to Vaccinate More Seniors: Ong Ye Kung.”.https://www.straitstimes.com/singapore/bigger-push-to-vaccinate-more-seniors-ong-ye-kung [Google Scholar]
- Long Victoria J.E., Koh Wei Shien, Saw Young Ern, Liu Jean C. Vulnerability to rumours during the COVID-19 pandemic in Singapore. Ann. Acad. Med. Singapore. 2021;50(3):232–240. [PubMed] [Google Scholar]
- Loomba Sahil, de Figueiredo Alexandre, Piatek Simon J., de Graaf Kristen, Larson Heidi J. Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nature Human Behaviour. 2021;5(3):337–348. doi: 10.1038/s41562-021-01056-1. [DOI] [PubMed] [Google Scholar]
- Machingaidze Shingai, Wiysonge Charles Shey. Understanding COVID-19 vaccine hesitancy. Nat. Med. 2021:1–2. doi: 10.1038/s41591-021-01459-7. [DOI] [PubMed] [Google Scholar]
- Malik Amyn A., McFadden SarahAnn M., Elharake Jad, Omer Saad B. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020;26:100495. doi: 10.1016/j.eclinm.2020.100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merkley Eric, Loewen Peter J. Anti-intellectualism and the mass public's response to the COVID-19 pandemic. Nature Human Behaviour. 2021;5(6):706–715. doi: 10.1038/s41562-021-01112-w. [DOI] [PubMed] [Google Scholar]
- Ministry of Health Government accepts recommendations of expert committee on COVID-19 vaccination. Ministry of Health. 2020 https://www.moh.gov.sg/news-highlights/details/government-accepts-recommendations-of-expert-committee-on-covid-19-vaccination [Google Scholar]
- Nguyen Kimberly H., Srivastav Anup, Razzaghi Hilda, Williams Walter, Lindley Megan C., Jorgensen Cynthia, Abad Neetu, Singleton James A. COVID-19 vaccination intent, perceptions, and reasons for not vaccinating among groups prioritized for early vaccination — United States, september and december 2020. Am. J. Transplant. 2021;21(4):1650–1656. doi: 10.1111/ajt.16560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nimmon Laura, Regehr Glenn. The complexity of patients' health communication social networks: a broadening of physician communication. Teach. Learn. Med. 2018;30(4):352–366. doi: 10.1080/10401334.2017.1407656. [DOI] [PubMed] [Google Scholar]
- Nutbeam Don. Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot. Int. 2000;15(3):259–267. doi: 10.1093/heapro/15.3.259. [DOI] [Google Scholar]
- Nutbeam Don. The evolving concept of health literacy. Soc. Sci. Med. 2008;67(12):2072–2078. doi: 10.1016/j.socscimed.2008.09.050. [DOI] [PubMed] [Google Scholar]
- Paul Elise, Steptoe Andrew, Fancourt Daisy. Anti-vaccine attitudes and risk factors for not agreeing to vaccination against COVID-19 amongst 32,361 UK adults: implications for public health communications. MedRxiv 2020. 2020;10.21:20216218. doi: 10.1101/2020.10.21.20216218. [DOI] [Google Scholar]
- Penning Margaret J. Health, social support, and the utilization of health services among older adults. J. Gerontol.: Ser. Bibliogr. 1995;50B(5):S330–S339. doi: 10.1093/geronb/50B.5.S330. [DOI] [PubMed] [Google Scholar]
- Perrin Andrew. Pew Research Centre; United States: 2015. Social Media Usage: 2005-2015. [Google Scholar]
- Prickett Kate C., Simon Chapple. Trust in government and covid-19 vaccine hesitancy. Policy Quarterly. 2021;17(3) doi: 10.26686/pq.v17i3.7135. [DOI] [Google Scholar]
- Reuters Singapore about-turns on masks, making them compulsory in virus fight. Reuters. 2020 https://www.reuters.com/article/us-health-coronavirus-singapore-idUSKCN21W1EW [Google Scholar]
- Ritchie Hannah, Mathieu Edouard, Rodés-Guirao Lucas, Appel Cameron, Giattino Charlie, Ortiz-Ospina Esteban, Joe Hasell, Macdonald Bobbie, Beltekian Diana, Roser Max. Coronavirus pandemic (COVID-19) Our World in Data. 2020 https://ourworldindata.org/coronavirus/country/singapore [Google Scholar]
- Romer Daniel, Jamieson Kathleen H. Conspiracy theories as barriers to controlling the spread of COVID-19 in the U.S. Soc. Sci. Med. 2020;263:113356. doi: 10.1016/j.socscimed.2020.113356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin Rita. COVID-19 vaccines vs variants—determining how much immunity is enough. JAMA. 2021;325(13):1241–1243. doi: 10.1001/jama.2021.3370. [DOI] [PubMed] [Google Scholar]
- Sentell Tetine, Joy Agner, Pitt Ruth, Davis James, Guo Mary, McFarlane Elizabeth. Considering health literacy, health decision making, and health communication in the social networks of vulnerable new mothers in Hawai‘i: a pilot feasibility study. Int. J. Environ. Res. Publ. Health. 2020;17(7):2356. doi: 10.3390/ijerph17072356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherbourne Cathy D., Stewart Anita L. The MOS social support survey. Social Science & Medicine (1982. 1991;32(6):705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- Straughan Paulin T., Adeline Seow. Attitudes as barriers in breast screening: a prospective study among Singapore women. Soc. Sci. Med. 2000;51(11):1695–1703. doi: 10.1016/s0277-9536(00)00086-1. [DOI] [PubMed] [Google Scholar]
- Tan Micah, Straughan Paulin, Lim Wensi, Cheong Grace. Centre for Research on Successful Ageing, Singapore Management University; Singapore: 2021. ROSA Special Report on COVID-19 Vaccination Trends Among Older Adults in Singapore. [Google Scholar]
- Teo Joyce. Why S’pore is back to phase 2: hospital capacity, community exposure to covid-19 among key considerations. The Straits Times. 2021 https://www.straitstimes.com/singapore/health/hospital-capacity-seniors-vaccination-numbers-community-exposure-to-covid-19 [Google Scholar]
- Teo Kai Xiang. Civil society responses to Singapore's online ‘fake news’ law. Int. J. Commun. 2021;15(0):4795–4815. 0. [Google Scholar]
- van Tilburg Theo. Losing and gaining in old age: changes in personal network size and social support in a four-year longitudinal study. J. Gerontol. Ser. Bibliogr. 1998;53B(6):S313–S323. doi: 10.1093/geronb/53B.6.S313. [DOI] [PubMed] [Google Scholar]
- Trent Mallory, Seale Holly, Chughtai Abrar A., Salmon Daniel, Raina MacIntyre C. Trust in government, intention to vaccinate and COVID-19 vaccine hesitancy: a comparative survey of five large cities in the United States, United Kingdom, and Australia. Vaccine. 2021 doi: 10.1016/j.vaccine.2021.06.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullah Irfan, Khan Kiran S., Tahir Muhammad J., Ahmed Ali, Harapan Harapan. Myths and conspiracy theories on vaccines and COVID-19: potential effect on global vaccine refusals. Vacunas. 2021;22(2):93–97. doi: 10.1016/j.vacun.2021.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaithianathan Rhema, Hool Bryce, Hurd Michael D., Rohwedder Susann. High-frequency internet survey of a probability sample of older Singaporeans: the Singapore life panel®. Singapore Econ. Rev. 2018;1842004 doi: 10.1142/S0217590818420043. [DOI] [Google Scholar]
- Walker Mark H. The contingent value of embeddedness: self-affirming social environments, network density, and well-being. Soc. Ment. Health. 2015;5(2):128–144. doi: 10.1177/2156869315574601. [DOI] [Google Scholar]
- Weller Bridget E., Bowen Natasha K., Faubert Sarah J. Latent class Analysis: a guide to best practice. J. Black Psychol. 2020;46(4):287–311. doi: 10.1177/0095798420930932. [DOI] [Google Scholar]
- Wilson Anne E., Parker Victoria A., Matthew Feinberg. Polarization in the contemporary political and media landscape. Current Opinion in Behavioral Sciences. 2020;34:223–228. doi: 10.1016/j.cobeha.2020.07.005. [DOI] [Google Scholar]
- Wong Catherine M.L., Jensen Olivia. The paradox of trust: perceived risk and public compliance during the COVID-19 pandemic in Singapore. J. Risk Res. 2020;23(7–8):1021–1030. doi: 10.1080/13669877.2020.1756386. [DOI] [Google Scholar]