Abstract
PURPOSE
Social integration and relationship issues have been understudied among adolescent and young adult (AYA) cancer survivors. This study compared social relationships (social networks, support, and isolation) between AYA cancer survivors and noncancer controls, and identified social integration mechanisms through which the cancer experience influences patient-reported outcomes (PROs).
MATERIALS AND METHODS
One hundred two AYA cancer survivors and 102 age, sex, and race-matched noncancer controls from a national Internet panel completed an online survey to identify up to 25 of closest friends and relatives whom they have contacted within the past 2 years. Participants' interpersonal connections were used to create a social network index. The Duke-UNC Functional Social Support Questionnaire, UCLA Loneliness Scale, and PROMIS-29 Profile were used to measure social support, perceived isolation or loneliness, and PROs (physical functioning, pain interference, fatigue, anxiety, and depression domains), respectively. Path analysis tested effects of cancer experience on PROs using serial social relationship variables as mediators.
RESULTS
Compared with controls, survivors of lymphoma, leukemia, and solid tumor had better social networks; however, survivors of solid tumor and central nervous system malignancies had higher perceived loneliness (all P values < .05). Cancer experience was directly associated with poor PROs (P values < .05 for all domains except fatigue) and indirectly associated through the social network-support-loneliness pathway (all P values < .05). Survivors with higher loneliness had lower physical functioning and higher pain interference, fatigue, anxiety, and depression versus controls with lower loneliness (all P values < .05).
CONCLUSION
Compared with controls, survivors were more socially connected but experienced greater loneliness, which was associated with poorer PROs. Screening social integration issues during follow-up care and providing appropriate interventions are warranted.
INTRODUCTION
Nearly 89,000 adolescents and young adults (AYAs) between age 15 and 39 years are diagnosed with cancer in the United States annually.1 This number is eight times that of individuals diagnosed with cancer between age 0 and 14 years.1 The AYA HOPE study found poorer self-reported physical and mental health in survivors age 25-44 years compared with the US general population.2 In contrast to noncancer controls, AYA survivors are more likely to experience various late effects.3,4 AYAs are in a critical developmental stage,5,6 inclusive of completing education, pursuing employment, establishing economic independence, finding a life partner, and forming a family. However, cancer experience during young adulthood may delay the achievement of these milestones, which require a great degree of connection to the society.7
CONTEXT
Key Objective
Previous studies have reported poorer social outcomes in adolescent and young adult (AYA) cancer survivors (eg, lower educational attainment and higher unemployment) compared with noncancer controls. Instead, this study explored social integration issues (social network, social support, and perceived loneliness) and the associations with patient-reported outcomes (PROs) in AYA cancer survivors and evaluated different social integration as pathways through cancer experience impacts PROs.
Knowledge Generated
Using a novel online platform to measure social integration, we found that compared with noncancer controls, AYA cancer survivors have better social networks; however, they perceived greater loneliness, which was associated with poorer PROs. In addition, cancer experience was directly and indirectly (through complex social integration pathways) associated with poor PROs.
Relevance
Screening social isolation and integration issues from the early stage throughout the follow-up care and providing appropriate psychosocial interventions to strengthen social integration might help to improve PROs in AYA cancer survivors.
The Childhood Cancer Survivor Study (CCSS) and St Jude Lifetime Cohort Study (SJLIFE) have reported poorer social outcomes of childhood cancer survivors compared with noncancer siblings and community controls, typically lower educational attainment, higher unemployment, higher proportion not married, and more likely to be living dependently.8,9 Survivors diagnosed with CNS tumors age between 15 and 20 years were more likely to attend special education programs compared with their siblings.10 A previous study by Kirchhoff et al11 found that AYA cancer survivors were at an increased risk of divorce compared with noncancer controls. However, social integration that involves connections and interactions between AYA cancer survivors and society and the associations with health outcomes are understudied.
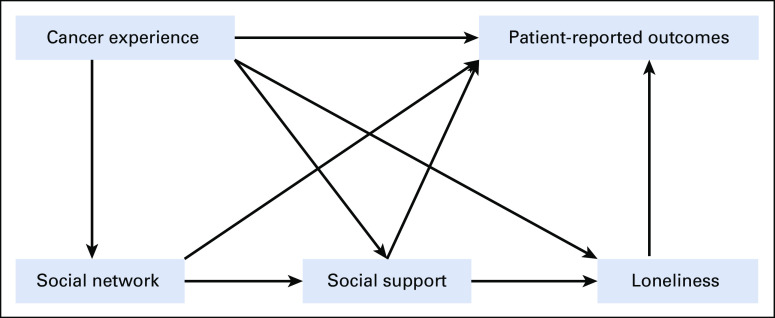
To bridge the gap, we adopted a framework proposed by Berkman et al12 (Appendix Fig A1) to investigate the influence of serial social integration variables (social network, social support, and perceived loneliness) on health outcomes among AYA cancer survivors. This framework articulates that appropriate ties or connections among individuals are the cornerstones to form social relations,13 which influence the health of an individual either directly or indirectly through mechanisms including more social supports and perceived less social isolation. Evidence suggests higher perceived intimacy and connectedness as key elements of social bonding have been associated with better physical and mental well-being and adherence to healthy behaviors,14 whereas lack of social ties, disconnectedness, and disintegration are associated with poorer health outcomes.12,15 In fact, adolescent cancer survivors have reported feeling socially disconnected or isolated.16 To our knowledge, some previous studies have applied the Berkman's framework, consisting of marital status, frequency of contact with friends and relatives, and membership in church and community organizations, to measure social network status for cancer populations, including survivors of colorectal17,18 and breast19,20 cancer.
Loneliness is a perceived social isolation and has received great attention recently,21,22 particularly relevant to suicidal ideation in the general population.23 A meta-analysis found that loneliness is associated with 26% elevated risk of premature mortality.24 Lonelier individuals are more likely to have pain, poorer physical functioning, depression, and fatigue in contrast to socially connected individuals.21 Longitudinal studies suggest that lonely cancer survivors have persistent clusters of multiple symptoms compared with less lonely individuals25 and that persistent symptoms occur through the altering of body physiology or neuroimmune pathways.26 Feelings of loneliness accompanied by anxiety, stress, and low self-confidence can trigger behavioral and neurobiologic pathways, leading to adverse health consequences.27
Previous studies have explored social integration issues in aging cancer survivors28,29; however, the social relationships in AYA cancer survivors and their influence on patient-reported outcomes (PROs) require thorough investigations. PROs, especially symptoms and poor quality of life, are prognostic factors for early onset of clinically ascertained health conditions and reduced survival in cancer populations.30,31 This study aimed to investigate social relationships and associations with PROs in AYA cancer survivors, with an inclusion of age, sex, and race-matched noncancer AYAs as a control group. Specifically, we (1) compared three social relationship variables (social network, social support, and perceived loneliness) between two AYA groups and (2) evaluated the contribution of social relationship variables to poor PROs.
MATERIALS AND METHODS
Study Design and Participants
This cross-sectional study included 102 AYA cancer survivors and 102 age, sex, and race-matched noncancer controls. We recruited participants from a national Internet survey panel maintained by Opinions 4 Good (Portsmouth, NH). Through the database of panel members, Opinions 4 Good identified a random sample of AYAs and sent an invitation e-mail with enclosed screening items to determine their eligibility. During the screening, survivors self-reported the type of cancer diagnosis, age at diagnosis, type of cancer treatment, and years from therapy completion. The enrollment criteria for survivors were individuals age 18-29.9 years at the time of survey, diagnosed with cancer at age 15-29.9 years as defined by the US National Cancer Institute's SEER program,32 and received no cancer therapy in the past 3 years. Our age criterion32 to define AYA cancer survivors is slightly different from the criteria (eg, age 15-39 years) used by various professional organizations.33,34 The enrollment criteria for noncancer controls were age 18-29.9 years at the time of survey with no history of cancer.
We used a quota sampling approach to recruit participants on the basis of age at enrollment, sex, race and ethnicity, and cancer diagnosis per the distribution of AYA cancer survivors in the CCSS. We used the same age, sex, and race and ethnicity criteria to select the matched noncancer controls. Data from survivors and controls were collected at the same period. If the eligible participants did not respond to our invitation, they were replaced by alternative participants with similar age, sex, race and ethnicity, and cancer diagnosis. This process was repeated until all prespecified slots were fulfilled. The participants were rewarded points when their survey was completed. The points earned from this and other studies could be redeemed if the threshold was reached. This study was approved by the IRB of St Jude Children's Research Hospital.
Data Collection
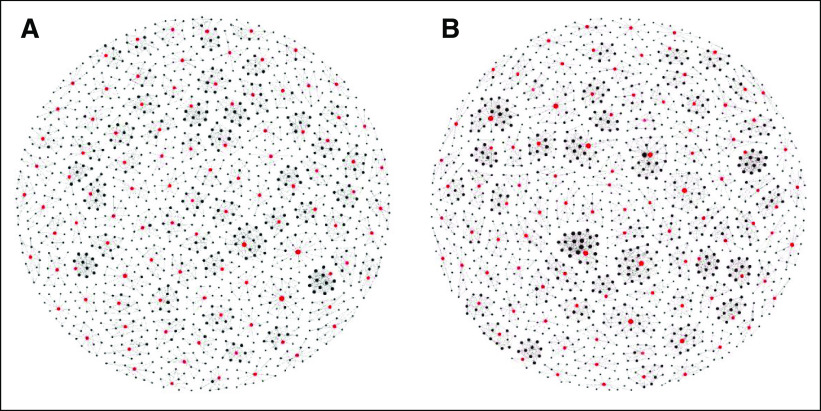
Data were collected between March and May 2015 through an online platform designed for social network research. Participants who were consented to this study completed a self-administered survey via smartphones, tablets, or desktop computers. The average survey length time was 30 minutes. The ordering of the survey includes demographics, cancer history, health habits, medical conditions, personal social network status, tangible and intangible support, loneliness, and PROs. If some items were not completed, the data collection platform will prompt a reminder for completion. We collected social network data using an egocentric approach, where participants reported their social relationship with friends and relatives without a confirmation from friends and relatives. Participants identified up to 25 close friends and relatives with whom they frequently contacted in the past 2 years and reported whether any of those friends and relatives knew and contacted each other. Each participant was asked about the type of relationship, type of communication used, and frequency of contact with each identified friend and relative. Additionally, participants reported resources available to them for emotional support, tangible support, physical activity advice, and weight management advice from each of the identified friends and relatives. A social network index created in our previous publication was used for each individual, with a higher score representing a stronger social network status.35 Approximately 5,000 social connectedness data elements were collected from 204 participants and included in the analysis (Fig 1).
FIG 1.
Social connectedness map representing (A) 102 AYA cancer survivors and (B) 102 age, sex, and race-matched noncancer controls. Note: Red dots represent participants and black dots represent participants' friends and relatives. AYA, adolescent and young adult.
Measures
PROs were collected using the Patient-Reported Outcomes Measurement Information System-29 Profile (PROMIS-29)36 with a focus on five domains of interest: physical functioning, pain interference, fatigue, anxiety, and depression. Higher scores in the physical functioning domain indicated better PROs, whereas higher scores in other domains indicated poorer PROs. Perceived social support was assessed using the Duke-UNC Functional Social Support Questionnaire (8 items),37 with higher domain scores indicating better satisfaction with social support. Perceived loneliness was assessed using the UCLA Loneliness Scale (20 items),38 with higher domain scores indicating more perceived isolation. We further defined high level of loneliness if domain scores were ≥ 30 and low loneliness if scores were < 30.38
Participants self-reported their sociodemographic characteristics (age, sex, race and ethnicity, educational attainment, annual household income, and marital status) and the presence of 15 chronic health conditions on the basis of a checklist (footnote of Table 1). Race and ethnicity was categorized as non-Hispanic White, non-Hispanic Black, Hispanic, and others; educational attainment as high school or below, college, and graduate levels; annual household income as < $40,000, $40,000-$75,999, and ≥ $80,000 (US dollars); and marital status as not married and married (ie, married or living with partner).
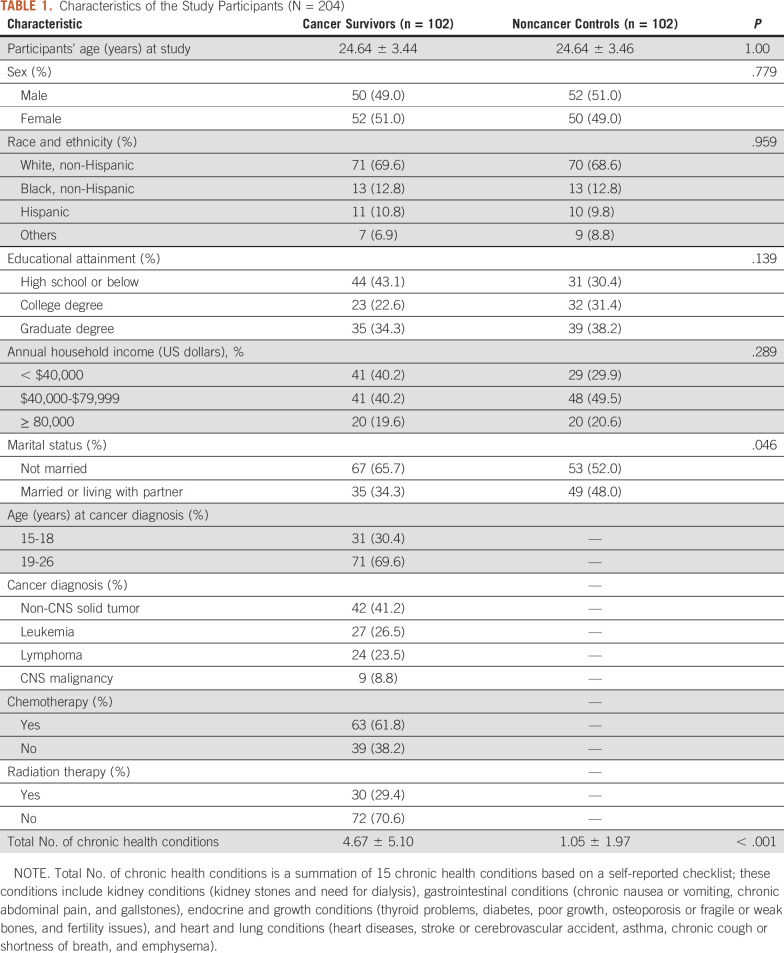
TABLE 1.
Characteristics of the Study Participants (N = 204)
Statistical Analysis
Chi-square tests were used to compare sociodemographic characteristics between survivors and controls. Multivariable linear regression analysis, adjusting for the number of chronic health conditions, was used to compare social network, social support, and perceived loneliness between survivors and controls. Path analysis was used to quantify total, direct, and indirect effects of cancer experience (v noncancer) on each of the PRO domains using serial social relationship variables (social network, social support, and perceived loneliness) as mediators. Total effect was estimated by the sum of direct and indirect effects. Mplus version 8 was used for path analysis39 and Stata version 15 for the remaining analyses.
RESULTS
Table 1 summarizes the characteristics of participants (N = 204). Sociodemographic characteristics did not significantly differ between survivors and noncancer controls (P values > .05), except for marital status (P value = .046). A lower proportion of survivors were married or living with partners compared with controls (34.3% v 48.0%; P value = .046). Among survivors, 69.6% were diagnosed with cancer at age 19-26 years and 30.4% at age 15-18 years; 41.2% were treated for a non-CNS solid tumor, 26.5% for leukemia, 23.5% for lymphoma, and 8.8% for a CNS malignancy. Survivors had a higher total number of chronic health conditions compared with controls (4.7 v 1.1; P value < .001).
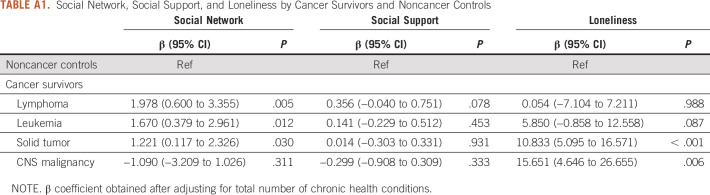
Appendix Table A1 compared social relationship variables between survivors and controls, adjusting for the number of present chronic health conditions. In contrast to controls, survivors of lymphoma, leukemia, and non-CNS solid tumor had significantly higher social network scores (β 1.978, 95% CI 0.600 to 3.355; β 1.670, 95% CI 0.379 to 2.961; and β 1.221, 95% CI 0.117 to 2.326, respectively). However, solid tumor and CNS malignancy survivors reported significantly higher loneliness scores compared with controls (β 10.833, 95% CI 5.095 to 16.571 and β 15.651, 95% CI 4.646 to 26.655, respectively). Perceived social support among cancer survivors and noncancer controls were comparable (P value > .05).
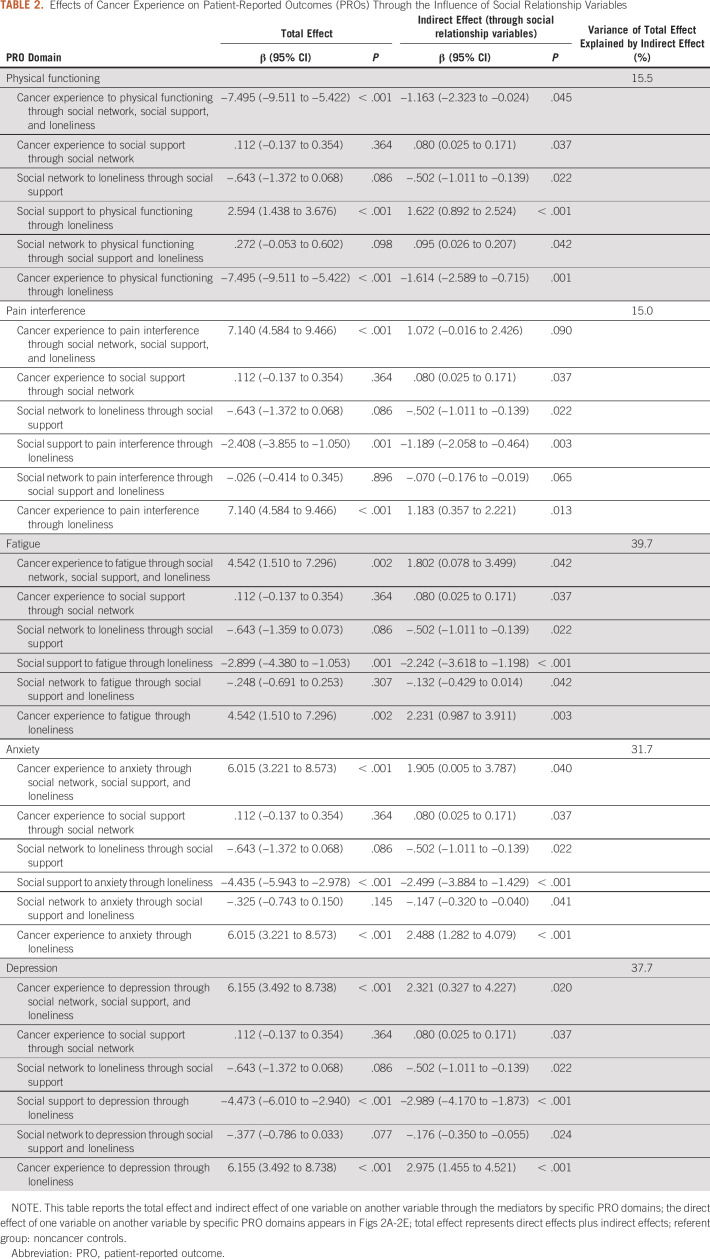
Figure 2 visualizes the significant direct effect from one variable to another variable, and Table 2 reports the total effect and indirect effect of one variable on another variable through the mediators by specific PRO domains. For physical functioning, survivors reported significantly poorer domain scores (β −7.495, 95% CI −9.511 to −5.422) compared with controls. Cancer experience directly explained 84.5% of variance in poor physical functioning. For pain interference, survivors had significantly poorer domain scores (β 7.140, 95% CI 4.584 to 9.466) compared with controls. Cancer experience directly explained approximately 85% of variance in pain interference. For fatigue, survivors reported significantly poorer domain scores (β 4.542, 95% CI 1.510 to 7.296) compared with controls, with no statistically significant direct effect of cancer experience. For anxiety, survivors had significantly poorer domain scores (β 6.015, 95% CI 3.221 to 8.573) compared with controls, with 68.3% of variance in anxiety directly explained by cancer experience. For depression, survivors had significantly poorer domain scores (β 6.155, 95% CI 3.492 to 8.738) compared with controls, with 62.3% of variance in depression directly explained by cancer experience.
FIG 2.
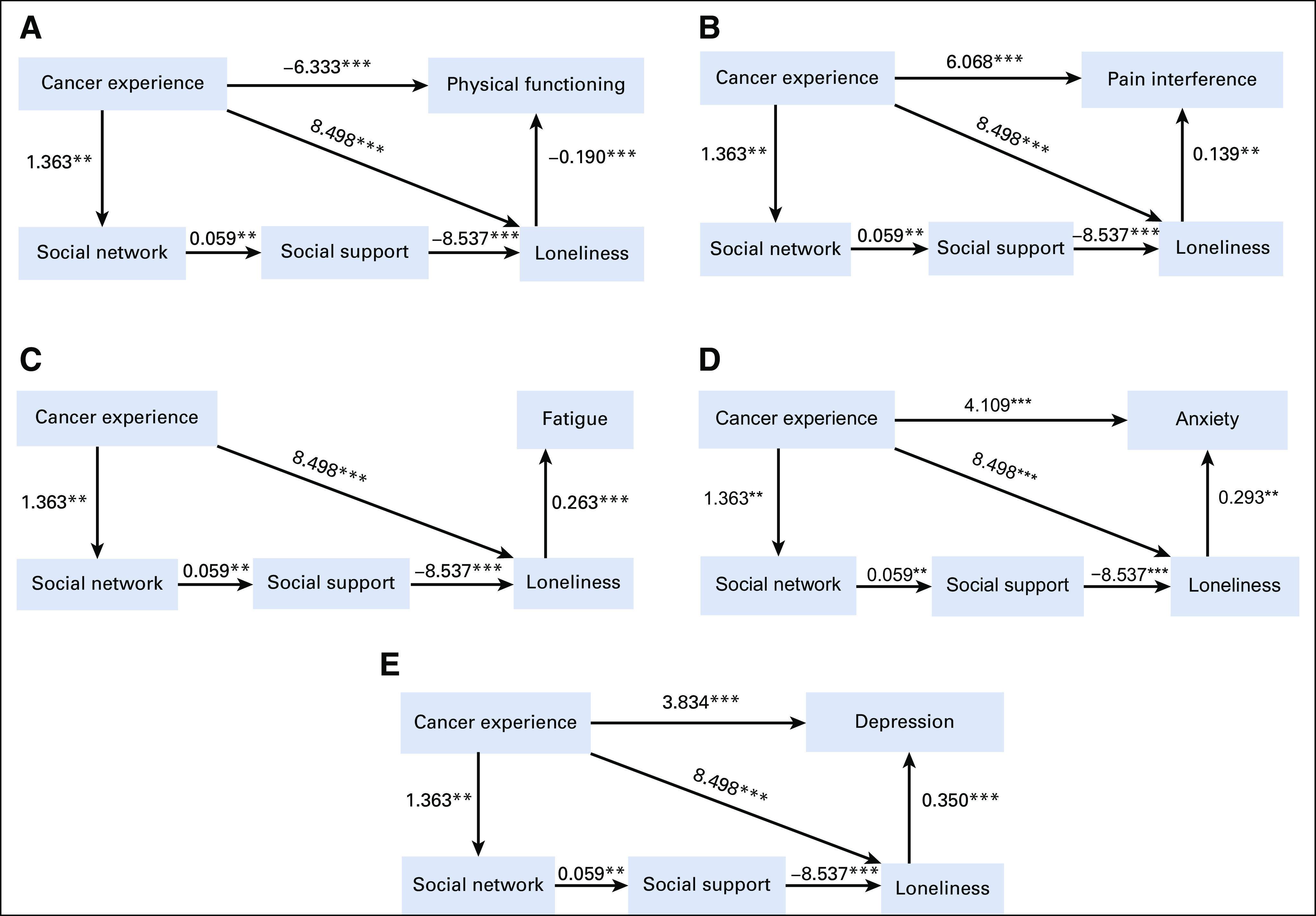
Direct effects of one variable on another variable by specific PRO domains (eg, cancer experience on physical functioning, cancer experience on loneliness, loneliness on physical functioning, etc): (A) all significant direct effects between variables within physical functioning domain, (B) all significant direct effects between variables within pain interference, (C) all significant direct effects between variables within fatigue domain, (D) all significant direct effects between variables within anxiety domain, and (E) all significant direct effects between variables within depression domain. Values alongside the lines represent significant direct effects; *P < .05; **P < .01; ***P < .001. PRO, patient-reported outcome.
TABLE 2.
Effects of Cancer Experience on Patient-Reported Outcomes (PROs) Through the Influence of Social Relationship Variables
Table 2 shows the effect of cancer experience on PRO domains indirectly through the influence of social relationship variables (ie, different indirect effects or pathways). Cancer experience was indirectly associated with poor physical functioning through all three social relationship variables (β −1.163, 95% CI −2.323 to −0.024) and perceived loneliness alone (β −1.614, 95% CI −2.589 to −0.715). Poor social networks were indirectly associated with poor physical functioning through both poor social support and loneliness (β 0.095, 95% CI 0.026 to 0.207). Cancer experience was indirectly associated with fatigue, anxiety, and depression through all three social relationship variables (β 1.802, 1.905, and 2.321, respectively; all P values < .05). Furthermore, cancer experience was indirectly associated with pain interference, fatigue, anxiety, and depression through perceived loneliness (β 1.183, 2.231, 2.488, and 2.975, respectively; all P values < .05). Additionally, poor social networks were indirectly associated with anxiety and depression through both poor social support and loneliness.
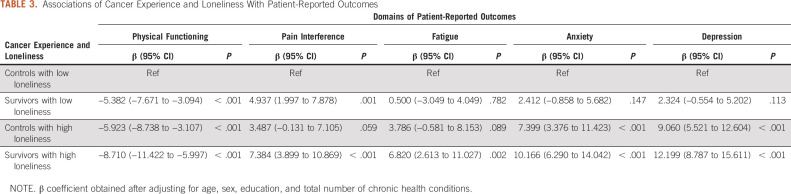
Table 3 shows associations of cancer experience and levels of loneliness with PROs. Compared with controls having low loneliness, survivors having high loneliness had poorest PROs, typically in physical functioning, anxiety, and depression, followed by controls having high loneliness and survivors having low loneliness. The decreased PROs between survivors with high loneliness and controls with low loneliness were up to 2-fold the minimal important difference or MID (note, 1 MID is 5 points) including depression (β 12.199, 95% CI 8.787 to 15.611), anxiety (β 10.166, 95% CI 6.290 to 14.042), poor physical functioning (β −8.710, 95% CI −11.422 to −5.997), pain interference (β 7.384, 95% CI 3.899 to 10.869), and fatigue (β 6.820, 95% CI 2.613 to 11.027).
TABLE 3.
Associations of Cancer Experience and Loneliness With Patient-Reported Outcomes
DISCUSSION
This study used an established social integration framework12 to elucidate the mechanistic influence of the AYA cancer experience on PROs through three social relationship variables (social network connection, social support, and perceived loneliness). We found that experiencing cancer had both direct and indirect associations (via three social relationship variables) with poor PROs in AYAs. Having better social network connection was significantly associated with more social supports and lower levels of loneliness, leading to better PROs.
Although poor social outcomes (eg, educational attainment, income, employment, and insurance status) have been well-characterized in childhood cancer survivors, the social relationship issue is understudied.40 Among the limited literature, Tremolada et al41 found that survivors often lacked social support from family, friends, and significant others compared with controls; however, survivors declared better health-related quality of life potentially because of increased resiliency over time. In addition, Soares et al42 found significant associations of social network and social support with lower levels of fatigue among cancer survivors. Although previous studies found the impact of cancer therapy on different PROs among AYA cancer survivors,43,44 these studies did not elucidate the social network pathway through which cancer therapy affects PROs.
Of the social relationship variables we studied, perceived social isolation or loneliness is of particular concern among cancer populations and deserves additional attention. Prevalence of perceived loneliness is increasing in our society across all ages, and lonelier individuals are at risk for premature mortality.24 Adams et al45 observed that social constraints increase cancer-specific loneliness, which in turn elevates symptom perception (pain interference, fatigue, sleep disturbance, and cognitive complaints). Among adult survivors of childhood cancer, those experiencing loneliness were found to have elevated risk for suicidal ideation and early mortality.46,47 In our study, as compared with controls with low loneliness, AYA cancer survivors with high loneliness had significantly poorer physical functioning and higher pain interference, fatigue, anxiety, and depression, followed by survivors with low loneliness and then controls with high loneliness. Our findings suggest the effect of cancer experience on PROs depends upon the levels of social isolation or loneliness. From a physiologic aspect, stressful situations associated with loneliness can affect immune function and elevate proinflammatory cytokines.48 Future studies are warranted to elucidate biologic and physiologic pathways by which loneliness affects late effects in cancer survivors.
Social integration challenges may vary among survivors experiencing different types of cancers. We found that solid tumor and CNS AYA cancer survivors had greater loneliness compared with survivors of other cancers. One previous study found that AYA survivors of CNS tumor reported poorer peer relations in contrast to general population.49 Strikingly, socially isolated breast cancer survivors have 1.7-fold and 2.1-fold elevated risk of all-cause and breast cancer–specific mortalities compared with socially integrated survivors.19 These studies suggest that screening social isolation and integration issues from the early stage throughout the follow-up, on the basis of the type of cancer, should be part of risk assessment. Health care providers may provide appropriate psychosocial interventions to strengthen survivors' social integration skill.
AYA cancer survivors often require support from different sources to address their health needs given the unique developmental stage. Parents, caregivers, or family members may be sources of emotional and economic support, whereas peer survivors may share experiences and provide emotional and informational support.50 AYA patients with cancer often look for resources that can help mitigate isolation, build a sense of community or inclusive environment, or provide opportunities to connect with other AYA patients with cancer or cancer survivors.51 Since the structure of social network data is complex, electronic platforms will facilitate the collection of social relationship data and further integration into informatic systems under the Big Data initiatives for assessing social determinants.
Cancer survivors commonly use online support via social media to gain a sense of empowerment and solve problems or concerns by sharing with other cancer survivors.52,53 However, limited interventions have been implemented to address social integration among AYA cancer survivors. Basically, technology-based health platforms can facilitate access to psychosocial and health support for AYA cancer survivors.54 Survivors with opportunities to communicate through Web-based channels (eg, discussion board, chat, e-mail, and blog) are likely to expand their social networks and receive useful social support.55 AYA patients with cancer and cancer survivors who participate in online support communities reported a greater sense of connectedness and felt less lonely.56 A recent study suggests that using Facebook as a communication platform may increase engagement in physical activities among young adult survivors through information sharing, increased motivation, and provision of tangible or intangible support.57 Although social networking and connections among survivors via chat groups or social media seem promising, the use of technology-based interventions is challenging for individuals who lack appropriate communication skills or mHealth literacy, especially survivors with cognitive impairment. In fact, medically relevant information shared on social media (eg, Facebook) could be inaccurate or misleading,58,59 and AYA cancer survivors may not discuss such information with family members because of concern of burdening them.59 Thus, clinicians need to recommend specific online resources that are appropriate to address medical and psychosocial needs of AYA cancer survivors. Future studies are needed to evaluate the effectiveness of platform-based social integration interventions to improve social connections and health outcomes for AYA cancer survivors.
This study has several limitations. First, the study design is cross-sectional, which precludes causal inferences; however, our social relationship variables were collected on the basis of a retrospective longitudinal design (ie, the past 2 years for social network status and 1 month for social isolation evaluation) and PROs were based on the past 7 days. Second, the use of cross-sectional design cannot fully address the confounding issues for the complex pathways between cancer experience, social integration, and PROs. These confounders include ones' fear about cancer reoccurrence, coping strategy, resiliency, and personality or optimism trait. Third, our social network data were collected through an egocentric approach, meaning a reliance on study participants to report their social relationships with friends and relatives without further validation. As a result, we were not able to investigate bidirectional relationships between survivors and their friends and relatives. Fourth, the response or no-response rate cannot be accurately estimated because the members of the Internet survey panel are changing on a daily basis. However, in line with previous study,60 we used a quota sampling approach to recruit study participants whose characteristics (age at enrollment, sex, race and ethnicity, and cancer diagnosis) are consistent with a target marginal distribution of the CCSS cohort. Fifth, we only evaluated PROs as proxies for late medical effects (eg, neurocognitive functioning and chronic health conditions) rather than through clinical ascertainment. These late medical outcomes may be affected by social integration variables (social network and social isolation), which require further investigation.
In conclusion, although AYA cancer survivors have better social networks, they experience greater loneliness than noncancer controls, which in turn is associated with poor PROs. Cancer experience was directly and indirectly (through social network, social support, and perceived loneliness) associated with poor PROs.
APPENDIX
FIG A1.
Conceptual framework showing the influence of social relationships on patient-reported outcomes.
TABLE A1.
Social Network, Social Support, and Loneliness by Cancer Survivors and Noncancer Controls
D. Kumar Srivastava
Consulting or Advisory Role: General Dynamics Information Technology Peer Review and Science Management
Kevin R. Krull
Patents, Royalties, Other Intellectual Property: Royalties from Wolters Kluwer
Melissa M. Hudson
Consulting or Advisory Role: Oncology Research Information Exchange Network, Princess Máxima Center
No other potential conflicts of interest were reported.
SUPPORT
Supported in part by the Eunice Kennedy Shriver National Institute of Child Health and Human Development/National Institutes of Health (K23 grant HD057146), the National Cancer Institute (Cancer Center Support grant P30 CA021765), and the American Lebanese Syrian Associated Charities.
AUTHOR CONTRIBUTIONS
Conception and design: I-Chan Huang
Financial support: Melissa M. Hudson, Leslie L. Robison
Administrative support: Melissa M. Hudson, Leslie L. Robison
Provision of study materials or patients: I-Chan Huang
Collection and assembly of data: Pragya G. Poudel, Hailey E. Bauer, I-Chan Huang
Data analysis and interpretation: All authors
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by the authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/cci/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
D. Kumar Srivastava
Consulting or Advisory Role: General Dynamics Information Technology Peer Review and Science Management
Kevin R. Krull
Patents, Royalties, Other Intellectual Property: Royalties from Wolters Kluwer
Melissa M. Hudson
Consulting or Advisory Role: Oncology Research Information Exchange Network, Princess Máxima Center
No other potential conflicts of interest were reported.
REFERENCES
- 1.National Cancer Institute Adolescents and young adults with cancer. https://www.cancer.gov/types/aya
- 2.Smith AW, Bellizzi KM, Keegan TH, et al. Health-related quality of life of adolescent and young adult patients with cancer in the United States: The adolescent and young adult health outcomes and patient experience study J Clin Oncol 312136–21452013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tai E, Buchanan N, Townsend J, et al. Health status of adolescent and young adult cancer survivors Cancer 1184884–48912012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baker KS, Syrjala KL.Long-term complications in adolescent and young adult leukemia survivors Hematology 2018146–1532018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zebrack B, Isaacson S.Psychosocial care of adolescent and young adult patients with cancer and survivors J Clin Oncol 301221–12262012 [DOI] [PubMed] [Google Scholar]
- 6.Hydeman JA, Uwazurike OC, Adeyemi EI, et al. Survivorship needs of adolescent and young adult cancer survivors: A concept mapping analysis J Cancer Surviv 1334–422019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eiser C, Aura K.Psychological support Bleyer WA, Barr RD.Cancer in Adolescents and Young Adults Berlin, Germany: Springer; 2007. pp 365–373 [Google Scholar]
- 8.Brinkman TM, Recklitis CJ, Michel G, et al. Psychological symptoms, social outcomes, socioeconomic attainment, and health behaviors among survivors of childhood cancer: Current state of the literature J Clin Oncol 362190–21972018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brinkman TM, Bass JK, Li Z, et al. Treatment‐induced hearing loss and adult social outcomes in survivors of childhood CNS and non‐CNS solid tumors: Results from the St. Jude Lifetime Cohort Study Cancer 1214053–40612015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mitby PA, Robison LL, Whitton JA, et al. Utilization of special education services and educational attainment among long‐term survivors of childhood cancer: A report from the Childhood Cancer Survivor Study Cancer 971115–11262003 [DOI] [PubMed] [Google Scholar]
- 11.Kirchhoff AC, Yi J, Wright J, et al. Marriage and divorce among young adult cancer survivors. Marriage and divorce among young adult cancer survivors J Cancer Surviv 6441–4502012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Berkman LF, Glass T, Brissette I, et al. From social integration to health: Durkheim in the new millennium Soc Sci Med 51843–8572000 [DOI] [PubMed] [Google Scholar]
- 13.Nausheen B, Gidron Y, Peveler R, et al. Social support and cancer progression: A systematic review J Psychosom Res 67403–4152009 [DOI] [PubMed] [Google Scholar]
- 14. Reblin M, Uchino BN. Social and emotional support and its implication for health. Curr Opin Psychiatry. 2008;21:201. doi: 10.1097/YCO.0b013e3282f3ad89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Due P, Holstein B, Lund R, et al. Social relations: Network, support and relational strain Soc Sci Med 48661–6731999 [DOI] [PubMed] [Google Scholar]
- 16.Jones BL, Parker-Raley J, Barczyk A.Adolescent cancer survivors: Identity paradox and the need to belong Qual Health Res 211033–10402011 [DOI] [PubMed] [Google Scholar]
- 17.Sapp AL, Trentham-Dietz A, Newcomb PA, et al. Social networks and quality of life among female long-term colorectal cancer survivors Cancer 981749–17582003 [DOI] [PubMed] [Google Scholar]
- 18.Sarma EA, Kawachi I, Poole EM, et al. Social integration and survival after diagnosis of colorectal cancer Cancer 124833–8402018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kroenke CH, Kubzansky LD, Schernhammer ES, et al. Social networks, social support, and survival after breast cancer diagnosis J Clin Oncol 241105–11112006 [DOI] [PubMed] [Google Scholar]
- 20.Beasley JM, Newcomb PA, Trentham-Dietz A, et al. Social networks and survival after breast cancer diagnosis J Cancer Surviv 4372–3802010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jaremka LM, Fagundes CP, Glaser R, et al. Loneliness predicts pain, depression, and fatigue: Understanding the role of immune dysregulation Psychoneuroendocrinology 381310–13172013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Valtorta NK, Kanaan M, Gilbody S, et al. Loneliness and social isolation as risk factors for coronary heart disease and stroke: Systematic review and meta-analysis of longitudinal observational studies Heart 1021009–10162016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Beutel ME, Klein EM, Brähler E, et al. Loneliness in the general population: Prevalence, determinants and relations to mental health BMC Psychiatry 171–72017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Holt-Lunstad J, Smith TB, Baker M, et al. Loneliness and social isolation as risk factors for mortality: A meta-analytic review Perspect Psychol Sci 10227–2372015 [DOI] [PubMed] [Google Scholar]
- 25. Jaremka LM, Andridge RR, Fagundes CP, et al. Pain, depression, and fatigue: Loneliness as a longitudinal risk factor. Health Psychol. 2014;33:948. doi: 10.1037/a0034012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bower JE.The role of neuro‐immune interactions in cancer‐related fatigue: Biobehavioral risk factors and mechanisms Cancer 125353–3642019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hawkley LC, Cacioppo JT.Loneliness matters: A theoretical and empirical review of consequences and mechanisms Ann Behav Med 40218–2272010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jones EC, Storksdieck M.Recent research on the social network concept and cancer Curr Opin Support Palliat Care 13225–2372019 [DOI] [PubMed] [Google Scholar]
- 29. Jones EC, Storksdieck M, Rangel ML. How social networks may influence cancer patients’ situated identity and illness-related behaviors. Front Public Health. 2018;6:240. doi: 10.3389/fpubh.2018.00240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Anker SD, Agewall S, Borggrefe M, et al. The importance of patient-reported outcomes: A call for their comprehensive integration in cardiovascular clinical trials Eur Heart J 352001–20092014 [DOI] [PubMed] [Google Scholar]
- 31.Mierzynska J, Piccinin C, Pe M, et al. Prognostic value of patient-reported outcomes from international randomised clinical trials on cancer: A systematic review Lancet Oncol 20e685–e6982019 [DOI] [PubMed] [Google Scholar]
- 32.Bleyer A, O’Leary M, Barr R, et al. Cancer Epidemiology in Older Adolescents and Young Adults 15 to 29 Years of Age, Including SEER Incidence and Survival: 1975-2000. Bethesda, MD: National Cancer Institute, NIH Pub. No. 06-5767; 2006. [Google Scholar]
- 33.SEER . Cancer Stat Facts: Cancer Among Adolescents and Young Adults (AYAs) (Ages 15-39) 2021. https://seer.cancer.gov/statfacts/html/aya.html Bethesda, MD, National Cancer Institute. [Google Scholar]
- 34.What should the age range be for AYA oncology? J Adolesc Young Adult Oncol 13–102011 [DOI] [PubMed] [Google Scholar]
- 35.Huang IC, Jones CM, Brinkman TM, et al. Development of the functional social network index for adolescent and young adult cancer survivors Cancer 1242220–22272018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cella D, Riley W, Stone A, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008 J Clin Epidemiol 631179–11942010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Broadhead W, Gehlbach SH, De Gruy FV, et al. The Duke-UNC Functional Social Support Questionnaire: Measurement of social support in family medicine patients Med Care 26709–7231988 [DOI] [PubMed] [Google Scholar]
- 38.Russell DW.UCLA Loneliness Scale (version 3): Reliability, validity, and factor structure J Pers Assess 6620–401996 [DOI] [PubMed] [Google Scholar]
- 39.Muthén LK, Muthén BO. Mplus User’s Guide. ed 8. Los Angeles, CA: Muthén & Muthén; 1998-2017. [Google Scholar]
- 40.Warner EL, Kent EE, Trevino KM, et al. Social well-being among adolescents and young adults with cancer: A systematic review Cancer 1221029–10372016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tremolada M, Bonichini S, Basso G, et al. Perceived social support and health‐related quality of life in AYA cancer survivors and controls Psychooncology 251408–14172016 [DOI] [PubMed] [Google Scholar]
- 42.Soares A, Biasoli I, Scheliga A, et al. Association of social network and social support with health-related quality of life and fatigue in long-term survivors of Hodgkin lymphoma Support Care Cancer 212153–21592013 [DOI] [PubMed] [Google Scholar]
- 43.Yen H-J, Eissa HM, Bhatt NS, et al. Patient-reported outcomes in survivors of childhood hematologic malignancies with hematopoietic stem cell transplant Blood 1351847–18582020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kandula T, Farrar MA, Cohn RJ, et al. Chemotherapy-induced peripheral neuropathy in long-term survivors of childhood cancer: Clinical, neurophysiological, functional, and patient-reported outcomes JAMA Neurol 75980–9882018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Adams RN, Mosher CE, Winger JG, et al. Cancer-related loneliness mediates the relationships between social constraints and symptoms among cancer patients J Behav Med 41243–2522018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ernst M, Brähler E, Wild PS, et al. Risk factors for suicidal ideation in a large, registry-based sample of adult long-term childhood cancer survivors J Affect Disord 265351–3562020 [DOI] [PubMed] [Google Scholar]
- 47.Brinkman TM, Zhang N, Recklitis CJ, et al. Suicide ideation and associated mortality in adult survivors of childhood cancer Cancer 120271–2772014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jaremka LM, Fagundes CP, Peng J, et al. Loneliness promotes inflammation during acute stress Psychol Sci 241089–10972013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hörnquist L, Rickardsson J, Lannering B, et al. Altered self-perception in adult survivors treated for a CNS tumor in childhood or adolescence: Population-based outcomes compared with the general population Neuro Oncol 17733–7402014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hauken MA, Larsen TM.Young adult cancer patients’ experiences of private social network support during cancer treatment J Clin Nurs 282953–29652019 [DOI] [PubMed] [Google Scholar]
- 51.Cheung CK, Zebrack B.What do adolescents and young adults want from cancer resources? Insights from a Delphi panel of AYA patients Support Care Cancer 25119–1262017 [DOI] [PubMed] [Google Scholar]
- 52.Falisi AL, Wiseman KP, Gaysynsky A, et al. Social media for breast cancer survivors: A literature review J Cancer Surviv 11808–8212017 [DOI] [PubMed] [Google Scholar]
- 53.Fallon EA, Driscoll D, Smith TS, et al. Description, characterization, and evaluation of an online social networking community: The American Cancer Society’s Cancer Survivors Network J Cancer Surviv 12691–7012018 [DOI] [PubMed] [Google Scholar]
- 54.Devine KA, Viola AS, Coups EJ, et al. Digital health interventions for adolescent and young adult cancer survivors JCO Clin Cancer Inform 21–152018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Owen JE, Curran M, Bantum EOC, et al. Characterizing social networks and communication channels in a web-based peer support intervention Cyberpsychol Behav Soc Netw 19388–3962016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Kaal SE, Husson O, van Dartel F, et al. Online support community for adolescents and young adults (AYAs) with cancer: User statistics, evaluation, and content analysis. Patient Prefer Adherence. 2018;12:2615. doi: 10.2147/PPA.S171892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Valle CG, Tate DF, Mayer DK, et al. A randomized trial of a Facebook-based physical activity intervention for young adult cancer survivors J Cancer Surviv 7355–3682013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gage-Bouchard EA, LaValley S, Warunek M, et al. Is cancer information exchanged on social media scientifically accurate? J Cancer Educ 331328–13322018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Domínguez M, Sapiña L.“Others Like Me”. An approach to the use of the internet and social networks in adolescents and young adults diagnosed with cancer J Cancer Educ 32885–8912017 [DOI] [PubMed] [Google Scholar]
- 60.Hays RD, Liu H, Kapteyn A.Use of Internet panels to conduct surveys Behav Res Methods 47685–6902015 [DOI] [PMC free article] [PubMed] [Google Scholar]