Abstract
Background
The hospitalization of children during the COVID-19 pandemic has affected their physical and mental health. Pediatric nurses have faced challenges in providing high-quality nursing care for children and their families. However, the pediatric nursing care recommendations for COVID-19 patients in the hospital setting remain unclear. The current scoping review provides recommendations for nursing interventions for pediatric COVID-19 patients in the hospital setting.
Methods and findings
The selected articles containing management and nursing recommendations for COVID-19 that have occurred in pediatric patients ages 0–19 years old. A search strategy was developed and implemented in seven databases. We included peer-reviewed articles that reported observational or interventional studies, as well as policy papers, guides or guidelines, letters and editorials, and web articles. A total of 134 articles and other documents relevant to this review were included. We categorized the results based on The Nursing Intervention Classification (NIC) taxonomy which consists of six domains (e.g., Physiological: Basic); eleven classes (e.g., Nutrition Support); and eighteen intervention themes (e.g., Positioning, Family Presence Facilitation, Family Support, and Discharge Planning).
Conclusion
Apart from the intervention of physical problems, there is a need to promote patient- and family-centered care, play therapy, and discharge planning to help children and families cope with their new situation.
Introduction
Corona virus disease is defined as an infectious disease caused by the newly discovered coronavirus SARS-CoV-2 [1–3]. It was identified in Wuhan, China, on 29 December 2019, as reported by the World Health Organization [4]. This disease was officially named COVID-19 by the WHO on 11 February 2020 [5]. To date, its spread continues to increase worldwide [6]. On 16 November 2021, an estimated 253,640,693 confirmed cases and 5,104,899 deaths caused by COVID-19 had been reported globally [7]. Most cases have occurred in the Americas, Europe, and South-East Asia [7].
Children are part of a population that requires further study [8]. A systematic literature review of 23 countries estimated that the prevalence of children suffering from COVID-19 was 1.9% [9]. Data reported from Spain showed 41 confirmed cases in children, of which 60% required hospital care and 9.7% needed to be admitted to the Pediatric Intensive Care Unit (PICU) [10]. Dong, et al. revealed that 2,143 pediatric patients (731 confirmed and 1412 suspected) who were admitted to hospital developed into moderate to severe cases, and 40% and 0.6% required admission to a Pediatric Intensive Care Unit (PICU), respectively [11]. In the USA, the CDC reported 2575 cases among children, of which up to 20% required hospital admission, and 2% needed care in a PICU [12]. Most studies in the literature reported physical complaints, such as fever, cough, rhinorrhea, nasal congestion, myalgia, fatigue, sore throat, shortness of breath, dyspnea, abdominal pain, diarrhea, vomiting, nausea, headache, mild to severe respiratory distress, and Multisystem Inflammatory Syndrome in Children (MIS-C) [13–23]. Moreover, an extensive systematic review concluded that the symptoms of COVID-19 in children differed widely from adult cases [24]. Nursing care is designed to overcome problems related to specific symptoms and conditions of the patient. However, the number of studies conducted on children with COVID-19 is limited [25].
In addition to physical complaints, the hospitalization itself can be a harmful and stressful experience for children [26]. Hospitalized children expressed fears, uncertainty, anger, helplessness, and anxiety caused by several medical procedures due to a lack of information and an unfamiliar physical and social environment [27–29], which could affect the mental and spiritual health of the child and parent [30]. A similar negative impact of hospitalization in the pediatric COVID-19 context has also been reported [31–33]. Moreover, restricted physical movement, parental separation, stigma, and social exclusion caused by hospitalized quarantined protocol were shown to complicate the care of pediatric patients with COVID-19 [32, 34–36]. Because of such issues, it has been particularly challenging for pediatric nurses to provide nursing care during the COVID-19 pandemic across various limitations [37].
Several nursing care guidelines have been developed to support nurses in managing COVID-19 patients in a wide range of situations across the world, such as initial general nursing care [38, 39], palliative care guidance for nursing homes [40], oncology nursing [41], and emergency nursing [42]. However, to our knowledge, no comprehensive nursing care guidelines have been developed to address the specific needs of children suffering from COVID-19 in a hospital setting. Hence, providing clear clinical nursing management guidance for nursing pediatric patients with COVID-19 is urgently needed. This study aims to provide guidance on nursing care for pediatric COVID-19 patients based on a systematic review of the relevant literature.
Methods
Study design
Arksey and O’Malley’s [43] framework, which is a commonly used guide in conducting a scoping review [44], consists of five steps: 1) identifying a clear research objective and search strategies; 2) identifying relevant research articles; 3) selecting research articles; 4) extracting and charting data; and 5) summarizing, discussing, analyzing, and reporting the results [45]. In this current scoping review, the Joanna Briggs Institute (JBI) guidelines, which is a leading source of scoping review guidance, was used as the primary protocol for conducting this research [46]. JBI guidelines was an extended and refined work from Arksey and O’Malley’s framework.
Literature search strategy
A systematic search of the CINAHL, Science Direct, ProQuest, Embase, SpringerLink, PubMed, and Taylor and Francis databases was performed, including references from inception of databases to 10 February 2021, using the terms ‘children’ AND ‘COVID-19’ with a combination of keywords. A detailed example of the search strategy is provided in S1 Table.
Identification and selection of relevant studies
Studies were eligible for a full-text analysis when all patients were under 18 years and the publication related to in an outpatient or in-hospital environment. Randomized controlled trials, controlled and non-controlled before-and-after studies, controlled and non-controlled interrupted time series, and cohort studies were included. The overall criteria of this study are provided in S2 Table.
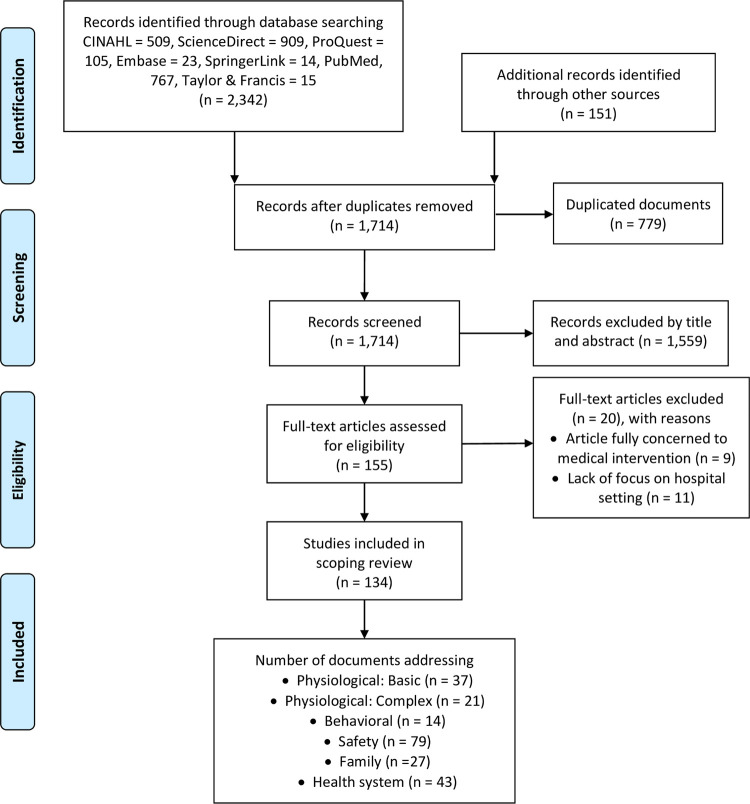
Systematic reviews, scoping reviews, and meta-analyses were excluded. Studies on both adults and children from which the extraction of pediatric data was not possible were also excluded. We excluded studies published before December 2020 because the concept of COVID-19 was formally introduced in that year. We did not include articles about types of disease other than COVID-19 and its’ related medical condition similarly MIS-C. Fig 1 shows the process used to search and select the research articles. Four investigators independently performed reviews of the titles, abstracts, and full texts (A.R.U., R.N., T.A.A., and R.Y.). Any disagreement regarding the collection of studies was resolved by discussion with a fifth reviewer (D.E.).
Fig 1. PRISMA flow diagram for the scoping review process.
Data synthesis and analysis
A structured data collection was conducted and a table (S3 Table) was created to document extracted data that summarized information about authors, year of publication, country, study time, type of article, and purpose of the study. Five authors (A.R.U., R.N., T.A.A., R.Y., and D.S.) conducted the data extraction from the included studies. They read every full text thoroughly to identify any statement that could be transformed into a clinical nursing intervention in the hospital setting. A.R.U., and R.N. adopted the Nursing Intervention Classification (NIC, 7th ed.) to rearrange the extracted data into suitable domains, classes, and interventions [47]. Each included study has chance to be generated in more than one domain, class, and intervention. Because it is a specialty among other pediatric patients, we divided nursing interventions for neonates into separate parts in each table. The recommendations were categorized according to the appropriate class and intervention. D.E. then performed an in-depth review for a new set of nursing recommendations that was derived from the previous authors who extracted the data (A.R.U., R.N., T.A.A., R.Y., and D.S.). Any changes made by D.E. were discussed with all authors involved in the data analysis process. We used our expertise and experience in delivering nursing care in the pediatric and neonatal wards, as well as in intensive care, to ensure the fine-tuning and applicability of these recommendations. We reported this scoping review following the PRISMA-ScR Checklist (S1 Checklist) [48].
Results
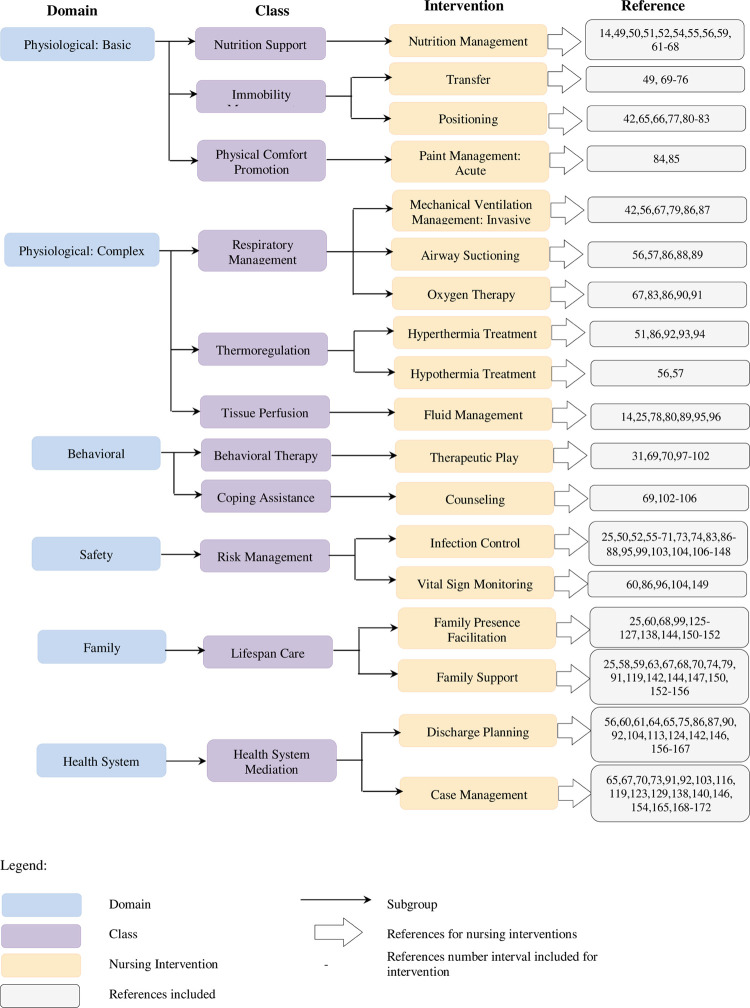
We initially identified 2,493 articles and screened the abstracts and titles for inclusion (Fig 1). After the removal of duplicates and irrelevant studies, 134 full-text articles were included in the review. The characteristics of the included studies are listed in S3 Table. The extracted articles contained information on child care recommendations in health care settings during the COVID-19 pandemic using a framework based on the NIC taxonomy [47]. Accordingly, from the documents included, we disseminate them into the eligible taxonomy comprise: six domains (Physiological: Basic, Physiological: Complex, Behavioural, Safety, Family, and Health System), eleven classes (Nutrition Support, Immobility Management, Physical Comfort Promotion, Respiratory Management, Thermoregulation, Tissue perfusion, Behavioural Therapy, Coping Assistance, Risk Management, Lifespan Care, Health System Mediation), and eighteen intervention themes (Nutrition Management, Transfer, Positioning, Pain Management: Acute, Mechanical Ventilation, Management: Invasive, Airway Suctioning, Oxygen Therapy, Hyperthermia Treatment, Hypothermia Treatment, Fluid Management, Therapeutic Play, Counseling, Infection Control, Family Presence Facilitation, Family Support, Discharge Planning, Case Management). The distribution of eligible studies in the taxonomy describes in Fig 2.
Fig 2. NIC framework for including study.
Among the six domains, the Physiological: Basic domain was widely discussed among the variety of interventions for Nutrition Support, Immobility Management, and Physical Comfort Promotion. Table 1 provides 16 interventions for Nutrition Management, Transfer, Positioning, and Pain Management: Acute. In addition, the Physiological: Complex domain showed various intervention recommendations for classes of Respiratory Management, Thermoregulation, and Tissue Perfusion (as described in Table 1). Thirteen interventions were identified: Mechanical Ventilation, Airway Suctioning, Oxygen Therapy, Hyperthermia Treatment, Hypothermia Treatment, and Fluid Management.
Table 1. Physiological basic and complex domain.
| Domain | Class | Intervention | Summary of Intervention |
|---|---|---|---|
| (1) Physiological: Basic | Nutrition Support | Nutrition Management | • Ensure adequate fluid, and nutrient intake [14, 49, 50]. Fulfil energy supply of 25–30 kcal /kg/day [51] and pay attention to the nutrition strategy for PICU critical children [52], post-critical recovery, and the acute phase [52–54]. NEONATES • Rooming-in, and direct breastfeeding or expressing breast milk (if the baby is sick and not admitted to rooming-in) is recommended for babies of mothers who have no symptoms / mild symptoms of COVID-19 and mothers can care for LBW independently by controlling the spread of infection [49, 55–64]• Caregivers who are not infected can assist in giving breast milk to the baby [61, 65] using a special bottle [62].• Give the mother support to breastfeeding the baby [56] and make decisions about breastfeeding [63, 66] by discussing the risks, and benefits of breastfeeding the baby in the covid-19 positive mother [67].• Assess the possibility of breastfeeding with re-lactation, wet nursing (another woman breastfeeding the baby), or donor breast milk according to culture and patient acceptance [66]. • Use pasteurized donor breast milk, and breastfeeding donors have performed a blood test if expressed breast milk is not available [62, 68]. Another suggestion states that dairy milk should not be pasteurized because it is believed that it is not a carrier of infection and pasteurization can reduce the biological and immunological levels of breast milk [59]. • Stop breastfeeding donations for two weeks if the mother is suspected of COVID-19 until she gets two negative swabs [62]. |
| Immobility Management | Transfer | • Use special vehicles to transfer infected patients, strict protection for transportation staff, vehicle disinfection [49, 69, 70], and pay attention to patient transfer procedures [71]. • Pay attention to the transport of the intubated patient. patient using ventilator needs to be supplemented with viral filters and consideration of additional sedation [72]. NEONATES • Transportation of neonates with suspected/confirmed COVID-19 must be equipped with PPE, disinfectant, ventilator, vital sign monitor, first aid drugs, and a closed incubator for transfer equipment [73–75]. • It is recommended to use a NETS ambulance as COVID-19 NETS to transport newborns [76]. |
|
| Positioning | • Position the patient in an early prone position or prolonged moderate to severe PARDS (i.e. PaO2 / FiO2 <150; OI ≥ 12; OSI ≥ 10 for 12–18 hours per day (avoid disconnection) [42, 65, 77–81] and discontinue if PaO2 / FiO2 ≥ 150; OI <12; OSI <10 [66, 82] or change the position to supine during a heart attack [80]. If the patient is intubated, cardiopulmonary resuscitation (CPR) can remain prone [80]. • If the long duration of prone position is not achievable, try to position the patient 1–2 hours 3–4 times/day [77, 83]. |
||
| Physical Comfort Promotion | Pain Management: Acute | • Treatments in pain management include physical therapy, psychology, medical providers, and complementary services such as massage, and acupuncture [84]. • Perform non-pharmacological techniques according to the location of the pain. Provide psychotherapy, such as distraction, spending time with family, playing games with others, laughter. Provide physical therapy such as acute pain, preferably rest but chronic pain, need regular movement every day so that much pain is reduced, for example; take a walk around the neighbourhood with the family, do fun online dance or yoga classes, ride a bike. Relaxation skills: diaphragmatic breathing, progressive muscle relaxation, guided imagery [84]. NENEONATES • Give D10% as a non-pharmacological action to reduce pain due to invasive action in neonates [85]. |
|
| (2) Physiological: Complex |
Respiratory Management | Mechanical Ventilation Management: Invasive | • Use cuffed endotracheal tubes [67, 79], and monitor the ETT cuff pressure every 6–12 hours to ensure there is no leak, and the pressure is at the safe limit of <20cm H2O [42]. • Use a disposable ventilator circuit for each new patient [86], attach a viral filter (HEPA) to the expiration circuit [56, 86] or a hydrophobic mechanical filter attached to the inspirational and expiratory section [87]. Heat and moisture exchanger (HME) must be replaced every 48 hours or when dirty [86]. |
| Airway Suctioning | • Closed suction is recommended [86, 88] if there is airway obstruction [89] or only if needed [57] and there are indications [56, 86]. | ||
| Oxygen Therapy | • Maintain SpO2> 92% [90], pay attention to the oxygen saturation value that is safe for patients [83]. • Early intubation is recommended for children with severe/critical symptoms of COVID-19 rather than non-invasive ventilation or high flow nasal cannula because it can produce aerosols [86] which should be minimized [91]. • Provide adequate humidity, and heating when giving oxygen, especially at concentrations> 3–4 L / minute [83]. • Avoid using high flow nasal cannulas [67], and NIV considering the potential for aerosol formation [86]. |
||
| Thermoregulation | Hyperthermia Treatment | • Observe body temperature regularly. It needs serious attention related to temperature increase, even though the increase is not too high [92]. • Pediatric patients with high fever exceeding 38.5°C and seem uncomfortable, it is recommended to physically cool down with warms baths, use antipyretic patches or fever-reducing drugs [51, 86, 93] and maintain good hydration when the child has a fever [94]. |
|
| Hypothermia Treatment |
NEONATES • After delivery, babies with COVID-19 are kept dry, given stimulation, warmed by the mother and breastfed immediately [57]. However, bathing is not recommended to prevent hypothermia and the spread of nosocomial infections [56]. |
||
| Tissue Perfusion | Fluid Management | • Adjust the patient’s fluid volume according to hemodynamic conditions. The amount of fluid restriction is adjusted according to the Holliday-Fresh formula [78], then record the hourly fluid intake, and output [25]. • Provide supportive care by providing, and maintaining a balanced body fluid intake, and adequate calories [14, 80, 89, 95] • Assess fluid status, and heart function before starting MISC (multisystem inflammatory syndrome-Children) treatment in children with COVID-19 [96]. |
COVID-19: Coronavirus Disease-2019, ETT: Endotracheal Tube, FiO2: Fraction of Inspired Oxygen, H2O: Dihydrogen Monoxide, HEPA: High-Efficiency Particulate Air, LBW: Low Birth Weight, NETS: Newborn Emergency Transport Service, NIV: Non-invasive Ventilation, OI: Oxygenation Index, OSI: Oxygen Saturation Index, PARDS: Pediatric Acute Respiratory Syndrome, PaO2: Partial Pressure of Oxygen, PICU: Pediatric Intensive Care Unit, PPE: Personal Protective Equipment, SpO2: Peripheral Capillary Oxygen Saturation.
The number in the point of intervention column corresponds to the order of the articles in S3 Table.
As shown in Table 2, the domain with the highest number of intervention recommendations was the Safety domain in the Risk Management class, which described the intervention recommendations for Infection Control (61 interventions) and Vital Sign Monitoring (six interventions). The domain with the lowest number of intervention recommendations was the Behavioral domain, which consisted of the Behavioral Therapy and Coping Assistance classes. A total of seven recommendations for Therapeutic Play and Counseling interventions were drawn from those two classes (see Table 2).
Table 2. Behavioral and safety domain.
| Domain | Class | Intervention | Summary of Intervention |
|---|---|---|---|
| (3) Behavioral | Behavioural Therapy | Therapeutic Play | • Develop children’s coping mechanisms through play activities according to their development [70]. • Intervene based on age to address and prevent psychological problems in children during the COVID-19 pandemic such as: • Singing or music therapy, making music with a bowl and spoon [31, 97, 98]. • Reading books and drawing [98]. • Helping school lessons, talking about what children like [98]. • Sports, or doing tasks together [98]. • Playing collaborative games [31]. • Painting, or playing with children [69]. • Playing the peek "a-boo" [99]. • Meet the needs of communication and emotional support with children and families [101]. • Offer mental health services to children, adolescents, and families by telephone or face-to-face [102]. |
| Coping Assistance | Counselling | • Facilitate all questions and concerns of patients, parents or other families with open communication, understanding and patience [103]. • Monitor and identify changes in mental health status, coping, and causes of pandemic stress in children and families, overcome if problems are identified [102, 104]. • Identify the needs of mental health in children with mental health and behavioural disorders [105]. • Provide palliative care based on the basic principles of palliative care for children [106]. • Avoid separating children from family, ask children to talk about their feelings [69]. |
|
| (4) Safety | Risk Management | Infection Control | • Triage nurses must use a medical mask then sort patients based on their risk level for COVID-19 infection [50, 107]. • Perform rapid screening of pediatric patients with suspected and confirmed COVID-19 [108]. Modify the triage flow arrangement and management of patient admissions to the hospital. separating patients who are at risk and not are essential [109–111]. • Health workers must wear PPE /special PPE for COVID-19 when performing procedures: delivery of infected or suspected COVID-19 mothers, preparation and administration of chemotherapy, triage, administration of inhalers and nebulizers, collection of respiratory diagnostic specimens and resuscitation [50, 57, 103, 112, 113]. Follow the general principles of management of patients who are at high risk of producing aerosol or AGP (aerosol-generating procedure) [114, 115]. • Management of PPE to prevent shortages [116]. • Wearing powered air-purifying respirators and also need to limit the number of health workers in the room [52, 57, 71, 86, 117–120]. Provide training related to the use of PPE for health workers [121]. • Invasive airway examinations or procedures and examination of the mouth cavity should not be performed if appropriate PPE is not used [50]. • Keep using a surgical mask when handling non-COVID-19 pediatric patients [50]. • Recommend that asymptomatic patients wear medical masks (especially N95) or respirators (especially FFP3), observe provisions for mask disposal [122]. • A HEPA (high-efficiency particulate air) filter can be attached to a BVM (bag valve mask), mechanical ventilator and non-invasive ventilation or aerosol box placement during intubation and suction procedures to reduce the spread of the virus [56, 74, 120, 123, 124]. • Introduce masks to children, explain the benefits of masks, and help children learn to understand the expressions and feelings of the eyes and eyebrows [99, 125–127]. • Perform nasopharyngeal/oropharyngeal swabs in a child-friendly environment and explain the test procedure to the older child [107]. • Use a single room with negative pressure for pediatric patients with suspected/confirmed COVID-19 [25, 70, 71, 86, 117, 128]. • Place contaminated clothing and sheets in infectious trash bags [106, 119]. • Early identification of infected children for immediate isolation if infected because children can become seriously ill after infection [129]. • Discontinue isolation after two negative laboratory results or with a symptom-based strategy [86, 95]. • Daily disinfection of all equipment and surfaces in the isolation room. Put trash from the isolation room separately from trash from other rooms [25, 130]. • Physical isolation for children who will undergo cancer treatment and kidney donors/recipients who will undergo transplantation surgery [87, 119, 131]. • Teach children about how to protect themselves from COVID-19 during clinic visits and evaluate knowledge about efforts to reduce the risk of infection in children [65, 104, 113, 132]. • Limit the number of visitors or people accompanying children who are hospitalized (1 member of family/ child) [87, 104, 109, 113, 116]. Perform temperature checks on all visitors before entering the hospital or NICU room [67]. • Maintain and increase awareness of maintaining hand hygiene, and physical-distancing. Use PPE (especially face masks) to reduce the spread of infection [111, 133]. • Consider the use of oxygen because it is potentially dangerous if it is not controlled [83]. • Put on a medical mask on children who use nasal prongs [86]. • Supervise the use of masks in children by parents [134]. • Protect healthcare workers and pediatric surgical patients from contracting COVID-19 [135]. • Cleaning the operating room and instruments using a disinfectant solution or UV light [118]. • Postoperative patient follow-up virtually whenever possible [136]. NEONATES • Prevent the spread of infection rooming-in mother-infant [55–59, 62]. • Maintain hand hygiene by washing with soap and water or alcohol before and after breastfeeding and touching babies or expressing breast milk [67]. • Routinely disinfect surfaces, baby drinking utensils and breast pumps [59, 66, 67]. • Mothers should wear surgical masks when breastfeeding babies and in close contact with babies [55–59, 62]. • The mother-infant room should be isolated from visitors [55–59, 62]. • Place the baby at a safe distance (2 meters) [55–59, 62]. • Avoid using disinfectants in breast milk containers [137]. • Disinfection of care areas for neonates with suspected/confirmed COVID-19 using 0.5% sodium hypochlorite, 70% alcohol, and hydrogen peroxide [56, 138]. • Do not delay clamping of the umbilical cord [56, 138–140]. • Avoid skin-to-skin contact of newborns with COVID-19 mothers [56, 138–142]. • Isolate and use a negative pressure incubator on babies who are at risk of COVID-19 [60, 67, 111, 143, 144]. • Advice parents to use surgical masks and wash hands before entering the NICU room [64, 67, 144]. • Isolate separately the baby who is positive for COVID-19 for 14 days [55, 69, 111, 120, 138, 140]. • Use PPE (gown, gloves, eye protection, N95 mask) when caring for premature babies suspected of having COVID-19 [88, 138]. • Do not use surgical loupe as a substitute for protective eyewear [88]. • Use P2 / N95 respirator (valveless), smoke evaluation kit, eye protection, powered air-purifying respirators (PARS) in aerosol-generating procedures [55, 67, 88, 143]. • Infant resuscitation is carried out by experienced health professionals and minimizes the number of health worker [74]. • Immediately bathe the baby after birth [145]. • Limit the number of visits to the neonatal unit [60, 64, 67, 133, 146]. • Immediately carry out the discharge of post-partum mothers [99] • COVID-19 examinations in infants with positive mothers for COVID-19 [60, 61]. • Monitor for signs and symptoms of infection in neonates [60]. Give a minimum distance of 6 feet to babies who have recently been positive but did not get AGP (aerosol-generating procedures) [67]. • Rooming-in is carried out if the mother has two negative nasopharyngeal swabs and the clinical condition improves [61]. • If rooming-in, teach parents to use masks and wash their hands regularly [68, 147]. • Use a face mask when breastfeeding as a hygiene measure [143]. • Infants infected with COVID-19 or at risk of contracting COVID-19 must be outpatient 14 days after discharge from the hospital [61]. Disinfectant: • Disinfection of the room per shift after mother and baby are discharged [64]. • Disinfect inanimate objects using diluted bleach [148]. • Use a disinfectant containing 62–71% ethanol [148]. • Perform UV irradiation for 24 hours and hydrogen peroxide in the operating room that COVID-19 patients have used [148]. • Use povidone-iodine or chlorhexidine on open wounds that are at risk of contracting COVID-19 [148]. • Disinfect large surfaces with 0.5% sodium hypochlorite (5000 ppm) and small appliances with 70% ethyl alcohol [73]. • Thoroughly clean the instrument used to measure the baby’s vital sign [140]. |
| Vital Sign Monitoring | • Monitor for signs and symptoms of infection in neonates [60] and children with a picture of pneumonia related to the need for ICU care [149]. • Measure vital sign before receiving (intravenous immunoglobulin) in patients with COVID-19 children with MIS_C (Multisystem inflammatory syndrome in children) as a vital sign baseline [96]. • Regular vital sign monitoring after administration of IVIG (intravenous immunoglobulin) [96]. • Ensure the patient’s blood pressure is stable before getting IVIG (intravenous immunoglobulin) [96]. • Monitoring and documenting vital sign regularly, especially SpO2, RR and HR [86]. • Closely monitor any worsening of symptoms (such as tachypnea, respiratory distress, or dehydration) and outpatient follow-up (children with illness) suspected or confirmed COVID-19 [104]. |
COVID-19: Coronavirus Disease-2019, FFP: Filtering Face Piece, HR: Heart Rate, ICU: Intensive Care Unit, NICU: Neonatal Intensive Care Unit, PPE: Personal Protective Equipment, RR: Rate Respiration, SpO2: Peripheral Capillary Oxygen Saturation, UV: Ultraviolet.
The number in the point of intervention column corresponds to the order of the articles in S3 Table.
Table 3 shows the Family domain, which consisted of two intervention themes: Family Presence Facilitation and Family Support. Twenty-seven recommendations were identified in the intervention themes. Furthermore, the Health System Mediation class in the Health System domain provided 33 recommendations for Discharge Planning interventions.
Table 3. Family and health system domain.
| Domain | Class | Intervention | Summary of Intervention |
|---|---|---|---|
| (5) Family | Lifespan Care | Family Presence Facilitation | • Parents can accompany the child to use their mask, wash their hands and maintain normal temperature [68, 150]. • Facilitate the presence and communication of parents with children in the PICU room [25]. • Involve other family members to increase family cohesion and support [151]. • Facilitate parents to contact health service through audio visual services [68]. NEONATES: • Only parents or primary supporters are allowed to visit the NICU indefinitely [144]. • Promote skin-to-skin contact without time limit and safe breastfeeding for babies who are not isolated [144, 152]. If the mother is quarantined, discuss family members who will do skin-to-skin contact [144]. • Maximize interaction with babies whether using / not wearing masks or using transparent masks as an alternative to connecting and communicating with babies [99, 125–127]. • Observe for excessive stress in infants who are separated from the mother and make sure the baby gets a touch of caregivers [152]. • Observe the symptoms of stress, anxiety and depression in the parents due to separation and restrictions with the baby [60]. • Provide support and facilitate communication when the mother-baby condition is separated [138]. |
| Family Support | Family-Centered Approach [153, 154]: • Joint decision making: Facilitate 2-way communication so that parents feel calmer [63, 153, 154]. Separating babies and mothers who are positive for COVID-19 must follow the existing provisions [74]. • Parental ties: • Help the family manage stress due to separation of children and families during the treatment period [70, 153, 154] • Provide support for parents via telephone or social media [70, 119]. • Intensively inform and motivate parents to give love to children with cancer during isolation [155]. • Facilitate contact between parents and children through audio-visual [68, 153, 154]. • Avoid separating healthy babies from mothers with suspected/confirmed COVID-19 with a health condition that does not require treatment [144, 152]. Unless, temporarily separate mother and baby if the mother is symptomatic of respiratory tract infections until the test result is negative [59, 152]. • Provide kangaroo care when a positive COVID-19 mother visits the NICU [67]. Communication • Convey the child’s condition with age-appropriate communication techniques (playing or telling stories) to children who are already able to understand [79, 150]. • Provide information and emotional support on the reasons for isolation and the risks if not isolation [25, 153, 154]. • Inform and actively involve parents regarding illness and child care plans [25, 58, 91, 142, 147, 156]. • Encourage parents to breastfeed according to scientific evidence [68]. • Collaboration between disciplines to provide support for parents [68, 70]. Transparency • Openly explain to the family the reasons for limiting visits [91]. • Limit one person to watch except for the end-of-life conditions [119]. • Inform the guidelines that apply to health services related to COVID-19 [67, 153, 154]. • Care with socio-culture • Provide culturally and linguistically sensitive nursing care [153, 154]. Give a touch to the baby experiencing stress due to separation from the mother [152]. |
||
| (6) Health System |
Health System Mediation | Discharge Planning | • Educate what to do at home and make sure the patient and family are ready to carry out medical procedures after being discharged [64, 142, 156, 157]. • Education for self-isolation at home for 14 days after treatment [60, 64, 86, 92, 142, 156, 158]. • In children with nephrotic syndrome, give education related to management, clinical status and home care plans [104] • Children are allowed to go home if the inflammation values are typical, no fever, normotensive, good hydration, and without oxygen support [159]. • Discharge planning care in the mother’s room or via video or telephone lines [124, 160]. • Provide educational media such as leaflets [64]. • Practices appear to have the capacity to deliver routinely recommended vaccines, allowing children who have missed vaccine doses because of the pandemic to catch up. Practices that are unable to provide immunization services should refer patients to other practices [75]. • Utilizing telemedicine/telehealth for follow-up and meeting patient needs [61, 64, 65, 87, 90, 92, 113, 146, 161–167]. NEONATES • If the baby is not rooming-in to the mother, she/he can be discharged from the hospital at the age of 24–48 hours [56]. • Before going home, educate parents about signs and symptoms of danger to neonates [56, 64]. • If the parents are positive, suggest care-giver from family member who has been COVID-19 negatively tested to care for the newborn in the home [124]. • Suggest doing basic vaccinations on schedule [64]. • Teach the mother to keep a distance and use a mask if there are still symptoms until seven days after the symptoms appear [61]. |
| Case Management | • Advise parents to communicate with children via video [168]. • Physical examination is carried out only on the part related to complaints [92]. • Non-chemotherapy transfusions and infusions in children with cancer can be given at home [103]. • Answer children’s questions honestly regarding COVID-19 according to their stage of development [65, 70]. • Facilitate children in expressing their needs [70]. • Create a protocol that allows the patient’s environment to remain safe during assessment and specimen collection [70, 91, 165]. • Ensure that neonates will be handled by well-trained health care personal [91, 119]. • Collaboration with parents regarding IEP (Individualized Education Program) in children with disabilities [169]. • Traffic restrictions among COVID-19 patients [140]. • Inform about the impact of COVID-19 on families [146]. • Communicate regarding the patient’s needs, discomfort, and support for the patient during the treatment process [129]. • Meet regularly (2 times a week) at the pediatric department to discuss developments related to COVID-19 management [116]. • Interdisciplinary collaboration and involving stakeholders are needed if urgent elective surgery is performed [170]. Actively communicate the surgical plan and reasons for postponing surgery to parents regarding COVID-19 [170]. • Monitoring children’s habits related to screen-time, sleep patterns, physical activity, habits, eating, and psychological responses [171]. • Carry out family tracing and activities on children infected with COVID-19 [172]. NEONATES: • Follow the modified algorithm directions by the neonatology team in case of the emergency airway in neonates [154]. • Modification of postnatal management of neonates from COVID-19 positive mothers if a separate isolation room is available or not available at the hospital [73]. • Do a neonatal COVID-19 test within 24 hours of birth to avoid false positives [67, 123]. • Provide supportive care to newborn infected with COVID-19 [138]. |
COVID-19: Coronavirus Disease-2019, NICU: Neonatal Intensive Care Unit, PICU: Pediatric Intensive Care Unit.
The number in the point of intervention column corresponds to the order of the articles in S3 Table.
Discussion
This scoping review was conducted to provide nursing intervention recommendations for nursing staff caring for pediatric patients with COVID-19 in the hospital setting. To the best of our knowledge, this study is the first to review the scope of the literature on the comprehensive nursing care of pediatric patients with COVID-19. Previous systematic and scoping reviews concerned epidemiological studies [23, 173], nursing approach in diagnosing COVID-19 in children [174], and patients’ clinical manifestations [13, 20]. Other previous studies discussed nurses’ efforts in preventing and controlling the spread of COVID-19 infection in neonates [175], improving clinical service in the maternity field [176], newborn care during the COVID-19 pandemic [177], and palliative care for people with dementia [178]. However, comprehensive reviews of nursing care in pediatric patients with COVID-19 are limited. Our research was conducted using a systematic method with a rigorous approach, which should be considered credible.
The three biggest domains revealed in this study are Safety, Health System, and Physiological: Basic which are comprised 79, 44, and 37 point of nursing interventions, respectively. Thus, Infection Control, Positioning, and Discharge Planning will be discussed as representative from those domains. Furthermore, we also highlight Ventilation Management: Invasive, Hyperthermia Treatment, Discharge Planning, Family Presence Facilitation, and Therapeutic Play because of their potency to fulfill practice gap in pediatric nursing alongside COVID-19 context.
Infection control
Infection control strategies are the main points highlighted in preventing the transmission of COVID-19 or SARS-CoV-2 infection. Nurses play an important role in infection prevention and control through some measures in daily practices [174]. Various changes in interventions occurred in the care of pediatric patients during the pandemic, but the emphasis of the recommendations that have been made still on the use of Personal Protective Equipment (PPE). Health workers must use PPE properly to protect themselves and prevent cross-infection, so training on the use of PPE needs to be provided for health workers [121]. In addition, nurses also need to follow the general principles of managing patients undergoing aerosol-generating procedures (AGP) [114, 115] when performing AGP such as chest compressions, airway management, ventilation, and suction [74] who are at high risk of transmitting infection. The use of PPE must be rational according to the setting, personnel, and type of activity [179].
Neonatal care settings are undergoing substantial changes. Before COVID-19, the WHO recommendation on the timing of the newborn’s first bath should be postponed until 24 hours after birth [180] considering the incidence of hypothermia in newborns. The results of a recent study even suggested delaying the first bath up to 48 hours after delivery to effectively maintain the baby’s body temperature and effectively maintain skin moisture which can have a positive impact on the development of the baby’s skin [181]. Unlike during COVID-19, babies are bathed immediately after birth to clean viral particles obtained from environmental exposure [145].
The direct contact of the baby with the mother, which was previously the main intervention carried out after birth, has turned into something that is not done or postponed until it meets the safety criteria from the transmission of COVID-19 infection. This context is the highlight of this scoping review. A total of 21 papers describe the regulation of contact between infants and mothers who are infected with COVID-19 or at risk of COVID-19. The types of interventions recommended by previous authors include avoiding skin-to-skin contact [56, 138–142], isolation of infants in negative pressure incubators [60, 67, 111, 143, 144] or isolation separately from the mother for 14 days [55, 77, 111, 120, 138, 140], rooming-in provision [61, 68, 147], and wear a face mask when breastfeeding or in close contact with infants [55–59, 62, 143].
Positioning
The prone position is highly recommended for COVID-19 patients with acute respiratory distress syndrome (ARDS) [182]. Early prone positioning is recommended for pediatric patients with moderate to severe pediatric acute respiratory distress syndrome (PARDS) for 12–18 hours per day (avoid disconnection) to improve the oxygen state [79]. The average time of prone positioning in children and adults is similar. In adult COVID-19 patients with severe ARDS, prone position can increase PaO2:FiO2, primarily in patients with PaO2:FiO2 <120 mm Hg. It can be delivered five sessions per day was 14 hours [183]. Another study noted that after 16 hours of prone position per day in adult COVID-19 patients, moderate to severe ARDS reduced mortality and improved physiological parameters [184]. The respiratory system mechanics of patients with ARDS, with or without COVID-19, were broadly similar, and the management of ARDS patients with or without COVID-19 was similar [185]. Multifactorial factors plays a role in improving oxygenation during prone ventilation by reducing lung compression and improving lung perfusion and changes in the distribution of extravascular lung fluid and secretions [186].
Discharge planning
Discharge from hospital to home or to another level of care is a transition situation in pediatric care [47, 187]. Nurses’ activities in managing patient discharge include providing patient care knowledge and skills, patient teaching, and post-discharge evaluation [47]. Discharge planning intervention recommendations were found to differ in knowledge preparation, re-examination, and post-treatment care. Before discharging a pediatric patient with COVID-19, children and families should be provided with knowledge about the post-treatment isolation period [60, 64, 86, 92, 142, 156, 158] and family tracing [172]. In addition, it must be ensured that newborns are cared for by parents or caregivers who are free from COVID-19 infection [124]. It is also important for nurses to educate patients and families about recognizing the signs and symptoms of danger to neonates and ensure that they have the ability to perform post-discharge medical procedures [68, 76, 119, 153]. The spread of infection from patients and families must be controlled by nurses by providing appropriate discharge education to prevent the spread of COVID-19.
Use of technology as telemedicine/telehealth for follow-up and fulfillment of patient needs [61, 64, 65, 87, 90, 92, 113, 146, 161–168] after discharge, seems to be the main issue in providing child services that can reduce physical contact and maintain distance during the period of social isolation or quarantine. Similar to the management of COVID-19 cases in children, the application of a safe distance in the clinical service setting [168] can limit direct contact with health workers. In this case, teleconsultation services and parental education through video media have a crucial role in maintaining the best possible service delivery to pediatric patients and their families [168].
Mechanical ventilation management
Intubation procedures occurred in 4.5% of pediatric patients admitted to intensive care units [188]. To prevent complications and air leaks in this study, nurses should check the endotracheal tube (ETT) cuff pressure at a safe limit of <20 cm H2O every 6–12 hours [79]. Our findings were similar to previous studies. Kumar et al. and Bulamba et al. [189, 190] proposed a pressure target of an ETT cuff at 20–30 cm H2O. The correct endotracheal cuff pressure must be less than the capillary perfusion pressure or less than 30 cm H2O [191]. Talekar et al. [192] also suggested ETT cuff daily monitoring every 6–12 hours. Increased pressure has the potential to decrease mucosal blood flow, possibly increasing the risk of subsequent tracheal stenosis, rupture, ventilator-associated pneumonia (VAP), and other complications [193]. Poor cuff pressure management could increase the number of days in the Intensive Care Unit (ICU) and prolong the use of mechanical ventilation [194].
Hyperthermia treatment
Another substantial change found in our review is the attitude toward fever in pediatric patients with COVID-19. Increases in body temperature need to be closely monitored even when they are minimal [92]. A previous study found maximum body temperature among the admission factors that led to the progression of COVID-19 [195]. Moreover, severe hyperthermia was expected, and increasing temperatures were independently associated with increased mortality rates [196]. A significant increase in mortality was recorded for every 0.5°C increase in maximum body temperature during COVID-19 [197].
Family presence facilitation
Patient and family-centered care (PFCC) has been an essential part of pediatric care during the pandemic [198]. Based on our findings, we recommend the presence of the families of pediatric patients in isolation. This recommendation is in line with former studies outside the COVID-19 context [199]. Additionally, our findings emphasized the challenges in involving families in child care with provisions for isolation and restrictions on admission to the care unit to stay safe and prevent the spread of the virus [25, 68]. Parents and caregivers must wear a mask, wash hands, and show average BT to reduce the risk of COVID-19 while accompanying the child [68, 150]. Other modes of family presence, such as virtual presence (video conference), should be considered when physical attendance is not possible [200]. However, in this mode, there are issues related to patient privacy and the exacerbation of racial, socioeconomic, and geographic disparities in populations that lack reliable internet access, devices, or technological literacy [153]. Several measures have been developed to maintain the family’s presence despite burden issues in pediatric isolation settings [153, 201].
Therapeutic play
The COVID-19 disease causes physical and psychological problems similar to those in the Ebola epidemic [202]. Signs and symptoms of changes in the psychological health status, coping mechanism, and causes or risk factors of pandemic stress in children and their families must be identified by pediatric nurses in treating pediatric COVID-19 patients [102, 104]. Pediatric COVID-19 patients in quarantine could experience mental health problems due to the loss or separation from parents or families who suffer from chronic illnesses [32, 34]. They could also suffer stigmatization, social exclusion [35], uncertainty about disease status, boredom, and restrictions on movements and daily activity [36]. The manifestations of psychological stress are anxiety, social interaction disorders, and negative changes in children’s behavior, such as aggression and affect [151], decreased appetite, depression, lethargy, irritability, and fear [31, 32]. Psychological interventions must be provided by child health services [34, 100] to reduce stress and increase the adaptability of children and families to life during the pandemic.
The results of this review showed that various kinds of therapeutic play interventions were recommended by previous authors to address the psychological problems of children of all ages due to the pandemic, such as playing collaborative games and painting [31, 69, 100]. In pediatric patients, playing can act as a medium to reduce loneliness, provide distractions [31], and improve health status and wellbeing [203]. However, strategies for fulfilling children’s play needs during isolation or quarantine different from those before the pandemic [203]. One guideline recommended the application of safe physical distancing in children’s physical activities and playtime [204].
The findings of this scoping review indicated that the amount of literature on physical, psychological, and social care is increasing. However, studies are lacking on the spiritual care of children and preparation for the death or loss of a child, parent, or family member, which could occur suddenly. Furthermore, cultural aspects have not been considered by many previous authors. The COVID-19 pandemic has led to many cultural changes. For example, the culture of maintaining health during COVID-19 requires wearing masks, frequent handwashing, and the increased consumption of fruits and vegetables, which may present special challenges in the pediatric population. Atout et al. [151] showed that many children refused to use masks and other personal protective equipment for non-essential reasons, such as feeling uncomfortable and feeling different from their peers. Therefore, further studies should be conducted to determine cultural influences on providing holistic care in children.
Limitations
This brief scoping review has several limitations. First, we included only articles that were published in the English language. Second, because of the heterogeneity of the design of this scoping review study, we did not perform a structured quality assessment. However, this is in line with accepted methodology of scoping review proposed by Arksey and O’Malley [43]. We accept low levels of evidence in order to understand the whole landscape of published literature.
Implications for practice
Besides physical complaint, the COVID-19 situation has led to psychological problems in children who suffer parental separation, social isolation, and stigmatization. Pediatric nurses are expected to be able to propose various creative ways to meet the needs of children and families despite the various limitations in isolation rooms. Pediatric should promote family presence where it is possible [200]. Using technology might become a good alternative to connect children with their families where physical contact is unaffordable. Some gadgets have developed specific software that enables the child, family, and health care team to stay connected all day. Pediatric nurses should manage the daily schedule where family can connect to health care team among the other routine tasks along the shift period [198].
Furthermore, the pandemic has caused a new situation that affects the readiness of both children and families in undergoing the transition from hospitalization to isolation at home. On this occasion, discharge planning can play an essential role in preparing child and family knowledge, and skill. Parents and child should be educated about the post-treatment isolation period including routine care, nutritional and emotional support, home isolation procedures, and sign of emergency. Pediatric nurses should also help family to decide on child-caregiver at home which may lead to family dilemma. The pandemic situation has prompted pediatric nurses to show leadership in managing resources to ensure that good nursing care has been delivered to consider all needs of pediatric patients and their families.
Conclusion
We found Safety, Health System, and Physiological: Basic as the three most domain revealed in this brief summarizing study. Accordingly, our guideline in Infection Control, Positioning, and Discharge Planning should be considered to be delivered to in-hospital pediatric nursing practice. Ventilation Management: Invasive, Hyperthermia Treatment intervention was formulated to address one of the major physical conditions in pediatric with COVID-19. Nursing intervention should pay attention to pediatric patients with psychological problem by providing Family Presence Facilitation, and Therapeutic Play. Using technology to promote proper discharge planning in pandemic context found to be essential to delivered nursing practice comprehensively. Pediatric nurses should collaborate with their interprofessional team members and use the resources available to ensure the best care despite various restrictions during the COVID-19 pandemic.
Supporting information
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
We would like to thank all pediatric nurses for their outstanding dedication to delivering nursing care during the COVID-19 pandemic around the world. We also thank our colleagues in the Indonesian Pediatric Nurses Association for their strong support while we conducted this study. Our special thanks to pediatric patients and families struggling during the COVID 19 pandemic. Finally, we gratefully acknowledge Ns. Bejo Utomo, MSc for proofreading and technical support.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
DW was funded by KEMENRISTEK/BRIN under Hibah PDUPT Tahun Anggaran 2021 (Contract No: NKB-072/UN2.RST/HKP.05.00/2021) The funders did not have authority to decided research methodology and article to be published.
References
- 1.Singhal T. A review of Coronavirus Disease-2019 (COVID-19). Indian J Pediatr. 2020;87:281–6. doi: 10.1007/s12098-020-03263-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ren L, Wang Y, Wu Z, Xiang Z, Guo L, Xu T, et al. Identification of a novel coronavirus causing severe pneumonia in human: A descriptive study. Chin Med J (Engl). 2020;133(9):1015–24. doi: 10.1097/CM9.0000000000000722 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hafeez A, Ahmad S, Siddqui SA, Ahmad M, Mishra S. A review of COVID-19 (Coronavirus Disease-2019) diagnosis, treatments and prevention. Eurasian J Med Oncol. 2020;4(2):116–25. 10.14744/ejmo.2020.90853. [DOI] [Google Scholar]
- 4.World Health Organization. Novel Coronavirus–China [Internet]. Geneva: World Health Organization; 2020. Available from: https://www.who.int/emergencies/disease-outbreak-news/item/2020-DON233. [Google Scholar]
- 5.World Health Organization. Naming the coronavirus disease (COVID-19) and the virus that causes it [Internet]. Geneva: World Health Organization; 2020. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it. [Google Scholar]
- 6.Adhikari SP, Meng S, Wu Y, Mao Y, Ye R, Wang Q, et al. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infect Dis Poverty. 2020;9(1):29. doi: 10.1186/s40249-020-00646-x . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization. WHO coronavirus disease (COVID-19) dashboard [internet]. Geneva: World Health Organization; 2020. Available from: https://covid19.who.int/. [Google Scholar]
- 8.National Institutes of Health. COVID-19 is an emerging, rapidly evolving situation. Special population. Bethesda: National Institutes of Health; 2020. [Google Scholar]
- 9.Barton M, Mehta K, Kumar K, Lu J, le Saux N, Sampson M, et al. COVID- 19 infection in children: estimating pediatric morbidity and mortality. medRxiv. 2020;1–26. 10.1101/2020.05.05.20091751. [DOI] [Google Scholar]
- 10.Tagarro A, Epalza C, Santos M, Sanz-Santaeufemia FJ, Otheo E, Moraleda C, et al. Screening and severity of coronavirus disease 2019 (COVID-19) in children in Madrid, Spain. JAMA Pediatr. 2020;e201346. doi: 10.1001/jamapediatrics.2020.1346 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z, et al. Epidemiology of COVID-19 among children in China. Pediatrics. 2020;145(6):e20200702. doi: 10.1542/peds.2020-0702 . [DOI] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. Care for children: summary of recent changes. Atlanta: Centers for Disease Control and Prevention; 2020. [Google Scholar]
- 13.Hoang A, Chorath K, Moreira A, Evans M, Burmeister-morton F, Burmeister F, et al. COVID-19 in 7780 pediatric patients: a systematic review. EClinicalMedicine. 2020;24:100433. doi: 10.1016/j.eclinm.2020.100433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zimmermann P, Curtis N. Coronavirus infections in children including COVID-19: an overview of the epidemiology, clinical features, diagnosis, treatment and prevention options in children. Pediatr Infect Dis J. 2020;39(5):355–68. doi: 10.1097/INF.0000000000002660 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Girona-Alarcon M, Bobillo-Perez S, Sole-Ribalta A, Hernandez L, Guitart C, Suarez R, et al. The different manifestations of COVID-19 in adults and children: a cohort study in an intensive care unit. BMC Infect Dis. 2021;21(1):87. doi: 10.1186/s12879-021-05786-5 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cai X, Ma Y, Li S, Chen Y, Rong Z, Li W. Clinical characteristics of 5 COVID-19 cases with non-respiratory symptoms as the first manifestation in children. Front Pediatr. 2020;8:258. doi: 10.3389/fped.2020.00258 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Soltani J, Sedighi I, Shalchi Z, Sami G, Moradveisi B, Nahidi S. Pediatric coronavirus disease 2019 (COVID-19): an insight from west of Iran. North Clin Istanb. 2020;7(3):284–91. doi: 10.14744/nci.2020.90277 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Choi S, Kim HW, Kang J, Kim DH, Cho EY. Epidemiology and clinical features of coronavirus disease 2019 in children. Clin Exp Pediatr. 2020;63(4):125–32. doi: 10.3345/cep.2020.00535 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hong H, Wang Y, Chung H, Chen C. Clinical characteristics of novel coronavirus disease 2019 (COVID-19) in newborns, infants and children. Pediatr Neonatol. 2020;61(2):131–2. doi: 10.1016/j.pedneo.2020.03.001 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chang TH, Wu JL, Chang LY. Clinical characteristics and diagnostic challenges of pediatric COVID-19: A systematic review and meta-analysis. J Formos Med Assoc. 2020;119(5):982–9. doi: 10.1016/j.jfma.2020.04.007 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Remppis J, Ganzenmueller T, Vasconcelos MK, Heinzel O, Handgretinger R, Renk H. A case series of children and young people admitted to a tertiary care hospital in Germany with COVID-19. BMC Infect Dis. 2021;21(1):133. doi: 10.1186/s12879-021-05791-8 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chao JY, Derespina KR, Herold BC, Goldman DL, Aldrich M, Weingarten J, et al. Clinical characteristics and outcomes of hospitalized and critically ill children and adolescents with coronavirus disease 2019 at a tertiary care medical center in New York City. J Pediatr. 2020;223:14–19.e2. doi: 10.1016/j.jpeds.2020.05.006 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bhuiyan MU, Stiboy E, Hassan MZ, Chan M, Islam MS, Haider N, et al. Epidemiology of COVID-19 infection in young children under five years: A systematic review and meta-analysis. Vaccine. 2021;39(4):667–77. doi: 10.1016/j.vaccine.2020.11.078 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.de Souza TH, Nadal JA, Nogueira RJN, Pereira RM, Brandão MB. Clinical manifestations of children with COVID-19: a systematic review. Pediatr Pulmonol. 2020;55(8):1892–9. doi: 10.1002/ppul.24885 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Farshi MR, Jabraeili M, Moharrami N, Malakouti J. Nursing care in a child with coronavirus disease 2019: a case study. Hormozgan Med J. 2020;24(4):e108040. 10.5812/hmj.108040. [DOI] [Google Scholar]
- 26.Li WHC, Chung JOK, Ho KY, Kwok BMC. Play interventions to reduce anxiety and negative emotions in hospitalized children. BMC Pediatr. 2016;16:36. doi: 10.1186/s12887-016-0570-5 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Salmela M, Salantera S, Aronen E. Child-reported hospital fears in 4 to 6-year-old children. Pediatr Nurs. 2009;35(5);269–76. . [PubMed] [Google Scholar]
- 28.Fernandes SC, Arriaga P. The effects of clown intervention on worries and emotional responses in children undergoing surgery. J Health Psychol. 2010;15(3):405–15. doi: 10.1177/1359105309350231 . [DOI] [PubMed] [Google Scholar]
- 29.Li HCW, Lopez V, Lee TLI. Effects of preoperative therapeutic play on outcomes of school-age children undergoing day surgery. Res Nurs Health. 2007;30(3):320–32. doi: 10.1002/nur.20191 . [DOI] [PubMed] [Google Scholar]
- 30.Bsiri-Moghaddam K, Basiri-Moghaddam M, Sadeghmoghaddam L, Ahmadi F. The concept of hospitalization of children from the view point of parents and children. Iran J Pediatr. 2011;21(2):201–8. . [PMC free article] [PubMed] [Google Scholar]
- 31.Jiao WY, Wang LN, Liu J, Fang SF, Jiao FY, Pettoello-Mantovani M, et al. Behavioral and emotional disorders in children during the COVID-19 epidemic. J Pediatr. 2020;221:264–6.e1. doi: 10.1016/j.jpeds.2020.03.013 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Passanisi S, Pecoraro M, Pira F, Alibrandi A, Donia V, Lonia P, et al. Quarantine due to the COVID-19 pandemic from the perspective of pediatric patients with type 1 diabetes: A web-based survey. Front Pediatr. 2020;8:491. doi: 10.3389/fped.2020.00491 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Conlon C, McDonnell T, Barrett M, Cummins F, Deasy C, Hensey C, et al. The impact of the COVID-19 pandemic on child health and the provision of Carein Paediatric Emergency Departments: a qualitative study of frontline emergency care staff. BMC Health Serv Res. 2021;21:279. doi: 10.1186/s12913-021-06284-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liu JJ, Bao Y, Huang X, Shi J, Lu L. Mental health considerations for children quarantined because of COVID-19. Lancet Child Adolesc Health. 2020;4(5):347–9. doi: 10.1016/S2352-4642(20)30096-1 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Imran N, Aamer I, Sharif MI, Bodla ZH, Naveed S. Psychological burden of quarantine in children and adolescents: A rapid systematic review and proposed solutions. Pak J Med Sci. 2020;36(5):1106–16. doi: 10.12669/pjms.36.5.3088 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–20. doi: 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Góes FGB, da Silva ACSS, Dos Santos AST, Pereira-Ávila FMV, da Silva LJ, da Silva LF, et al. Challenges faced by pediatric nursing workers in the face of the covid-19 pandemic. Rev Lat Am Enfermagem. 2020;28:e3367. doi: 10.1590/1518-8345.4550.3367 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sharma SK, Nuttall C, Kalyani V, Hemlata. Clinical nursing care guidance for management of patient with COVID-19. J Pak Med Assoc. 2020;70(Suppl3)(5):S118–23. doi: 10.5455/JPMA.29 . [DOI] [PubMed] [Google Scholar]
- 39.Hu Y, Wang L, Hu S, Fang F. Facility-level case report of nursing care processes for patients with suspected 2019 Novel Coronavirus disease in Shanghai, China. J Emerg Nurs. 2020;46(6):898–906. doi: 10.1016/j.jen.2020.08.001 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gilissen J, Pivodic L, Unroe KT, Block L Van den. International COVID-19 palliative care guidance for nursing homes leaves key themes unaddressed. J Pain Symptom Manage. 2020;60(2):e56–69. doi: 10.1016/j.jpainsymman.2020.04.151 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Paterson C, Gobel B, Gosselin T, Haylock PJ, Papadopoulou C, Slusser K, et al. Oncology nursing during a pandemic: Critical reflections in the context of COVID-19. Semin Oncol Nurs. 2020;36(3):151028. doi: 10.1016/j.soncn.2020.151028 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Deitrick K, Adams J, Davis J. Emergency nursing care of patient with novel coronavirus disease 2019. J Emerg Nurse. 2020;46(6):748–59. doi: 10.1016/j.jen.2020.07.010 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 44.McMeekin N, Wu O, Germeni E, Briggs A. How methodological frameworks are being developed: evidence from a scoping review. BMC Med Res Methodol. 2020;20(1):173. doi: 10.1186/s12874-020-01061-4 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5:69. doi: 10.1186/1748-5908-5-69 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Aromataris EMZ. JBI Manual for Evidence Synthesis. Adelaide: Joanna Briggs Institute; 2020. Available from: https://synthesismanual.jbi.global. [Google Scholar]
- 47.Butcher HK, Bulechek GM, Dochterman JM, Wagner CM. Nursing Intervention Classification (NIC). 7th ed. Missouri: Elsevier; 2018. [Google Scholar]
- 48.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73. doi: 10.7326/M18-0850 . [DOI] [PubMed] [Google Scholar]
- 49.Chen ZM, Fu JF, Shu Q, Chen YH, Hua CZ, Li FB, et al. Diagnosis and treatment recommendations for pediatric respiratory infection caused by the 2019 novel coronavirus. World J Pediatr. 2020;16(3):240–6. doi: 10.1007/s12519-020-00345-5 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Devrim I, Bayram N. Infection control practices in children during COVID-19 pandemic: differences from adults. Am J Infect Control. 2020;48(8);933–9. doi: 10.1016/j.ajic.2020.05.022 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shen K, Yang Y, Wang T, Zhao D, Jiang Y, Jin R, et al. Diagnosis, treatment, and prevention of 2019 novel coronavirus infection in children: experts’ consensus statement. World J Pediatr. 2020;16(3):223–31. doi: 10.1007/s12519-020-00343-7 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Marino LV, Valla FV, Tume LN, Jotterand-Chaparro C, Moullet C, Latten L, et al. Considerations for nutrition support in critically ill children with COVID-19 and paediatric inflammatory multisystem syndrome temporally associated with COVID-19. Clin Nutr. 2021;40(3):895–900. doi: 10.1016/j.clnu.2020.10.007 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Joosten KFM, Eveleens RD, Verbruggen SCAT. Nutritional support in the recovery phase of critically ill children. Curr Opin Clin Nutr Metab Care. 2019;22(2):152–8. doi: 10.1097/MCO.0000000000000549 . [DOI] [PubMed] [Google Scholar]
- 54.Mihatsch W, Shamir R, van Goudoever JB, Fewtrell M, Lapillonne A, Lohner S, et al. ESPGHAN/ESPEN/ESPR/CSPEN guidelines on pediatric parenteral nutrition: Guideline development process for the updated guidelines. Clin Nutr. 2018;37(6 Pt B):2306–8. doi: 10.1016/j.clnu.2018.06.943 . [DOI] [PubMed] [Google Scholar]
- 55.American Academy of Pediatrics. FAQs: Management of Infants Born to Mothers with Suspected or Confirmed COVID-19 [internet]. American Academy of Pediatrics; 2020. Available from: https://www.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/clinical-guidance/faqs-management-of-infants-born-to-covid-19-mothers/. [Google Scholar]
- 56.Chawla D, Chirla D, Dalwai S, Deorari AK, Ganatra A, Gandhi A, et al. Perinatal-neonatal management of COVID-19 infection—guidelines of the Federation of Obstetric and Gynaecological Societies of India (FOGSI), National Neonatology Forum of India (NNF), and Indian Academy of Pediatrics (IAP). Indian Pediatr. 2020;57(6):536–48. doi: 10.1007/s13312-020-1852-4 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ezenwa BN, Fajolu IB, Akinajo OR, Makwe CC, Oluwole AA, Akase IE, et al. Management of covid-19: a practical guideline for maternal and newborn health care providers in Sub-Saharan Africa. J Matern Fetal Neonatal Med. 2020;1–7. doi: 10.1080/14767058.2020.1763948 . [DOI] [PubMed] [Google Scholar]
- 58.Gale C, Quigley MA, Placzek A, Knight M, Ladhani S, Draper ES, et al. Characteristics and outcomes of neonatal SARS-CoV-2 infection in the UK: A prospective national cohort study using active surveillance. Lancet Child Adolesc Health. 2021;5(2):113–21. doi: 10.1016/S2352-4642(20)30342-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Giuliani C, Li Volsi P, Brun E, Chiambretti A, Giandalia A, Tonutti L, et al. Breastfeeding during the COVID-19 pandemic: suggestions on behalf of woman study group of AMD. Diabetes Res Clin Pract. 2020;165:108239. doi: 10.1016/j.diabres.2020.108239 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Green J, Petty J, Bromley P, Walker K, Jones L. COVID-19 in babies: knowledge for neonatal care. J Neonatal Nurs. 2020;26(5):239–46. doi: 10.1016/j.jnn.2020.06.005 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hester M. AAP issues guidance for managing infants born to mothers with COVID-19 [internet]. Dayton, OH: Contemporary Pediatrics; 2020. Available from: https://www.contemporarypediatrics.com/view/aap-issues-guidance-managing-infants-born-mothers-covid-19. [Google Scholar]
- 62.Moro GE, Bertino E. Breastfeeding, human milk collection and containers, and human milk banking: hot topics during the COVID-19 pandemic. J Hum Lact. 2020;36(4):604–8. doi: 10.1177/0890334420934391 . [DOI] [PubMed] [Google Scholar]
- 63.Peng S, Zhu H, Yang L, Cao L, Huang X, Dynes M, et al. A study of breastfeeding practices, SARS-CoV-2 and its antibodies in the breast milk of mothers confirmed with COVID-19. Lancet Reg Health West Pac. 2020;4:100045. doi: 10.1016/j.lanwpc.2020.100045 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Trevisanuto D, Weiner G, Lakshminrusimha S, Azzimonti G, Nsubuga JB, Velaphi S, et al. Management of mothers and neonates in low resources setting during covid-19 pandemia. J Matern Fetal Neonatal Med. 2020;1–12. doi: 10.1080/14767058.2020.1784873 . [DOI] [PubMed] [Google Scholar]
- 65.Rajapakse N, Dixit D. Human and novel coronavirus infections in children: a review. Paediatr Int Child Health. 2021;41(1):36–55. doi: 10.1080/20469047.2020.1781356 . [DOI] [PubMed] [Google Scholar]
- 66.Pereira A, Cruz-Melguizo S, Adrien M, Fuentes L, Marin E, Forti A, et al. Breastfeeding mothers with COVID-19 infection: a case series. Int Breastfeed J. 2020;15(1):69. doi: 10.1186/s13006-020-00314-8 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Krishnamurthy G, Sahni R, Leone T, Kim F, Brooks MC, Morales SV, et al. Care of the COVID-19 exposed complex newborn infant. Semin Perinatol. 2020;44(7):151282. doi: 10.1016/j.semperi.2020.151282 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Montes MT, Herranz-Rubia N, NeNe Nursing Group. Neonatal nursing in the COVID-19 pandemic: can we improve the future? J Neonatal Nurs. 2020;26(5):247–51. doi: 10.1016/j.jnn.2020.07.005 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Aleebrahim-Dehkordi E, Soveyzi F, Deravi N, Rabbani Z, Saghazadeh A, Rezaei N. Human coronaviruses SARS-CoV, MERS-CoV, and SARS-CoV-2 in children. J Pediatr Nurs. 2020;56:70–9. doi: 10.1016/j.pedn.2020.10.020 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sarman A, Tuncay S. Principles of approach to suspected or infected patients related Covid‐19 in newborn intensive care unit and pediatric intensive care unit. Perspect Psychiatr Care. 2021;57(2):957–64. doi: 10.1111/ppc.12643 . [DOI] [PubMed] [Google Scholar]
- 71.Kazzaz Y m, Alkhalaf H, Alharbi M, Al Shaalan M, Almuneef M, Alshehri A, et al. Hospital preparedness and management of pediatric population during COVID‑19 outbreak. Ann Thorac Med. 2020;15(3):107–17. doi: 10.4103/atm.ATM_212_20 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Matava CT, Kovatsis PG, Lee JK, Castro P, Denning S, Yu J, et al. Pediatric airway management in COVID-19 patients: Consensus guidelines from the Society for Pediatric Anesthesia’s Pediatric Difficult Intubation Collaborative and the Canadian Pediatric Anesthesia Society. Anesth Analg. 2020;131(1):61–73. doi: 10.1213/ANE.0000000000004872 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kallem VR, Sharma D. COVID 19 in neonates. J Matern Fetal Neonatal Med. 2020;1–9. doi: 10.1080/14767058.2020.1759542 . [DOI] [PubMed] [Google Scholar]
- 74.Nolan JP, Monsieurs KG, Bossaert L, Böttiger BW, Greif R, Lott C, et al. European Resuscitation Council COVID-19 guidelines executive summary. Resuscitation. 2020;153:45–55. doi: 10.1016/j.resuscitation.2020.06.001 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Vogt TM, Zhang F, Banks M, Black C, Arthur B, Kang Y, et al. Provision of pediatric immunization services during the covid-19 pandemic: an assessment of capacity among pediatric immunization providers participating in the vaccines for children program—United States, May 2020. MMWR Morb Mortal Wkly Rep. 2020;69(27):859–63. doi: 10.15585/mmwr.mm6927a2 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Cavicchiolo ME, Doglioni N, Ventola MA, Biban P, Baraldi E, Trevisanuto D. Neonatal emergency transport system during COVID-19 pandemic in the Veneto Region: proposal for standard operating procedures. Pediatr Res. 2021;89:399–401. doi: 10.1038/s41390-020-0937-z [DOI] [PubMed] [Google Scholar]
- 77.Udrea DS, Lopez M, Avesar M, Qureshi S, Moretti A, Abd-Allah SA, et al. Acute COVID-19 infection in a pediatric patient with ROHHAD. J Pediatr Genet. 2020;4. 10.1055/s-0040-1718874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Carlotti APdCP, de Carvalho WB, Johnston C, Rodriguez IS, Delgado AF. Covid-19 diagnostic and management protocol for pediatric patients. Clinics (Sao Paulo). 2020;75:e1894. doi: 10.6061/clinics/2020/e1894 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.European Society Paediatric and Neonatal Intensive Care. Nursing guidance for the care of the child with suspected or proven COVID-19 infection [internet]. Geneva: European Society for Paediatric and Neonatal Intensive Care; 2020. Available from: https://www.espnic.eu/nursing-guidance-for-the-care-of-the-child-with-suspected-or-proven-covid-19-infection/. [Google Scholar]
- 80.Kache S, Chisti MJ, Gumbo F, Mupere E, Zhi X, Nallasamy K, et al. COVID-19 PICU guidelines: for high- and limited-resource settings. Pediatr Res. 2020;88(5):705–16. doi: 10.1038/s41390-020-1053-9 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Shang Y, Pan C, Yang X, Zhong M, Shang X, Wu Z, et al. Management of critically ill patients with COVID-19 in ICU: statement from front-line intensive care experts in Wuhan, China. Ann Intensive Care. 2020;10(1):73. doi: 10.1186/s13613-020-00689-1 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kneyber MCJ, Medina A, i Alapont VM, Blokpoel R, Brierly J, Chidini G, et al. Practice recommendations for the management of children with suspected or proven COVID-19 infections from the Paediatric Mechanical Ventilation Consensus Conference (PEMVECC) and the section Respiratory Failure from the European Society for Paediatric and Neonatal Intensive Care (ESPNIC). Geneva: European Society of Paediatric and Neonatal Intensive Care; 2020. Available from: https://sviluppo.senzafiltro.it/espnic/wp-content/uploads/2021/07/2020-ESPNIC-PEMVECC-COVID-19-practice-recommendations.pdf. [Google Scholar]
- 83.Marraro GA, Spada C. Consideration of the respiratory support strategy of severe acute respiratory failure caused by SARS-CoV-2 infection in children. Zhongguo Dang Dai Er Ke Za Zhi. 2020;22(3):183–94. doi: 10.7499/j.issn.1008-8830.2020.03.002 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hahn A, Vater L. COVID-19 and kids: managing chronic pain at home [internet]. Columbus, OH: Nationwide Children’s Hospital; 2020. Available from: https://www.nationwidechildrens.org/family-resources-education/700childrens/2020/07/covid-19-and-kids-managing-chronic-pain-at-home. [Google Scholar]
- 85.Kassab M, Nuseair K, Al-Qaoud N, Hamadneh S, Roy AN. Is facilitated tucking by parents more effective than dextrose water (10%) in reducing full-term neonatal pain during the heel-lancing procedure: a randomized controlled trial. Int J Pharm Res. 2020;12(1):2178–86. 10.31838/ijpr/2020.12.01.341. [DOI] [Google Scholar]
- 86.Kaushik A, Gupta S, Sood M. COVID-19 in children: clinical approach and management- correspondence. Indian J Pediatr. 2020;87(11):970–2. doi: 10.1007/s12098-020-03374-0 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Teoh CW, Gaudreault-Tremblay MM, Blydt-Hansen TD, Goldberg A, Arora S, Feber J, et al. Management of pediatric kidney transplant patients during the COVID-19 pandemic: guidance from the Canadian Society of Transplantation Pediatric Group. Can J Kidney Health Dis. 2020;7:2054358120967845. doi: 10.1177/2054358120967845 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Extracorporeal Life Support Organization. Extracorporeal Life Support Organization COVID-19 Interim Guidelines. Ann Arbor: Extracorporeal Life Support Organization; 2020. [Google Scholar]
- 89.Venturini E, Montagnani C, Garazzino S, Donà D, Pierantoni L, Lo Vecchio A, et al. Treatment of children with COVID-19: position paper of the Italian Society of Pediatric Infectious Disease. Ital J Pediatr. 2020;46(1):139. doi: 10.1186/s13052-020-00900-w . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kumar P, Dawman L, Panda P, Sharawat IK. Feasibility and effectiveness of teleconsultation in children with epilepsy amidst the ongoing COVID-19 pandemic in a resource-limited country. Seizure. 2020;81:29–35. doi: 10.1016/j.seizure.2020.07.013 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Nicholas DB, Belletrutti M, Dimitropoulos G, Katz SL, Rapoport A, Urschel S, et al. Perceived impacts of the COVID-19 pandemic on pediatric care in Canada: a roundtable discussion. Glob Pediatr Heal. 2020;7:2333794X20957652. doi: 10.1177/2333794X20957652 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Monzani A, Ragazzoni L, Corte FD, Rabbone I, Franc JM. COVID-19 pandemic: perspective from Italian pediatric emergency physicians. Disaster Med Public Health Prep. 2020;14(5):648–51. doi: 10.1017/dmp.2020.198 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Shen KL, Yang YH, Jiang RM, Wang TY, Zhao DC, Jiang Y, et al. Updated diagnosis, treatment and prevention of COVID-19 in children: experts’ consensus statement (condensed version of the second edition). World J Pediatr. 2020;16(3):232–9. doi: 10.1007/s12519-020-00362-4 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Schmitt BD, Offit PA. Could fever improve COVID-19 outcomes?. Contemp Pediatr. 2020;37(7):8. [Google Scholar]
- 95.Peck JL. COVID-19: impacts and implications for pediatric practice. J Pediatr Health Care. 2020;34(6):619–29. doi: 10.1016/j.pedhc.2020.07.004 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.MaGowan N, Darcy J, Mosiello A, Gomes C, Miller N. Navigating through the uncharted territory of Multisystem Inflammatory Syndrome in Children (MIS-C): what the pediatric clinical nurse must know. Pediatr Nurs. 2020;46(6):273–7. [Google Scholar]
- 97.United Nations International Children’s Emergency Fund India Country Office & ChildLine India Foundation. Psychosocial support for children during COVID-19: a manual for parents and caregivers. Lucknow: United Nations International Children’s Emergency Fund India Country Office; 2020. Available from: https://www.unicef.org/india/reports/psychosocial-support-children-during-covid-19. [Google Scholar]
- 98.Willer BL, Thung AK, Corridore M, D’Mello AJ, Schloss BS, Malhotra PS, et al. The otolaryngologist’s and anesthesiologist’s collaborative role in a pandemic: a large quaternary pediatric center’s experience with COVID-19 preparation and simulation. Int J Pediatr Otorhinolaryngol. 2020;136:110174. doi: 10.1016/j.ijporl.2020.110174 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Green J, Staff L, Bromley P, Jones L, Petty J. The implications of face masks for babies and families during the COVID-19 pandemic: a discussion paper. J Neonatal Nurs. 2021;27(1):21–5. doi: 10.1016/j.jnn.2020.10.005 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Ye J. Pediatric mental and behavioral health in the period of quarantine and social distancing with COVID-19. JMIR Pediatr Parent. 2020;3(2):e19867. doi: 10.2196/19867 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Mirlashari J, Ebrahimpour F, Salisu WJ. War on two fronts: experience of children with cancer and their family during COVID-19 pandemic in Iran. J Pediatr Nurs. 2021;57:25–31. doi: 10.1016/j.pedn.2020.10.024 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Dokken D, Ahmann E, Miller D, Weaver J. Mental health needs during COVID-19: Responses in pediatric health care. Pediatr Nurs. 2020. Nov;46(6):304–7. [Google Scholar]
- 103.Slone JS, Ozuah N, Wasswa P. Caring for children with cancer in Africa during the COVID-19 crisis: implications and opportunities. Pediatr Hematol Oncol. 2020;37(7):549–53. doi: 10.1080/08880018.2020.1772913 . [DOI] [PubMed] [Google Scholar]
- 104.Robinson C, Ruhl M, Kirpalani A, Alabbas A, Noone D, Teoh CW, et al. Management of Canadian pediatric patients with glomerular diseases during the COVID-19 pandemic: Recommendations from the Canadian Association of Pediatric Nephrologists COVID-19 Rapid Response Team. Can J Kidney Heal Dis. 2020;7:1–17. doi: 10.1177/2054358120970713 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Leff RA, Setzer E, Cicero MX, Auerbach M. Changes in pediatric emergency department visits for mental health during the COVID-19 pandemic: a cross-sectional study. Clin Child Psychol Psychiatry. 2021;26(1):33–8. doi: 10.1177/1359104520972453 . [DOI] [PubMed] [Google Scholar]
- 106.Wang L, Shi Y, Xiao T, Fu J, Feng X, Mu D, et al. Chinese expert consensus on the perinatal and neonatal management for the prevention and control of the 2019 novel coronavirus infection (First edition). Ann Transl Med. 2020;8(3):47. doi: 10.21037/atm.2020.02.20 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kari JA, Shalaby MA, Albanna AS, Alahmadi T, Sukkar SA, MohamedNur HAH, et al. Coronavirus disease in children: a multicentre study from the Kingdom of Saudi Arabia. J Infect Public Health. 2021;14(4):543–9. doi: 10.1016/j.jiph.2021.01.011 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Shi Y, Wang X, Liu G, Zhu Q, Wang J, Yu H, et al. A quickly, effectively screening process of novel corona virus disease 2019 (COVID-19) in children in Shanghai, China. Ann Transl Med. 2020. Mar;8(5):241. doi: 10.21037/atm.2020.03.22 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Abuali M, Bonner R, Irigoyen M. Operationalizing an academic pediatric practice during the COVID-19 crisis. Am J Infect Control. 2021;49(2):226–8. doi: 10.1016/j.ajic.2020.07.003 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Bressan S, Buonsenso D, Farrugia R, Parri N, Oostenbrink R, Titomanlio L, et al. Preparedness and response to pediatric COVID-19 in European Emergency Departments: a survey of the REPEM and PERUKI networks. Ann Emerg Med. 2020;76(6):788–800. doi: 10.1016/j.annemergmed.2020.05.018 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ding H, Shi Z, Ruan Z, Cheng X, Li R, Zhang L, et al. Consideration of the management of pediatric fever clinics during the novel coronavirus pneumonia outbreak. Disaster Med Public Health Prep. 2020;1–7. doi: 10.1017/dmp.2020.289 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Yago MAR, Mayayo IA, López RG, Ángel MNP, Miranda AP, Aracil MC, et al. Recommendations on cardiopulmonary resuscitation in patients with suspected or confirmed SARS-CoV-2 infection (COVID-19). Executive summary. Med Intensiva (English Ed). 2020;44(9):566–76. doi: 10.1016/j.medin.2020.05.004 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Taylor JB, Oermann CM, Deterding RR, Redding G, Davis SD, Piccione J, et al. Innovating and adapting in pediatric pulmonology and sleep medicine during the COVID‐19 pandemic: ATS Pediatric assembly web committee consensus statement for initial COVID‐19 virtual response. Pediatr Pulmonol. 2021;56(2):539–50. doi: 10.1002/ppul.25218 . [DOI] [PubMed] [Google Scholar]
- 114.Frauenfelder C, Butler C, Hartley B, Cochrane L, Jephson C, Nash R, et al. Practical insights for paediatric otolaryngology surgical cases and performing microlaryngobronchoscopy during the COVID-19 pandemic. Int J Pediatr Otorhinolaryngol. 2020;134:110030. doi: 10.1016/j.ijporl.2020.110030 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Soma M, Jacobson I, Brewer J, Blondin A, Davidson G, Singham S. Operative team checklist for aerosol generating procedures to minimise exposure of healthcare workers to SARS-CoV-2. Int J Pediatr Otorhinolaryngol. 2020;134:110075. doi: 10.1016/j.ijporl.2020.110075 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Jain PN, Finger L, Schieffelin JS, Zerr DM, Hametz PA. Responses of three urban U.S. children’s hospitals to COVID-19: Seattle, New York and New Orleans. Paediatr Respir Rev. 2020;35:15–9. doi: 10.1016/j.prrv.2020.06.002 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Al Juhani T, Al Zughaibi N, Haroun A, Al Saad A. Perioperative care of pediatric anesthesia for children with suspected or confirmed COVID-19. Saudi J Anaesth. 2020;14(3):370–7. doi: 10.4103/sja.SJA_358_20 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Lakhani A, Sharma E. Corona virus (Covid-19)–ITS implications in pediatric orthopedic care. J Orthop. 2020;21:326–30. doi: 10.1016/j.jor.2020.06.002 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Sullivan M, Bouffet E, Rodriguez-Galindo C, Luna-Fineman S, Khan MS, Kearns P, et al. The COVID‐19 pandemic: a rapid global response for children with cancer from SIOP, COG, SIOP‐E, SIOP‐PODC, IPSO, PROS, CCI, and St Jude Global. Pediatr Blood Cancer. 2020;67(7):e28409. doi: 10.1002/pbc.28409 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Thampi S, Yap A, Fan L, Ong J. Special considerations for the management of COVID-19 pediatric patients in the operating room and pediatric intensive care unit in a tertiary hospital in Singapore. Paediatr Anaesth. 2020;30(6):642–6. doi: 10.1111/pan.13863 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Tan W, Ye Y, Yang Y, Chen Z, Yang X, Zhu C, et al. Whole-process emergency training of personal protective equipment helps healthcare workers against COVID-19: design and effect. J Occup Environ Med. 2020;62(6):420–3. doi: 10.1097/JOM.0000000000001877 . [DOI] [PubMed] [Google Scholar]
- 122.Lotfi M, Hamblin MR, Rezaei N. COVID-19: Transmission, prevention, and potential therapeutic opportunities. Clin Chim Acta. 2020;508:254–66. doi: 10.1016/j.cca.2020.05.044 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.DeFazio JR, Kahan A, Fallon EM, Griggs C, Kabagambe S, Zitsman J, et al. Development of pediatric surgical decision-making guidelines for COVID-19 in a New York City children’s hospital. J Pediatr Surg. 2020;55(8):1427–30. doi: 10.1016/j.jpedsurg.2020.05.043 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Verma S, Lumba R, Lighter JL, Bailey SM, Wachtel E V, Kunjumon B, et al. Neonatal intensive care unit preparedness for the Novel Coronavirus Disease-2019 pandemic: a New York City hospital perspective. Curr Probl Pediatr Adolesc Health Care. 2020;50(4):100795. doi: 10.1016/j.cppeds.2020.100795 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Royal College of Paediatrics and Child Health. BAPM—COVID-19: Frequently asked questions within neonatal services [internet]. Bristol: British Association Perinatal Medicine; 2020. Available from: https://www.rcpch.ac.uk/resources/bapm-covid-19-pandemic-frequently-asked-questions-within-neonatal-services. [Google Scholar]
- 126.World Health Organization. Clinical management of COVID-19: interim guidance [internet]. Geneva: World Health Organization; 2020. Available from: https://apps.who.int/iris/handle/10665/332196. [Google Scholar]
- 127.WIDEX. How you can help communication when face masks are needed [internet]. WIDEX; 2020. Available from: https://www.widexpro.com/en-ca/blog/global/how-you-can-help-communication-when-face-masks-are-needed/. [Google Scholar]
- 128.Center for Disease Control & Prevention. Strategies for optimizing the supply of N95 respirators [internet]. Atlanta: Center for Disease Control & Prevention; 2021. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/respirators-strategy/index.html. [Google Scholar]
- 129.Yonker LM, Neilan AM, Bartsch Y, Patel AB, Regan J, Arya P, et al. Pediatric severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2): clinical presentation, infectivity, and immune responses. J Pediatr. 2020;227:45–52.e5. doi: 10.1016/j.jpeds.2020.08.037 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Wei L, Huang W, Lu X, Wang Y, Cheng L, Deng R, et al. Contamination of SARS-CoV-2 in patient surroundings and on personal protective equipment in a non-ICU isolation ward for COVID-19 patients with prolonged PCR positive status. Antimicrob Resist Infect Control. 2020;9:167. doi: 10.1186/s13756-020-00839-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Bouffet E, Challinor J, Sullivan M, Biondi A, Rodriguez‐Galindo C, Pritchard‐Jones K. Early advice on managing children with cancer during the COVID‐19 pandemic and a call for sharing experiences. Pediatr Blood Cancer. 2020;67(7):e28327. doi: 10.1002/pbc.28327 . [DOI] [PubMed] [Google Scholar]
- 132.Hanekamp C, Huang FS. COVID-19 (Coronavirus) [internet]. Cincinnati: Cincinnati Children’s; 2020. Available from: https://www.cincinnatichildrens.org/health/c/covid-19-coronavirus. [Google Scholar]
- 133.Green J, Petty J, Whiting L, Fowler C. Exploring modifiable risk-factors for premature birth in the context of COVID-19 mitigation measures: A discussion paper. J Neonatal Nurs. 2021;27(3):172–9. doi: 10.1016/j.jnn.2020.11.004 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Ahmad MDF, Wahab S, Ahmad AF, Alam IM, Ather H, Siddiqua A, et al. A novel perspective approach to explore pros and cons of face mask in prevention the spread of SARS-CoV-2 and other pathogens. Saudi Pharm J. 2021;29(2):121–33. doi: 10.1016/j.jsps.2020.12.014 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Ingram M-CE, Raval MV, Newton C, Lopez ME, Berman L. Characterization of initial North American pediatric surgical response to the COVID-19 pandemic. J Pediatr Surg. 2020;55(8):1431–5. doi: 10.1016/j.jpedsurg.2020.06.001 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Skarsgard ED, Pediatric Surgical Chiefs of Canada. Prioritizing specialized children’s surgery in Canada during the COVID-19 pandemic. CMAJ. 2020;192(41):E1212–3. doi: 10.1503/cmaj.201577 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Human Milk Banking Association of North America. Milk Handling for COVID-19 Positive or Suspected Mothers in the Hospital Setting [internet]. Fort Worth, TX: Human Milk Banking Association of North America; 2020. Available from: https://www.hmbana.org/news/milk-handling-for-covid-19-positive-or-suspected-mothers-in-the-hospital-setting.html. doi: 10.6061/clinics/2020/e1932 [DOI] [Google Scholar]
- 138.Wang H, Zeng T, Wu X, Sun H. Holistic care for patients with severe coronavirus disease 2019: an expert consensus. Int J Nurs Sci. 2020;7(2):128–34. doi: 10.1016/j.ijnss.2020.03.010 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Ashokka B, Loh MH, Tan CH, Su LL, Young BE, Lye DC, et al. Care of the pregnant woman with coronavirus disease 2019 in labor and delivery: anesthesia, emergency cesarean delivery, differential diagnosis in the acutely ill parturient, care of the newborn, and protection of the healthcare personnel. Am J Obstet Gynecol. 2020;223(1):66–74.e3. doi: 10.1016/j.ajog.2020.04.005 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Aubey J, Zork N, Sheen J-J. Inpatient obstetric management of COVID-19. Semin Perinatol. 2020;44(7):151280. doi: 10.1016/j.semperi.2020.151280 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Boelig RC, Manuck T, Oliver EA, Di Mascio D, Saccone G, Bellussi F, et al. Labor and delivery guidance for COVID-19. Am J Obstet Gynecol MFM. 2020;2(2):100110. doi: 10.1016/j.ajogmf.2020.100110 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Zhang FJ, Hu DY, Liu YL, Li H, Zhu XP, Pan SS. Expert consensus on nurses’ human caring for COVID-19 patients in different sites. Curr Med Sci. 2020;40(4):602–7. doi: 10.1007/s11596-020-2222-0 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Deprest J, Choolani M, Chervenak F, Farmer D, Lagrou K, Lopriore E, et al. Fetal diagnosis and therapy during the COVID-19 pandemic: guidance on behalf of the International Fetal Medicine and Surgery Society. Fetal Diagn Ther. 2020;47:689–98. doi: 10.1159/000508254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Tscherning C, Sizun J, Kuhn P. Promoting attachment between parents and neonates despite the COVID-19 pandemic. Acta Paediatr. 2020;109(10):1937–43. doi: 10.1111/apa.15455 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Castillero AB, Beam KS, Bernardini LB, Ramos EGC, Davenport PE, Duncan AR, et al. COVID-19: neonatal–perinatal perspectives. J Perinatol. 2020;2. doi: 10.1038/s41372-020-00874-x . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Gralton KS, Korom N, Kavanaugh K, Wenner S, Norr K. COVID-19: impact for pediatric research, evidence-based practice and quality processes and projects. J Pediatr Nurs. 2020;55:264–5. doi: 10.1016/j.pedn.2020.08.009 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Salvatore CM, Han JY, Acker KP, Tiwari P, Jin J, Brandler M, et al. Neonatal management and outcomes during the COVID-19 pandemic: an observation cohort study. Lancet Child Adolesc Health. 2020;4(10):721–7. doi: 10.1016/S2352-4642(20)30235-2 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Sharafi SM, Ebrahimpour K, Nafez A. Environmental disinfection against COVID-19 in different areas of health care facilities: a review. Rev Environ Health. 2020. doi: 10.1515/reveh-2020-0075 [DOI] [PubMed] [Google Scholar]
- 149.Bogiatzopoulou A, Mayberry H, Hawcutt DB, Whittaker E, Munro A, Roland D, et al. COVID-19 in children: what did we learn from the first wave?. Paediatr Child Health (Oxford). 2020;30(12):438–43. doi: 10.1016/j.paed.2020.09.005 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Schlaudecker JD. Essential family caregivers in long-term care during the COVID-19 pandemic. J Am Med Dir Assoc. 2020;21(7):983–4. doi: 10.1016/j.jamda.2020.05.027 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Atout M, Tarawneh FS, Al-Kharabsheh A. Challenges faced by mothers caring for children with leukaemia during COVID-19 pandemic: a qualitative study. J Pediatr Nurs. 2021;58:e74–80. doi: 10.1016/j.pedn.2021.01.009 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Choi KR, Records K, Low LK, Alhusen JL, Kenner C, Bloch JR, et al. Promotion of maternal–infant mental health and trauma-informed care during the COVID-19 pandemic. J Obstet Gynecol Neonatal Nurs. 2020;49(5):409–15. doi: 10.1016/j.jogn.2020.07.004 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Hart JL, Turnbull AE, Oppenheim IM, Courtright KR. Family-centered care during the COVID-19 era. J Pain Symptom Manage. 2020;60(2):e93–7. doi: 10.1016/j.jpainsymman.2020.04.017 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Teti SL, Cummings C, King LP, Coleman CC, Tabari K, Mitchell C. Should new mothers with Covid-19 be separated from their newborns? [internet]. New York: The Hastings Center; 2020. Available from: https://www.thehastingscenter.org/why-new-mothers-with-covid-19-should-not-be-separated-from-their-newborns/. [Google Scholar]
- 155.Rathore P, Kumar S, Shweta, Singh N, Krishnapriya V, Thankachan A, et al. A child with acute lymphoblastic leukemia in institutional isolation during the COVID pandemic: a multifaceted responsibility. Indian J Palliat Care. 2020;26(Suppl 1):S170–2. doi: 10.4103/IJPC.IJPC_167_20 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Sankar J, Dhochak NS, Kabra S., Lodha R. COVID-19 in children: clinical approach and management. Indian J Pediatr. 2020;87(6):433–42. doi: 10.1007/s12098-020-03292-1 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Michigan Department of Health & Human Services (MDHHS). COVID-19 guidance for healthcare facilities for discharge of residents. Lansing: MDHHS; 2020. Available from: https://www.michigan.gov/documents/coronavirus/Guidance_for_Health_Care_Facilities_for_Discharge_of_COVID_FINAL_684358_7.pdf. [Google Scholar]
- 158.Dumpa V, Kamity R, Vinci AN, Noyola E, Noor A. Neonatal Coronavirus 2019 (COVID-19) infection: a case report and review of literature. Cureus. 2020;12(5):e8165. doi: 10.7759/cureus.8165 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Jiang L, Tang K, Levin M, Irfan O, Morris SK, Wilson K, et al. COVID-19 and multisystem inflammatory syndrome in children and adolescents. Lancet Infect Dis. 2020;20(11):e276–88. doi: 10.1016/S1473-3099(20)30651-4 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Naranje KM, Gupta G, Singh A, Bajpai S, Verma A, Jaiswal R, et al. Neonatal COVID-19 infection management. Journal of Neonatology. 2020;34(1–2):88–98. 10.1177/0973217920928638. [DOI] [Google Scholar]
- 161.Barney A, Buckelew S, Mesheriakova V, Raymond-Flesch M. The COVID-19 pandemic and rapid implementation of adolescent and young adult telemedicine: challenges and opportunities for innovation. J Adolesc Health. 2020;67(2):164–71. doi: 10.1016/j.jadohealth.2020.05.006 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Campagnaro R, Collet G de O, Andrade MP de, Salles JP da SL, Calvo Fracasso M de L, Scheffel DLS, et al. COVID-19 pandemic and pediatric dentistry: fear, eating habits and parent’s oral health perceptions. Child Youth Serv Rev. 2020;118:105469. doi: 10.1016/j.childyouth.2020.105469 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Chen H, Selix N, Nosek M. Perinatal anxiety and depression during COVID-19. J Nurse Pract. 2021;17(1):26–31. doi: 10.1016/j.nurpra.2020.09.014 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Enyama D, Chelo D, Njinkui DN, Kouam JM, Puepi YFD, Nkwele IM, et al. Impact of the COVID-19 pandemic on pediatricians’ clinical activity in Cameroon. Arch Pediatr. 2020;27(8):423–7. doi: 10.1016/j.arcped.2020.09.004 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Evans Y, Golub S, Sequeira GM, Eisenstein E, North S. Using telemedicine to reach adolescents during the COVID-19 pandemic. J Adolesc Health. 2020;67(4):469–71. doi: 10.1016/j.jadohealth.2020.07.015 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Gerall CD, DeFazio JR, Kahan AM, Fan W, Fallon EM, Middlesworth W, et al. Delayed presentation and sub-optimal outcomes of pediatric patients with acute appendicitis during the COVID-19 pandemic. J Pediatr Surg. 2021;56(5):905–10. doi: 10.1016/j.jpedsurg.2020.10.008 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Sattar S, Kuperman R. Telehealth in pediatric epilepsy care: a rapid transition during the COVID-19 pandemic. Epilepsy Behav. 2020;111:107282. doi: 10.1016/j.yebeh.2020.107282 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Mulay KV, Aishworiya R, Lim TSH, Tan MY, Kiing JSH, Chong SC, et al. Innovations in practice: adaptation of developmental and behavioral pediatric service in a tertiary center in Singapore during the COVID-19 pandemic. Pediatr Neonatol. 2021;62(1):70–9. doi: 10.1016/j.pedneo.2020.09.003 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Houtrow A, Harris D, Molinero A, Levin-Decanini T, Robichaud C. Children with disabilities in the United States and the COVID-19 pandemic. J Pediatr Rehabil Med. 2020;13(3):415–24. doi: 10.3233/PRM-200769 . [DOI] [PubMed] [Google Scholar]
- 170.Johnson SJ, Dupler AE. pediatric surgery nurses lead and coordinate COVID-19 recovery efforts. Paper presented at: 2021 Providence RN Conference; 2021. June. Available from: https://digitalcommons.psjhealth.org/prov_rn_conf_all/18/. [Google Scholar]
- 171.López-Bueno R, López-Sánchez GF, Casajús JA, Calatayud J, Tully MA, Smith L. Potential health-related behaviors for pre-school and school-aged children during COVID-19 lockdown: a narrative review. Prev Med. 2021;143:106349. doi: 10.1016/j.ypmed.2020.106349 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Lopez AS, Hill M, Antezano J, Vilven D, Rutner T, Bogdanow L, et al. Transmission dynamics of COVID-19 outbreaks associated with child care facilities—Salt Lake City, Utah, April-July 2020. MMWR Morb Mortal Wkly Rep. 2020;69(37):1319–23. doi: 10.15585/mmwr.mm6937e3 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Badal S, Bajgain KT, Badal S, Thapa R, Bajgain BB, Santana MJ. Prevalence, clinical characteristics, and outcomes of pediatric COVID-19: a systematic review and meta-analysis. J Clin Virol. 2021;135:104715. doi: 10.1016/j.jcv.2020.104715 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Sarman A, Tuncay S, Sarman E. Diagnosis of Covid-19 in Children and Nursing Approach: A Systematic Review. Acta Medica Alanya. 2021;5(1):98–106. 10.30565/medalanya.843403. [DOI] [Google Scholar]
- 175.Freitas BHBM, Alves MDSM, Gaiva MAM. Prevention and control measures for neonatal COVID-19 infection: a scoping review. Rev Bras Enferm. 2020;73(Suppl 2):e20200467. doi: 10.1590/0034-7167-2020-0467 . [DOI] [PubMed] [Google Scholar]
- 176.Abdollahpour S, Khadivzadeh T. Improving the quality of care in pregnancy and childbirth with coronavirus (COVID-19): a systematic review. J Matern Fetal Neonatal Med. 2020;1–9. doi: 10.1080/14767058.2020.1759540 . [DOI] [PubMed] [Google Scholar]
- 177.Mascarenhas VHA, Caroci-Becker A, Venâncio KCMP, Baraldi NG, Durkin AC, Riesco MLG. Care recommendations for parturient and postpartum women and newborns during the covid-19 pandemic: a scoping review. Rev Lat Am Enfermagem. 2020;28:e3359. doi: 10.1590/1518-8345.4596.3359 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Bolt SR, van der Steen JT, Mujezinović I, Janssen DJA, Schols JMGA, Zwakhalen SMG, et al. Practical nursing recommendations for palliative care for people with dementia living in long-term care facilities during the COVID-19 pandemic: a rapid scoping review. Int J Nurs Stud. 2021;113:103781. doi: 10.1016/j.ijnurstu.2020.103781 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.World Health Organization (WHO). Rational use of personal protective equipment for coronavirus disease 2019 (COVID-19): Interim guidance [Internet]. Geneva: World Health Organization; 2020. Available from: https://apps.who.int/iris/bitstream/handle/10665/331215/WHO-2019-nCov-IPCPPE_use-2020.1-eng.pdf. [Google Scholar]
- 180.World Health Organization (WHO). Postnatal care of the mother and newborn 2013 [Internet]. Geneva: WHO Press; 2014. Available from: http://apps.who.int/iris/bitstream/handle/10665/97603/9789241506649_eng.pdf. [PubMed] [Google Scholar]
- 181.Gozen D, Caka SY, Besirik SA, Perk I. First bathing time of newborn infants after birth: A comparative analysis. J Spec Pediatr Nurs. 2019;24(2):e12239. doi: 10.1111/jspn.12239 . [DOI] [PubMed] [Google Scholar]
- 182.Klaiman T, Silvestri JA, Srinivasan T, Szymanski S, Tran T, Oredeko F, et al. Improving prone positioning for severe acute respiratory distress syndrome during the COVID-19 pandemic. An implementation-mapping approach. Ann Am Thorac Soc. 2021;18(2):300–7. doi: 10.1513/AnnalsATS.202005-571OC . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Gleissman H, Forsgren A, Andersson E, Lindqvist E, Falck AL, Cronhjort M, et al. Prone positioning in mechanically ventilated patients with severe acute respiratory distress syndrome and coronavirus disease 2019. Acta Anaesthesiol Scand. 2020;65(3):360–3. doi: 10.1111/aas.13741 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Shelhamer MC, Wesson PD, Solari IL, Jensen DL, Steele WA, Dimitrov VG, et al. Prone positioning in moderate to severe acute respiratory distress syndrome due to COVID-19: A cohort study and analysis of physiology. J Intensive Care Med. 2021;36(2):241–52. doi: 10.1177/0885066620980399 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Fan E, Beitler JR, Brochard L, Calfee LSC, Ferguson ND, Slutsky AS, et al. COVID-19-associated acute respiratory distress syndrome: is a different approach to management warranted?. Lancet Respir Med. 2020;8(8):816–21. doi: 10.1016/S2213-2600(20)30304-0 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Petrone P, Brathwaite CEM, Joseph DAK. Prone ventilation as treatment of acute respiratory distress syndrome related to COVID-19. Eur J Trauma Emerg Surg. 2021;47(4):1017–22. doi: 10.1007/s00068-020-01542-7 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Breneol S, Hatty A, Bishop A, Curran JA. Nurse-led discharge in pediatric care: a scoping review. J Pediatr Nurs. 2018;41:60–8. doi: 10.1016/j.pedn.2018.01.014 . [DOI] [PubMed] [Google Scholar]
- 188.Loomba RS, Villarreal EG, Farias JS, Bronicki RA, Flores S. Pediatric intensive care unit admissions for COVID-19: insights using state-level data. Int J Pediatr. 2020;2020:9680905. doi: 10.1155/2020/9680905 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Kumar CM, Seet E, Van Zundert TCRV. Measuring endotracheal tube intracuff pressure no room for complacency. J Clin Monit Comput. 2021;35(1):3–10. doi: 10.1007/s10877-020-00501-2 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Bulamba F, Kintu A, Ayupo N, Kojjo C, Ssemogerere L, Wabule A, et al. Achieving the recommended endotracheal tube cuff pressure: a randomized control study comparing loss of resistance syringe to pilot balloon palpation. Anesthesiol Res Pract. 2017;2017:2032748. doi: 10.1155/2017/2032748 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Beccaria LM, Doimo TMA, Polletti NAA, Barbosa TP, da Silva DC, Werneck AL. Tracheal cuff pressure change before and after the performance of nursing care. Rev Bras Enferm. 2017;70(6):1145–50. doi: 10.1590/0034-7167-2016-0486 . [DOI] [PubMed] [Google Scholar]
- 192.Talekar CR, Udy AA, Boots RJ, Lipman J, Cook D. Tracheal cuff pressure monitoring in the ICU: a literature review and survey of current practice in Queensland. Anaesth Intensive Care. 2014;42(6):761–70. doi: 10.1177/0310057X1404200612 . [DOI] [PubMed] [Google Scholar]
- 193.Orsborn J, Graham J, Moss M, Melguizo M, Nick T, Stroud M. Pediatric endotracheal tube cuff pressures during aeromedical transport. Pediatr Emerg Care. 2016. Jan;32(1):20–2. doi: 10.1097/PEC.0000000000000365 . [DOI] [PubMed] [Google Scholar]
- 194.AlQahtani A. Inappropriate Endotracheal Tube (ETT) cuff pressure and its relation to ventilator-associated pneumonia (VAP) in Intensive care unit (ICU). Eur Respir J. 2020;56:2026. 10.1183/13993003.congress-2020.2026. [DOI] [Google Scholar]
- 195.Liu W, Tao ZW, Wang L, Yuan ML, Liu K, Zhou L, et al. Analysis of factors associated with disease outcomes in hospitalized patients with 2019 novel coronavirus disease. Chin Med J (Engl). 2020;133(9):1032–8. doi: 10.1097/CM9.0000000000000775 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Choron RL, Butts CA, Bargoud C, Krumrei NJ, Teichman AL, Schroeder ME, et al. Fever in the ICU: a predictor of mortality in mechanically ventilated COVID-19 patients. J Intensive Care Med. 2021;36(4):484–93. doi: 10.1177/0885066620979622 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Drewry AM, Hotchkiss R, Kulstad E. Response to “Body temperature correlates with mortality in COVID-19 patients.” Crit Care. 2020;24(1):460. doi: 10.1186/s13054-020-03186-w . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Goldschmidt K, Mele C. Disruption of patient and family centered care through the COVID-19 pandemic. J Pediatr Nurs. 2021;58:102–3. doi: 10.1016/j.pedn.2021.03.001 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Phiri PGMC, Chan CWH, Wong CL. The scope of family-centred care practices, and the facilitators and barriers to implementation of family-centred care for hospitalised children and their families in developing countries: an integrative review. J Pediatr Nurs. 2020;55:10–28. doi: 10.1016/j.pedn.2020.05.018 . [DOI] [PubMed] [Google Scholar]
- 200.Voo TC, Senguttuvan M, Tam CC. Family presence for patients and separated relatives during COVID-19: Physical, virtual, and surrogate. J Bioeth Inq. 2020;17(4):767–72. doi: 10.1007/s11673-020-10009-8 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Frampton S, Agrawal S, Guastello S. Guidelines for family presence policies during the COVID-19 pandemic. Jama Health Forum. 2020;1(7):e200807. 10.1001/jamahealthforum.2020.0807. [DOI] [PubMed] [Google Scholar]
- 202.Reardon S. Ebola’s mental-health wounds linger in Africa. Elderly Care. 2015;519(7541):13–4. doi: 10.1038/519013a . [DOI] [PubMed] [Google Scholar]
- 203.Graber KM, Byrne EM, Goodacre EJ, Kirby N, Kulkarni K, O’Farrelly C, et al. A rapid review of the impact of quarantine and restricted environments on children’s play and the role of play in children’s health. Child Care Health Dev. 2021;47(2):143–53. doi: 10.1111/cch.12832 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Moore SA, Faulkner G, Rhodes RE, Brussoni M, Chulak-Bozzer T, Ferguson LJ, et al. Impact of the COVID-19 virus outbreak on movement and play behaviours of Canadian children and youth: a national survey. Int J Behav Nutr Phys Act. 2020;17(1):85. doi: 10.1186/s12966-020-00987-8 . [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.