ABSTRACT
People with diabetes are more likely to require surgical intervention than those without and have an increased risk of developing postoperative complications. The Highs and lows review from the National Confidential Enquiry into Patient Outcome and Death reported on inadequate diabetes care in the perioperative period. As a result, the Centre for Perioperative Care has published guidance on perioperative management of diabetes recently.
Early identification and glucose optimisation pre-operatively is key, and assists in formulating an individualised plan for diabetes care during admission, surgery and postoperatively. The plan will include dose adjustments of diabetes medication, and use of variable rate insulin infusion or continuous subcutaneous insulin infusion where applicable. The guideline also highlights the importance of improved communication between healthcare teams involved in the perioperative pathway in order to improve outcomes and care.
KEYWORDS: diabetes, surgery, perioperative care
Introduction
Around 3.9 million people in the UK live with diabetes mellitus.1 Ninety per cent of these have type 2 diabetes (T2D), 8% have type 1 diabetes (T1D), with uncommon forms making up the remainder. Diabetes-related complications are associated with significant morbidity, mortality and healthcare costs.
The National Diabetes Inpatient Audit (NaDIA) found that around 18% of hospital beds are occupied by a person with diabetes.2 People with diabetes are more likely to require surgical intervention compared with those without diabetes, and are also more likely to develop perioperative complications (such as infection, poor wound healing or cardiovascular events).3
New guidance on perioperative management of patients with diabetes has recently been published by the Centre for Perioperative Care (CPOC).4 While of most relevance to surgeons, anaesthetists and diabetes clinicians, this guidance may also be of relevance to junior doctors dealing with queries for such patients while on call.
In this commentary, we discuss the salient points highlighted in this document.
Why is this guidance needed?
It is recognised that diabetes as a comorbidity in a surgical patient increases risk of adverse outcomes.5 One study found the incidence of postoperative adverse events in those with diabetes was 7.7%, and a rise in plasma glucose postoperatively of 1 mmol/L increased adverse events by 1.31-fold.5 The physiological stress of surgery, plus anaesthetic agents, can further raise plasma glucose levels and increase insulin resistance.6 If untreated, these may progress to diabetes emergencies, such as diabetic ketoacidosis (DKA) or hyperosmolar hyperglycaemic state (HHS). Conversely, hypoglycaemia is associated with an increased length of stay and inpatient mortality.7
The NaDIA audit found that only 43% of patients had capillary blood glucose (CBG) levels recorded at the recommended stages of the perioperative pathway; even less in those undergoing emergency surgery.2 However, approximately two-thirds of hospitals surveyed had a referral pathway to ensure elective patients underwent pre-admission optimisation of diabetes control.
The National Confidential Enquiry into Patient Outcome and Death (NCEPOD) has also looked at the perioperative management of diabetes, and published a report, Highs and lows.8 This highlighted a number of deficiencies in diabetes care in the perioperative period, in particular, around poor communication between specialties. Furthermore, the report suggested there was inadequate CBG monitoring intra- and postoperatively, and a lack of planning around diabetes management prior, during and after surgery.
As a result of these findings, a national joint standard and policy for the multidisciplinary management of patients with diabetes who require surgery was developed: the Guideline for perioperative care for people with diabetes mellitus undergoing elective and emergency surgery, published in 2021.4
What does the CPOC guidance recommend?
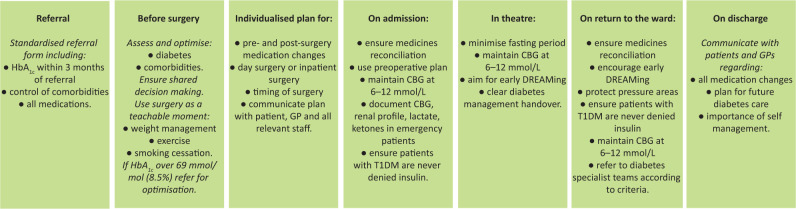
The CPOC recommendations are summarised in Fig 1.4
Fig 1.
The perioperative pathway for people with diabetes undergoing elective and emergency surgery.4 CBG = capillary blood glucose; DREAMing = drinking, eating and mobilising; GP = general practitioner; HbA1c = glycated haemoglobin; shared decision making = the process whereby patients and clinicians work together to make evidence-based decisions centred on patient values and preferences, including risks, benefits, alternatives and optimisation; T1DM = type 1 diabetes mellitus.
Referral and assessment prior to surgery
Referrals for surgery on all patients with diabetes should contain the following information:
type of diabetes
last diabetes review, presence of comorbidities and complications
glycated haemoglobin (HbA1c) within 3 months prior to referral
list of all current medications and medical devices used.
The Perioperative Quality Improvement Programme found that 69% of patients with diabetes had a HbA1c recorded prior to surgery, and 20% of these patients had HbA1c greater than the recommended upper threshold.9 There is, however, no randomised controlled trial evidence to ascertain the optimum level of glucose control prior to surgery. Therefore, the CPOC guidance has suggested a pragmatic level of HbA1c <69 mmol/mol (8.5%) before undertaking surgery should be achieved, where clinically safe and possible.
The guidance recommends that all trusts that provide surgical services have a clear perioperative pathway and referral process to support people with diabetes. The guidance suggests that this will require:
electronic administration systems enabling rapid identification of patients with diabetes
a named clinical lead for oversight and implementation for perioperative diabetes care
specific teams to coordinate individualised perioperative care for people with diabetes.
Clear communication and referral pathways between primary care, surgical, anaesthetic and diabetes teams are highlighted as paramount to ensure pre-operative optimisation.
Individualised plan for admission and surgery
CPOC recommends that, prior to surgery, a care plan should be established in conjunction with the patient and clinical teams involved in their care. This care plan should be easily accessible and referred to during the perioperative period. The following factors should be taken into consideration and addressed:
type of diabetes
glucose lowering medications
HbA1c as indicator of diabetes control
urgency of procedure
degree of metabolic derangement at presentation (if emergency)
anticipated period of total fasting (one missed meal versus greater than one).
Day surgery versus inpatient admission
The option of day surgery for specific procedures should be considered in those with diabetes using the same principles as those without. It is recognised that people with diabetes are often better at managing their own diabetes and admitting them to hospital may disrupt their routine and glycaemic control.10 Scheduling of surgery should aim to minimise the period of fasting for patients with diabetes.
Intra-operatively, the guideline recommends:
glucose levels should be maintained between 6–12 mmol/L
CBG should be checked at induction and at least hourly if on insulin or insulin secretagogues, otherwise a minimum of 2 hourly
immediate access to glucose meter, ketone meter and hypoglycaemia management.
Medication adjustment
The guideline provides advice on adjustment to diabetes treatments on the day prior to and of surgery, depending on whether planned for morning or afternoon. This reference is for guidance only, and up-to-date information can be found in the UK Clinical Pharmacy Association’s The Handbook of Perioperative Medicines.11
Long-acting or premixed insulin can usually be continued the day before and day of surgery but with a dose reduction (usually between 50%–80% depending on the type of insulin used). This should reduce the need for the use of variable rate insulin infusion (VRII).
A newer class of agent now widely used in glucose management are sodium-glucose transport-2 inhibitors (SLGT-2i) or ‘gliflozins’, which block the SGLT-2 transporter, preventing renal glucose reabsorption, thereby lowering blood glucose. They have significant cardio-renal protective effects.12 A rare but potentially serious and life-threatening association between SGLT-2i and euglycaemic DKA has been recognised, the risk of which is increased when there is a restriction to food or fluid intake (such as fasting for surgical procedures).13 SLGT-2i should, therefore, be withheld in any patient who has been hospitalised for major surgery or acute serious illness. Ketones levels should be monitored daily, even if asymptomatic with normal blood glucose levels, and the drugs should only be restarted once the clinical condition has stabilised and normal oral intake is established.
Variable rate insulin infusion
Many people with diabetes undergoing elective surgery may have been admitted the night before surgery and started on a VRII (also known as a sliding scale). While VRII can maintain tight glucose control, it brings potential risks, including hyper- and hypoglycaemia from incorrect infusion rates or inadequate monitoring, rebound hyperglycaemia and possible ketoacidosis if infusion is stopped inappropriately, fluid overload and electrolyte disturbances.14 NaDIA data suggests that 6.5% of all inpatients are treated with VRII unnecessarily.15
With thorough optimisation and individualised planning, it is possible to avoid the use of VRII while still maintaining good glycaemic control. The use of VRII, however, may be preferrable in the following circumstances:
patients with T1D or T2D undergoing surgery with a fasting period of >1 meal
patients with T1D undergoing surgery who have not received background/basal insulin
suboptimal diabetes control (HbA1c >69 mmol/mol)
requiring emergency surgery
persistent hyperglycaemia in the perioperative period in the context of acute decompensation.
The CPOC guideline covers the practicalities of VRII use, including adjustment if there are risk factors for hypoglycaemia (such as chronic kidney disease, low body weight or low total daily insulin).
Continuous subcutaneous insulin infusions
Continuous subcutaneous insulin infusions (CSII), also known as insulin pump therapy, delivers fast acting insulin subcutaneously continuously from a refillable storage reservoir with boluses delivered by the patient at mealtimes. Around 15% of patients with T1D manage their diabetes with CSII, and their use is growing.
As patients on CSII therapy do not take long-acting insulin, if there is a disruption to delivery of their insulin, metabolic decompensation can rapidly occur. If a patient is unable to manage their pump independently, an alternative administration of insulin should be used and CSII removed.16 Insulin pumps are not licensed to be used near diathermy or imaging devices, and manufacturers advise patients are switched to a VRII or subcutaneous insulin regimens during most surgical procedures. Patients, however, may wish to continue using CSII in the perioperative period and it could avoid unnecessary use of VRII and associated problems. Lack of familiarity of many non-specialists, however, means that use of CSII perioperatively may be risky, unless carefully supervised by the diabetes team.
Return to ward and discharge planning
Communication from the theatre team to ward team post-surgery can be an area of risk, and handover should include medications given in theatre, CBG level on leaving the recovery area and the plan for ward-based management of diabetes.
Postoperatively, blood glucose should continue to remain in the target range of 6–12 mmol/L. The aim is to restore usual diet and normal diabetes medication as soon as is clinically safe to do so. This can be achieved through early ‘DREAMing’ (DRinking, EAting and Mobilising), which is the cornerstone of postoperative care.17 Appropriate use of anti-emetics and analgesia, avoidance of intravenous fluids if able to meet needs orally or enterally, and promotion of mobilisation are crucial.
Patients should be encouraged to self-manage their diabetes and be involved in decisions regarding their diabetes care. If discharge delays are diabetes related, then involvement of the diabetes specialist team should be sought. Timely communication with all services on discharge, especially in primary care, is vital. This is particularly important if changes have been made to diabetes management or there have been concerns regarding diabetes management during the admission.
Conclusion
People living with diabetes have an increased risk of perioperative complications. The recently published CPOC guideline outlines key recommendations for the perioperative period in such patients. Communication between specialist teams and the patient alongside pre-operative diabetic care planning and optimisation forms much of the focus. It also includes practical resources around medication adjustment, VRII, management of hypo- and hyperglycaemia, and use of CSII during the perioperative period. Junior doctors and doctors from other specialties may be called upon to offer advice on such patients while on call, and a working knowledge of these guidelines, or at least how and where to access them, is worth knowing.
Implementation of the guidance is likely to improve outcomes for people with diabetes undergoing surgical intervention, which is likely to reduce mortality, morbidity, length of stay and cost to the NHS.
Key points
People with diabetes are more likely to require surgical interventions and are at increased risk of complications, such as infection, cardiovascular events and poor wound healing.
Primary care referrals should cover all aspects of a patient’s diabetes care and a HbA1c <69 mmol/mol (8.5%) should be achieved pre-operatively where possible. Patients should have an individualised plan for admission, surgery and postoperative care. Day surgery for specific procedures should be considered equally in those with diabetes as in those without.
Most oral and injectable diabetic medications (including insulin) can be continued the day before and day of surgery with dose adjustments. SGLT-2i should be stopped prior to surgery.
CSII (insulin pumps) can be continued in the perioperative period if a patient’s wishes with careful monitoring and involvement of the specialist diabetes team.
Postoperatively, aiming for early eating and drinking should enable patients to promptly restore their usual diabetes regimen.
Clear communication and documentation between the patient and the specialist teams is required throughout the perioperative pathway.
References
- 1.Diabetes UK . Diabetes Prevalence 2019. Diabetes UK, 2019. www.diabetes.org.uk/professionals/position-statements-reports/statistics/diabetes-prevalence-2019 [Accessed 03 May 2021]. [Google Scholar]
- 2.NHS Digital . National Diabetes Inpatient Audit (NaDIA) –2019. NHS, 2020. https://digital.nhs.uk/data-and-information/publications/statistical/national-diabetes-inpatient-audit/2019 [Accessed 03 May 2021]. [Google Scholar]
- 3.Dagogo-Jack S, George MM, Alberti K. Management of diabetes mellitus in surgical patients. Diabetes Spectrum 2002;15:44–8. [Google Scholar]
- 4.Centre for Perioperative Care . Guideline for perioperative care for people with diabetes mellitus undergoing elective and emergency surgery. CPOC, 2021. https://cpoc.org.uk/sites/cpoc/files/documents/2021-03/CPOC-Diabetes-Guideline2021_0.pdf [Accessed 03 May 2021]. [Google Scholar]
- 5.Want J, Chen K, Li X, et al. Postoperative adverse events in patients with diabetes undergoing orthopedic and general surgery. Medicine (Baltimore) 2019;98:e15089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Akiboye F, Rayman G. Management of Hyperglycaemia and Diabetes in Orthopedic Surgery. Current Diabetes Reports 2017;17:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nirantharakumar K, Marshall T, Kennedy A, et al. Hypoglycaemia is associated with increased length of say and mortality in people with diabetes who are hospitalized. Diabetic Medicine 2012;29:e445–8. [DOI] [PubMed] [Google Scholar]
- 8.The National Confidential Enquiry into Patient Outcome and Death . Highs and lows. NCEPOD, 2018. www.ncepod.org.uk/2018pd/Highs%20and%20Lows_Full%20Report.pdf [Accessed 03 May 2021]. [Google Scholar]
- 9.Perioperative Quality Improvement Programme . Annual report 2017-18. The Royal College of Anaesthetists, 2018. https://rcoa.ac.uk/sites/default/files/documents/2019-09/PQIP%20Annual%20Report%202017-18.pdf [Accessed 03 May 2021]. [Google Scholar]
- 10.Getting it Right First Time . National Day Surgery Delivery Pack. GIRFT, 2020. www.gettingitrightfirsttime.co.uk/wp-content/uploads/2020/10/National-Day-Surgery-Delivery-Pack_Sept2020_final.pdf [Accessed 03 May 2021]. [Google Scholar]
- 11.UK Clinical Pharmacy Association . The Handbook of Perioperative Medicines. UKCPA, 2021. www.ukcpa-periophandbook.co.uk [Accessed 03 May 2021]. [Google Scholar]
- 12.Lo KB, Gul F, Ram P, et al. The effects of SGLT2 inhibitors on cardiovascular and renal outcomes in diabetic patients: a systematic review and meta-analysis. Cardiorenal Med 2020;10:1–10. [DOI] [PubMed] [Google Scholar]
- 13.Medicines and Healthcare products Regulatory Agency . SGLT2 inhibitors: updated advice on the risk of diabetic ketoacidosis. MHRA, 2016. www.gov.uk/drug-safety-update/sglt2-inhibitors-updated-advice-on-the-risk-of-diabetic-ketoacidosis [Accessed 03 May 2021]. [Google Scholar]
- 14.Joint British Diabetes Societies for Inpatient Care . The use of variable rate intravenous insulin infusion (VRII) for medical inpatients. JBDS-IP, 2014. www.diabetes.org.uk/resources-s3/2017-09/Use%20of%20variable%20rate%20intravenous%20insulin%20infusion%20in%20medical%20inpatients_0.pdf [Accessed 03 May 2021]. [Google Scholar]
- 15.NHS Digital . National Diabetes Inpatient Audit (NaDIA) –2012. NHS, 2013. https://files.digital.nhs.uk/publicationimport/pub10xxx/pub10506/nati-diab-inp-audi-12-nat-rep.pdf [Accessed 03 May 2021]. [Google Scholar]
- 16.Association of British Clinical Diabetologists Diabetes Technology Network UK . Guidelines for managing continuous subcutaneous insulin infusion (CSII, or ‘insulin pump’) therapy in hospitalised patients. ABCD, 2018. https://abcd.care/sites/abcd.care/files/CSII_DTN_FINAL%20210218.pdf [Accessed 03 May 2021]. [Google Scholar]
- 17.Levy N, Mills P, Mythen M. Is the pursuit of DREAMing (drinking, eating and mobilising) the ultimate goal of anaesthesia? Anaesthesia 2016;71:1008–12. [DOI] [PubMed] [Google Scholar]