Abstract
Objective:
To determine the effect of orthognathic surgery on pharyngeal airway in Class III patients and to (1) compare the results of different surgical techniques, (2) determine the change at the position of the hyoid bone, and (3) evaluate the craniocervical posture changes related to pharyngeal airway change.
Materials and Methods:
Forty-eight Class III adult patients were included in the study to assess airway space after orthognathic surgery. Nine patients were treated with maxillary advancement, seven patients were treated with mandibular set back, and 32 patients were treated with bimaxillary surgery. Cephalometric records were taken before treatment, after surgery, and about 1 year after surgery (at the end of the treatment).
Results:
No differences were determined at the position of hyoid bone and craniocervical posture. Nasopharyngeal area was significantly increased in all groups (P < .05). Oropharyngeal area and SPSS and IPS parameters were significantly decreased after mandibular set back operation (P < .05). In bimaxillary and maxillary advancement groups, PPS parameter was significantly increased (P < .01), and IPS parameter was significantly decreased (P < .05). No differences were detected at oropharyngeal and hypopharyngeal areas in bimaxillary and maxillary advancement groups.
Conclusion:
Different surgical procedures have different effects on pharyngeal airway space.
Keywords: Orthognathic surgery, Class III, Pharyngeal airway
INTRODUCTION
Class III skeletal deformity can be the result of mandibular prognathism and/or maxillary deficiency.1 In the past years only mandibular set back operations were used for the correction of skeletal Class III deformity; however, with the advancement in techniques and knowledge, bimaxillary surgical procedures are frequently used now for the surgical correction of this deformity.2 Currently, bimaxillary surgery is preferred in 40% of Class III patients, while mandibular set back is preferred in 10%, and maxillary advancement in 50%.3
Since soft palate, tongue and hyoid bone, and associated tissues are attached directly or indirectly to the maxilla and mandible, movement of the jaws affects those tissues, causing alterations in the pharyngeal area. Mandibular set back surgery can reduce the volume of the pharyngeal airway4–16 and change the position of the hyoid bone and tongue.8–10,13,14,17–21 The narrowing of the pharyngeal airway can cause obstructive sleep apnea (OSA) syndrome.22 After mandibular set back operations, head posture can also change to sustain normal breathing.4,23,24 On the contrary, maxillary advancement operations can be used mainly together with mandibular advancement operations for the treatment of OSA syndrome because of the positive effect on breathing.25,26
Several studies have attempted to investigate the effect of orthognathic surgery on posterior airway space in Class III patients. Most of these studies included mandibular set back operations. Although in recent years bimaxillary operations were also mentioned, there are few studies comparing mandibular set back, maxillary advancement, and bimaxillary surgery groups in Class III patients.11,19,27
Hyoid bone, cervical posture, and the pharyngeal area are dependent factors which mainly affect breathing. Our study is the first study evaluating all those factors in three surgical groups for Class III orthognathic surgery patients. It may be hypothesized that when maxillary hard and soft tissues go forward, a relaxation occurs in the oropharyngeal and nasopharyngeal regions, thus reducing the adverse effect of mandibular set back operations on breathing.
The aim of our study was the assessment of pharyngeal airway change after maxillary advancement (MA), mandibular set back (MS), and bimaxillary (BM) operations and comparing the results for each surgical procedure; our study also included post operative evaluation of hyoid bone and change in head posture.
MATERIALS AND METHODS
The patients were selected among those treated in the University of Ankara, Faculty of Dentistry, Department of Orthodontics and Maxillofacial Surgery. Inclusion criteria were adult patients with skeletal and dental Class III deformity, surgical treatment consisting of mandibular set back and/or maxillary advancement, and lateral cephalograms of good quality. Exclusion criteria included previous orthognathic surgery, genioplasty, OSA, cleft, and craniofacial anomalies. Ethical committee approval from Ankara University Faculty of Dentistry and patient consent from each patient were received for this study.
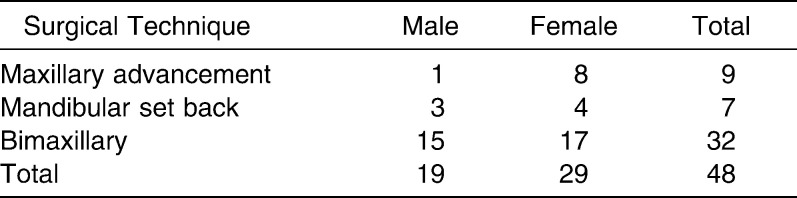
Twenty of the patient radiographs were obtained from the university archive. Twenty-eight of the patients were treated orthodontically (Dr Memikoğlu) and surgically (Dr Karasu) with the same doctor and treatment protocol. Nine of the patients were treated with MA, seven of the patients were treated with MS, and 32 of the patients were treated with the BM surgical procedure. The distribution of patients with respect to surgical technique and gender is shown in Table 1. Bilateral sagittal split ramus osteotomy with semi-rigid fixation and/or Le Fort I osteotomy with rigid fixation were used for the mandible and maxilla. In the Le Fort I surgical technique, the maxilla was positioned upwards when needed.
Table 1.
The Distribution of Patients With Respect to Surgical Technique and Gender
Cephalometric Analysis
The lateral cephalometric radiographs were taken by the same operator on the same machine before treatment (T1), before surgery (T2), and at the end of the fixed treatment (T3). Cephalograms were obtained under standardized conditions in natural head position with the mandible in centric relation; patients were informed not to swallow during radiography.
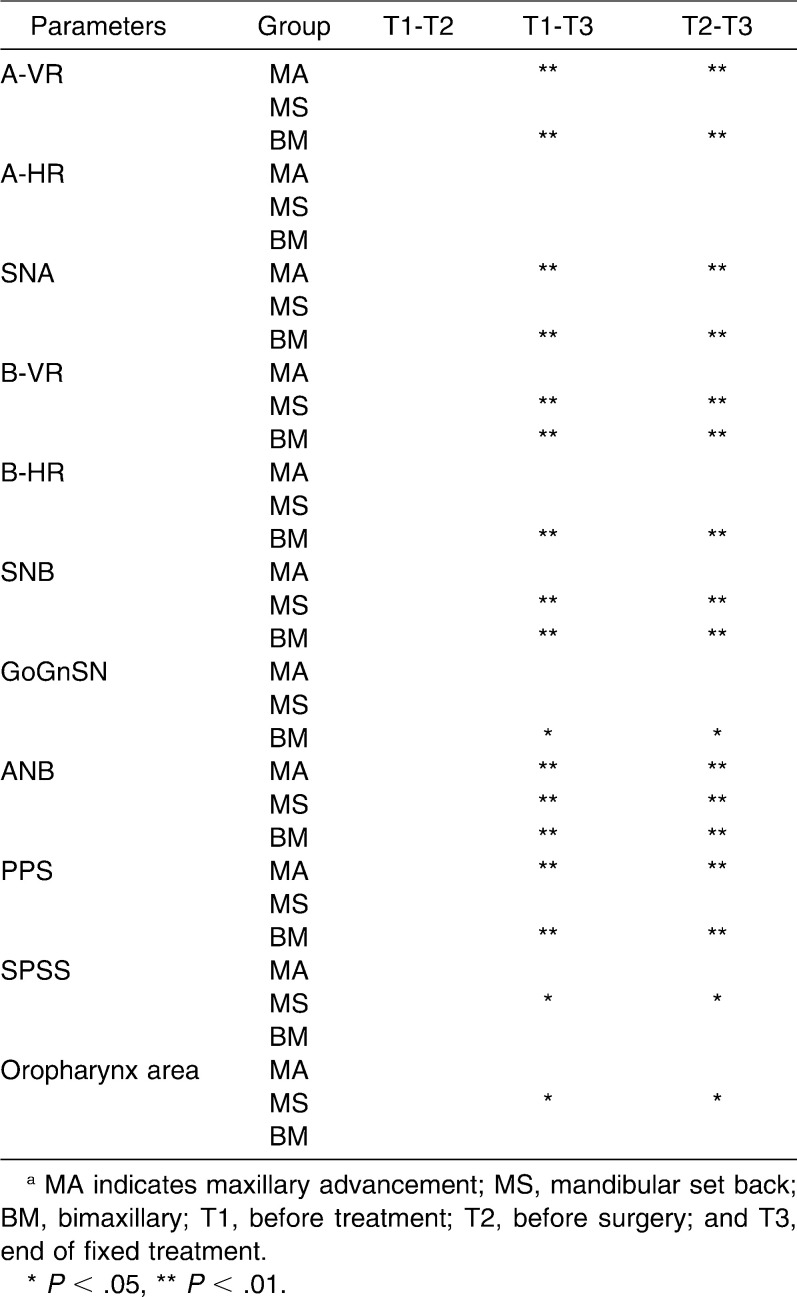
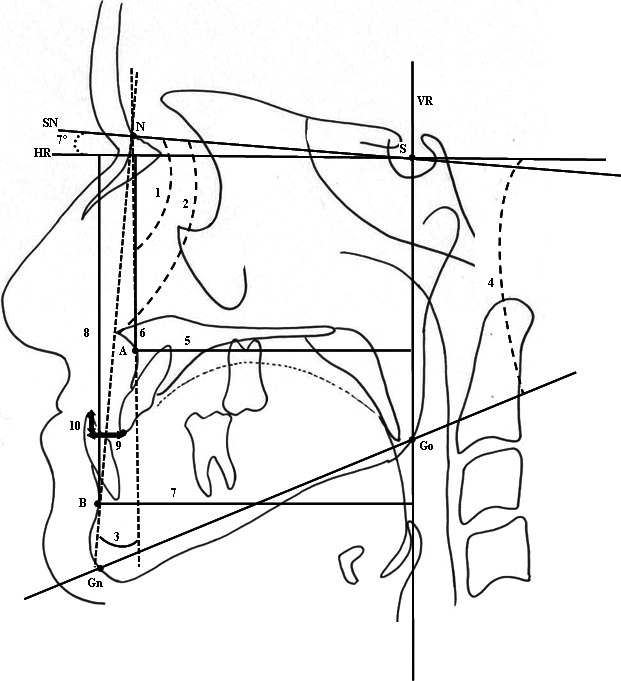
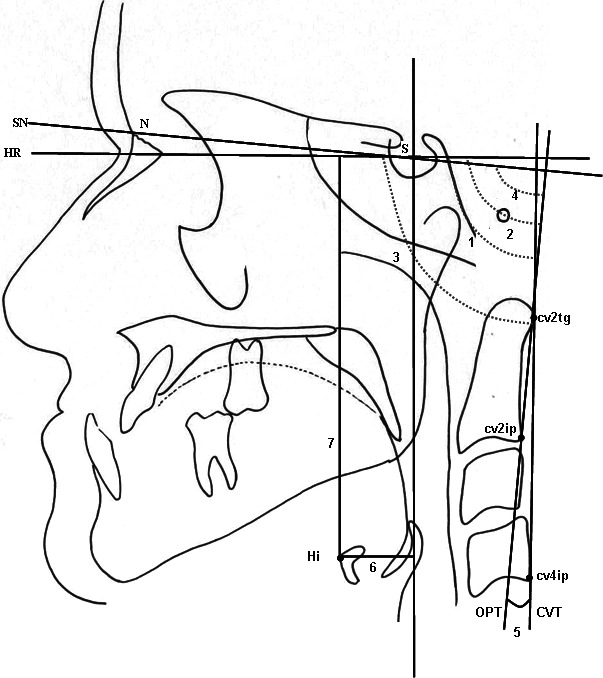
Lateral cephalograms were traced and cephalometric reference points were determined by using acetate paper. Seven degrees to the sella nasion plane through sella point was taken as the horizontal reference plane (HR) and perpendicular to HR through S point was taken as the vertical reference plane (VR) (Figure 1). These reference planes were used as the guides in measuring the projected distances of the reference landmarks (Figure 1). Ten skeletal and dental (Figure 1), seven craniocervical and hyoidal (Figure 2), seven pharyngeal linear (Figure 3), and three pharyngeal area (Figure 4) measurements were used in the study. Linear and angular measurements were done with the help of PorDios program. Area measurements of the pharyngeal airway were done with digital planimeter (Ushikata X-Plan380Dııı/460Dııı, Tokyo, Japan) (Figure 5 a,b). The pharyngeal airway measurements were chosen similar to the investigations done previously.28,29
Figure 1.
Skeletal measurements. (1) SNA. (2) SNB. (3) ANB. (4) GoGnSN. (5) A-VR. (6) A-HR. (7) B-VR. (8) B-HR. Dental measurements. (9) Overjet. (10) Overbite.
Figure 2.
Craniocervical and hyoidal measurements. (1) SN.OPT. (2) SN.CVT. (3) OPT.HR. (4) CVT.HR. (5) OPT.CVT. (6) Hi-VR. (7) Hi-HR.
Figure 3.
Pharyngeal linear measurements. (1) PNS-R: on the line passing from PNS and R. (2) PPS: palatal pharyngeal distance: on the line passing from PNS, parallel to FHP. (3) SPSS, superior posterior pharyngeal distance: on the line passing from the midpoint of the soft palate, parallel to FHP. (4) MPS, middle pharyngeal distance: on the line passing from P, parallel to FHP. (5) Go-P, gonial pharyngeal distance: on the line passing from Go, parallel to FHP. (6) IPS, inferior pharyngeal distance: on the line passing from cv2a, parallel to FHP. (7) EPS, epiglottic pharyngeal distance: on the line passing from E, parallel to FHP.
Figure 4.
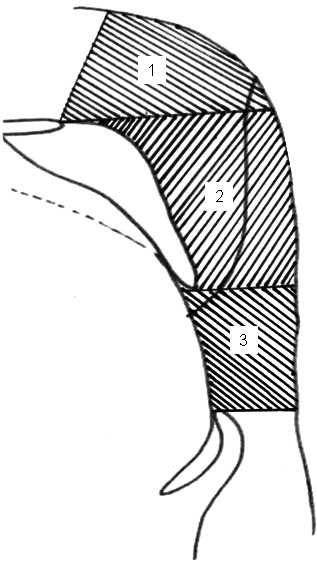
Pharyngeal area measurements. (1) Nasopharynx. (2) Oropharynx. (3) Hypopharynx.
Figure 5.
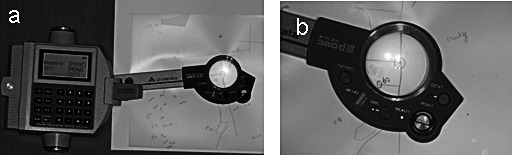
(a) Digital planimeter. (b) Measurement of the areas using a digital planimeter.
Statistical Analysis
The statistical analysis of the study was performed by using repeated-measures analysis of variance and Bonferroni test. Repeated-measures analysis of variance was used to compare intragroup and intergroup cephalometric and planimetric measurements at each time interval. The Bonferroni test was used when interaction was observed.
Error Study
All digitizing points and measurements were repeated on 35 randomly selected radiographs. Measurements were compared and correlation coefficients (r2) were obtained. Cephalometric landmarks of the radiographs were digitized twice, area measurements were repeated three times by the same investigator, and the average values of three measurements were calculated to eliminate errors in measurements.
RESULTS
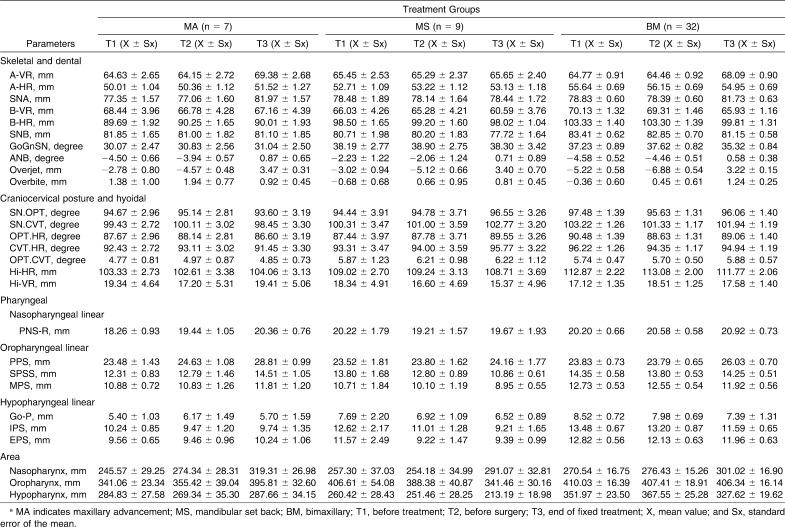
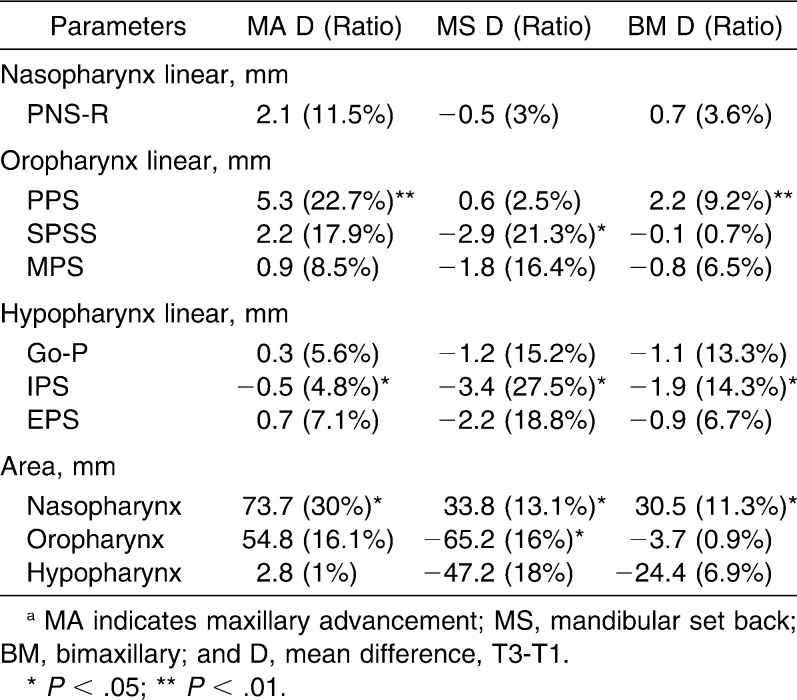
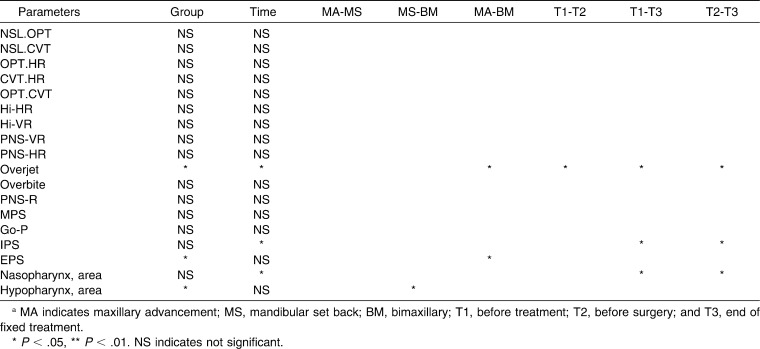
The reliability of the method was high, with the correlation coefficients ranging between 0.9916 and 0.9985. The mean values and standard error of the means of the variables at each time interval for three surgery groups are presented in Table 2. The mean amounts of maxillary advancement in the MA and BM groups were 4.75 and 3.32 mm, respectively. The mean backward movements of the mandible were 5.44 and 4.20 mm in the MS and BM groups, respectively. In Table 3, the change in the pharyngeal airway after surgery and the ratios of the changes are presented. Table 4 shows the comparison of the changes among three surgery groups and time intervals (Bonferroni and repeated-measures analysis of variance). No significant differences were identified in craniocervical angulation; hyoid bone positions; overbite; and PNS-R, MPS, and Go-P parameters between time intervals and groups. The amount of change for EPS differed significantly between the MA and BM groups, whereas the amount of change for the hypopharynx differed significantly between MS and BM groups. IPS significantly decreased and nasopharynx significantly increased in all groups after surgery.
Table 2.
The Mean Values and Standard Error of the Means of the Variables at Each Time Interval for Three Surgery Groupsa
Table 3.
The Differences Between T3 and T1 Periods and the Ratios of the Differences for Three Surgery Groupsa
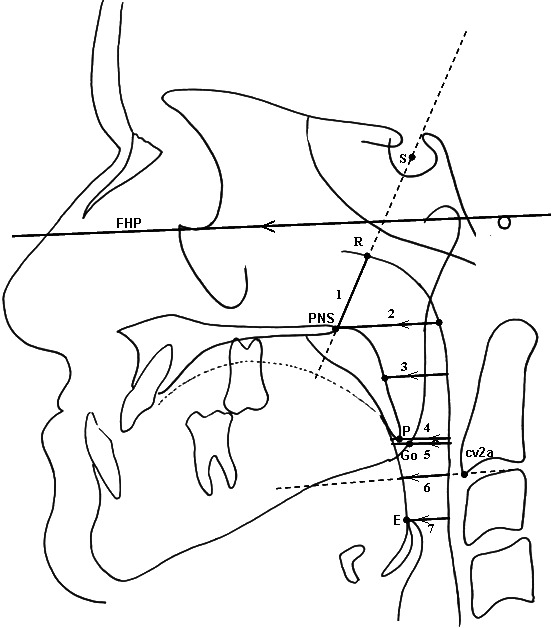
Table 4.
Comparison of the Changes Among Three Surgery Groups and Time Intervalsa
Parameters showing interaction are evaluated on Table 5. A-VR and SNA increased significantly in both the MA and BM groups postoperatively. B-VR and SNB decreased significantly in the MS and BM groups. ANB increased significantly in all groups. B-HR and GoGnSN decreased significantly in the BM group. When the pharyngeal airway measurements were evaluated, PPS increased significantly in the MA and BM groups. SPSS and oropharynx significantly decreased postoperatively in the MS group.
Table 5.
Parameters Showing Interactiona
DISCUSSION
The relatively small sample size of the MS and MA groups is a result of the extent of BM operations in our clinic. Improvements in skeletal and soft tissue variables were achieved after surgery in all patients included in the study.
Lateral cephalograms and computed tomography have been used to assess the pharyngeal airway space in patients after orthognathic surgery.4,15 According to Riley and Powell,30 pharyngeal airway space measured by cephalograms was highly correlated with measurements using a three-dimensional computed tomography scan with considerably high accuracy in predictability.
Most of the operations evaluating the pharyngeal airway include mandibular set back surgeries. There are few studies suggesting bimaxillary surgery can prevent narrowing of the upper airway in the correction of Class III deformities in comparison with mandibular set back surgery.2,19,30 The effect on the pharyngeal airway after surgery including maxillary advancement procedures is not known exactly. It is essential to compare the results of different surgical procedures under the same standard conditions and evaluate the effects on the pharyngeal airway separately and comparatively. This is the only study evaluating the effect of orthognathic surgery on the pharyngeal airway, hyoid bone, and craniocervical posture in MS, MA, and BM patients.
There are few studies comparing three surgical Class III groups in the same study.11,19,26 Samman et al.19 found a significant increase in the nasopharynx in the MA group after 6 months, and Pereira-Filho et al.26 found a significant increase in the nasopharynx and oropharynx after MA and BM operations. In our study, it was not significant, but there was an 11.5% increase in the PNS-R level (nasopharynx), and there was a significant increase in PPS (oropharynx) in the MA group. According to Riley et al.31 and Nimkarn et al.,32 the effect of MA operations on the nasopharynx is significant when the maxilla is protruded at least 10 mm.
In our study, there was a significant increase in the nasopharyngeal area in all groups after surgery. The maximum increase was seen in the MA group (30%). When the maxilla and mandible are protruded, widening occurs in the velopharyngeal airway with the elevation of the tissues attached to the maxilla, mandible, and hyoid bone.33 There has been no investigation evaluating the nasopharyngeal area in MS patients. The increase in the nasopharyngeal area in the MS group was an expected result based on the previous experience. In our opinion, the increase can be due to a compensation mechanism after oropharyngeal and hypopharyngeal airway collapse in MS surgery patients. The area and linear parameters in the nasopharynx did not support each other. Therefore, the area measurement is vital in the evaluation of the pharyngeal airway.
In the MA group, the oropharyngeal area increase was 16.1%. The positive effect of MA on airway was seen mostly on the nasopharynx (30.0%) then oropharynx (16.1%) and at least hypopharynx (2.83%) because of anatomic relationship. In the study of Greco et al.,5 there was a 16% of increase in oropharynx after MA operations.
Studies carried out up to now have frequently emphasized the narrowing effect of mandibular set back procedures on the oropharyngeal and hypopharyngeal airway.4–16 Pereira-Filho et al.26 found no significant decrease in the MS group for the oropharynx and hypopharynx. In our study, the most distinctive decreases in the pharyngeal area for all parameters were seen in the MS group. According to the ratios in Table 3, in the MS group, the oropharynx and hypopharynx were affected similarly after surgery, whereas in the BM surgery group, the hypopharynx was affected much more adversely than the oropharynx. BM operations reduce the negative effect of mandibular set back on the oropharynx with the advancement of the maxilla.2,30
The tongue has positional changes after orthognathic surgery that affect the pharyngeal airway.20 Tongue position is usually determined with hyoid bone position. In our study, all groups showed significant change. But the maximum positional change was seen in the MS group with 2.97 mm of posterior movement (16%). According to the literature, after MS surgery hyoid bone moves inferior,8,17,19,24 both inferior and posterior,9,13,14,20,21 and both inferior and forward.10 According to some studies, hyoid bone returns to its original position for maintaining the airway resistance.6,8,10,13–15,20,21 In our study hyoid bone and the tongue moved posteriorly after MS operation.
According to Bibby and Preston36 and Bibby,35 the hyoid triangle is maintained regardless of cranial posture, and the position of the hyoid bone was independent of cranial posture. Therefore, a change in hyoid bone position can only indicate the effects of posterior movement of the mandible, not a change in cranial posture. Therefore, we evaluated craniocervical posture together with hyoid bone position.
In order to maintain sufficient airway, postural head changes can be observed.36–38 According to Muto et al.23 and Winnberg et al.,39 there is a correlation in pharyngeal airway and cervical vertebra inclination. In our study, despite the decrease of the pharyngeal airway in the MS group there was no significant change seen in craniocervical posture. However, in the MS group there was a tendency to cervical flexion that was not observed in the MA and BM groups.
CONCLUSIONS
Among Class III orthognathic operations, mandibular set back operations cause the most narrowing effect on the pharyngeal airway.
Bimaxillary operations mostly decrease the narrowing effect of the MS operations and must be preferred when planning these operations.
Maxillary advancement operations have a widening effect on the pharyngeal airway.
No significant change occurs in craniocervical posture and hyoid bone position after Class III orthognathic operations.
REFERENCES
- 1.Obwegeser H. L. Surgical correction of small or retrodisplaced maxillae. The ‘dish face’ deformity. Plast Reconstr Surg. 1969;43:351–365. doi: 10.1097/00006534-196904000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Chen F, Terada K, Hua Y, Saito I. Effects of bimaxillary surgery and mandibular set back surgery on pharyngeal airway measurements in patients with Class III skeletal deformities. Am J Orthod Dentofacial Orthop. 2007;131:372–377. doi: 10.1016/j.ajodo.2005.06.028. [DOI] [PubMed] [Google Scholar]
- 3.Busby B. R, Bailey L. J, Proffit W. R, Phillips C, White R. P., Jr Long-term stability of surgical Class III treatment: a study of 5-year post-surgical results. Int J Adult Orthodon Orthognath Surg. 2002;17:159–170. [PubMed] [Google Scholar]
- 4.Wenzel A, Williams S, Ritzau M. Changes in head posture and nasopharyngeal airway following surgical correction of mandibular prognathism. Eur J Orthod. 1989;11:37–42. doi: 10.1093/oxfordjournals.ejo.a035962. [DOI] [PubMed] [Google Scholar]
- 5.Greco J. M, Frohberg U, Van Sickels J. E. Cephalometric analysis of long-term airway space changes with maxillary osteotomies. Oral Surg Oral Med Oral Pathol. 1990;70:552–554. doi: 10.1016/0030-4220(90)90394-8. [DOI] [PubMed] [Google Scholar]
- 6.Enacar A, Aksoy AÜ, Şençift Y, Haydar B, Aras K. Changes in hypopharyngeal airway space and in tongue and hyoid bone positions following the surgical correction of mandibular prognathism. Int J Adult Orthodon Orthognath Surg. 1994;9:285–290. [PubMed] [Google Scholar]
- 7.Hochban W, Schurmann R, Bradenburg U, Conradt R. Mandibular set back for the surgical correction of mandibular hyperplasia—does it provoke sleep-related breathing disorders. Int J Oral Maxillofac Surg. 1996;25:333–338. doi: 10.1016/s0901-5027(06)80024-x. [DOI] [PubMed] [Google Scholar]
- 8.Achilleos S, Krogstad O, Lyberg T. Surgical mandible set back and changes in uvuloglossopharyngeal morphology and head posture: a short- and long-term cephalometric study in males. Eur J Orthod. 2000;22:383–394. doi: 10.1093/ejo/22.4.383. [DOI] [PubMed] [Google Scholar]
- 9.Kawamata A, Fujishita M. Three-dimensional computed tomographic evaluation of morphologic airway changes after mandibular set back osteotomy for prognathism. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:278–287. doi: 10.1016/s1079-2104(00)70089-8. [DOI] [PubMed] [Google Scholar]
- 10.Tselnik M, Pogrel A. M. Assessment of the pharyngeal airway space after mandibular set back surgery. J Oral Maxillofac Surg. 2000;58:282–285. doi: 10.1016/s0278-2391(00)90053-3. [DOI] [PubMed] [Google Scholar]
- 11.Turnbull N. R, Battagel J. M. The effects of orthognathic surgery on pharyngeal airway dimensions and quality of sleep. J Orthod. 2000;27:235–247. doi: 10.1179/ortho.27.3.235. [DOI] [PubMed] [Google Scholar]
- 12.Liukkonen M, Vahatalo K, Peltomaki T, Tiekso J, Happonen R. P. Effect of mandibular set back surgery on the posterior airway size. Int J Adult Orthodon Orthognath Surg. 2002;17:41–46. [PubMed] [Google Scholar]
- 13.Eggensperger N, Smolka W, Ilzuka T. Long-term changes of hyoid bone position and pharyngeal airway size following mandibular setback by sagittal split ramus osteotomy. J Craniomaxillofac Surg. 2005;33:111–117. doi: 10.1016/j.jcms.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 14.Güven O, Saraçoğlu U. Changes in pharyngeal airway space and hyoid bone positions after body ostectomies and sagittal split ramus osteotomies. J Craniofac Surg. 2005;16:23–30. doi: 10.1097/00001665-200501000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Kawakami M, Yamamoto K, Fujimoto M, Ohgi K, Inoue M, Kirita T. Changes in tongue and hyoid positions, and posterior airway space following mandibular set back surgery. J Craniomaxillofac Surg. 2005;33:107–110. doi: 10.1016/j.jcms.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 16.Muto T, Yamazaki A, Takeda S. Relationship between the pharyngeal airway space and craniofacial morphology, taking into account head posture. Int J Oral Maxillofac Surg. 2006;36:132–136. doi: 10.1016/j.ijom.2005.04.022. [DOI] [PubMed] [Google Scholar]
- 17.Takagi Y, Gamble J. W, Proffit W. R, Chiristiansen R. L. Postural change of the hyoid bone following osteotomy of the mandible. Oral Surg Oral Med Oral Pathol. 1967;23:688–692. doi: 10.1016/0030-4220(67)90352-0. [DOI] [PubMed] [Google Scholar]
- 18.Fromm B, Lundberg M. Postural behaviour of the hyoid bone in normal occlusion and before and after surgical correction of mandibular protrusion. Sven Tandlak Tidskr. 1970;63:425–433. [PubMed] [Google Scholar]
- 19.Samman N, Tang S. S, Xia J. Cephalometric study of the upper airway in surgically corrected Class III deformity. Int J Adult Orthodon Orthognath Surg. 2002;17:180–190. [PubMed] [Google Scholar]
- 20.Wickwire N. A, White R. P, Jr, Proffit W. R. The effect of mandibular osteotomy on tongue position. J Oral Surg. 1972;30:184–190. [PubMed] [Google Scholar]
- 21.Lew K. Changes in tongue and hyoid bone positions following anterior mandibular subapical osteotomy in patients with Class III malocclusion. Int J Adult Orthodon Orthognath Surg. 1993;8:123–128. [PubMed] [Google Scholar]
- 22.Riley R. W, Powell N. B, Guilleminault C, William W. Obstructive sleep apnea syndrome following surgery for mandibular prognathism. J Oral Maxillofac Surg. 1987;45:450–452. doi: 10.1016/0278-2391(87)90016-4. [DOI] [PubMed] [Google Scholar]
- 23.Muto T, Takeda S, Kanazawa M. The effect of head posture on pharyngeal airway space (PAS) Int J Oral Maxillofac Surg. 2002;31:579–583. doi: 10.1054/ijom.2002.0279. [DOI] [PubMed] [Google Scholar]
- 24.Waite P. D, Vilos G. A. Surgical changes of posterior airway space in obstructive sleep apnea. Oral Maxillofac Surg Clin North Am. 2002;14:385. doi: 10.1016/s1042-3699(02)00033-x. [DOI] [PubMed] [Google Scholar]
- 25.Goodday R. Diagnosis, treatment planning, and surgical correction of obstructive sleep apnea. J Oral Maxillofac Surg. 2009;67:2183. doi: 10.1016/j.joms.2009.03.035. [DOI] [PubMed] [Google Scholar]
- 26.Pereira-Filho V. A, Castro-Silva L. M, Moraes M. Cephalometric evaluation of pharyngeal airway space changes in class III patients undergoing orthognathic surgery. J Oral Maxillofac Surg. 2011 July doi: 10.1016/j.joms.2011.02.132. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 27.Ono T, Lowe A. A, Ferguson K. A, Fleetham J. A. Associations among upper airway structure, body position and obesity in skeletal Class I male patients with obstructive sleep apnea. Am J Orthod Dentofacial Orthop. 1996;109:625–634. doi: 10.1016/s0889-5406(96)70074-4. [DOI] [PubMed] [Google Scholar]
- 28.Tsuiki S, Hiyama S, Ono T, Immura N, Ishiwata N, Kuroda T. Effect of a titratable oral appliance on supine airway size in awake non-apneic individuals. Sleep. 2001;24:554–560. doi: 10.1093/sleep/24.5.554. [DOI] [PubMed] [Google Scholar]
- 29.Riley R. W, Powell N. B. Maxillofacial surgery and obstructive sleep apnea syndrome. Otolaryngol Clin North Am. 1990;23:809–826. [PubMed] [Google Scholar]
- 30.Değerliyurt K, Koichiro U, Hashiba Y, Marukawa K, Nakagawa K, Yamamato E. A comparative CT evaluation of pharyngeal airway changes in class III patients receiving bimaxillary surgery or mandibular set back surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:495–502. doi: 10.1016/j.tripleo.2007.11.012. [DOI] [PubMed] [Google Scholar]
- 31.Riley R. W, Nelson B, Powell N. B, Guilleminault C. Obstructive sleep apnea syndrome. A surgical protocol for dynamic upper airway reconstruction. J Oral Maxillofac Surg. 1993;51:742–747. doi: 10.1016/s0278-2391(10)80412-4. [DOI] [PubMed] [Google Scholar]
- 32.Nimkarn Y, Miles P. G, Waite P. D. Maxillomandibular advancement surgery in obstructive sleep apnea syndrome patients. J Oral Maxillofac Surg. 1995;53:1414–1418. doi: 10.1016/0278-2391(95)90667-3. [DOI] [PubMed] [Google Scholar]
- 33.Prinsell J. R. Maxillomandibular advancement surgery in a site-specific treatment approach for obstructive sleep apnea in 50 consecutive patients. Chest. 1999;116:1519–1529. doi: 10.1378/chest.116.6.1519. [DOI] [PubMed] [Google Scholar]
- 34.Bibby R. E, Preston C. B. The hyoid triangle. Am J Orthod. 1981;80:92–97. doi: 10.1016/0002-9416(81)90199-8. [DOI] [PubMed] [Google Scholar]
- 35.Bibby R. E. The hyoid bone position in mouth breathers and tongue thrusters. Am J Orthod. 1984;85:431–433. doi: 10.1016/0002-9416(84)90164-7. [DOI] [PubMed] [Google Scholar]
- 36.Solow B, Kreiborg S. Soft-tissue stretching: a possible control factor in craniofacial morphogenesis. Scand J Dent Res. 1977;85:505–507. doi: 10.1111/j.1600-0722.1977.tb00587.x. [DOI] [PubMed] [Google Scholar]
- 37.Linder-Aronson S. Naso-respiratory function and craniofacial growth. In: McNamara J. A, editor. Nasorespiratory Function and Craniofacial Growth Monograph 9. Ann Arbor, Mich: University of Michigan; 1979. pp. 121–147. [Google Scholar]
- 38.Solow B, Siersbaek-Nielsen P. W, Greve E. Airway adequacy, head posture and craniofacial morphology. Am J Orthod. 1984;86:214–223. doi: 10.1016/0002-9416(84)90373-7. [DOI] [PubMed] [Google Scholar]
- 39.Winnberg A, Pancherz H, Westesson P. L. Head posture and hyomandibular function in man: a synchronized electromyographic and videofluorographic study of the open close-clench cycle. Am J Orthod Dentofacial Orthop. 1988;94:393–404. doi: 10.1016/0889-5406(88)90128-x. [DOI] [PubMed] [Google Scholar]