Abstract
Objective:
To compare the dentofacial effects of maxillary protraction with two facemask therapies in growing Class III patients: facemask in association with miniscrew implants (MSI/FM) and facemask with rapid maxillary expanders (RME/FM).
Materials and Methods:
Forty-three Chinese patients with Class III malocclusion and maxillary deficiency were randomly assigned to a MSI/FM sample of 20 patients and a RME/FM sample of 23 subjects. The changes in dentofacial cephalometric variables from the beginning (T1) to the end of treatment (T2) were compared with t-test for paired samples in both groups and for independent samples between the two groups.
Results:
No significant cephalometric differences were observed between the two groups in active treatment effects except for maxillary dental variables. However, significant favorable changes in both maxillary and mandibular skeletal components were noted in two groups after treatment. Sagittal measurements showed the maxilla was advanced, mandibular projection was reduced, and the relative sagittal intermaxillary discrepancy improved. Patients experienced additional unfavorable outcomes of clockwise rotation of the mandible as well as retroclination of the lower incisors. The soft tissue profile was improved remarkably in both groups. Proclination of the maxillary incisors and mesialization of the maxillary dentition were significantly different between the two groups. The increases in U1-SN, U1-VR, and U6-VR were 6.41°, 2.78 mm, and 1.24 mm less in the MSI/FM group than in the RME/FM group, respectively.
Conclusions:
Compared with the RME/FM therapy, the MSI/FM protocol using a smaller magnitude of protraction force improves skeletal relationships and soft tissue profile and reduces the undesired dentoalveolar effects.
Keywords: Class III malocclusion, Maxillary protraction, Miniscrew implants
INTRODUCTION
Protraction of the maxilla with facemask is a common treatment for Class III malocclusion with maxillary deficiency, especially at early ages. However, a conventional force system that uses dental anchorage has some inherent challenges. Indirect application of force limits the potential for orthopedic change and inevitably causes undesired tooth movements such as mesial movement and extrusion of the maxillary molars and proclination of the maxillary incisors.1–3
Orthopedic anchorage for maxillary protraction is a new area of research and has been used increasingly over recent years.4–12 Miniplates6–10 have been reported successful for maxillary protraction in Class III patients. In 1997, Kanomi13 first mentioned a temporarily placed miniscrew for orthodontic anchorage. The following years brought more refined screw designs. Miniscrews have now become established orthodontic anchorage aids.11,12,14,15 Compared with other skeletal anchorage systems, miniscrew implants have the advantages of operational convenience, comfort, and inexpensiveness. Additionally, immediate loading and long-term stabilization are possible using miniscrew implants as rigid anchors.
The purpose of this study was to evaluate the effects of maxillary protraction using miniscrew implants with facemask (MSI/FM). Specifically, we compared the active treatment effects of skeletal, dentoalveolar, and soft tissue structures in the MSI/FM group with changes in a matched control group treated by using rapid maxillary expanders in conjunction with facemask (RME/FM).
MATERIALS AND METHODS
Subjects
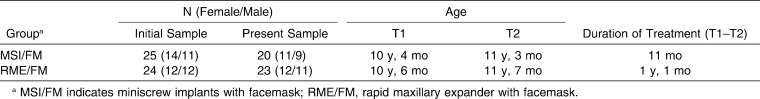
The original sample of 49 Chinese patients (26 female and 23 male) with a prepubertal stage of skeletal maturity according to the cervical vertebral maturation method (CS1–CS3) was recruited. The patients met the following criteria: skeletal and dental Class III malocclusion with maxillary deficiency (ANB < −0°; Wits appraisal < −2 mm), reverse incisor relationship and positive overbite, no significant skeletal asymmetry, and no systemic diseases or congenital deformities. This study was reviewed and approved by the Ethics Committee of ShenZhen Children's Hospital. After informed consent, the patients were randomly assigned to the MSI/FM group (25 patients, 14 female and 11 male) or the RME/FM group (24 patients, 12 female and 12 male). During treatment, four subjects of the initial MSI/FM group were excluded because of the mobility of miniscrews, and one subject of each group was excluded because of poor cooperation. At the end of treatment, the MSI/FM group had 20 subjects (11 female and 9 male; mean age at T1, 10 years 4 months; mean treatment duration, 11 months), and the RME/FM group had 23 subjects (12 female and 11 male; mean age at T1, 10 years 6 months; mean treatment duration, 1 year 1 month). The patient details are presented in Table 1.
Table 1.
Number, Age at Start (T1) and End (T2) of Treatment, and Duration of Treatment of the Patients
MSI/FM Protocol
The miniscrew was 2 mm in diameter and 14 mm in length (ShenGang, ZhangHua, Taiwan). The implant site was the zygomatic buttress of the maxilla. The miniscrews were inserted under local anesthesia. A 4-mm vertical incision was made with a surgical blade at the mucogingival junction above the maxillary first molar. A mucoperiosteal flap was elevated to expose the zygomatic process of the maxilla. A 1.5-mm spiral drill was used to drill a pilot hole under irrigation with normal saline solution. The miniscrew was then driven into the pilot hole with a screwdriver at an angle of 55° to 70° to the maxillary occlusal plane as suggested by Loiu et al.16 and Lin.17 The head of the miniscrews remained outside the mucogingival junction so that elastics could be attached. The miniscrews were left for 2 weeks to allow adequate wound healing before loading.
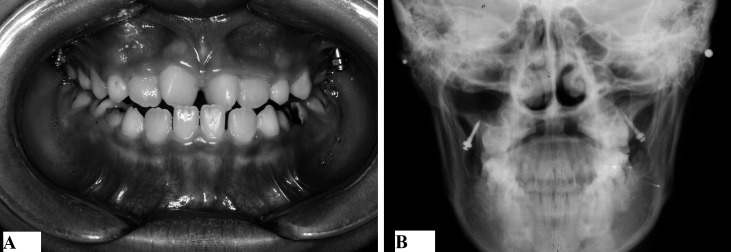
A Petit facemask was subsequently fitted with the application of 200 g to 250 g force to the miniscrews on each side at a 30° angle downward to the occlusal plane. The patients were instructed to wear the facemasks for at least 14 hours per day (Figure 1).
Figure 1.
(A) Intraoral view of the miniscrews. (B) Cephalometric view of the miniscrews.
RME/FM Protocol
Treatment began with the placement of a bonded maxillary expander (Hyrax, Leone, Florence, Italy). Patients were instructed to activate the expander twice a day with a quarter turn (0.5 mm/d) until the desired transverse width was achieved. The patients were given facemask and RME simultaneously. Elastics were attached from the hooks of the expander to the Petit facemask in a downward and forward vector, producing orthopedic forces of 400 g to 500 g per side.
All patients were treated to a positive dental overjet before discontinuing treatment. Standardized lateral cephalograms of each patient were taken at the beginning (T1) and end of treatment (T2). All radiographs were taken with the same cephalometer.
Cephalometric Analysis
The radiographs were scanned into the digital format at 600 dpi and then processed by one investigator (Dr Ge) using Dental Studio NX software (NemoCeph-C software, Nemotec, Madrid, Spain). The customized cephalometric analysis containing measurements from the analyses of Jacobson, McNamara, Ricketts, Wits, and Steiner generated 24 variables for each tracing.
To examine the movement of the maxillary dentition relative to the maxilla, a maxillary horizontal reference plane (HR) was drawn along the ANS-PNS line, and a vertical line passing through PNS and perpendicular to the HR was the maxillary vertical reference plane (VR) (Figure 2).
Figure 2.
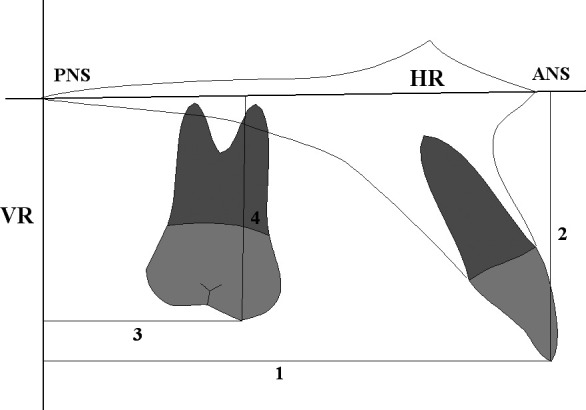
Maxillary dentoalveolar measurements used in the study. (1) U1-VR, mm. (2) U1-HR, mm. (3) U6-VR, mm. (4) U6-HR, mm.
To evaluate tracing and measurement errors, 40 lateral cephalograms of 20 patients were randomly selected and remeasured by the same investigator 1 month later. The estimate of random errors was made using the Dahlberg formula. No systematic errors were found. The mean errors for angular and linear measurements were from 0.4° to 1.4° and from 0.1 to 1.2 mm, respectively.
Statistical Analysis
Descriptive statistics were calculated for all measurements at T1 and T2 by using the Statistical Package for Social Science (version 13.0, SPSS, Chicago, Ill). Paired samples t-tests were used to determine the statistical significance of cephalometrics between T1 and T2 for each group. T1–T2 changes in both groups and the differences of the changes between two groups were assessed with independent sample t-tests. Statistical significance was tested at P < .05, P < .01, and P < .001.
RESULTS
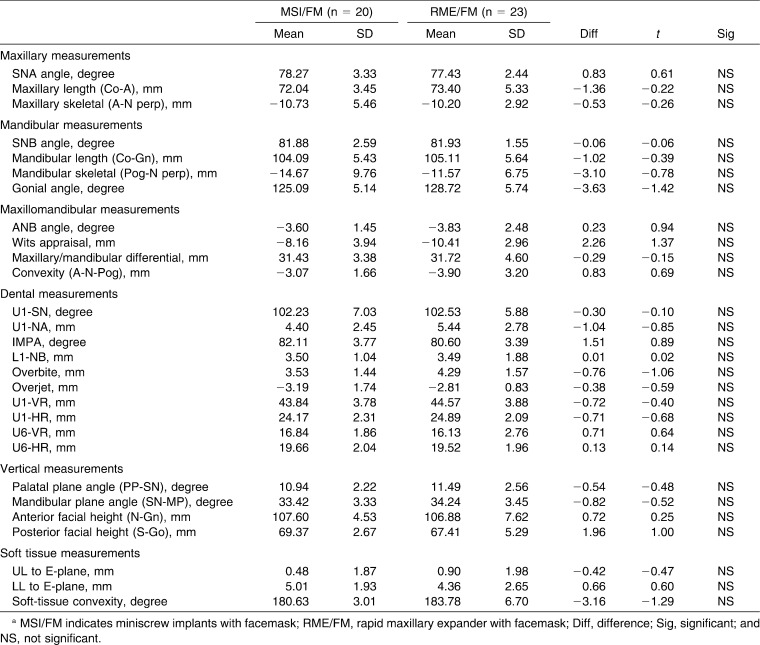
The analysis of the dentofacial characteristics at T1 (Table 2) revealed that there were no statistically significant differences between the two groups for the analyzed parameters. The homogeneity of the two groups allowed for comparisons without annualizing the data.
Table 2.
Comparison of Cephalometric Measurements Between the MSI/FM Group and the RME/FM Group at T1a
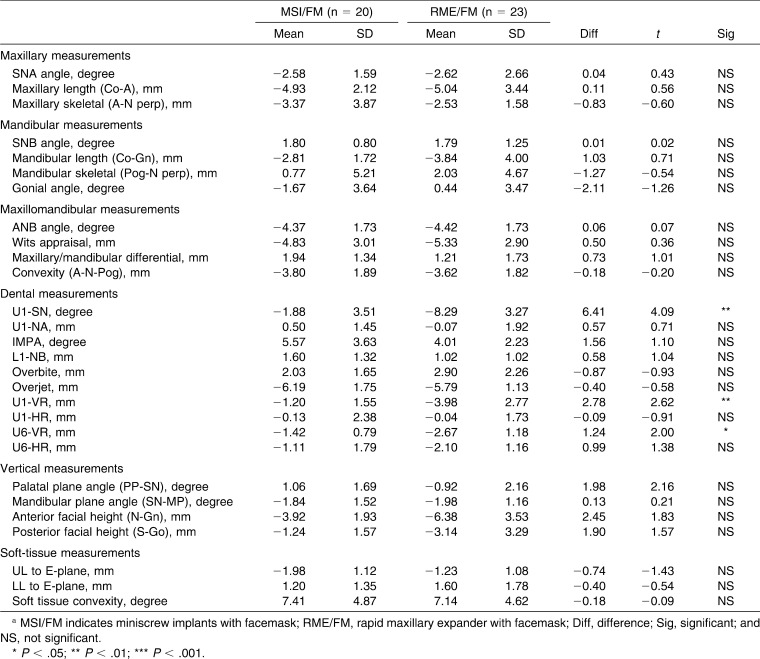
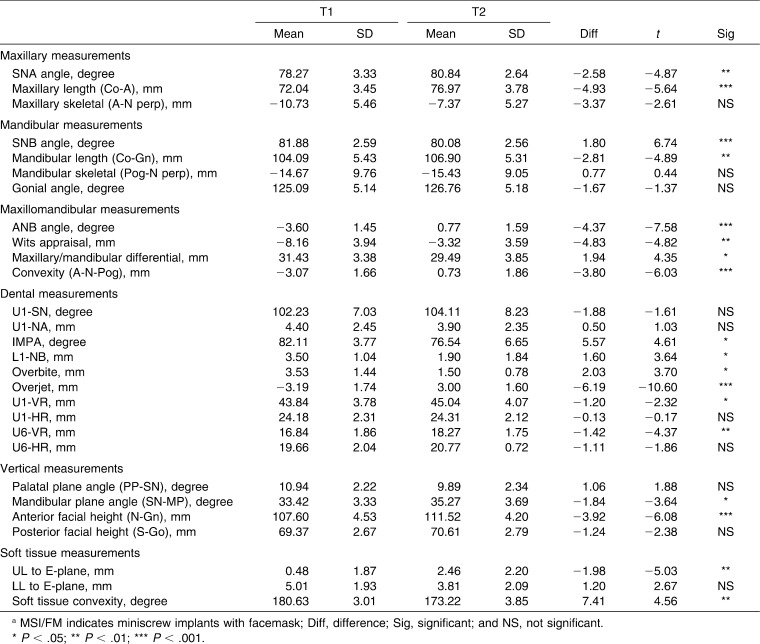
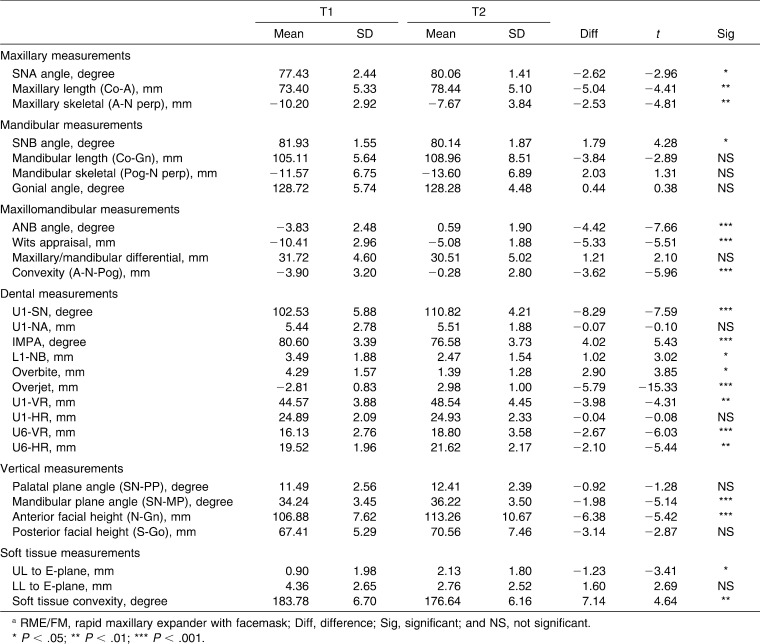
There were no significant differences for T1–T2 changes (Table 3) between groups MSI/FM and RME/FM in any skeletal measured cephalometric variable. The changes between T1 and T2 (Tables 4 and 5), however, revealed significant treatment effects in both groups. Co-A showed average improvements of 4.93 mm in the MSI/FM group and 5.04 mm in the RME/FM group; and A-N perp increased 3.37 mm and 2.53 mm, respectively. Significant restraining effects on mandibular growth were recorded in two groups, both at B-point and Pog-point. The combined movement of the maxilla and the mandible produced highly significant intermaxillary skeletal improvements, with increases in the Wits appraisal of 4.83 mm and 5.33 mm, and an average increase in the convexity of 3.80 mm and 3.62 mm in the MSI/FM and RME/FM group, respectively. Significant clockwise rotation of the mandibular plane and increase in the anterior facial height were found after treatment in both groups.
Table 3.
Comparison of Treatment Changes (T1–T2) Between the MSI/FM Group and the RME/FM Groupa
Table 4.
Comparison of Cephalometric Measurements of the MSI/FM Group Between T1 and T2a
Table 5.
Comparison of Cephalometric Measurements of the RME/FM Group Between T1 and T2a
Of the dentoalveolar measurements, overjet improved significantly—6.19 mm and 5.79 mm in the MSI/FM and the RME/FM group, respectively. A significant retroclination was recorded for the mandibular incisors in both the MSI/FM and RME/FM groups, but no significant difference was found between the two groups. However, significant differences in the changes of maxillary dentoalveolar parameters between the two groups were detected. The measurements associated with the position of the maxillary dentition relative to the maxilla showed significant forward movements of the maxillary dentition in both groups, whereas this movement was more evident in the RME/FM group. The maxillary incisors showed significant proclination (U1-SN) in the RME/FM group, whereas this was not seen in the MSI/FM group (Tables 4 and 5). The increases in U1-SN, U1-VR, and U6-VR were 6.41°, 2.78 mm, and 1.24 mm less in the MSI/FM group than in RME/FM group, respectively.These three variables were the only significant differences between the two groups (Table 3).
Soft tissue variables showed significant improvements. UL to E-plane increased 1.98 mm and 1.08 mm in the MSI/FM vs the RME/FM group; soft tissue convexity increased 7.41° and 7.14°, respectively (Tables 4 and 5), whereas no significant difference was seen between groups (Table 3).
DISCUSSION
Anatomically, the zygomatic buttress of the maxilla is a pillar of cortical bone running along the zygomatic process of the maxilla and zygoma. It has two cortical plates—the buccal cortical plate and the sinus floor. This anatomic advantage allows for bicortical fixation and possibly contributes to better primary stability of the miniscrew. Miniscrews achieve their retention purely mechanically,18 so a thicker bone allows greater miniscrew biting depth, more osseous contact and subsequently better primary stability of the miniscrew. According to Misch19 and Misch and Kircos,20 bone density of the zygomatic buttress is greater than that of the maxillary alveolar ridge. The zygomatic buttress is chosen as an insertion site for orthodontic skeletal anchorage because of its absence of adjacent tooth structure, ease of surgical access, and subsequent ability to apply elastic traction in addition to its thicker bone.
The zygomatic buttress has been used successfully to place skeletal anchorage for maxillary protraction, anterior retraction, maxillary retraction, distal movement of the whole maxillary dentition, and intrusion of the maxillary posterior teeth.4,16,17,21–23 In this study, six miniscrews of four subjects in the MSI/FM group were mobile and these four patients were excluded from the sample. An additional four loose miniscrews were replaced and afterwards remained stable throughout the treatment. Forty-two of all 48 implants survived until the planned orthopedic correction was completed. The success rate of the miniscrews was 87.5%. This coincides with results of available literatures, which reported the mean success rate of miniscrews was 87.9% ± 7.6% ranging from 61.2% to 100%.15,24,25 Using miniscrews inserted in the maxillary zygomatic buttress as skeletal orthopedic anchorage, one may have concerns about the maintenance of stable miniscrews throughout treatment; the underlying concern was that excessive force applied to any temporary skeletal anchors can result in clinical failure, even though most of the literature does not support this idea.25–27 To date, no conclusive evidence exists whether the amount of loading is a decisive factor affecting the success rate of screw implants used as orthodontic anchorage. This study showed that miniscrews inserted in the maxillary zygomatic buttress are a stable anchorage for maxillary protraction. The success rate of miniscrews in this study suggests that the MSI/FM protocol may offer a treatment alternative to standard facemask therapy for Class III patients with maxillary deficiency.
Application of 500 g to 1500 g of the total force is recommended for the protraction of the maxilla. In this study, forces used in the RME/FM group were about 800 g to 1000 g. In the MSI/FM group, however, miniscrew implants were used as rigid skeletal anchors to directly transfer forces to the sutural sides of the maxilla by bypassing the periodontal ligament area, so relatively low loading forces of 200 g to a maximum of 250 g per side were applied, and seemed adequate to achieve clinical improvements. The results showed that both groups produced similar changes in maxillary advancement and the relative sagittal intermaxillary discrepancy improvement with a smaller magnitude of force in the MSI/FM group, suggesting that the forces from the miniscrews were dispersed directly to the circummaxillary sutures by bypassing the periodontal ligament area of the dentition.
The response of the craniofacial complex to active orthopedic treatment with MSI/FM and RME/FM therapies was observed and compared. Significant favorable changes in both maxillary and mandibular skeletal components were noted. The treatment effects produced by the MSI/FM therapy were similar to those produced by the RME/FM therapy. When compared with those reported by other investigators, the cephalometric data of the present study showed encouraging results. In patients treated with facemask and various bone-borne anchors, maxillary advancement ranged from 2.0 mm to 4.8 mm.4–9 Singer et al.4 reported maxillary advancement of 4 mm by using osseointegrated implants as an adjunct to facemask therapy. Enacar et al.5 demonstrated that the entire maxillary complex was affected positively by 4 mm of advancement. Kircelli et al.6 showed that 4.8-mm A-point advancement was achieved with skeletally anchored facemask therapy. Our results in the MSI/FM group parallel these studies.
Two studies8,9 have shown that the facemasks in conjunction with bone-borne anchorage devices result in greater maxillary advancement than those with tooth-borne anchorage devices, but this was not found in our study. The probable reason might have been due to magnitude of protraction force. Forces of 400 g or at least 400 g per side were applied in both bone-borne device group and tooth-borne device group of those two studies. But in our study, the protraction forces were 200 g to 250 g per side in the MSI/FM group and 400 g to 500 g per side in the RME/FM group. Whether higher force levels would result in greater or more rapid orthopedic changes needs to be elucidated in carefully controlled studies.
The incisors relationship improved significantly in both groups as in previous studies.28,29 It has been well documented that facemask treatment results in an increase in maxillary incisor angulation and a decrease in mandibular incisor angulation.1–3 A significant amount of lingual inclination of the mandibular incisors that was also noted previously was observed in both groups. However, the MSI/FM group did not show the significant proclination of maxillary incisors that was present in the RME/FM group. Compared with the RME/FM group, smaller changes were noted in the amount of mesialization of maxillary incisors and molars in the MSI/FM group. The MSI/FM protocol actually eliminated the proclination of the maxillary incisors and reduced the movement of the maxillary dentition usually observed in conventional facemask therapy. The possible explanation of these significant differences in the changes of maxillary dentoalveolar parameters between the two groups could be that the MSI/FM protocol was strictly skeletal. This is an advantage to the MSI/FM treatment, since chance of later relapse would be minimized.
The soft tissue profile reflected the favorable changes noted for the skeletal and dental components of the craniofacial complex. The upper lip had a more anterior position in relation to the E-plane. The improvements in soft tissue convexity agree with the data reported by Macdonald et al.29
Clinicians should be aware of some possible drawbacks of the MSI/FM protocol such as loosening of miniscrews, soft tissue irritation, and infection due to poor oral hygiene. However, this treatment approach offers an alternative to growing Class III patients with maxillary deficiency.
CONCLUSIONS
Miniscrews can be used as a reliable means of rigid anchorage for maxillary protraction. The zygomatic buttress of the maxilla is a substantial region where skeletal anchorage can be placed.
Compared with the RME/FM protocol, the MSI/FM therapy produces a similar maxillary advancement and mandibular restraining in Class III patients with maxillary deficiency using a smaller magnitude of protraction force.
The MSI/FM protocol improves skeletal relationships and soft tissue profile and eliminates the undesired proclination of the maxillary incisors and reduces the mesialization of the maxillary dentition, which are present in the RME/FM therapy.
REFERENCES
- 1.Nartallo-Turley P. E, Turley P. K. Cephalometric effects of combined palatal expansion and facemask therapy on Class III malocclusion. Angle Orthod. 1998;68:217–224. doi: 10.1043/0003-3219(1998)068<0217:CEOCPE>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 2.Hägg U, Tse A, Bendeus M, Rabie A. B. Long term follow-up of early treatment with reverse headgear. Eur J Orthod. 2003;25:95–102. doi: 10.1093/ejo/25.1.95. [DOI] [PubMed] [Google Scholar]
- 3.Franchi L, Baccetti T, McNamara J. A., Jr Postpubertal assessment of treatment timing for maxillary expansion and protraction therapy followed by fixed appliances. Am J Orthod Dentofacial Orthop. 2004;126:555–568. doi: 10.1016/j.ajodo.2003.10.036. [DOI] [PubMed] [Google Scholar]
- 4.Singer S. L, Henry P. J, Rosenberg I. Osseointegrated implants as an adjunct to facemask therapy: a case report. Angle Orthod. 2000;70:253–262. doi: 10.1043/0003-3219(2000)070<0253:OIAAAT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 5.Enacar A, Giray B, Pehlivanoglu M, Iplikcioglu H. Facemask therapy with rigid anchorage in a patient with maxillary hypoplasia and severe oligodontia. Am J Orthod Dentofacial Orthop. 2003;123:571–577. doi: 10.1067/mod.2003.S0889540603000520. [DOI] [PubMed] [Google Scholar]
- 6.Kircelli B. H, Pektas Zo. Midfacial protraction with skeletally anchored facemask therapy: a novel approach and preliminary results. Am J Orthod Dentofacial Orthop. 2008;133:440–449. doi: 10.1016/j.ajodo.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 7.Cevidanes L, Baccetti T, Franchi L, McNamara J. A, Jr, De Clerk H. Comparison of two protocols for maxillary protraction: bone anchors versus face mask with rapid maxillary expansion. Angle Orthod. 2010;80:799–806. doi: 10.2319/111709-651.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Şar C, Arman-Özçırpıcı A. A, Uçkan S, Yazıcı A. C. Comparative evaluation of maxillary protraction with or without skeletal anchorage. Am J Orthod Dentofacial Orthop. 2011;139:636–649. doi: 10.1016/j.ajodo.2009.06.039. [DOI] [PubMed] [Google Scholar]
- 9.Kaya D, Kocadereli I, Kan B, Tasar F. Effects of facemask treatment anchored with miniplates after alternate rapid maxillary expansions and constrictions: a pilot study. Angle Orthod. 2011;81:639–646. doi: 10.2319/081010-473.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee N. K, Yang I. H, Baek S. H. The short-time treatment effects of face mask in Class III patients based on the anchorage device. Angle Orthod. 2012 Jan 20 doi: 10.2319/090811-584.1. [Epub ahead of print] DOI: 10.2319/090811-584.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ludwig B, Glas B, Bowman S. J, Drescher D, Wilmes B. Miniscrews-supported Class III treatment with the Hybrid RPE Advancer. J Clin Orthod. 2010;44:533–539. [PubMed] [Google Scholar]
- 12.Wilmes B, Nienkemper M, Ludwing B, Kau C. H, Drescher D. Early Class III treatment with a hybrid hyrax-mentoplate combination. J Clin Orthod. 2011;45:15–21. [PubMed] [Google Scholar]
- 13.Kanomi R. Mini-implant for orthodontic anchorage. J Clin Orthod. 1997;31:763–767. [PubMed] [Google Scholar]
- 14.Justens E, Bruyn H. D. Clinical outcome of miniscrews used as orthodontic anchorage. Clin Implant Dent Relat Res. 2008;10:174–180. doi: 10.1111/j.1708-8208.2008.00072.x. [DOI] [PubMed] [Google Scholar]
- 15.Crismani A. G, Bertl M. H, Čelar A. G, Bantleon H. P, Burstone C. J. Miniscrew in orthodontic treatment: review and analysis of published clinical trials. Am J Orthod Dentofacial Orthop. 2010;137:108–113. doi: 10.1016/j.ajodo.2008.01.027. [DOI] [PubMed] [Google Scholar]
- 16.Liou E. J, Chen P, Wang Y, Lin J. C. A computed tomographic image study on the thickness of the infrazygomatic crest of the maxilla and its clinical implications for miniscrew insertion. Am J Orthod Dentofacial Orthop. 2007;131:352–356. doi: 10.1016/j.ajodo.2005.04.044. [DOI] [PubMed] [Google Scholar]
- 17.Lin J. J. The new method of IZC miniscrew placement. Chin J Orthod. 2009;16:38–44. [Google Scholar]
- 18.Cope J. B. Temporary anchorage devices in orthodontics: a paradigm shift. Semin Orthod. 2005;11:3–9. [Google Scholar]
- 19.Misch C. E. Bone character: second vital implant criterion. Dent Today. 1988;7:39–40. [Google Scholar]
- 20.Misch C. E, Kircos L. T. Diagnostic imaging and techniques. In: Mish C. E, editor. Contemporary Implant Dentistry 2nd ed. St Louis, Mo: Mosby; 1999. pp. 73–87. [Google Scholar]
- 21.Melsen B, Peterson J. K, Costa A. Zygoma ligatures: an alternative form of maxillary anchorage. J Clin Orthod. 1998;32:154–158. [PubMed] [Google Scholar]
- 22.Clerck H, Geerinckx V, Siciliano S. The zygoma anchorage system. J Clin Orthod. 2002;36:455–459. [PubMed] [Google Scholar]
- 23.Lin J. C. Y, Liou E. J. A new bone screw for orthodontic anchorage. J Clin Orthod. 2003;37:676–682. [PubMed] [Google Scholar]
- 24.Chen Y. J, Chang H. H, Huang C. Y, Hung H. C, Lai E. H, Yao C. C. A retrospective analysis of the failure rate of three different orthodontic skeletal anchorage systems. Clin Oral Implants Res. 2007;18:768–775. doi: 10.1111/j.1600-0501.2007.01405.x. [DOI] [PubMed] [Google Scholar]
- 25.Park H. S, Jeong S. H, Kwon O. W. Factors affecting the clinical success of screw implants used as orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2006;130:18–25. doi: 10.1016/j.ajodo.2004.11.032. [DOI] [PubMed] [Google Scholar]
- 26.Miyawaki S, Koyama I, Inoue M, Mishima K, Sugahara T, Takano-Yamamoto T. Factors associated with the stability of titanium screws placed in the posterior region for orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2003;124:373–378. doi: 10.1016/s0889-5406(03)00565-1. [DOI] [PubMed] [Google Scholar]
- 27.Kuroda S, Sugawara Y, Deguchi T, Kyung H. M, Takano-Yamamoto T. Clinical use of miniscrew implants as orthodontic anchorage: success rates and postoperative discomfort. Am J Orthod Dentofacial Orthop. 2007;131:9–15. doi: 10.1016/j.ajodo.2005.02.032. [DOI] [PubMed] [Google Scholar]
- 28.Baccetti T, McGill J. S, Franchi L, McNamara J. A, Jr, Tollaro I. Skeletal effects of early treatment of Class III malocclusion with maxillary expansion and face-mask therapy. Am J Orthod Dentofacial Orthop. 1998;113:333–343. doi: 10.1016/s0889-5406(98)70306-3. [DOI] [PubMed] [Google Scholar]
- 29.Macdonald K. E, Kapust A. J, Turley P. K. Cephalometric changes after correction of Class III malocclusion with maxillary expansion/facemask therapy. Am J Orthod Dentofacial Orthop. 1999;116:13–24. doi: 10.1016/S0889-5406(99)70298-2. [DOI] [PubMed] [Google Scholar]