Abstract
Objective:
To evaluate, using multislice computed tomography (MSCT), the morphologic changes in the upper airway after large incisor retraction in adult bimaxillary protrusion patients.
Materials and Methods:
Thirty adult patients with bimaxillary protrusion had four first premolars extracted, and then miniscrews were placed to provide anchorage. A CT scan was performed before incisor retraction and again posttreatment. Three-dimensional (3D) reconstruction of the pre- (T1) and post- (T2) CT data was used to assess for morphological changes of the upper airway. A paired t-test was used to compare changes from T1 to T2. The relationship among the three variables (upper incisor retraction amount, upper airway size, and hyoid position) was analyzed by Pearson correlation coefficient.
Results:
The amounts of upper incisor retraction at the incisal edge and apex were 7.64 ± 1.68 mm and 3.91 ± 2.10 mm, respectively. The hyoid was retracted 2.96 ± 0.54 mm and 9.87 ± 2.92 mm, respectively, in the horizontal and vertical directions. No significant difference was observed in the mean cross-sectional area of the nasopharynx (P > .05) between T1 and T2, while significant differences between T1 and T2 were found in the mean cross-sectional areas of the palatopharynx, glossopharynx, and hypopharynx (P < .05); these mean cross-sectional areas were decreased by 21.02% ± 7.89%, 25.18% ± 13.51%, and 38.19% ± 5.51%, respectively. The largest change in the cross-sectional area is always noted in the hypopharynx. There was a significant correlation among the retraction distance of the upper incisor at its edge, the retraction distance of the hyoid in the horizontal direction, and the decrease of the hypopharynx.
Conclusion:
Large incisor retraction leads to narrowing of the upper airway in adult bimaxillary protrusion patients.
Keywords: Upper airway morphology, Large incisor retraction, Bimaxillary protrusion, Multislice computed tomography (MSCT), 3D registration
INTRODUCTION
The goal of orthodontic treatment is not only the coordination and stability of dentofacial structure and facial appearance but also the normal functioning of the stomatognathic system and airway. Bimaxillary protrusion is a common disease in China and is commonly characterized by protrusive and prominent upper and lower incisors and an increased procumbency of the lips.1–4 Typical orthodontic treatment includes extraction of the bimaxillary premolars and anterior tooth retraction, with maximum anchorage achieved through the placement of miniscrews, which enable the practitioners to achieve maximum anterior tooth retraction without undesirable movements of the posterior teeth. Despite the fact that the relationship between maximum anchorage and tooth displacement is well recognized,5,6 retrospective upper airway analysis after retraction of the large incisors remains to be established. The upper airway plays an important role in respiration, swallowing, and pronunciation. Therefore, detailed assessment of the upper airway is still an important foundation of routine orthodontic diagnosis and planning.7,8
Many studies8–10 have demonstrated that the size of the tongue, soft palate and parapharyngeal fat pads, and the position of the lateral pharyngeal walls and mandible and maxillary are all important determinants of upper airway morphology. Previous studies have reported a significant decrease in the size of the upper airway after mandibular setback surgery11,12; this decrease is caused by the permanent posterior and inferior movement of the tongue after mandibular setback surgery.13 These studies have largely examined changes in the upper airway in two dimensions, but two-dimensional assessment of the upper airway morphology is not sufficient to measure the changes in three-dimensional (3D) airway structure. However, there have been no reports related to the upper airway morphologic 3D changes involving large incisor retraction with maximum anchorage in adult patients. For this reason, 3D evaluation is necessary, which could provide changes in the upper airway.
Although cone beam computed tomography allows for accurate assessment of the entire volume of the upper airway, it cannot quantify the upper airway changes caused by the pre- and posttreatment 3D registration as a result of the lack of stable references with a 3D craniofacial model.14 Multislice computed tomography (MSCT) registration might be an acceptable imaging technique supplying quantitative assessment of the upper airway changes in clinics,15,16 and this method might permit an accurate topographical calculation of the upper airway displacements with subvoxel accuracy after identification of the cranial base structures.17,18 In addition, compared with magnetic resonance imaging, MSCT can offer an alternative to reduce the time required to reduce the breathing effects on airway volume. Therefore, this retrospective, analytical study was designed to evaluate the upper airway morphology changes occurring after large incisor retraction in patients with adult bimaxillary malocclusion by retrospective 3D registration.
MATERIALS AND METHODS
Subjects
This research was accepted by the Research Ethic Committee of Shandong University Dental School. Thirty bimaxillary dentoalveolar protrusion patients were randomly selected. All patients provided informed consent and were notified of potential risks, including the damage potentially associated with CT radiation and miniscrew methodologies. They were treated using oriental preadjusted appliance KOSAKA slot brackets (OPA-K, Tomy; Fukushima-ken, Japan), and miniscrews were placed as an anchor for the integral retraction and intrusion of the maxillary teeth. A force of 150 g per side of elastic chains was applied from the miniscrew to the upper crimpable hook to retract and intrude the upper anterior tooth (Figure 1). The patients were seen at 1-month intervals over a period of 12 ± 3 months to retract the upper and lower anterior teeth.
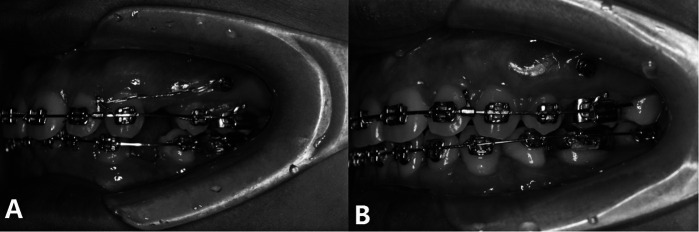
Figure 1.
Miniscrews were placed in the interradicular locations between the first molar and second premolar and were attached at gingival-level height: pretreatment (A) and posttreatment (B).
CT Data Acquisition
The skull CT scans were performed before incisor retraction (T1) and posttreatment (T2) with natural head posture and maximum intercuspation during the patients' awake periods at the end of eupnoea, respectively, which was done in the same way using 16-row helical CT (Light Speed Plus, General Electric, Fairfield, Conn), and the patients were asked to maintain the resting position of the tongue tip, which was in contact with the anterior part of the hard palate without touching the anterior teeth.
The CT scans were performed perpendicular to the long axis of the lower central incisors on each slice. The lateral scanogram of the head position set the gantry angle. Scans were made from the level at the nasion to a level at the C3 point (slice thickness: 0.625 mm; reconstruction interval: 0.3 mm; scan time: 1.0 seconds, 120 kV, 250 MA). The CT data were saved in the DICOM (Digital Imaging and Communications in Medicine) format.
3D Virtual Model Reconstruction
All 3D models were constructed from CT images with a voxel dimension of 0.35 × 0.625 × 0.625 mm. The bone, tooth, and upper airway morphology structure were separated, respectively, by the threshold based on Hounsfield Units (HU) in Materialism's Interactive Medical Image Control System (MIMICS, version 10.01; Leuven, Belgium). The separated and independent masks were created for each part, which allowed the next generation of individual geometrical files and 3D models. All 3D masks were exported as stereolithography (STL).
To build 3D models of the upper airway before and after incisor retraction, T1 and T2 CT data were loaded into MIMICS software. Once segmented, the upper airway was refined to obtain the true shape by eliminating projections that did not belong to the airway, and four landmarks were marked in the midsagittal plane (posterior nasal spine, the end of the uvula, the top of the epiglottis, and the C3 point). Following the landmarks, the corresponding cross-sectional slice can be found, which divided the total upper airway into four regions: the nasopharynx, palatopharynx, glossopharynx, and hypopharynx. All of the regions were also reconstructed (Figures 2 and 3).
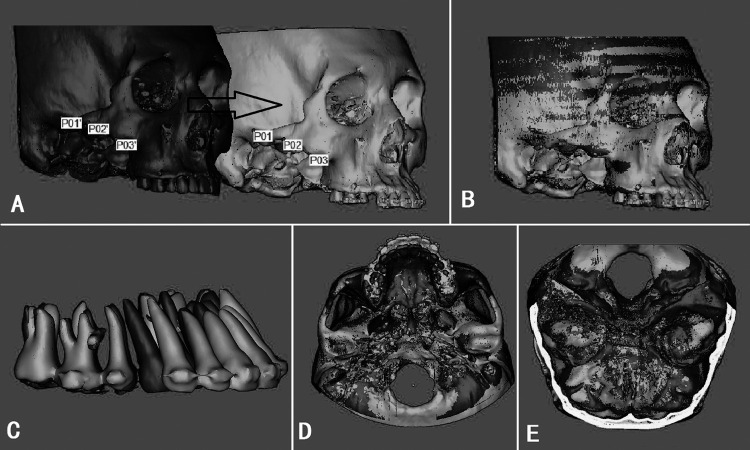
Figure 2.
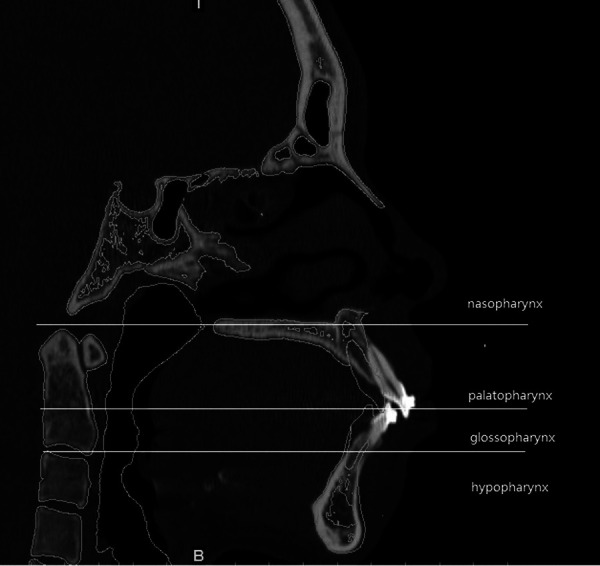
CT scan in sagittal plane after point registration and STL registration; the pharynx was subdivided into four parts by three planes perpendicular to the sagittal plane.
Figure 3.
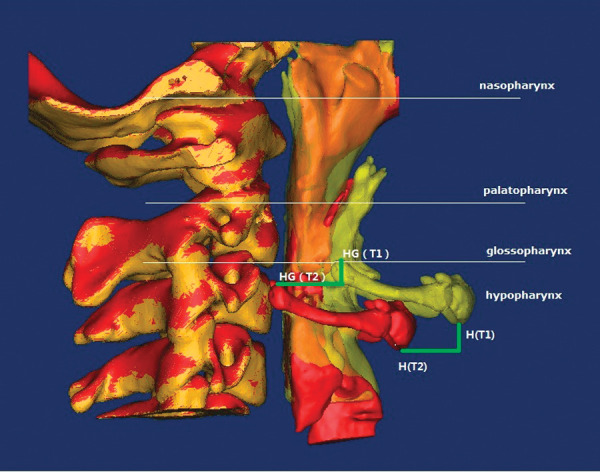
The 3D model of four parts of the pharynx, hyoid, and cervical vertebra after point registration and STL registration and the distance between T1 and T2 models were measured.
Registration of Pre- and Posttreatment Models
In MIMICS, STL was moved to a certain location by point registration, which was accomplished by laying the zygomatic arch landmarks on the pre- and posttreatment STLs and 3D models (Figure 4A,B).14,15 The software calculated the transformation matrix to fit best between the start-end points on STL and then applied it on the selected one. After point registration, STL registration was performed to place STL on the CT mask in order to improve the accuracy. In order to ensure the precision, corresponding landmarks were identified repeatedly (minimal point distance filter was 0.10 mm, which was satisfied, as in Figure 4D,E). All of the registrations were done three times over the course of 2 weeks, and the best registration was chosen for the measurements.
Figure 4.
The effect of point registration (A, B) and STL registration (C, D, E). The teeth and maxilla were registered with the surface points that did not change after orthodontic treatment: (A) the most protruding points on the inferior margin of the zygomatic arch; (B) registration of pre- and posttreatment models; (C) the pre- and posttreatment models of the teeth were matched to each other after the registration of maxillary; (D) STL registration with cranial base; and (E) STL model occlusal view.
3D Measurement
In this study, the nasopharynx was defined as the region between the roof of the upper airway and the hard palate; the palatopharynx lay between the hard palate and the end of the uvula; the glossopharynx was from the end of the uvula to the top of the epiglottis; and the hypopharynx was between the top of the epiglottis and the base of the epiglottis (the level of C3). After registration, the cross-sectional area of each region from nasopharynx to hypopharynx was measured using the MIMICS. The displacement of the upper incisor and hyoid were also calculated in the 3D model. The landmarks identified on each 3D model were incisor crown edge (ICE), incisor root apex (IRA; Figure 5), the most anterior and inferior point on the hyoid (H point), the most anterior and superior point on the greater born of the hyoid on both sides (GH point; Figure 3), and the cross-sectional areas (CSA) of the pharynx on each CT sagittal slice (Figure 6). The preceding variables measured on each 3D model are shown in Table 1. Every subject was measured three times by the same investigator, and then the measurements were averaged.
Figure 5.
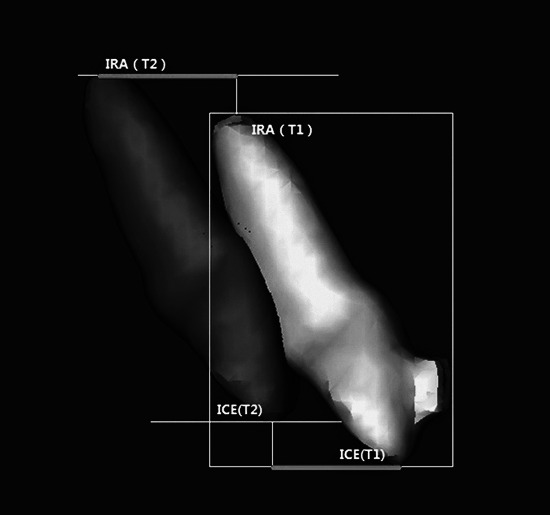
Changes in the teeth between the T1 and T2 models were measured.
Figure 6.
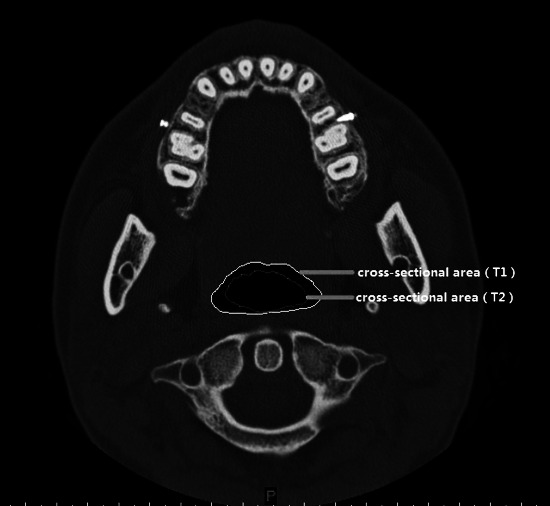
Changes in the cross-sectional areas of the pharynx between T1 and T2 models were measured.
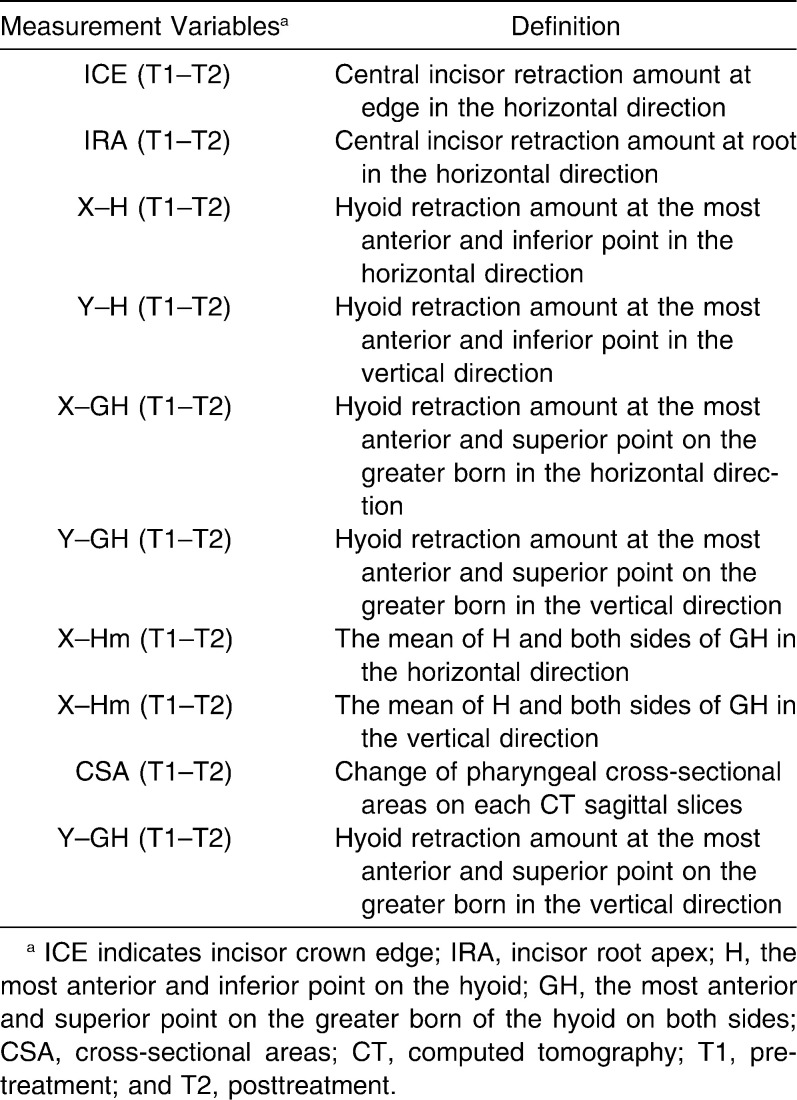
Table 1.
Measurement Parameters of Teeth, Hyoid and Cross-sectional Areas of Pharynx Used
Statistical Analysis
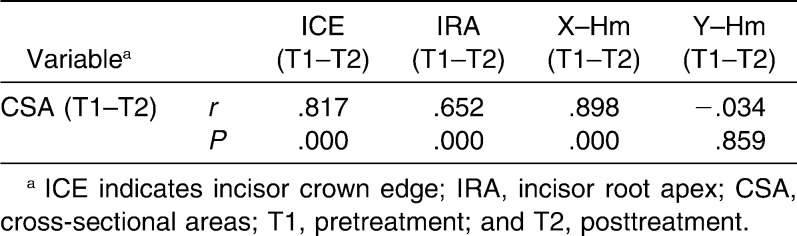
All statistical analyses were performed using the SAS software package (version 9.13, SAS Institute, Cary, NC). For each variable measured on the 3D models, the mean and the standard deviation (SD) were calculated. Differences in the cross-sectional area of the upper airway between T1 and T2 were assessed using paired t-tests, and then the relationships between the three variables (upper incisor retraction amount, the distance change of hyoid retraction in the horizontal direction and vertical direction [X–Hm, Y–Hm; this value is the mean of H and both sides of GH], and the change in the pharyngeal cross-sectional area) were assessed using the Pearson correlation coefficient. The error of the method, based on double measurements at a 2-month interval, was calculated for 30 randomly selected patients for 3D linear measurements (as described by Houston19) and was calculated as follows: s = √Σ (d)2/2n (where d indicates deviations between the two measurements and n indicates number of paired objects). The error was 0.26 mm (SD of d is 0.14 mm) for 3D linear measurement and was 0.13 mm2 (SD of d is 0.07 mm2) for measurement of the upper airway cross-sectional area. The statistical difference was not significant between the two measurements by paired t-test at the significance level of α = .05.
RESULTS
Using the paired t-test, we tested whether there was a significant difference in the size of the nasopharynx, palatopharynx, glossopharynx, and hypopharynx between pre- and posttreatment. By setting the significance level at α = .05 and determining the value of t0.05(n − 1) = t0.05(29) = 1.699 based on the t-distribution with n − 1 degrees of freedom, there was a significant difference if ti > t0.05(29), i = 0, 1, 2, 3, where ti is the sample value of the t-test statistic based on 30 sample values at the nasopharynx, palatopharynx, glossopharynx, and hypopharynx. Otherwise, there was no significant difference. We computed t3 > t2 > t1 > t0.05(29) > t0; namely, we concluded that there was no significant difference in nasopharynx between pre- and posttreatment, and the cross-sectional area decreased significantly in the palatopharynx, glossopharynx, and hypopharynx. In addition, the mean cross-sectional areas of these three parts of the upper airway were decreased by 21.02% ± 7.89% (mean ± SD), 25.18% ± 13.51%, and 38.19% ± 5.51%, respectively. In addition, the change in the hypopharynx was greatest.
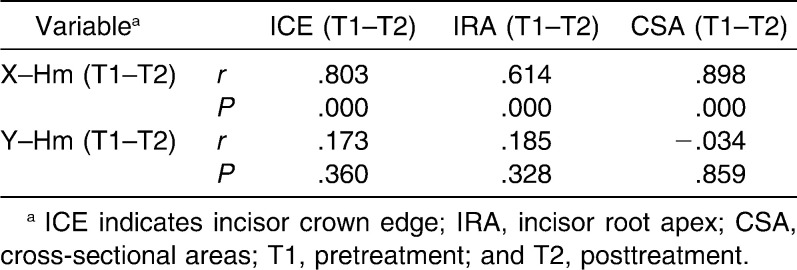
The amounts of upper incisor retraction at the edge and apex were 7.64 ± 1.68 mm (mean ± SD) and 3.91 ± 2.10 mm, respectively, and with the retraction of the incisors, the hyoid was retracted by 2.96 ± 0.54 mm and 9.87 ± 2.92 mm in the horizontal and vertical directions, respectively. A significant correlation was observed in the mean amount of central incisor retraction at the edge, the hyoid retraction amount in the horizontal direction, and the change of cross-sectional area in the hypopharynx (Tables 2 and 3).
Table 2.
Pearson Correlation Coefficient Analysis Between the Hyoid Retraction Amount and Some Parameters (n = 30)
Table 3.
Pearson Correlation Coefficient Analysis Between the Changes of Hypopharynx and Some Parameters (n = 30)
DISCUSSION
Narrowing in one or more segments of the upper airway may induce breathing problems. The upper airway is an irregular lumen. As a result of individual differences, the volume of the upper airway cannot reflect the narrowest position of the airway. Thus, cross-sectional area is a better indicator than volume with which to evaluate change in the size of the upper airway.19 The changes in the sizes of the palatopharynx, glossopharynx, and hypopharynx between pre- and posttreatment are shown in our study, and the greatest change occurs in the hypopharynx, which is inconsistent with the findings of other studies, showing that extraction of four premolars with retraction of incisors does not affect oropharynx (OP) airway volume.20 In addition, some studies have described that the nasopharynx and hypopharynx were not easy to deform because of supportive bone and cartilage, while the antetheca of the palatopharynx and glossopharynx was made up of the soft palate and tongue, which were easily affected by the change in the surrounding tissue. Retraction of large incisors with extraction and use of miniscrews decreased the oral volume, which in turn reduced the tongue's space in terms of the sagittal condition, and then the tongue retracted to press the soft palate, and this movement resulted in an adaptation leading to the diminution of the upper airway.21
However, using the Pearson correlation coefficient, a significant correlation is observed among the amount of central incisor retraction at the edge, the hyoid retraction amount in the horizontal direction, and the change of the cross-sectional area in the hypopharynx. Therefore, we infer that the main reason for the narrowing of the hypopharynx may be the retraction of the hyoid, which is caused by the retraction of the central incisor. Previous studies have shown a possible relationship between hypopharynx and skeletal structures, soft tissues, and musculature. For example, hyoid position changes after mandibular setback surgery. Kawakami et al.13 confirmed that the vertical and horizontal spaces around the tongue were maintained postoperatively with the backward and downward movement of the hyoid, which compensates for the reduction in oral volume caused by the mandibular setback.22 Furthermore, some studies14,23,24 showed that the positional change in the hyoid decreased the pharyngeal airway size. Thus, the hyoid plays a vital role in the narrowing of the upper airway caused by large incisor retraction. However, the long-term stability of the hyoid and pharyngeal size are unknown; further long-term research on the dynamic analysis of airway resistance is needed.
CONCLUSION
The mechanobiological response of the upper airway should be taken into consideration during large incisor retraction, as the pursuit of large incisor retraction may lead to a narrowing of the upper airway in bimaxillary protrusion adult patients.
Acknowledgments
Based on a thesis submitted to the graduate faculty, University of Shandong, in partial fulfillment of the requirements for the master's degree, this study was supported by grants from Shandong Science and Technology Planning Project Contract Research (2008GG30002019 and 2008GG30001001, Y2008C66, 2009GG10002059) and Shandong University Dental School Project Research (2011JC009, P2009009) of China.
REFERENCES
- 1.Bills D. A, Handelman C. S, BeGole E. A. Bimaxillary dentoalveolar protrusion: traits and orthodontic correction. Angle Orthod. 2005;75:333–339. doi: 10.1043/0003-3219(2005)75[333:BDPTAO]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 2.Lai E. H, Yao C. C, Chang J. Z, Chen I, Chen Y. J. Three-dimensional dental model analysis of treatment outcomes for protrusive maxillary dentition: comparison of headgear, miniscrew, and miniplate skeletal anchorage. Am J Orthod Dentofacial Orthop. 2008;134:636–645. doi: 10.1016/j.ajodo.2007.05.017. [DOI] [PubMed] [Google Scholar]
- 3.Leonardi R, Annunziata A, Licciardello V, Barbato E. Soft tissue changes following the extraction of premolars in nongrowing patients with bimaxillary protrusion. A systematic review. Angle Orthod. 2010;80:211–216. doi: 10.2319/010709-16.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chu Y. M, Bergeron L, Chen Y. R. Bimaxillary protrusion: an overview of the surgical-orthodontic treatment. Semin Plast Surg. 2009;23:32–39. doi: 10.1055/s-0028-1110099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yao C. C, Lai E. H, Chang J. Z, Chen I, Chen Y. J. Comparison of treatment outcomes between skeletal anchorage and extraoral anchorage in adults with maxillary dentoalveolar protrusion. Am J Orthod Dentofacial Orthop. 2008;134:615–624. doi: 10.1016/j.ajodo.2006.12.022. [DOI] [PubMed] [Google Scholar]
- 6.Deguchi T, Murakami T, Kuroda S, Yabuuchi T, Kamioka H, Takano-Yamamoto T. Comparison of the intrusion effects on the maxillary incisors between implant anchorage and J-hook headgear. Am J Orthod Dentofacial Orthop. 2008;133:654–660. doi: 10.1016/j.ajodo.2006.04.047. [DOI] [PubMed] [Google Scholar]
- 7.Schwab R. J, Goldberg A. N. Upper airway assessment: radiographic and other imaging techniques. Otolaryngol Clin North Am. 1998;31:931–968. doi: 10.1016/s0030-6665(05)70100-6. [DOI] [PubMed] [Google Scholar]
- 8.Jakobsone G, Stenvik A, Espeland L. The effect of maxillary advancement and impaction on the upper airway after bimaxillary surgery to correct Class III malocclusion. Am J Orthod Dentofacial Orthop. 2011;139:e369–e376. doi: 10.1016/j.ajodo.2010.07.022. [DOI] [PubMed] [Google Scholar]
- 9.Shigeta Y, Ogawa T, Ando E, Clark G. T, Enciso R. Influence of tongue/mandible volume ratio on oropharyngeal airway in Japanese male patients with obstructive sleep apnea. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:239–243. doi: 10.1016/j.tripleo.2010.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ozturk E, Dalayman D, Sonmez G, Mutlu H, Sildiroglu H. O, Basekim C. C, Kizilkaya E. The effect of pharyngeal soft tissue components on snoring. Clin Imaging. 2007;31:259–263. doi: 10.1016/j.clinimag.2007.02.024. [DOI] [PubMed] [Google Scholar]
- 11.Chemello P. D, Wolford L. M, Buschang P. H. Occlusal plane alteration in orthognathic surgery—part II: long-term stability of results. Am J Orthod Dentofacial Orthop. 1994;106:434–440. doi: 10.1016/S0889-5406(94)70066-4. [DOI] [PubMed] [Google Scholar]
- 12.Kawamata A, Fujishita M, Ariji Y, Ariji E. Three-dimensional computed tomographic evaluation of morphologic airway changes after mandibular setback osteotomy for prognathism. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:278–287. doi: 10.1016/s1079-2104(00)70089-8. [DOI] [PubMed] [Google Scholar]
- 13.Kawakami M, Yamamoto K, Fujimoto M, Ohgi K, Inoue M, Kirita T. Changes in tongue and hyoid positions, and posterior airway space following mandibular setback surgery. J Craniomaxillofac Surg. 2005;33:107–110. doi: 10.1016/j.jcms.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 14.Cevidanes L. H, Motta A, Proffit W. R, Ackerman J. L, Styner M. Cranial base superimposition for 3-dimensional evaluation of soft-tissue changes. Am J Orthod Dentofacial Orthop. 2010;137:S120–S129. doi: 10.1016/j.ajodo.2009.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gibbs J. D, Graham M. W, Higgins W. E. 3D MDCT-based system for planning peripheral bronchoscopic procedures. Comput Biol Med. 2009;39:266–279. doi: 10.1016/j.compbiomed.2008.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu D. X, Liu H, Lv T. Application of three dimensional registration based on CT data for orthodontics. Hua Xi Kou Qiang Yi Xue Za Zhi. 2010;28:119–123. [PubMed] [Google Scholar]
- 17.Liu H, Liu D-X, Wang G, Wang C-L, Zhao Z. Accuracy of surgical positioning of orthodontic miniscrews with a computer-aided design and manufacturing template. Am J Orthod Dentofacial Orthop. 2010;137:728.e1–728.e10. doi: 10.1016/j.ajodo.2009.12.025. [DOI] [PubMed] [Google Scholar]
- 18.Liu H, Lv T, Wang N. N, Zhao F, Wang K. T, Liu D. X. Drift characteristics of miniscrews and molars for anchorage under orthodontic force: 3-dimensional computed tomography registration evaluation. Am J Orthod Dentofacial Orthop. 2011;139:e83–e89. doi: 10.1016/j.ajodo.2010.07.018. [DOI] [PubMed] [Google Scholar]
- 19.Houston W. J. B. The analysis of errors in orthodontic measurements. Am J Orthod. 1983;83:382–390. doi: 10.1016/0002-9416(83)90322-6. [DOI] [PubMed] [Google Scholar]
- 20.Bhattacharyya N, Blake S. P, Fried M. P. Assessment of the airway in obstructive sleep apnea syndrome with 3-dimensional airway computed tomography. Otolaryngol Head Neck Surg. 2000;123:444–449. doi: 10.1067/mhn.2000.109367. [DOI] [PubMed] [Google Scholar]
- 21.Valiathan M, El H, Hans M. G, Palomo M. J. Effects of extraction versus non-extraction treatment on oropharyngeal airway volume. Angle Orthod. 2010;80:1068–1074. doi: 10.2319/010810-19.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ke-feng X. U, Wei C, Liu Y-H. Effects of large retraction of incisors due to orthodontic treatment on the upper airway dimensions in young adult patients with malocclusion. J Clin Stomatol. 2010;26:600–603. [Google Scholar]
- 23.Eggensperger N, Smolka W, Iizuka T. Long-term changes of hyoid bone position and pharyngeal airway size following mandibular setback by sagittal split ramus osteotomy. J Craniomaxillofac Surg. 2005;33:111–117. doi: 10.1016/j.jcms.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 24.Enacar A, Aksoy A. U, Sençift Y, Haydar B, Aras K. Changes in hypopharyngeal airway space and in tongue and hyoid bone positions following the surgical correction of mandibular prognathism. Int J Adult Orthod Orthognath Surg. 1994;9:285–290. [PubMed] [Google Scholar]
- 25.Achilleos S, Krogstad O, Lyberg T. Surgical mandibular setback and changes in uvuloglossopharyngeal morphology and head posture: a short- and long-term cephalometric study in males. Eur J Orthod. 2000;22:383–394. doi: 10.1093/ejo/22.4.383. [DOI] [PubMed] [Google Scholar]