Abstract
Objective:
To determine if there are significant clinical differences between self-ligating brackets (SLB) and conventional brackets (CB) during orthodontic treatment, as perceived by orthodontists.
Materials and Methods:
A survey was developed and distributed to evaluate how SLB compare to CB in terms of orthodontists' perceptions (n = 430).
Results:
SLB were preferred during the initial stage of treatment based on the shorter adjustment appointments and faster initial treatment progress they provided (P < .0001). On the other hand, practitioners preferred CB during the finishing and detailing stages of treatment (P < .0001). CB were also preferred over SLB because they were cheaper and resulted in fewer emergency appointments.
Conclusions:
The orthodontists' preference was significantly influenced by (1) the proportion of patients treated with SLB (P < .0001), (2) the number of cases it took them to become accustomed to SLB (P < .0001), and (3) the average appointment intervals associated with SLB (P < .0001).
Keywords: Self-ligating brackets, Perception, Bracket preference
INTRODUCTION
Currently, the orthodontic market includes several different types of self-ligating brackets (SLB). Manufacturers and advocates of SLB claim that SLB offers advantages over conventional brackets (CB). The most advantageous features proposed with SLB are reduced friction between the archwire and the bracket and full archwire engagement, resulting in faster alignment and space closure.1,2 In addition, it is believed that with self-ligation mechanics, greater arch expansion with less incisor proclination is achieved, and, therefore, fewer extractions are required to provide space to alleviate crowding.3 Other claimed advantages of SLB include less need for chairside assistance, shorter adjustment appointments, shorter overall treatment time, increased patient comfort, better oral hygiene, and increased patient cooperation and acceptance.2,4
Unfortunately, the literature provides conflicting findings with regard to friction and treatment efficiency with the use of SLB. While some studies5–7 have reported less friction with SLB regardless of bracket angulation, others8,9 have found that when tipping and angulation are accounted for, these brackets produce similar or higher friction compared with CB. Furthermore, a recent systematic review10 concluded that, in comparison to CB, SLB maintain lower friction only when coupled with small round archwires in an ideally aligned arch. Sufficient evidence, however, has not been found to claim that SLB produce lower friction with large rectangular wires in the presence of tipping and/or torque and in arches with considerable malocclusion.
Studies on treatment efficiency have reported that on average, patients treated with SLB finished their treatment 4 to 6 months sooner and had fewer appointments than did patients with CB. Contrary to these findings, several studies11–13 reported no difference in total treatment time between cases treated using CB and those treated using SLB.
A systematic review by Fleming and Johal14 reported that there was no evidence to support the use of self-ligating fixed orthodontic appliances over conventional appliance systems (or vice versa). Furthermore, it was concluded that there is not sufficient evidence indicating that the orthodontic treatment is more or less efficient with SBL than with CB. In 2010, the American Association of Orthodontists' Council on Scientific Affairs15 reported that there was either no evidence or weak evidence to support most of the claims indicating that SLB systems provide superior treatment efficiency and efficacy. Therefore, it is possible that the popularity of these bracket systems results from effective marketing and advertisement. The purpose of this study is to determine if the reported advantages of SLB are indeed perceived by orthodontists in their daily practice and whether there is a relationship between the bracket a practitioner prefers and the perceived advantages of that bracket system.
MATERIALS AND METHODS
Prior to beginning the study, approval was obtained from the Institutional Review Board of the Virginia Commonwealth University Office of Research. A one-page questionnaire was developed to determine whether responding orthodontists perceived differences in clinical performance between SLB and CB based on their experience with these appliances.
The initial series of questions obtained individual practitioner characteristics and focused on the responding clinician's experience with SLB in his practice (eg, “How long have you been using SLB?” and “What percentage of your patients do you treat with SLB?”). The second part of the survey assessed a variety of treatment factors, allowing orthodontists to indicate a preference for either SLB or CB based on their experience and perceived clinical results. Duration of treatment time, discomfort experienced by the patients, and likelihood of extraction treatment were some of the factors evaluated in this section of the study. Each survey had a blank section for the respondents' comments.
Power analysis indicated a sample size of 1000 for statistical significance at the significance level of .05. Upon request, The American Association of Orthodontists (AAO) provided a randomly generated list of the names and addresses of 1000 orthodontists under the age of 60 who were practicing in the United States. The AAO granted permission to use these names and addresses for conducting the study, and as a result of antitrust issues, the use of brand names was not allowed by the AAO in exchange for providing the mailing lists of participants. Therefore, the surveys (with addressed, postage-paid return envelopes) were mailed to 1000 orthodontists. A short explanation of the study was provided on the front page of the survey, which requested the orthodontists' voluntary participation. There were identifying markers on the survey to trace back individual respondents, which were matched to a coding list at the mailing center in order to maintain the confidentiality of the submitted responses. A follow-up survey was sent to the orthodontists who did not return a completed survey with the first mailing.
Multi-way repeated-measures analysis of variance (ANOVA) was used to evaluate each of the practitioner characteristics (Table 1) to determine if they had any association with treatment factors when considering bracket preference (Table 2). To determine if there was a preference for either SLB or CB, a score of −1 was used for CB, a score of 0 for no difference, and a score of +1 for SLB. The level of statistical significance across all of the items was controlled using a Bonferroni correction. Statistical significance was maintained at P < .05 for all analyses.
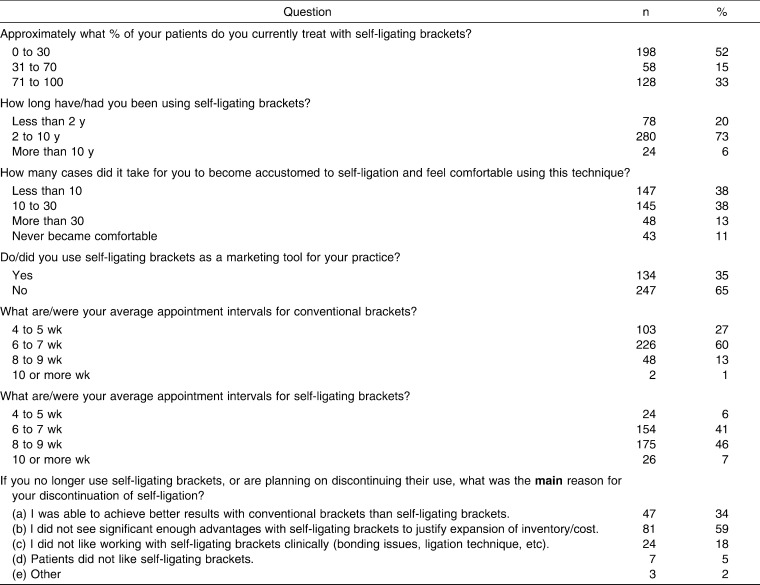
Table 1.
Practitioner Characteristics
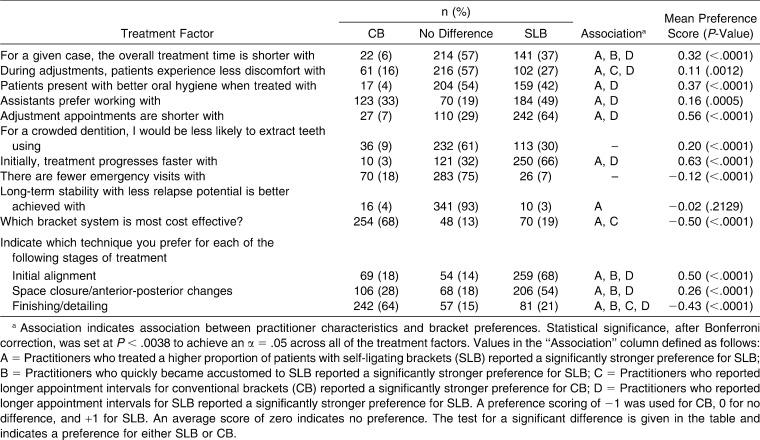
Table 2.
Responses by Orthodontists on Bracket Preference for a Variety of Treatment Factorsa
RESULTS
Out of 1000 survey invitations, 982 were successfully delivered. A total of 430 out of 982 surveys were completed (44% return rate). Of the 430 responding practitioners, 384 (90%) reported that they used or had previously used SLB (Table 1). About half of the orthodontists (52%) indicated that they used SLB on no more than 30% of their patients. The majority of the practitioners (73%) had been using SLB for between 2 and 10 years, and most (76%) became comfortable with them after treating fewer than 30 cases. Thirty-six percent of orthodontists who had used SLB reported that they no longer use them or were planning on discontinuing their use of SLB. Of those who had stopped using SLB, the majority indicated that this was due to the lack of noticeable advantages compared to justifying the expanded inventory and increased costs. Overall, 64% of orthodontists reported that they did not use SLB as a marketing tool for their practice.
The practitioners' preferences for either SLB or CB with regard to a variety of treatment factors are summarized in Figure 1. The repeated-measures ANOVA results are further reported as mean preference scores in Table 2. The 95% confidence intervals on the left side of Figure 1 indicate a preference for CB and on the right side indicate a preference for SLB. Across almost all treatment considerations, there is a preference for SLB (as indicated by the fact that the confidence intervals in Figure 1 do not overlap the “no preference” line and the significant P-value in Table 2).When considering treatment time, 37% of orthodontists indicated that SLB yielded a shorter overall treatment time, and 6% reported that CB yielded a shorter overall treatment time. The remaining 57% of orthodontists reported no difference in overall treatment time between the two bracket types. When asked which bracket causes less discomfort during adjustments, 27% of orthodontists reported that their patients experienced less discomfort during adjustments with SLB, while 57% reported no difference. While 54% of orthodontists indicated that they had not perceived a difference in the oral hygiene of patients treated with CB vs SLB, 42% reported that they perceived better oral hygiene in patients with SLB, as opposed to only 4% with CB (P < .0001). It was perceived that assistants prefer working with SLB (49%) more than CB (33%) (P = .0005). Sixty-four percent of orthodontists claimed shorter adjustment appointments with SLB, and only 30% indicated less likelihood of extracting teeth with SLB than with CB (P < .0001). The majority of respondents (61%) expressed no difference between the two bracket systems when considering the likelihood of extracting teeth in crowded dentitions. Sixty-six percent of orthodontists indicated faster initial treatment with SLB (P < .001). Seventy-five percent of orthodontists reported no difference in the number of emergency visits between SLB and CB. With regard to long-term stability and relapse potential, no significant bracket preference was indicated by the practitioners (P = .2129).
Figure 1.
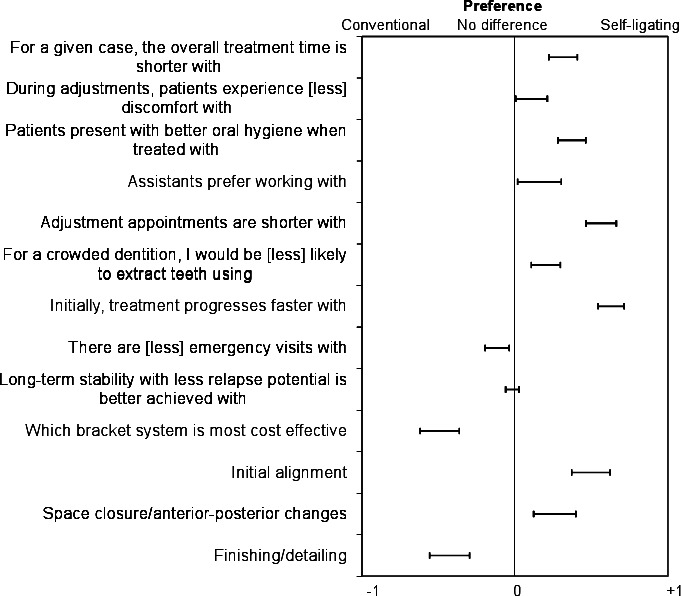
Preferences for SLB or CB for a variety of treatment factors. The bracket preferences are shown as 95% confidence intervals.
While SLB were reported to be significantly preferred based on the shorter adjustment appointments and faster initial treatment progress associated with this bracket system, there were some treatment factors associated with CB that were significantly preferred. CB were found (68%) to be the most cost-effective bracket systems and were significantly preferred over SLB in this regard (P < .0001). While 68% of orthodontists preferred SLB during the initial alignment stage, 64% indicated that they preferred CB over SLB during the finishing and detailing stages of treatment (P < .0001).
When the responses of the practitioners using SLB were further analyzed, no significant association was found between an orthodontist's bracket preference and (1) the length of time during which he used SLB (P = .1267) or (2) whether he used SLB as a marketing tool (P = .1342). There was, however, a significant association between bracket preference and three of the practitioner characteristics. These included the percentage of patients treated with SLB (P < .0001), the number of cases required to become accustomed to SLB (P < .0001), and the average appointment intervals for SLB (P < .0001). For example, practitioners who quickly became accustomed to SLB reported a significantly stronger preference for SLB.
These characteristics were further analyzed to determine their influence on bracket preference when considering each individual treatment factor (Table 2). For example, when evaluating overall treatment time, the practitioners who preferred SLB were those who treated a higher proportion of patients with SLB (association A), who quickly became accustomed to SLB (association B), and who reported longer appointment intervals for SLB (association D). The only treatment factors in which bracket preference was not influenced by any practitioner characteristics were the likelihood of extraction treatment and the frequency of emergency visits.
DISCUSSION
Most practitioners reported using SLB on either a low percentage or a high percentage of patients. This was demonstrated by the fact that 52% of respondents reported using SLB on fewer than 30% of patients, while 33% reported using SLB on the majority (70%–100%) of patients. These findings were similar to those of a 2009 survey16 of SLB users, in which 33% of the practitioners used SLB in all their cases and 11% used them in most cases. In the current survey, only 15% of orthodontists reported using SLB with a somewhat comparable frequency to use of CB. Overall, it was no surprise that practitioners who treated a higher proportion of patients with SLB were more likely to prefer SLB over CB for almost every treatment factor.
In addition, bracket preference was also shown to be significantly affected by the number of cases it took the practitioners to become accustomed to SLB and by the average appointment intervals for SLB and CB. Clinicians who quickly became accustomed to self-ligation were more likely to prefer SLB during all stages of treatment and were also more likely to report a shorter overall treatment time with SLB compared to CB.
The results of this study indicated a significant relationship between an orthodontist's appointment intervals and his bracket preference. Practitioners who reported longer appointment intervals (10 or more weeks) with SLB were more likely to prefer SLB for the majority of the treatment factors, including faster initial treatment progress, better oral hygiene, shorter adjustment appointments, and an overall shorter treatment time in comparison with CB. In addition, in this survey, a small proportion of practitioners reported using even longer intervals of 10 or more weeks for SLB. However, it is possible that longer appointment intervals could also result in longer treatment times. Even with longer appointment intervals for SLB, however, these practitioners were not more likely to indicate SLB as being more cost effective than CB. Overall, SLB were still found to be statistically significantly preferred by responding practitioners for shorter adjustment appointments, faster initial treatment progress, and preferred ligation method during the initial alignment stage of treatment.
Sixty-six percent of practitioners perceived initial treatment to progress faster with SLB than with CB. Likewise, 68% of practitioners indicated a preference for SLB during the initial alignment stage of treatment, compared to the 18% who preferred CB brackets for this treatment stage. Despite this significance, one orthodontist stated, “I have treated over 100 cases with SLB and have to say I saw no advantage in the speed of treatment.” Some other respondents indicated that “While overall treatment time may be similar between brackets, there are less total appointments when using SLB.” Studies17,18 on treatment efficiency have found that on average, patients treated with SLB finished treatment 4 to 6 months sooner and had four to seven fewer appointments than did patients with CB. However, a recent systematic review14 reported that currently prospective research considering the efficiency of orthodontic alignment and rate of space closure has consistently shown few differences between SLB and CB. One of these studies13 reported no overall difference between the two modes of ligation in terms of the time required to resolve mandibular crowding. Another study19 found no difference in the rate of en masse space closure between passive SLB and CB.
SLB have also been proposed20 to improve oral hygiene in patients as a result of decreased plaque retention with the elimination of elastomeric ligatures. In this study, orthodontists indicated a significant preference for SLB when comparing oral hygiene in patients with SLB and CB. However, several studies10,21,22 reported that there are no significant differences in oral hygiene between the patients bonded with CB and those bonded with SLB.
It has been argued23,24 that fewer extractions are required with SLB as a result of less incisor proclination and labial protrusion along with more significant posterior expansion. In this study the majority (61%) of orthodontists stated that bracket type made no difference in the extraction decision, which is consistent with the findings of other studies25,26 showing that the use of SLB and CB does not result in differences in incisor proclination and intercanine expansion.
With regard to long-term stability, the overwhelming majority of orthodontists (93%) perceived there was no difference in long-term stability and relapse potential between SLB and CB. Currently there is not sufficient evidence regarding the influence of bracket type on long-term stability, and future studies are required before any conclusions can be drawn.
A reported27 disadvantage of SLB has been the difficulty in finishing patients as a result of greater clearance or “slop” of the archwire in the slot of SLB. The majority of orthodontists (64%) from our survey indicated that they preferred CB over SLB during the finishing and detailing stages of treatment. This preference was clearly emphasized by many orthodontists who commented “It is difficult, if not impossible to finish cases with SLB. I have stripped and rebonded cases with CB to finish treatment” or that “CB are far superior during finishing.” Nevertheless, one practitioner stated the following: ”SLB have better quality of finish because you get to finishing wires faster and have more time to detail.”
Currently available SLB are clearly more expensive than most CB. A concern repeated by many orthodontists was whether any perceived increase in clinical efficiency with SLB justified the increased cost.15 From this study, orthodontists significantly preferred CB in this regard, with the majority of practitioners (68%) indicating that CB are more cost effective than SLB. In fact, the majority of orthodontists who discontinued use of SLB reported doing so mainly because they did not see significant enough advantages over CB brackets to make up for the increased cost. Practitioners stated, “I like SLB but the benefits, which are minimal, don't justify the expense,” and “I can't believe I was convinced that I should pay extra for SLB.”
In this study, as a result of antitrust issues the use of brand names was not allowed by the AAO (in exchange for providing the mailing lists for participants). Therefore, when assessing the results from this study, one must keep in mind that not all SLB are the same and that differing locking mechanisms (active vs passive) give them unique characteristics that could influence their performance with regard to several of the treatment factors evaluated in this study.
It must be noted that this study evaluated the perceptions of orthodontists regarding SLB and CB. It is likely that responses from advocates and detractors of SLB may have biased the results, since only 44% of orthodontists responded to the survey. Respondents would, of course, be expected to answer the questions in a way that was biased toward the bracket system they use in their practices. The conclusions of this study, therefore, are based on perceptions of clinicians and are not necessarily based on objective measures of performance.
CONCLUSIONS
The orthodontists participating in this study reported a perceived clinical difference between SLB and CB with regard to orthodontic treatment.
SLB were preferred by orthodontists more often than CB for the majority of the treatment factors evaluated.
The orthodontists' bracket preference was significantly influenced by the proportion of patients they treated with SLB, the number of cases it took them to become accustomed to SLB, and the average appointment intervals for both SLB and CB.
REFERENCES
- 1.Harradine N. W. T. Self-ligating brackets: where are we now. J Orthod. 2003;30:262. doi: 10.1093/ortho/30.3.262. [DOI] [PubMed] [Google Scholar]
- 2.Harradine N. W. The history and development of self-ligating brackets. Semin Orthod. 2008;14:5–18. [Google Scholar]
- 3.Birnie D, Harradine N. W. Introduction. Semin Orthod. 2008;14:1–4. [Google Scholar]
- 4.Rinchuse D. J, Miles P. G. Self-ligating brackets: present and future. Am J Orthod Dentofacial Orthop. 2007;132:216–222. doi: 10.1016/j.ajodo.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 5.Pizzoni L, Ravnholt G, Melsen B. Frictional forces related to self-ligating brackets. Eur J Orthod. 1998;20:283–291. doi: 10.1093/ejo/20.3.283. [DOI] [PubMed] [Google Scholar]
- 6.Cordasco G, Farronato G, Festa F, Nucera R, Parazzoli E, Grossi G. In vitro evaluation of the frictional forces between brackets and archwire with three passive self-ligating brackets. Eur J Orthod. 2009;31:643–646. doi: 10.1093/ejo/cjp054. [DOI] [PubMed] [Google Scholar]
- 7.Kim T, Kim K, Baek S. Comparison of frictional forces during the initial leveling stage in various combinations of self-ligating brackets and archwires with a custom-designed typodont system. Am J Orthod Dentofacial Orthop. 2008;133:187.e15. doi: 10.1016/j.ajodo.2007.08.013. [DOI] [PubMed] [Google Scholar]
- 8.Bednar J. R, Gruendeman G. W, Sandrik J. L. A comparative study of frictional forces between orthodontic brackets and arch wires. Am J Orthod Dentofacial Orthop. 1991;100:513–522. doi: 10.1016/0889-5406(91)70091-A. [DOI] [PubMed] [Google Scholar]
- 9.Redlich M, Mayer Y, Harari D, Lewinstein I. In vitro study of frictional forces during sliding mechanics of “reduced-friction” brackets. Am J Orthod Dentofacial Orthop. 2003;124:69. doi: 10.1016/s0889-5406(03)00238-5. [DOI] [PubMed] [Google Scholar]
- 10.Ehsani S, Mandich M, El-Bialy T, Flores-Mir C. Frictional resistance in self-ligating orthodontic brackets and conventionally ligated brackets. A systematic review. Angle Orthod. 2009;79:592–601. doi: 10.2319/060208-288.1. [DOI] [PubMed] [Google Scholar]
- 11.Yorita R. S. G. Comparison of self-ligating and conventional orthodontic bracket systems. J Dent Res. 2007:86. (Special Issue A): Abstract number 1918. [Google Scholar]
- 12.Pandis N, Strigou S, Eliades T. Maxillary incisor torque with conventional and self-ligating brackets: a prospective clinical trial. Orthod Craniofac Res. 2006;9:193–198. doi: 10.1111/j.1601-6343.2006.00375.x. [DOI] [PubMed] [Google Scholar]
- 13.Pandis N, Polychronopoulou A, Eliades T. Self-ligating vs conventional brackets in the treatment of mandibular crowding: a prospective clinical trial of treatment duration and dental effects. Am J Orthod Dentofacial Orthop. 2007;132:208–215. doi: 10.1016/j.ajodo.2006.01.030. [DOI] [PubMed] [Google Scholar]
- 14.Fleming P, Johal A. Self-ligating brackets in orthodontics. Angle Orthod. 2010;80:575–584. doi: 10.2319/081009-454.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marshall S. D, Currier G. F, Hatch N. E, Huong G. J, Nah H. D, Queens S. E, Shroff B, Southard T. E, Suri L, Turpin D. L. Reader's Forum Ask Us. Am J Orthod Dentofacial Orthop. 2010;138:128–131. doi: 10.1016/j.ajodo.2010.04.019. [DOI] [PubMed] [Google Scholar]
- 16.Sheridan J. The readers' corner. J Clin Orthod. 2009;43:577–579. [PubMed] [Google Scholar]
- 17.Harradine N. W. Self-ligating brackets and treatment efficiency. Clin Orthod Res. 2001;4:220–227. doi: 10.1034/j.1600-0544.2001.40406.x. [DOI] [PubMed] [Google Scholar]
- 18.Eberting J. J, Straja S. R, Tuncay O. C. Treatment time, outcome, and patient satisfaction comparisons of Damon and conventional brackets. Clin Orthod Res. 2001;4:228–234. doi: 10.1034/j.1600-0544.2001.40407.x. [DOI] [PubMed] [Google Scholar]
- 19.Miles P. Self-ligating vs conventional twin brackets during en-masse space closure with sliding mechanics. Am J Orthod Dentofacial Orthop. 2007;132:223–225. doi: 10.1016/j.ajodo.2007.04.028. [DOI] [PubMed] [Google Scholar]
- 20.Pandis N, Vlachopoulos K, Polychronopoulou A, Madianos P, Eliades T. Periodontal condition of the mandibular anterior dentition in patients with conventional and self-ligating brackets. Orthod Craniofac Res. 2008;11:211–215. doi: 10.1111/j.1601-6343.2008.00432.x. [DOI] [PubMed] [Google Scholar]
- 21.Henao S. P, Kusy R. P. Evaluation of the frictional resistance of conventional and self-ligating bracket designs using standardized archwires and dental typodonts. Angle Orthod. 2004;74:202–211. doi: 10.1043/0003-3219(2004)074<0202:EOTFRO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 22.Burrow S. J. Friction and resistance to sliding in orthodontics: a critical review. Am J Orthod Dentofac Orthop. 2009;135:442–447. doi: 10.1016/j.ajodo.2008.09.023. [DOI] [PubMed] [Google Scholar]
- 23.Birnie D. J. The Damon Passive Self-Ligating Appliance System. Semin Orthod. 2008;14:19–35. [Google Scholar]
- 24.Chen S. S, Greenlee G. M, Kim J. E, Smith C. L, Huang G. J. Systematic review on self-ligating brackets. Am J Orthod Dentofacial Orthop. 2010;137:e1–e8. doi: 10.1016/j.ajodo.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 25.Fleming P, DiBiase A, Sarri G, Lee R. Comparison of mandibular arch changes during alignment and leveling with 2 preadjusted edgewise appliances. Am J Orthod Dentofacial Orthop. 2009;136:340–347. doi: 10.1016/j.ajodo.2007.08.030. [DOI] [PubMed] [Google Scholar]
- 26.Pandis N, Polychronopoulou A, Makou M, Eliades T. Mandibular dental arch changes associated with treatment of crowding using self-ligating and conventional brackets. Eur J Orthod. 2009;Epub:1–6. doi: 10.1093/ejo/cjp123. [DOI] [PubMed] [Google Scholar]
- 27.Harradine N. W, Birnie D. J. The clinical use of Active self-ligating brackets. Am Orthod Dentofac Orthop. 1996;109:319–328. doi: 10.1016/s0889-5406(96)70155-5. [DOI] [PubMed] [Google Scholar]