Abstract
Objective
This study investigated trends in hospital utilization by patients with schizophrenia during the first wave of the COVID-19 outbreak in Korea.
Methods
The Prophet algorithm was used to predict the monthly number of patients with schizophrenia in 2020 based on medical insurance data between 2010 and 2019. The projected expectations were compared with the actual number of patients receiving outpatient and inpatient treatment each month in the first half of 2020. We conduct interrupted time series analyses of short-term data to determine the significance of recent changes in the trend of hospital visits by patients with schizophrenia.
Results
The prediction model showed that the actual number of patients receiving treatment each month during the early COVID-19 outbreak decreased by up to 3.6% compared to the projected expectations. The interrupted time series model also revealed a significant change in hospital utilization compared to the year before the onset of COVID-19 in Korea (F = 8.961, p = 0.010).
Conclusion
This suggests that many patients with schizophrenia were not receiving adequate treatment during the COVID-19 outbreak. A strategy should be developed to keep treating patients with schizophrenia during the COVID-19 pandemic.
Keywords: COVID-19, Forecasting, Interrupted time series analysis, Schizophrenia
INTRODUCTION
Continuity of care is essential to prevent relapse and to ensure a better outcome in patients with schizophrenia [1]. In most cases, it is necessary to maintain antipsychotic treatment to lower the risk of relapse. Long-term rehabilitation with community mental health services can also help to improve negative symptoms and social dysfunction. In this respect, accessible mental health care is a prerequisite for the recovery of patients with schizophrenia.
Since early 2020, the novel coronavirus pandemic, officially designated the coronavirus disease 2019 (COVID-19) by the World Health Organization, has introduced huge changes to people’s daily lives worldwide [2]. Stringent public health measures have been implemented to curtail the spread of COVID-19, including quarantining those in close contact with a patient or overseas entrant, restricting public gatherings, closing schools, and requiring the wearing of face masks in public facilities. People fearful about contracting COVID-19 have restricted their daily activities, such as meeting family and friends, exercising, and visiting hospitals.
Given these restricted activities, mental health experts are concerned about the worsening of pre-existing psychiatric conditions in people with severe mental illness during the COVID-19 outbreak [3]. Specifically, it is necessary to evaluate the impact of the COVID-19 outbreak on mental health service delivery to patients with schizophrenia [4]. There is concern that patients with schizophrenia were reluctant to visit the hospital or did not come to the scheduled visits during this period due to fear of infection and social distancing. Therefore, this study investigated whether hospital visits by and admissions of patients with schizophrenia decreased during the early COVID-19 outbreak using time-series analysis based on National Health Insurance claims data.
METHODS
We collected the number of patients receiving outpatient and inpatient treatment for schizophrenia, schizotypal disorder, delusional disorders, acute and transient psychotic disorders, schizoaffective disorder, and other and unspecific nonorganic psychosis as primary diagnosis codes (F20, F21, F22, F23, F25, F28, and F29, respectively) each month between January 2010 and July 2020 using the Health Insurance Review and Assessment Service data provided by the Health Insurance Big Data Open System [5]. This study included only patients covered by the National Health Insurance, and not by Medical Aid or uninsured medical benefits. This study was approved by the Institutional Review Board of Chonnam National University Hospital (IRB number: CNUH-EXP-2021-047).
We used Facebook Prophet, a time series forecasting procedure based on an additive model that fits non-linear trends with seasonality and holiday effects [6]. We constructed a Prophet forecasting model based on 120 observations between 2010 and 2019. Yearly seasonality including the holiday effects of Korean New Year’s Day and Korean Thanksgiving was also modeled with extra regressors. Prediction was performed with the data frame for a 12-month forecast period. We visualized the predicted values with 95% uncertainty intervals for 2020 together with the actual values up to July 2020.
In addition, to determine whether there was any significant change in hospital utilization before and after the COVID-19 outbreak, we conducted interrupted time series analyses. Considering very short-term observations after the COVID-19 outbreak, we employed the ‘its.analysis’ package, a modelling technique for short time series data based on a Type II Sum Squares ANCOVA lagged dependent variable model [7]. This model was applied to data collected 12 months before and 6 months after the February 2020 beginning of the COVID-19 outbreak.
The p values less than 0.05 were considered statistically significant. All analyses were conducted using R (ver. 4.0.3; R Development Core Team, Vienna, Austria).
RESULTS
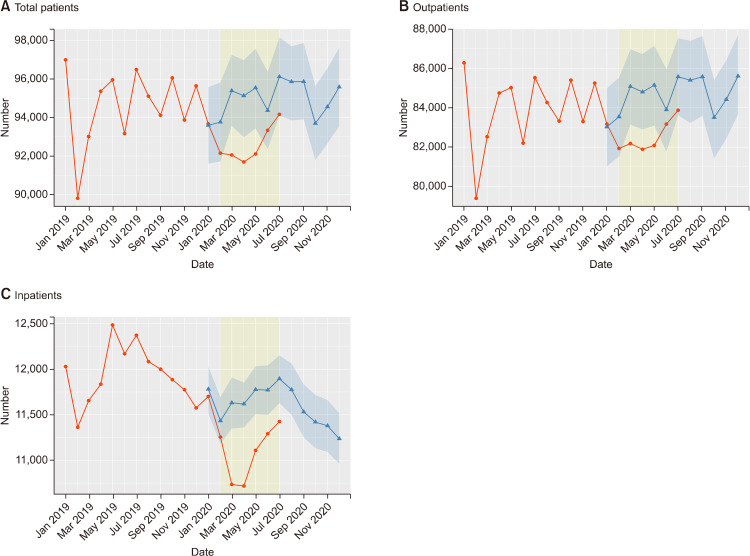
Figure 1 shows the trends in hospital utilization by patients with schizophrenia between January 2019 and July 2020 in Korea. The actual number of patients began to deviate significantly from the projected expectations in March, and it was about 3.6% lower than the projected expectations between April and May (Table 1). Then, in June, the number of patients increased and recovered to within the expected range. We observed similar trends in the numbers of outpatients and inpatients during this period (Fig. 1).
Fig. 1.
The Actual (circle dots) and predicted (triangle dots) number of patients (A) with schizophrenia receiving outpatient (B) and inpatient (C) treatment in a month between 2019 and 2020 in Korea. The predicted values were calculated from forecasting models based on data from 2010 to 2019.
Table 1.
The actual and predicted number of patients with schizophrenia receiving outpatient and inpatient treatment in a month during the early COVID-19 outbreak in Korea
| Date | February 2020 | March 2020 | April 2020 | May 2020 | June 2020 | July 2020 |
|---|---|---|---|---|---|---|
| Total patients | ||||||
| Actual | 92,145 | 92,054 | 91,691 | 92,105 | 93,341 | 94,170 |
| Predicted | 93,767 (91,718−95,833) | 95,398 (93,572−97,267) |
95,136 (92,984−96,999) |
95,548 (93,432−97,576) |
94,370 (92,365−96,373) |
96,126 (94,109−98,186) |
| Outpatients | ||||||
| Actual | 81,933 | 82,183 | 81,892 | 82,088 | 83,168 | 83,869 |
| Predicted | 83,538 (81,529−85,524) |
85,078 (83,146−86,955) |
84,796 (82,896−86,722) |
85,141 (83,095−87,139) |
83,897 (81,778−85,952) |
85,568 (83,617−87,528) |
| Inpatients | ||||||
| Actual | 11,255 | 10,735 | 10,718 | 11,109 | 11,292 | 11,425 |
| Predicted | 11,433 (11,185−11,693) |
11,631 (11,349−11,910) |
11,618 (11,362−11,853) |
11,776 (11,506−12,032) |
11,771 (11,498−12,042) |
11,895 (11,628−12,152) |
Data are shown as number or 95% uncertainty interval.
The number of total patients does not match the sum of the numbers of outpatients and inpatients due to the record overlap of outpatients and inpatients.
According to the interrupted time series models, significant changes in hospital visits by, and admissions of, patients with schizophrenia occurred after February 2020 compared to the trend over the previous 12 months (total patients: F = 8.961, p = 0.010; outpatients: F = 6.339, p = 0.025; inpatients: F = 6.538, p = 0.023).
DISCUSSION
In Korea, after the first patient with COVID-19 was identified on January 20, 2020, the number of confirmed patients began to increase rapidly from mid-February [8]. By the end of April, when the accumulated number of confirmed cases exceeded 10,000 nationwide, the first wave of the COVID-19 outbreak had passed in Korea. Subsequently, the spread of COVID-19 seemed to have been controlled. However, in mid-August, the second wave of the COVID-19 outbreak started. The number of confirmed cases at that time was lower in Korea than in European and American countries. However, in Korea, in-hospital infections of Middle East Respiratory Syndrome coronavirus (MERS-CoV) had occurred in 2015 and patients admitted to an oriental medicine hospital in Daegu were the first confirmed cases in the first wave of the COVID-19 outbreak [8,9]. Consequently, patients with severe mental illness and their caregivers may have been reluctant to visit hospitals during the COVID-19 outbreak, despite worsening symptoms and running out of medication. A few psychiatric hospitals actually closed due to nosocomial COVID-19 infection. Unfortunately, the first official reported death from COVID-19 in Korea was a hospitalized patient with chronic schizophrenia [8].
This study investigated the change in hospital utilization by patients with schizophrenia after the COVID-19 outbreak began in Korea. Until 2019, the number of outpatients with schizophrenia in Korea had been increasing gradually, while the number of hospitalized patients had been decreasing [10]. Considering the non-linear trend and seasonal variation in hospital utilization, it is inappropriate to compare the number of patients treated in early 2020 with the number of patients in previous years directly. Therefore, we tried to determine by how much the actual number of patients had decreased after the COVID-19 outbreak compared to the number of patients in 2020, predicted by a forecasting model.
We observed that the numbers of patients with schizophrenia receiving outpatient and inpatient treatment per month after the first wave of the COVID-19 outbreak decreased significantly compared to the projected expectations. Our interrupted time series model also found significant changes in the recent trend. This suggests that the COVID-19 outbreak was a major changing point in the hospital utilization trends of patients with schizophrenia. Although social lockdown and stay-at-home orders were not enforced in Korea, the decline in hospital utilization might be attributed to reluctance to visit public places due to fear of infection, service limitation at community mental health centers, and the complicated process of psychiatric hospitalization for infection prevention [11]. From the beginning of the COVID-19 outbreak, mental health experts were concerned about limiting access to mental healthcare services during the outbreak [3,4]. A survey of mental health institutions reported a drastic reduction in the number of beds and admissions to psychiatric wards during this period [12]. Patients were also concerned about the disruption of mental health services and running out of their medications [13]. In line with this, our findings show how much the COVID-19 outbreak hindered hospital care of patients with schizophrenia numerically.
In this study, the rapid decline in hospital utilization by patients with schizophrenia might have caused many patients undergoing treatment to have stopped taking medication or prevented untreated patients from being evaluated or treated, despite their worsening symptoms, during the first wave of the COVID-19 outbreak. Fortunately, the declining trend recovered in June when the first wave subsided. However, the accessibility and continuity of mental health care may have been compromised significantly in Korea during the ongoing COVID-19 outbreak [14]. Moreover, limited telemedicine may be a major obstacle to healthcare delivery for patients with severe mental illness in Korea [15,16]. As a result, the delay or interruption in accessing care during the COVID-19 outbreak may have led not only to further deterioration of the mental and physical health of patients with schizophrenia but also to serious problems, such as violence in society [4].
This study had some methodological limitations. First, it did not include patients covered by Medical Aid; annually it covers close to 60% of the patients covered by National Health Insurance [17]. Second, due to the wide range of selected diagnosis codes, this study may have included some patients who did not actually have schizophrenia. Third, this study used only one forecasting procedure: Prophet. Additional analyses are needed using other forecasting techniques such as autoregressive integrated moving average.
In conclusion, we found a rapid decrease in hospital utilization by patients with schizophrenia during the early COVID-19 outbreak in Korea, below the projected expectations. This suggests that many patients were not receiving adequate treatment during that period. Mental health professionals should carefully monitor the continuing treatment of patients with schizophrenia and strengthen community mental health services during the COVID-19 pandemic.
Footnotes
Funding
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI19C0481, HC19C0316).
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Conceptualization: Sung-Wan Kim, Seunghyong Ryu. Data acquisition: Hee Jung Nam, Seon-Hwa Baek. Formal analysis: Seunghyong Ryu, Min Jhon. Funding: Sung-Wan Kim. Supervision: Jae-Min Kim. Writing—original draft: Sung-Wan Kim, Seunghyong Ryu, Hee Jung Nam. Writing—review & editing: Jae-Min Kim, Sung-Wan Kim.
References
- 1.Anderson KK, Norman R, MacDougall A, Edwards J, Palaniyappan L, Lau C, et al. Effectiveness of early psychosis intervention: comparison of service users and nonusers in population-based health administrative data. Am J Psychiatry. 2018;175:443–452. doi: 10.1176/appi.ajp.2017.17050480. [DOI] [PubMed] [Google Scholar]
- 2.Kim M, Park IH, Kang YS, Kim H, Jhon M, Kim JW, et al. Comparison of psychosocial distress in areas with different COVID-19 prevalence in Korea. Front Psychiatry. 2020;11:593105. doi: 10.3389/fpsyt.2020.593105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim SW, Su KP. Using psychoneuroimmunity against COVID-19. Brain Behav Immun. 2020;87:4–5. doi: 10.1016/j.bbi.2020.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kozloff N, Mulsant BH, Stergiopoulos V, Voineskos AN. The COVID-19 global pandemic: implications for people with schizophrenia and related disorders. Schizophr Bull. 2020;46:752–757. doi: 10.1093/schbul/sbaa051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Healthcare Bigdata Hub, author. Disease statistics [Internet] Health Insurance Review & Assessment Service; Wonju: 2021. [cited 2021 Mar 25]. https://opendata.hira.or.kr/home.do. [Google Scholar]
- 6.Taylor S, Letham B. R package version 0.6.1 [Internet] MIT; Cambridge: 2020. prophet: Automatic Forecasting Procedure 2020. [Google Scholar]
- 7.English P. The its.analysis R package- modelling short time series data [Internet] SSRN. 2019. Jun 6, [cited 2021 Mar 25]. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3398189.
- 8.Korean Society of Infectious Diseases; Korean Society of Pediatric Infectious Diseases; Korean Society of Epidemiology; Korean Society for Antimicrobial Therapy; Korean Society for Healthcare-associated Infection Control and Prevention; Korea Centers for Disease Control and Prevention, author. Report on the epidemiological features of Coronavirus disease 2019 (COVID-19) outbreak in the Republic of Korea from January 19 to March 2, 2020. J Korean Med Sci. 2020;35:e112. doi: 10.3346/jkms.2020.35.e112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ki M. 2015 MERS outbreak in Korea: hospital-to-hospital transmission. Epidemiol Health. 2015;37:e2015033. doi: 10.4178/epih/e2015033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Go DS, Shin KC, Paik JW, Kim KA, Yoon SJ. A review of the admission system for mental disorders in South Korea. Int J Environ Res Public Health. 2020;17:9159. doi: 10.3390/ijerph17249159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ryu S, Park IH, Kim M, Lee YR, Lee J, Kim H, et al. Network study of responses to unusualness and psychological stress during the COVID-19 outbreak in Korea. PLoS One. 2021;16:e0246894. doi: 10.1371/journal.pone.0246894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carpiniello B, Tusconi M, Zanalda E, Di Sciascio G Di Giannantonio M; Executive Committee of The Italian Society of Psychiatry, author. Psychiatry during the COVID-19 pandemic: a survey on mental health departments in Italy. BMC Psychiatry. 2020;20:593. doi: 10.1186/s12888-020-02997-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Costa M, Pavlo A, Reis G, Ponte K, Davidson L. COVID-19 concerns among persons with mental illness. Psychiatr Serv. 2020;71:1188–1190. doi: 10.1176/appi.ps.202000245. [DOI] [PubMed] [Google Scholar]
- 14.World Health Organization, author. The impact of COVID-19 on mental, neurological and substance use services: results of a rapid assessment. World Health Organization; Geneva: 2020. [Google Scholar]
- 15.Kim JW, Stewart R, Kang SJ, Jung SI, Kim SW, Kim JM. Telephone based Interventions for psychological problems in hospital isolated patients with COVID-19. Clin Psychopharmacol Neurosci. 2020;18:616–620. doi: 10.9758/cpn.2020.18.4.616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oh JY, Park YT, Jo EC, Kim SM. Current status and progress of telemedicine in Korea and other countries. Healthc Inform Res. 2015;21:239–243. doi: 10.4258/hir.2015.21.4.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cho SJ, Kim J, Kang YJ, Lee SY, Seo HY, Park JE, et al. Annual prevalence and incidence of schizophrenia and similar psychotic disorders in the Republic of Korea: a national health insurance data-based study. Psychiatry Investig. 2020;17:61–70. doi: 10.30773/pi.2019.0041. [DOI] [PMC free article] [PubMed] [Google Scholar]