Abstract
Ischemia in the absence of obstructive coronary artery disease (INOCA) is an increasingly recognized cause of angina, which is more commonly diagnosed in women. Coronary microvascular dysfunction (CMD), or the abnormal dilation and constriction of the small vessels of the heart, is one such etiology of INOCA. This review discusses coronary microvascular pathophysiology, considerations for invasive coronary function testing (CFT) and non-invasive diagnostic modalities, implications for management and remaining knowledge gaps.
Keywords: Coronary Microvascular Dysfunction, Coronary Function Testing, Non-Obstructive Coronary Artery Disease, INOCA, Ischemia
Introduction
It is estimated that one-half to two-thirds of women with symptoms of angina who undergo coronary angiography for suspected ischemic heart disease have no obstructive coronary artery disease.1, 2 This condition, characterized by symptoms and objective signs of Ischemia in the setting of Non-Obstructive Coronary Artery disease (less than 50% stenosis on diagnostic angiography), is known as INOCA.3 Recent studies have estimated that in total, there are at least 3 to 4 million patients with stable INOCA in the United States.4 Prevalence continues to increase as there is growing clinical recognition of this condition and utilization of diagnostic modalities for microvascular dysfunction.
Coronary microvascular dysfunction (CMD) and vasospasm of the epicardial arteries are the two most common causes of INOCA.5 In studies, nearly 50% of individuals with INOCA have been found to have abnormal vasomotor behavior of the coronary microvasculature.6 While the condition is more common among women, CMD has also been shown to be prevalent in men, with a recent study finding 60% of males and 66% of females with non-obstructive CAD to have CMD on invasive testing.7, 8
Historically, patients with INOCA were thought to have good prognosis and relatively low incidence of major adverse cardiac events (MACE). However, this understanding has since been refuted by many studies showing that patients with INOCA have elevated risk for cardiovascular events including acute coronary syndrome, heart failure hospitalizations, stroke and death.9
The Women’s Ischemia Syndrome Evaluation (WISE) Study was initiated by the National Institutes of Health-National Heart, Lung and Blood Institute in 1996 to investigate women with signs and symptoms of ischemia.10 To date, the evaluation has followed more than 900 women for a median follow up of 9.5 years after clinically indicated coronary angiography. Of these women, 551 were found to have no obstructive coronary artery disease (CAD). Analysis of this cohort found that INOCA was associated with a 2.5% rate of MACE, including death, nonfatal myocardial infarction, nonfatal stroke and heart failure hospitalization at 5-year follow up.11 Angina hospitalizations continued at relatively constant rates at longer-term follow-up of 9.1 years.12 Furthermore, women with stable INOCA and non-obstructive CAD had 10-year all-cause death and cardiac death rates of 17% and 11% respectively, compared to 10% and 6% in women with normal coronaries.13 The WISE study has also demonstrated that females with CMD are at increased risk for progression to obstructive CAD.14
In addition to adverse clinical outcomes, CMD and persistent anginal symptoms affect quality of life, limit exercise capacity and may contribute to unnecessary testing, costs and frequent visits to healthcare providers.15 Thus, early diagnosis and intervention are crucial.
At present, invasive coronary function testing (CFT) is the gold standard to diagnose both CMD as well as coronary vasospasm. CFT identifies those at higher risk of MACE and facilitates medical management accordingly.16 This review will discuss the coronary microvasculature physiology, CFT and other non-invasive diagnostic modalities, treatment options, as well as knowledge gaps and future directions regarding CMD.
Tiny Vessels, Big Effects
The coronary microvasculature consists of the smaller vessels of the heart including the pre-arterioles (100–500 μm) and intracardiac arterioles (< 100 μm) (Figure 1).17 These arterioles are regulated by different mechanisms that work in tandem to modulate blood flow to the heart: (1) larger proximal arterioles use endothelial-dependent vasodilatory mechanisms by which an increase in coronary blood flow leads to vasodilation and a decrease in blood flow leads to vasoconstriction, (2) medium-sized arterioles have vascular smooth muscle cell stretch receptors to detect intraluminal pressure and (3) the smallest distal arterioles are regulated by local metabolic activity.18
Figure 1.
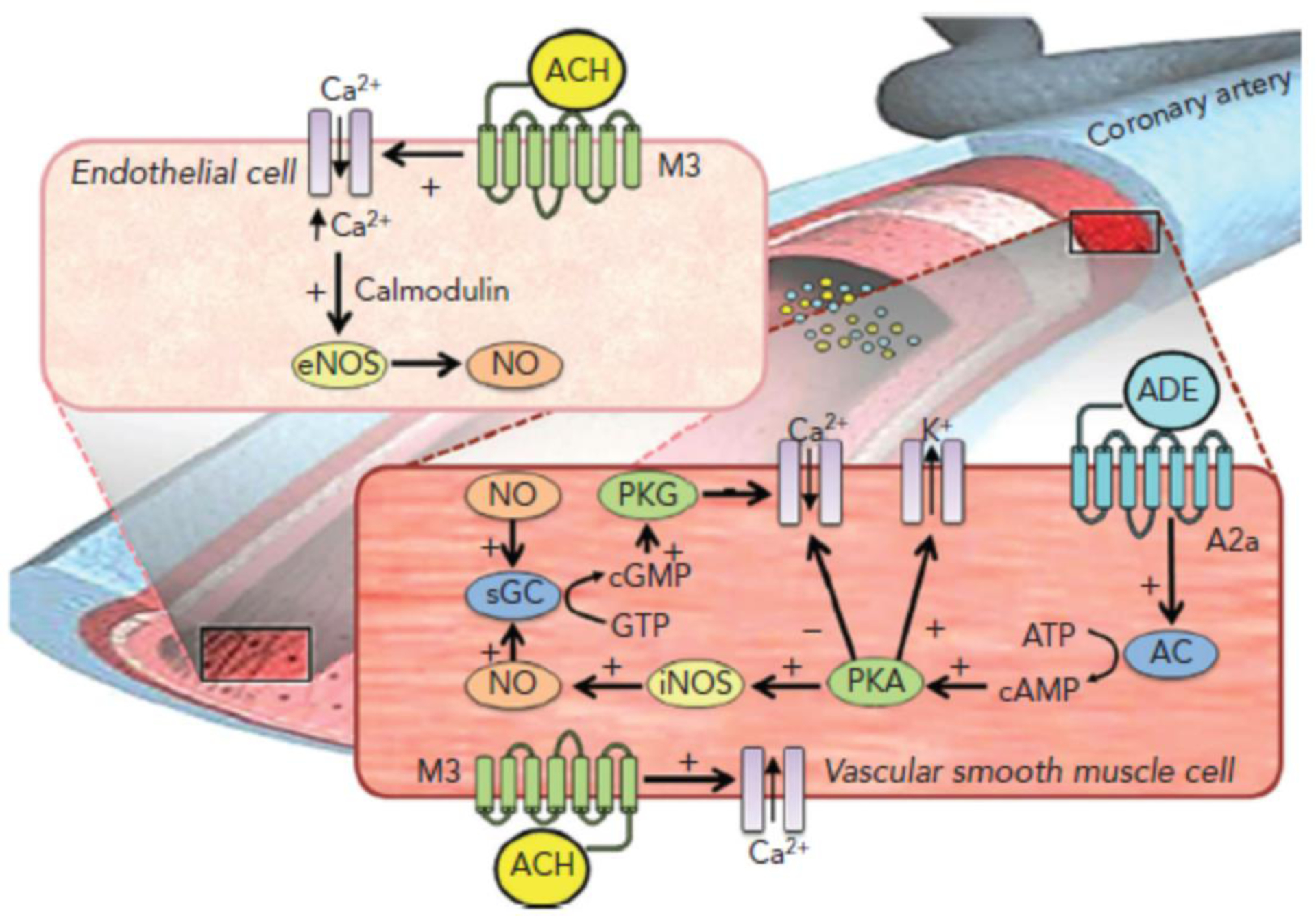
Schematic demonstrating the influence of acetylcholine and adenosine on the smooth muscle of the coronary vasculature. Acetylcholine binds to the muscarinic receptor, stimulating the release of calcium into the vascular smooth muscle cell, which drives both nitric oxide formation for vasodilation as well as contraction for vasoconstriction. Adenosine stimulates the conversion of adenosine triphosphate to cyclic adenosine monophosphate, leading to inhibition of calcium influx and induction of nitric oxide formation, both of which result in vasodilation. AC = adenylate cyclase; ACh = acetylcholine; ADE = adenosine; ATP – adenosine triphosphate; cAMP = cyclic adenosine monophosphate; cGMP = cyclic guanosine monophosphate; eNOS = endothelial nitric oxide synthase; GTP = guanosine triphosphate; iNOS = inducible nitric oxide synthase; M3 = muscarinic receptor’ NO = nitric oxide; PKA protein kinase activation; PKG = guanosine monophosphate-dependent protein kinase; sGC = soluble guanylate-cyclase; Ca+ = calcium; A2a = adenosine receptor. Adapted from Ref 14 with permissions.
The endothelium, or the layer of cells lining the arteries and arterioles, play a vital role in regulating blood flow delivery to the myocardium.19 A healthy endothelium promotes vasodilation, antioxidant effects, inhibition of smooth muscle cell proliferation and anticoagulant effects. Furthermore, the cells act to regulate inflammation and also serve as a barrier to potentially toxic materials.20 An imbalance of nitric oxide consumption is thought to be the primary driver of dysfunction, leading to an inability to properly dilate and subsequent ischemia.21 Dysfunction of the endothelium is a principal contributor to both macro- and microvascular coronary dysfunction and also thought to be a key player in the development of plaque progression and atherosclerosis.19
CMD may be characterized by heightened sensitivity of the small vessels to vasoconstrictor stimuli and/or decreased microvascular vasodilator capacity.22 In healthy vessels, adenosine, acetylcholine and nitroglycerin induce vasodilation.23 However, in CMD, the microvasculature may exhibit a blunted vasodilatory response to one or more of these agents. Coronary flow reserve (CFR), or the ratio of coronary blood flow at maximal dilation in response to intracoronary adenosine from baseline, is impaired in patients with CMD. In the setting of endothelial dysfunction, acetylcholine may induce paradoxical vasoconstriction and micro- or macrovascular vasospasm in compromised vessels. Nitroglycerin response is used to evaluate for non-endothelial dependent macrovascular function.
Risk Factors and Clinical Presentation
Traditional cardiovascular risk factors including hypertension, hyperlipidemia, advanced age, obesity, smoking, and diabetes have been found to be associated with CMD.22, 24 Aging is associated with an increase in arterial wall stiffness, medial thickening and lumen enlargement that results in an increase in pulse pressure and hypertrophy of arteries –ultimately contributing to endothelial dysfunction.25 Studies have demonstrated reduced CFR in diabetics, thought to be a consequence of the microvascular inflammation that also leads to diabetic retinopathy and nephropathy.26 Additionally, smokers and patients with chronic inflammatory conditions such as rheumatoid arthritis and systemic lupus erythematous have also been found to have lower CFR, with a 21% reduction observed amongst smokers.27, 28 There is increasing evidence that women who have history of adverse pregnancy outcomes including preeclampsia, gestational hypertension or diabetes may have an increased risk of microvascular dysfunction.14
Symptoms include chest discomfort, dyspnea and reduced exercise tolerance, with some patients having angina that persists after cessation of exertion.29 As nitroglycerin acts preferentially to dilate larger vessels of the heart and has little effect on the smaller arterioles, patients with CMD may not have symptom relief with its administration.30 Objective clinical evidence of myocardial ischemia can include elevated troponin, ST-segment or imaging abnormalities at rest or with stress.31
Coronary Function Testing
When is CFT Appropriate?
Testing for CMD should be considered for patients with persistent symptoms and objective signs suggestive of myocardial ischemia despite absence of obstructive CAD (<50% coronary artery diameter reduction).32 Prior to invasive testing, patients should be evaluated for alternative diagnostic explanations including hyperthyroidism, anemia, hypertensive urgency or substance abuse.
For patients with persistent symptoms but angiographically normal coronary arteries or non-obstructive CAD, the 2019 European Society of Cardiology guidelines recommend consideration of guidewire-based CFR measurements (Class 2A recommendation) and consideration of intracoronary acetylcholine for assessment of spasm (Class 2B recommendation).33 These guidelines also recommendation consideration of non-invasive transthoracic Doppler of the left anterior descending artery, cardiac magnetic resonance imaging and positron emission tomography for CFR measurement (Class 2B recommendation).
The decision to proceed with invasive CFT depends on a variety of considerations including local hospital practices, patient preference, goals and availability of CFT and other non-invasive diagnostic modalities. Discussion with the patient includes a comprehensive individualized evaluation, in order to determine whether there is more benefit than risk. In patients with prior myocardial infarction or high suspicion for vasospasm, invasive CFT with acetylcholine provocation testing is preferable due to its ability to delineate pathways and elicit spasm.
Procedure
CFT is an angiographic procedure to evaluate both endothelial and non-endothelial dependent macro- and micro-vasculature response to vasoactive agents (Figure 2). Following a diagnostic angiogram to exclude obstructive epicardial disease, myocardial bridging and other coronary anomalies, adenosine, acetylcholine and nitroglycerin are then administered sequentially to evaluate for microvascular function, vasospasm and smooth muscle response.
Figure 2.
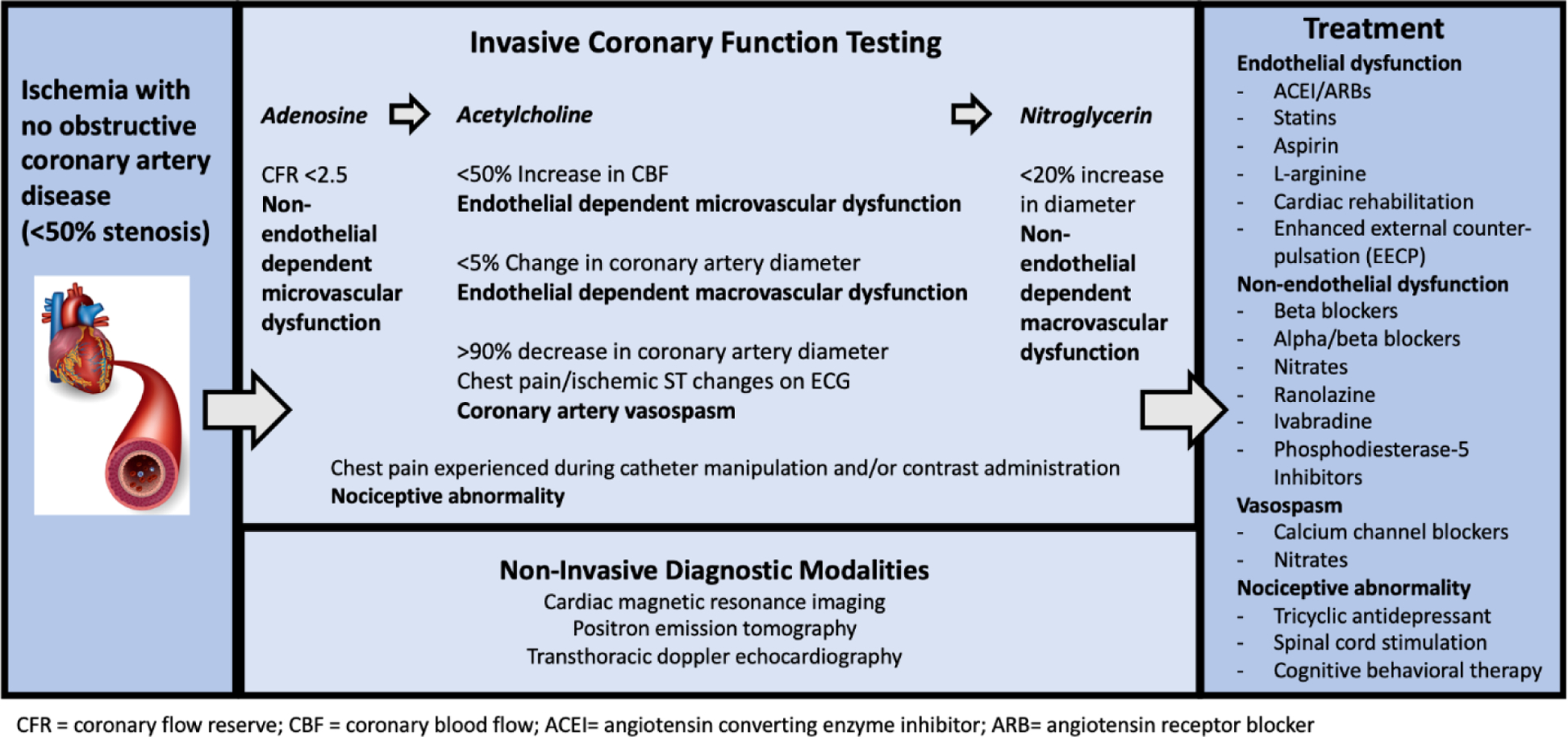
Coronary Microvascular Dysfunction: Diagnosis and Treatment
The functional testing involves insertion of a guiding catheter and positioning of a Doppler wire into the coronary artery to be studied. Typically, this evaluation is done in the left anterior descending artery, but testing can also be performed in the left circumflex and right coronary arteries. First, an intracoronary injection of adenosine is given to assess non-endothelial dependent dysfunction. Flow reserves are measured before and following administration. Graded doses are used to achieve maximum hyperemia. A CFR < 2.5 is diagnostic for non-endothelial dependent microvascular dysfunction. When interpreting CFR results, it is important to note that this measurement has been shown to be a continuous predictor of MACE, similar to blood pressure and low-density lipoprotein cholesterol levels.11 It has also been shown that stable INOCA patients with a CFR<2 have more MACE in both females and males.8 In the WISE study, it was shown that a CFR < 2.32 best predicted adverse outcomes in women.11
Next, acetylcholine is given to assess for endothelial-dependent dysfunction. It is given in increasing concentrations to stimulate the release of nitric oxide. An increase in coronary blood flow <50% is diagnostic of endothelial-dependent microvascular dysfunction. Vessel diameter response is measured and a change of <5% is diagnostic for endothelial-dependent macrovascular dysfunction. A higher dose of acetylcholine is given to assess for coronary spasm. Coronary vasospasm is defined as >90% diameter reduction with chest pain and ischemic ST changes. Lastly, nitroglycerin is administered to test macrovascular function. A change in diameter less than 20% is indicative of abnormal smooth muscle reactivity and non-endothelial dependent macrovascular dysfunction (Figure 2). A detailed description of the CFT protocol and methods is provided in Appendix A.
Heightened pain sensitivity at any point in the procedure, demonstrated by chest pain during catheter manipulation and/or contrast administration is suggestive of nociceptive abnormality. It is thought to be associated with altered afferent neuronal pathways, change in cerebral cortical activation or reduced endogenous opioid release.34
CFT has been shown to be overall safe and effective, with the WISE study reporting serious adverse events to be low (0.7%).35 These low event rates were observed at centers of excellence. A prospective multicenter study has reported cases of coronary artery dissection, ST-elevation myocardial infarction associated with vasospasm, transient air micro-embolism and deep venous thrombosis—but overall peri-procedural adverse event rates have been found to be low at 1.4%.35 As the reactivity testing prolongs the length of angiography, precautions must be taken for those at higher risk of contrast-induced nephropathy.36 Adenosine should be avoided or used with caution in patients with history of asthma, as it may contribute to bronchospasm.
Other Diagnostic Modalities
Pharmacologic stress testing using positron emission tomography or cardiac magnetic resonance imaging, transthoracic Doppler echocardiography and empiric therapy can alternatively be used to assess for CMD. Positron emission tomography utilizes various radioactive tracers at rest and with vasodilator-stress to quantify absolute myocardial blood flow and detect regional variations suggestive of CMD. Computed tomography can also be concurrently performed, to determine coronary artery calcium score for risk stratification.37
Stress cardiac magnetic resonance imaging is a tool with high diagnostic accuracy, low ionizing radiation and high spatial resolution, which can also be used to quantify myocardial perfusion reserve index and assess for late gadolinium enhancement, a signal of myocardial damage and scar, associated with vasomotor dysfunction.38 The presence of scar is useful for risk stratification. This modality is more widely available than the invasive CFT.
Doppler echocardiogram of the left anterior descending artery can be used to quantify coronary blood flow. It has been demonstrated that CFR calculated by this procedure correlates well with measurements obtained through positron emission tomography and invasive techniques.39 This method is more inexpensive and accessible than other techniques, lacks ionizing radiation, but limits evaluation to that of the left anterior descending artery.
Implementation and assessment of the response to an empiric trial of therapy is another informative approach. For example, for sporadic angina responsive to nitrates suggestive of vasospasm, providers can implement and monitor symptomatic response to a trial of calcium channel blockade. For those with comorbid hyperlipidemia and hypertension and high pre-test probability for endothelial dysfunction and CMD, anginal response to the initiation of statins and angiotensin converting enzyme inhibitors (ACEI), respectively, can be monitored. This may be a suitable approach for patients who are hesitant to proceed with invasive testing or those with contraindications or allergies precluding diagnostic procedures.
Treatment
Identification of the affected pathway(s) by CFT guides selection of the best targeted therapeutic approaches (Figure 2).40 The CorMicA trial randomized patients with INOCA to stratified medical therapy guided by CFT results versus standard care (control blinded to interventional diagnostic procedure results) and found that those patients receiving stratified medical therapy had improved angina and quality of life.41 It is important to note that treatment strategies remain unclear and non-standardized, largely due to a lack of evidence-based guidelines.
Non-endothelial-dependent dysfunction: Non-endothelial CMD is treated with medications targeting ischemia. Beta and alpha/beta blockers reduce frequency and severity of angina and improve CFR.42 They act by reducing myocardial oxygen consumption and increasing diastolic filling time. Both short acting and long acting nitrates help angina by promoting vasodilation and reducing preload.42 Ranolazine and ivabradine can be considered in patients with refractory angina with contraindications to traditional anti-anginal medications as they have less hemodynamic effect. More recently, phosphodiesterase-5 inhibitors have been used to drive vasodilation in CMD.
Endothelial Dysfunction: Treatment options aimed at both macro- and micro-vascular dysfunction are similar to those targeting atherosclerotic disease, including ACEI, angiotensin receptor blockers, statins and low-dose aspirin. High-dose quinapril has been associated with reduced angina among women with CMD, likely by benefiting vascular inflammation.43 Statins have been demonstrated to improve exercise tolerance and reduce angina due to anti-inflammatory effects on endothelial function.44 Aspirin is recommended due to the observation that even in patients with no significant plaque burden seen on angiography, a majority of patients with CMD were demonstrated to have coronary atherosclerosis when evaluated by intravascular ultrasound.45 L-arginine, a precursor for nitric oxide, has been shown to improve coronary blood flow.46
Vasospasm: Calcium channel blockers and nitrates are preferred in the setting of vasospastic angina.33 Such calcium channel blockers include amlodipine, diltiazem, verapamil or long-acting nifedipine. A randomized trial of patients with angina, small coronary arteries and limited vasodilator reserve showed that patients on verapamil and nifedipine had fewer episodes of angina, consumed less nitroglycerin tablets and had increased exercise tolerance compared to patients on placebo.47 Tachyphylaxis is a known risk with long-term nitrate use and thus drug-free intervals (12 hours daily) are recommended. Unopposed beta blockade should be avoided as it may contribute to spasm.48 If beta blockers are indicated in patients with vasospasm, combined alpha/beta agents such as carvedilol are favored.
Nociceptive Abnormality: For nociceptive abnormality demonstrated by CFT, low-dose tricyclic antidepressants reduce the frequency of angina.42 In refractory cases, spinal cord stimulation, cognitive behavioral therapy and biofeedback can be considered.42
Non-pharmacologic Treatments
Multiple alternative non-pharmacologic approaches are available for CMD. Cardiac rehabilitation has been shown to improve diastolic resting blood pressure, body mass index and exercise capacity. These programs also improve overall quality of life and psychological morbidity.42, 49 Enhanced external counter-pulsation, a therapy consisting of the inflation and deflation of pneumatic stockings on the lower extremities during systole and diastole, respectively, can also improve CMD symptoms.42 This therapy promotes collateral coronary flow and improves endothelial function by reducing afterload and increasing preload. Therapeutic lifestyle recommendations include smoking cessation, nutrition counseling, weight reduction and regular moderate intensity physical therapy.
Knowledge Gaps Remain
Despite considerable evidence regarding MACE and long-term adverse prognosis associated with INOCA, neither the American College of Cardiology nor American Heart Association have guidelines to direct therapeutic strategies. As such, both internists and cardiologists alike may lack confidence in the recognition, diagnosis and management of this phenotype of ischemic heart disease. In 2017, the American College of Cardiology convened a group to review the current knowledge and provide next steps for evidence-based management.11 In 2019, the European Society of Cardiology guidelines for chronic coronary syndromes include a discussion and recommendation for evaluation of vasospastic and microvascular disease.33
At present, no standardized diagnostic algorithm exists. Decisions regarding testing may depend on patient risk stratification (i.e. history of prior myocardial infarction), extent of anginal symptoms on quality of life and local availability of testing modalities. Compared to the noninvasive methods, functional reactivity testing has the benefit of identifying the specific mechanism of dysfunction (i.e. non-endothelial dependent vs. endothelial dependent, presence of spasm and nociceptive abnormality) to better direct therapeutics. However, this approach is invasive, can be time consuming and requires specially trained cardiac interventionalists.31 Further work is presently ongoing to evaluate how functional testing may be implemented following standard diagnostic angiogram, when no obstructive lesions are found. A streamlined and abbreviated protocol of adenosine for CFR measurement followed by acetylcholine to observe angiographically for vasospasm may be easily employed by interventionalists.
Lastly, gender differences remain evident and require further investigation. It has been postulated that women may have a greater ability to widen and narrow arteries perhaps as a result of the need to control blood flow during pregnancy. Additionally, women have been shown to have more pain sensation compared to men and thus may have more perceived pain and anginal symptoms.50 With regard to outcomes, females with INOCA have been shown to have higher rates of cardiac events compared to men. One study of 13,695 subjects with INOCA found a 3-fold higher MACE rate in women compared to men in the first year.51 A significant knowledge gap remains on this matter.
Future Directions
Recent studies have suggested that cardiomyocyte injury and myocardial stiffness caused by CMD may play a role in the pathophysiology of patients with heart failure with preserved ejection fraction (HFpEF).52 It is hypothesized that microvascular endothelial dysfunction, decreased nitric oxide bioavailability and increased cytokine signaling may contribute to the increased microvascular inflammation and myocardial fibrosis observed in HFpEF.53, 54 Clinically, it has been shown that a decreased CFR has been found to be associated with diastolic dysfunction, and also been associated with a five-fold increased rate of HFpEF hospitalizations.52 Clinical studies also suggest there is also a higher prevalence of HFpEF in females compared to men.55 The association between CMD and HFpEF is an area that lends itself to further investigation, specifically with regard to gender differences.
In order to better target prevention and treatment, a deeper understanding of risk factors is needed. While traditional co-morbid risk factors such as hypertension, hyperlipidemia and diabetes have been implicated, less is known regarding autoimmune conditions and adverse pregnancy outcomes. Additionally, much remains to be studied about novel risk markers including high-sensitivity C-reactive protein, lipoproteins, interleukins and other inflammatory markers.
Regarding treatment, more randomized trials are needed to guide an evidence-based approach. One such ongoing study is The Women’s Ischemia Trial to Reduce Events in Non-Obstructive CAD (WARRIOR) trial (NCT#03417388), a multicenter, prospective, randomized blinded outcome trial, to explore the long-term outcomes of intensive statin, ACEI and aspirin therapy versus usual care among women with INOCA.40 This trial aims to enroll 4,442 participants. Randomized stem cell trials are also presently underway to evaluate the effectiveness of coronary CD34+ infusions in improving CFR in patients with CMD and persistent refractory angina.56
Conclusion
In patients who present with anginal symptoms but who have no evidence of obstructive coronary artery disease, it is important to consider the diagnoses of INOCA and CMD due to the substantial morbidity associated with this condition. At present, there remains no uniform comprehensive diagnostic and therapeutic strategy or algorithm—but several options exist. Both non-invasive and invasive methods are available to establish the diagnosis. Coronary function testing is currently the gold standard. It provides a useful means to determine mechanistic pathways for coronary microvascular dysfunction, which then further guides targeted therapeutic options with the goal of preventing future adverse cardiac events. Our evolving understanding of CMD and its management considerations relies on ongoing investigation and outcome clinical trials.
Table 1.
CFT Assessment of Pathway Function
| Pathway | Vasoactive Agent | Calculation | Abnormality |
|---|---|---|---|
| Non-endothelial dependent microvascular | Adenosine | CFR = pAPV/bAPV | CFR < 2.5 |
| Endothelial-dependent macrovascular | ACH | ((Post ACH peak Dm – baseline Dm)/baseline Dm) × 100 | <5% increase in Dm |
| Endothelial-dependent microvascular | ACH | CBF = 3.14 × (Dm/2)^2 × (APV/2) | ΔCBF < 50% |
| Vasospasm | ACH | N/A | >90% Dm reduction + chest pain/ischemic ST changes |
| Non-endothelial dependent macrovascular | NTG | ((Post NTG peak Dm - baseline Dm)/baseline Dm) × 100 | <20% increase in Dm |
| Nociceptive Abnormality | N/A | N/A | Chest pain from catheter or contrast |
ACH = acetylcholine, CFR = coronary flow reserve, pAPV = peak average peak velocity, bAPV = baseline average peak velocity, Dm = diameter, CBF = coronary blood flow, NTG = nitroglycerin
Table 2.
Coronary Microvascular Dysfunction (CMD) Treatment Options
| Endothelial Dysfunction |
| Angiotensin Converting Enzyme Inhibitors (ACE-I) |
| HMG-CoA Reductase Inhibitors (Statins) |
| Cardiac Rehabilitation |
| Enhanced External Counterpulsation (EECP) |
| Non-Endothelial Dysfunction |
| Beta-Blockers/Alpha-Beta Blockers |
| Nitrates |
| Ranolazine |
| Ivabradine |
| Phosphodiesterase-5 Inhibitors |
| Vasospasm or Abnormal Smooth Muscle Function (Prinzmetal’s Angina) |
| Calcium Channel Blockers |
| Nitrates |
| Nociceptive Abnormality |
| Low Dose Tricyclic Medication |
| Spinal Cord Stimulation |
| Cognitive Behavioral Therapy |
Key Points:
Women presenting with signs and symptoms of myocardial ischemia are more likely to have no obstructive coronary artery disease (CAD) on coronary angiography compared to men.
Coronary microvascular dysfunction (CMD) should be considered in patients presenting with persistent angina, evidence of ischemia and no obstructive CAD.
The presence of CMD is associated with considerable risk of major adverse cardiac events (MACE) including heart failure, myocardial infarction, stroke and death.
Coronary function testing (CFT) is the gold standard diagnostic test for CMD and characterizes the pathway(s) of dysfunction.
Management of CMD, as guided by CFT, is currently aimed at reducing risk of MACE and improving quality of life. More clinical outcome trials are needed and presently ongoing.
Funding:
This work was supported by contracts from the National Heart, Lung and Blood Institutes nos. N01-HV-68161, N01-HV-68162, N01-HV-68163, N01-HV-68164, grants U0164829, U01 HL649141, U01 HL649241, K23HL105787, K23HL127262, K23HL125941, T32HL69751, R01 HL090957, R01 HL146158, U54 AG065141, 1R03AG032631 from the National Institute on Aging, GCRC grant MO1-RR00425 from the National Center for Research Resources, the National Center for Advancing Translational Sciences Grant UL1TR000124 and UL1TR000064, and grants from the Gustavus and Louis Pfeiffer Research Foundation, Danville, NJ, The Women’s Guild of Cedars-Sinai Medical Center, Los Angeles, CA, The Ladies Hospital Aid Society of Western Pennsylvania, Pittsburgh, PA, and QMED, Inc., Laurence Harbor, NJ, the Edythe L. Broad and the Constance Austin Women’s Heart Research Fellowships, Cedars-Sinai Medical Center, Los Angeles, California, the Barbra Streisand Women’s Cardiovascular Research and Education Program, Cedars-Sinai Medical Center, Los Angeles, The Society for Women’s Health Research (SWHR), Washington, D.C., The Linda Joy Pollin Women’s Heart Health Program, the Erika Glazer Women’s Heart Research Initiative, and the Adelson Family Foundation, Cedars-Sinai Medical Center, Los Angeles, California.
Appendix A: Coronary Function Testing Protocol
Several protocols exist for performance of coronary function testing (CFT) for the purposes of evaluating for coronary microvascular dysfunction (CMD) and coronary vasospasm. At our institution, we utilize the following outlined methods:
Patient Preparation:
Patients fast for 12 hours before the scheduled procedure.35 To avoid confounding of results, patients are asked to discontinue caffeine, long-acting nitrates, short-acting calcium channel blockers, alpha and beta blockers, angiotensin-converting enzyme inhibitors (ACEI) or angiotensin receptor blockade, renin and aldosterone inhibitors, ranolazine, diuretics, angiotensin-neprilysin inhibitors, ticagrelor and Aggrenox for 24 hours prior to the procedure. Long-acting calcium channel blockers (CCB) are withheld for 48 hours and sublingual nitroglycerin and nicotine for 4 hours prior to testing.
Vasoactive Agent Preparation:
Two concentrations of acetylcholine (0.182 μg/mL and 18.2 μg/mL, respectively) are premixed by the hospital pharmacy, within three hours of the scheduled procedure.35 Two doses of adenosine (18 μg and 100 μg, respectively) and 200 μg of nitroglycerin are prepared by the catheterization lab nursing staff. Of note, the precise agent dosages used may vary by institution.
Angiography to Confirm Non-Obstructive Disease:
Coronary angiography is performed to assess for atherosclerosis, myocardial bridging, anomalies or slow flow. Any catheter-induced spasm or chest pain observed during contrast administration or catheter manipulation are also documented. Left ventricular end-diastolic pressure is measured. Fractional flow reserve should be measured to rule out hemodynamically significant stenoses. Any obstructive disease or spontaneous spasm observed at this time may obviate the need for further testing.
Intracoronary Vasoactive Agent Infusions:
Patients are given body-weight adjusted heparin to achieve activated clotting time above 250.35 A 0.014” Volcano Doppler FloWire is placed into the proximal to mid left anterior descending artery until an adequate Doppler signal is obtained. Prior to each infusion, a baseline heart rate, blood pressure and average peak velocity of blood flow are recorded. At specified time intervals, the peak heart rate, blood pressure and average peak velocity are documented. The line is flushed and return to baseline average peak velocity permitted before infusion of subsequent dosages and agents. Any symptoms, ischemic ECG changes or arrhythmias during infusions are noted. Baseline and peak (immediately after peak average peak velocity taken) cine images are taken to allow quantitative coronary angiography measurements of the vessel diameter 5 mm distal to the Doppler FloWire tip.
Assessment of Mechanistic Pathways and Significance:
This assessment is most often performed to completion, in the specified order, to assess for the simultaneous presence of multiple pathways of coronary artery dysfunction. If the patient experiences a complication at any time, the procedure may be aborted.
Non-endothelial dependent microvascular function: First, 18 μg and 100 μg dosages of adenosine are consecutively delivered via intracoronary bolus, to induce maximal hyperemia.35 Volcano ComboMap calculates coronary flow reserve (CFR), which is equivalent to the ratio of the peak to baseline average peak velocities.35, 57 A peak CFR less than 2.5 is considered abnormal.
Endothelial-dependent macrovascular function: Next, the 0.182 and 18.2 μg/mL concentrations of acetylcholine are infused via infusion pump at a rate of 2 to 3 mL over 3 minutes. The change in vessel diameter is then calculated by quantitative coronary angiography. A less than or equal to 5% increase in mean lumen diameter suggests dysfunction. Of note, the infusion rate may vary according to institutional protocol. Coronary angiography is performed after each dosage of acetylcholine, in order to evaluate for epicardial vasospasm. It is important to withdraw the contents of the guide catheter prior to angiography, in order to avoid inadvertently delivering a bolus of any acetylcholine that may be left in the guide following the slow infusion.
Endothelial-dependent microvascular function: The aforementioned infusion of the 18.2 μg/mL concentration of acetylcholine is used to calculate coronary blood flow, with 2 to 3mL infused over 3 minutes. Coronary angiography is performed following each dose of acetylcholine to evaluate for epicardial vasospasm. Again, it is important to withdraw the contents of the guide catheter prior to angiography. A < 50% increase in coronary blood flow is considered abnormal. As described above, the infusion rate may vary according to institutional protocol.
Vasospasm: As the graded 0.182 and 18.2 μg/mL dose infusions of acetylcholine occur, the operator assesses for signs of spasm. If no spasm is exhibited, a higher concentration of acetylcholine is infused at a rate of 2 mL/minute for 3 minutes. If spasm is provoked, subsequent higher acetylcholine dose testing is withheld, and nitroglycerin is administered immediately. Epicardial vasospasm is defined as >90% diameter reduction associated with chest pain and/or ischemic ST changes, while microvascular coronary spasm is suggested by chest pain and ischemic ST changes, without significant epicardial artery vasoconstriction.
Non-endothelial dependent macrovascular function: Following acetylcholine infusion, nitroglycerin (150–200 μg) is given, and quantitative coronary angiography is performed after 30 seconds. Dilation < 20% is considered abnormal. This measurement allows for assessment of the macrovascular responsiveness to treatment with nitrates.
Nociceptive abnormality: Heightened pain sensitivity at any point in the procedure, demonstrated by chest pain during catheter manipulation and/or contrast administration is suggestive of nociceptive abnormality.
References:
- 1.Farrehi PM, Bernstein SJ, Rasak M, et al. Frequency of negative coronary arteriographic findings in patients with chest pain is related to community practice patterns. Am J Manag Care. Jul 2002;8(7):643–8. [PubMed] [Google Scholar]
- 2.Sharaf BL, Pepine CJ, Kerensky RA, et al. Detailed angiographic analysis of women with suspected ischemic chest pain (pilot phase data from the NHLBI-sponsored Women’s Ischemia Syndrome Evaluation [WISE] Study Angiographic Core Laboratory). Am J Cardiol. Apr 15 2001;87(8):937–41; A3. doi: 10.1016/s0002-9149(01)01424-2 [DOI] [PubMed] [Google Scholar]
- 3.Marinescu MA, Loffler AI, Ouellette M, Smith L, Kramer CM, Bourque JM. Coronary microvascular dysfunction, microvascular angina, and treatment strategies. JACC Cardiovasc Imaging. Feb 2015;8(2):210–20. doi: 10.1016/j.jcmg.2014.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Johnson BD, Shaw LJ, Buchthal SD, et al. Prognosis in women with myocardial ischemia in the absence of obstructive coronary disease: results from the National Institutes of Health-National Heart, Lung, and Blood Institute-Sponsored Women’s Ischemia Syndrome Evaluation (WISE). Circulation. Jun 2004;109(24):2993–9. doi: 10.1161/01.CIR.0000130642.79868.B2 [DOI] [PubMed] [Google Scholar]
- 5.Ford TJ, Berry C. How to Diagnose and Manage Angina Without Obstructive Coronary Artery Disease: Lessons from the British Heart Foundation CorMicA Trial. Interv Cardiol. May 2019;14(2):76–82. doi: 10.15420/icr.2019.04.R1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anderson RD, Petersen JW, Mehta PK, et al. Prevalence of Coronary Endothelial and Microvascular Dysfunction in Women with Symptoms of Ischemia and No Obstructive Coronary Artery Disease Is Confirmed by a New Cohort: The NHLBI-Sponsored Women’s Ischemia Syndrome Evaluation-Coronary Vascular Dysfunction (WISE-CVD). J Interv Cardiol. 2019;2019:7169275. doi: 10.1155/2019/7169275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sara JD, Widmer RJ, Matsuzawa Y, Lennon RJ, Lerman LO, Lerman A. Prevalence of Coronary Microvascular Dysfunction Among Patients With Chest Pain and Nonobstructive Coronary Artery Disease. JACC Cardiovasc Interv. Sep 2015;8(11):1445–53. doi: 10.1016/j.jcin.2015.06.017 [DOI] [PubMed] [Google Scholar]
- 8.Murthy VL, Naya M, Taqueti VR, et al. Effects of sex on coronary microvascular dysfunction and cardiac outcomes. Circulation. Jun 2014;129(24):2518–27. doi: 10.1161/CIRCULATIONAHA.113.008507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Day LJ, Sowton E. Clinical features and follow-up of patients with angina and normal coronary arteries. Lancet. Aug 14 1976;2(7981):334–7. doi: 10.1016/s0140-6736(76)92591-5 [DOI] [PubMed] [Google Scholar]
- 10.Merz CN, Kelsey SF, Pepine CJ, et al. The Women’s Ischemia Syndrome Evaluation (WISE) study: protocol design, methodology and feasibility report. J Am Coll Cardiol. May 1999;33(6):1453–61. doi: 10.1016/s0735-1097(99)00082-0 [DOI] [PubMed] [Google Scholar]
- 11.Bairey Merz CN, Pepine CJ, Walsh MN, Fleg JL. Ischemia and No Obstructive Coronary Artery Disease (INOCA): Developing Evidence-Based Therapies and Research Agenda for the Next Decade. Circulation. Mar 14 2017;135(11):1075–1092. doi: 10.1161/CIRCULATIONAHA.116.024534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aldiwani H, Zaya M, Suppogu N, et al. Angina Hospitalization Rates in Women With Signs and Symptoms of Ischemia But no Obstructive Coronary Artery Disease: A Report from the WISE (Women’s Ischemia Syndrome Evaluation) Study. J Am Heart Assoc. 02 2020;9(4):e013168. doi: 10.1161/JAHA.119.013168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kenkre TS, Malhotra P, Johnson BD, et al. Ten-Year Mortality in the WISE Study (Women’s Ischemia Syndrome Evaluation). Circ Cardiovasc Qual Outcomes. Dec 2017;10(12)doi: 10.1161/CIRCOUTCOMES.116.003863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Patel H, Aggarwal NT, Rao A, et al. Microvascular Disease and Small-Vessel Disease: The Nexus of Multiple Diseases of Women. J Womens Health (Larchmt). Feb 19 2020;doi: 10.1089/jwh.2019.7826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shaw LJ, Merz CN, Pepine CJ, et al. The economic burden of angina in women with suspected ischemic heart disease: results from the National Institutes of Health--National Heart, Lung, and Blood Institute--sponsored Women’s Ischemia Syndrome Evaluation. Circulation. Aug 29 2006;114(9):894–904. doi: 10.1161/CIRCULATIONAHA.105.609990 [DOI] [PubMed] [Google Scholar]
- 16.AlBadri A, Bairey Merz CN, Johnson BD, et al. Impact of Abnormal Coronary Reactivity on Long-Term Clinical Outcomes in Women. J Am Coll Cardiol. Feb 19 2019;73(6):684–693. doi: 10.1016/j.jacc.2018.11.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Radico F, Cicchitti V, Zimarino M, De Caterina R. Angina pectoris and myocardial ischemia in the absence of obstructive coronary artery disease: practical considerations for diagnostic tests. JACC Cardiovasc Interv. May 2014;7(5):453–63. doi: 10.1016/j.jcin.2014.01.157 [DOI] [PubMed] [Google Scholar]
- 18.Kuo L, Davis MJ, Chilian WM. Longitudinal gradients for endothelium-dependent and -independent vascular responses in the coronary microcirculation. Circulation. Aug 1 1995;92(3):518–25. doi: 10.1161/01.cir.92.3.518 [DOI] [PubMed] [Google Scholar]
- 19.Lerman A, Burnett JC. Intact and altered endothelium in regulation of vasomotion. Circulation. Dec 1992;86(6 Suppl):III12–19. [PubMed] [Google Scholar]
- 20.Kinlay S, Ganz P. Role of endothelial dysfunction in coronary artery disease and implications for therapy. Am J Cardiol. Nov 1997;80(9A):11I–16I. doi: 10.1016/s0002-9149(97)00793-5 [DOI] [PubMed] [Google Scholar]
- 21.Yang Z, Li J, Kong J, Wu S. Impairment of vascular endothelial function following reperfusion therapy in patients with acute myocardial infarction. J Int Med Res. Aug 2013;41(4):1074–8. doi: 10.1177/0300060513487650 [DOI] [PubMed] [Google Scholar]
- 22.Chen C, Wei J, AlBadri A, Zarrini P, Bairey Merz CN. Coronary Microvascular Dysfunction- Epidemiology, Pathogenesis, Prognosis, Diagnosis, Risk Factors and Therapy. Circ J. Dec 22 2016;81(1):3–11. doi: 10.1253/circj.CJ-16-1002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Britten MB, Zeiher AM, Schachinger V. Clinical importance of coronary endothelial vasodilator dysfunction and therapeutic options. J Intern Med. Apr 1999;245(4):315–27. doi: 10.1046/j.1365-2796.1999.00449.x [DOI] [PubMed] [Google Scholar]
- 24.Lee DH, Youn HJ, Choi YS, et al. Coronary flow reserve is a comprehensive indicator of cardiovascular risk factors in subjects with chest pain and normal coronary angiogram. Circ J. Jul 2010;74(7):1405–14. doi: 10.1253/circj.cj-09-0897 [DOI] [PubMed] [Google Scholar]
- 25.Moreau P, d’Uscio LV, Lüscher TF. Structure and reactivity of small arteries in aging. Cardiovasc Res. Jan 1998;37(1):247–53. doi: 10.1016/s0008-6363(97)00225-3 [DOI] [PubMed] [Google Scholar]
- 26.Pitkänen OP, Nuutila P, Raitakari OT, et al. Coronary flow reserve is reduced in young men with IDDM. Diabetes. Feb 1998;47(2):248–54. doi: 10.2337/diab.47.2.248 [DOI] [PubMed] [Google Scholar]
- 27.Recio-Mayoral A, Mason JC, Kaski JC, Rubens MB, Harari OA, Camici PG. Chronic inflammation and coronary microvascular dysfunction in patients without risk factors for coronary artery disease. Eur Heart J. Aug 2009;30(15):1837–43. doi: 10.1093/eurheartj/ehp205 [DOI] [PubMed] [Google Scholar]
- 28.Kaufmann PA, Gnecchi-Ruscone T, di Terlizzi M, Schäfers KP, Lüscher TF, Camici PG. Coronary heart disease in smokers: vitamin C restores coronary microcirculatory function. Circulation. Sep 2000;102(11):1233–8. doi: 10.1161/01.cir.102.11.1233 [DOI] [PubMed] [Google Scholar]
- 29.Lanza GA, Crea F. Primary coronary microvascular dysfunction: clinical presentation, pathophysiology, and management. Circulation. Jun 2010;121(21):2317–25. doi: 10.1161/CIRCULATIONAHA.109.900191 [DOI] [PubMed] [Google Scholar]
- 30.Kanatsuka H, Eastham CL, Marcus ML, Lamping KG. Effects of nitroglycerin on the coronary microcirculation in normal and ischemic myocardium. J Cardiovasc Pharmacol. May 1992;19(5):755–63. [PubMed] [Google Scholar]
- 31.Wei J, Cheng S, Merz CNB. Coronary Microvascular Dysfunction Causing Cardiac Ischemia in Women. JAMA. Nov 2019;doi: 10.1001/jama.2019.15736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ong P, Camici PG, Beltrame JF, et al. International standardization of diagnostic criteria for microvascular angina. Int J Cardiol. Jan 2018;250:16–20. doi: 10.1016/j.ijcard.2017.08.068 [DOI] [PubMed] [Google Scholar]
- 33.Knuuti J, Wijns W, Saraste A, et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. Jan 14 2020;41(3):407–477. doi: 10.1093/eurheartj/ehz425 [DOI] [PubMed] [Google Scholar]
- 34.Rosen SD, Paulesu E, Wise RJ, Camici PG. Central neural contribution to the perception of chest pain in cardiac syndrome X. Heart. Jun 2002;87(6):513–9. doi: 10.1136/heart.87.6.513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wei J, Mehta PK, Johnson BD, et al. Safety of coronary reactivity testing in women with no obstructive coronary artery disease: results from the NHLBI-sponsored WISE (Women’s Ischemia Syndrome Evaluation) study. JACC Cardiovasc Interv. Jun 2012;5(6):646–53. doi: 10.1016/j.jcin.2012.01.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kodzwa R. ACR Manual on Contrast Media: 2018 Updates. Radiol Technol. Sep 2019;91(1):97–100. [PubMed] [Google Scholar]
- 37.Schindler TH, Schelbert HR, Quercioli A, Dilsizian V. Cardiac PET imaging for the detection and monitoring of coronary artery disease and microvascular health. JACC Cardiovasc Imaging. Jun 2010;3(6):623–40. doi: 10.1016/j.jcmg.2010.04.007 [DOI] [PubMed] [Google Scholar]
- 38.Feher A, Sinusas AJ. Quantitative Assessment of Coronary Microvascular Function: Dynamic Single-Photon Emission Computed Tomography, Positron Emission Tomography, Ultrasound, Computed Tomography, and Magnetic Resonance Imaging. Circ Cardiovasc Imaging. Aug 2017;10(8)doi: 10.1161/CIRCIMAGING.117.006427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Saraste M, Koskenvuo J, Knuuti J, et al. Coronary flow reserve: measurement with transthoracic Doppler echocardiography is reproducible and comparable with positron emission tomography. Clin Physiol. Jan 2001;21(1):114–22. doi: 10.1046/j.1365-2281.2001.00296.x [DOI] [PubMed] [Google Scholar]
- 40.Barsky L, Merz CNB, Wei J, et al. Even “WISE-R?”-an Update on the NHLBI-Sponsored Women’s Ischemia Syndrome Evaluation. Curr Atheroscler Rep. Jun 18 2020;22(8):35. doi: 10.1007/s11883-020-00852-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ford TJ, Stanley B, Sidik N, et al. 1-Year Outcomes of Angina Management Guided by Invasive Coronary Function Testing (CorMicA). JACC Cardiovasc Interv. Jan 13 2020;13(1):33–45. doi: 10.1016/j.jcin.2019.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Samim A, Nugent L, Mehta PK, Shufelt C, Bairey Merz CN. Treatment of angina and microvascular coronary dysfunction. Curr Treat Options Cardiovasc Med. Aug 2010;12(4):355–64. doi: 10.1007/s11936-010-0083-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pauly DF, Johnson BD, Anderson RD, et al. In women with symptoms of cardiac ischemia, nonobstructive coronary arteries, and microvascular dysfunction, angiotensin-converting enzyme inhibition is associated with improved microvascular function: A double-blind randomized study from the National Heart, Lung and Blood Institute Women’s Ischemia Syndrome Evaluation (WISE). Am Heart J. Oct 2011;162(4):678–84. doi: 10.1016/j.ahj.2011.07.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kayikcioglu M, Payzin S, Yavuzgil O, Kultursay H, Can LH, Soydan I. Benefits of statin treatment in cardiac syndrome-X1. Eur Heart J. Nov 2003;24(22):1999–2005. doi: 10.1016/s0195-668x(03)00478-0 [DOI] [PubMed] [Google Scholar]
- 45.Lee BK, Lim HS, Fearon WF, et al. Invasive evaluation of patients with angina in the absence of obstructive coronary artery disease. Circulation. Mar 2015;131(12):1054–60. doi: 10.1161/CIRCULATIONAHA.114.012636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lerman A, Burnett JC, Higano ST, McKinley LJ, Holmes DR. Long-term L-arginine supplementation improves small-vessel coronary endothelial function in humans. Circulation. Jun 1998;97(21):2123–8. doi: 10.1161/01.cir.97.21.2123 [DOI] [PubMed] [Google Scholar]
- 47.Cannon RO, Watson RM, Rosing DR, Epstein SE. Efficacy of calcium channel blocker therapy for angina pectoris resulting from small-vessel coronary artery disease and abnormal vasodilator reserve. Am J Cardiol. Aug 1985;56(4):242–6. doi: 10.1016/0002-9149(85)90842-2 [DOI] [PubMed] [Google Scholar]
- 48.Lanza GA, Maseri A. Coronary Artery Spasm. Curr Treat Options Cardiovasc Med. Feb 2000;2(1):83–90. doi: 10.1007/s11936-000-0031-0 [DOI] [PubMed] [Google Scholar]
- 49.Laksanakorn W, Laprattanagul T, Wei J, et al. Cardiac rehabilitation for cardiac syndrome X and microvascular angina: A case report. Int J Case Rep and Images 2015. p. 239–244. [Google Scholar]
- 50.Bairey Merz CN. Testing for Coronary Microvascular Dysfunction. JAMA. Nov 2019;doi: 10.1001/jama.2019.16625 [DOI] [PubMed] [Google Scholar]
- 51.Sedlak TL, Lee M, Izadnegahdar M, Merz CN, Gao M, Humphries KH. Sex differences in clinical outcomes in patients with stable angina and no obstructive coronary artery disease. Am Heart J. Jul 2013;166(1):38–44. doi: 10.1016/j.ahj.2013.03.015 [DOI] [PubMed] [Google Scholar]
- 52.Taqueti VR, Solomon SD, Shah AM, et al. Coronary microvascular dysfunction and future risk of heart failure with preserved ejection fraction. Eur Heart J. Mar 7 2018;39(10):840–849. doi: 10.1093/eurheartj/ehx721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mohammed SF, Hussain S, Mirzoyev SA, Edwards WD, Maleszewski JJ, Redfield MM. Coronary microvascular rarefaction and myocardial fibrosis in heart failure with preserved ejection fraction. Circulation. Feb 2015;131(6):550–9. doi: 10.1161/CIRCULATIONAHA.114.009625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Paulus WJ, Tschöpe C. A novel paradigm for heart failure with preserved ejection fraction: comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. J Am Coll Cardiol. Jul 2013;62(4):263–71. doi: 10.1016/j.jacc.2013.02.092 [DOI] [PubMed] [Google Scholar]
- 55.Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. Jul 2006;355(3):251–9. doi: 10.1056/NEJMoa052256 [DOI] [PubMed] [Google Scholar]
- 56.Johnson GL, Henry TD, Povsic TJ, et al. CD34. Stem Cells Transl Med. 10 2020;9(10):1147–1152. doi: 10.1002/sctm.20-0046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gagliardi MG, Adorisio R, Crea F, Versacci P, Di Donato R, Sanders SP. Abnormal vasomotor function of the epicardial coronary arteries in children five to eight years after arterial switch operation: an angiographic and intracoronary Doppler flow wire study. J Am Coll Cardiol. Oct 18 2005;46(8):1565–72. doi: 10.1016/j.jacc.2005.06.065 [DOI] [PubMed] [Google Scholar]


