Abstract
Context
In France, care workers and health students have been intensely mobilized during the first wave of the COVID-19 pandemic. But few studies have evaluated psychological distress on non-medical health students, in addition to the challenges posed by pedagogical continuity while universities are closed following health and safety regulations.
Objectives
This study aims to assess COVID-19's impact on health students in France on different levels: psychological, educational and social.
Methods
An online national cross-sectional study, from April 11 to May 30 2020, included sociodemographic, work conditions and numeric scales.
Results
A total of 4411 students answered. Regarding the K6 scale, 39% of students had moderate distress, and 21% had a high level of distress. Risk factors of psychological distress included being a woman (P < 0.001), being between 19 and 21 years old (P < 0.001), living alone (P = 0.008), and not having the ability to isolate (P < 0.001). Students on the frontline had less psychological distress (57 vs 62%, P = 0.003), better quality of sleep (34% vs 28% high quality, P < 0.001) but a higher consumption of medical (8.5% vs 6.5%, P = 0.044) and non-medical (18% vs 10%, P < 0.001) psychotropic drugs. Nurse and medical students had more distress and used more non-medical psychotropic substances than other health students (15% vs 9.2%).
Discussion
COVID-19’ crisis had an important impact on health students’ mental health, social life and training with discrepancies regarding the speciality whether they were on the frontline or not. There is an urgent need for psychological and pedagogical support for students, and even more so regarding the prolongation of the COVID-19 epidemic.
Keywords: Health students, Mental health, COVID-19, Psychological distress
Résumé
Objectifs
Durant la première vague de la pandémie de COVID-19 en France, les professionnels et étudiants en santé ont été intensément mobilisés pour faire face à l’augmentation exponentielle des besoins de soins dans le système de santé. Une étude française dans 21 unités de soins intensifs au cours du premier mois de confinement a révélé que la prévalence des symptômes d’anxiété et de dépression chez les soignants était de 50,4 %, et 30,4 % respectivement. En revanche, peu études se sont consacrées à l’évaluation de la détresse psychologique des étudiants en santé durant cette période. Dans la population générale des étudiants français, une étude a révélé que la prévalence des pensées suicidaires, de la détresse grave et du niveau élevé de stress perçu pendant la première vague était de 11,4 %, 22,4 % et 24,7 % respectivement. L’objectif de notre étude est d’évaluer l’impact du COVID-19 sur la santé mentale des étudiants en santé (médecine, soins infirmiers, pharmacie, maïeutique, odontologie, ergothérapie, orthoptie, orthophonie, psychomotricité, audioprothésiste) en France pendant la 1re vague.
Méthodes
Un questionnaire en ligne a été proposé du 11 avril au 30 mai 2020 auprès des étudiants en santé de France. La diffusion a été réalisé par l’intermédiaire de réseaux sociaux et de mails de différents groupes institutionnels (conférences des doyens, présidents d’université, Centre National d’appui à la qualité de vie des étudiants en santé…). Le questionnaire comprenait l’échelle de Kessler en 6 items (K6), la Social Provision Scale SPS-10, la consommation de drogues et de psychotropes et l’évaluation du sommeil. Les tests du Chi2 et test exact de Fisher ont été utilisés pour comparer la prévalence entre les groupes. Par la suite, des modèles de régression logistique ajustés sur l’âge et le sexe ont été utilisés (analyses multivariées).
Résultats
Un total of 4411 étudiants ont répondu: 39 % présentaient une détresse modérée et 21 % une détresse élevée à l’échelle de détresse psychologique de Kessler. Plusieurs facteurs de risque de détresse psychologique ont été retrouvés: être une femme (p < 0,001), avoir entre 19 et 21 ans (p < 0,001), vivre seul (p = 0,008) et ne pas avoir la possibilité de s’isoler chez soi pour travailler (p < 0,001). Les étudiants en « première ligne » face aux patients expriment moins de détresse que les étudiants qui sont confinés sans activité clinique (57 % contre 62 %, p = 0,003), une meilleure qualité du sommeil (34 % contre 28 %, p < 0,001) mais une augmentation de la consommation de médicaments (8,5 % contre 6,5 %, p = 0,044) ou d’autres substances psychoactives (18 % contre 10 %, p < 0,001). Les étudiants en soins infirmiers et étudiants en médecine présentent une détresse psychologique et une augmentation de la consommation de produits plus importantes que les autres étudiants (15 % contre 9,2 %).
Conclusions
La pandémie COVID-19 a eu un impact certain sur la santé mentale des étudiants en santé et leur formation, bien que des disparités existent selon les cursus, et selon la participation aux soins des étudiants. Cette étude présente certaines limites: le taux de réponse était faible; les jeunes étudiants (18–21 ans) étaient surreprésentés. Il s ‘agit de la première étude nationale sur la santé mentale des étudiants en santé et elle pourra servir de référence pour comparer avec les futures études. Il semble urgent d’intervenir pour améliorer le bien-être des étudiants en santé d’autant plus que la crise sanitaire tend à se prolonger.
Mots clés: Étudiant en santé, Santé mentale, COVID-19, Détresse psychologique
Introduction
Caregivers’ mental health has been a concern for a long time, especially for physicians who have increased suicide rates [1]. More recently, a meta-analysis found a high level of burnout in physicians [2]. But bad mental health began before graduation in health students. Meta-analysis highlighted the elevated prevalence of depressive symptoms (27%) and suicidal ideation (11%) on the one hand [3] and burnout (44%) on the other hand [4]. This alarming situation is not specific to medical students. A meta-analysis also found an elevated prevalence of depressive symptoms in dental students [5] and nursing students [6]. In midwife students, a narrative review found evidence of the important prevalence of distress [7].
In France, some surveys have been done. In medical students, a 2016 survey by students’ associations found a high prevalence of anxiety symptoms (66%), depressive symptoms (27%) and suicidal thoughts (23%). In dental students, a 2018 survey found a prevalence of 28% for depressive syndrome and high stress levels [8]. In pharmacist students, a 2019 survey found a prevalence of 28% for the depressive syndrome; 76% said they “suffer from a lack of wellbeing due to their course” [9]. All these data came from studies before COVID 19's pandemic.
In France, following a ministerial report on the subject [10], the Ministry of Health and the Ministry of Higher Education and Research launched a National Support Center for the Quality of Life of Health Students (Centre National d’Appui, CNA) on July 15, 2019. The CNA provides expertise, support and training in quality of life and success with health students and teachers.
Like all countries, France was impacted by the COVID-19 pandemic [11], [12]. The French government declared a nationwide lockdown from March 17 until May 11 2020, to control the propagation of the disease and mitigate the tensions within the health care system [13]. Health workers were exposed to increased psychosocial risks [14], [15] during this period: work overload, lack of staff and protective equipment, multiples critical care situations, …
International literature essentially based on Chinese [16], Italian [17] or Emirati [18] healthcare personnel, or that have been observed during previously pandemics (SARS-COV-1), includes several warnings toward the psychological consequences that a health crisis can have on health workers, whether they are in training or professionals [14], [19], [20], [21], [22]. In this new situation (pandemics and lockdown), psychiatrists alerted the risk of increased suicide and mental illness rates, especially in young people [23].
A French study on 21 ICU health workers during the first month of lockdown found the prevalence of symptoms of anxiety, depression, and peritraumatic dissociation were 50.4%, 30.4%, and 32%, respectively [24]. Health students were also mobilized against SARS-COV-2 in France. They usually take professional responsibilities early on during their curriculum, but during the pandemic, a significant part of these students had been called upon as makeshift health workers due to the high demand for health professionals.
In general French student's population, a study during the first wave (data collected from April 17 to May 4) found the prevalence of suicidal thoughts, severe distress and high level of perceived stress were 11.4%, 22.4% and 24.7%, respectively [25]. But health students (medical, pharmacists, dental, nurse, midwives, …) are different from others students because of their involvement in the fight against COVID 19.
The CNA and CESP (Centre de recherche en Epidémiologie et Santé des Populations, Research Center in Epidemiology and Population Health) have directed this cross-sectional study to observe the specific impact of the first wave of the COVID-19 pandemic on the health students’ quality of life in France.
Material and Method
We conducted an online survey on health students from April 11 to May 30, 2020.
The link of the web questionnaire has been sent to health students by the universities’ enrolment services and posted on social media (Facebook and Twitter) by students’ representative organizations.
Population
Health students came from various healthcare academic fields. Students in the following fields were included in the study: medicine, pharmacy, nursing, midwifery, odontology (dental students), occupational therapy, orthoptic, speech therapy, psychomotricity, and hearing care. Medical, pharmacist and dental students have a longer study duration, which can be divided into three stages (preclinic, clinic, and residents). Because of the low number of subjects, we don’t distinguish regarding the stage.
Material
The questionnaire started with sociodemographic questions including birth year, field of study, year of study, sex, leaving alone or not, and ability to isolate themselves at home.
Two validated scales were used: Kessler's K6 scale and social provision scale SPS-10. Kessler's K6 is a 6 items scale to evaluate psychological distress according to the Diagnostic and Statistical Manual of Mental Disorders 4th (DSM4) [26]. Answers go on Likert's scale from 1(“Every Time”) to 5 (’Never“). The result is calculated by adding the scores of each item. If the final score is under 8, there is no issue; between 8 and 12, the subject has moderate stress, and over 13, it's compatible with a serious mental illness (anxiety disorder, mood disorder). The Kessler scale, which measures psychological distress in the general population, has the merit of being short and distinguishing between both patients with psychiatric symptoms from healthy subjects without being diagnostic. In 2002, authors noted, “The brevity, strong psychometric properties, and ability to discriminate DSM-IV cases from non-cases make the K10 and K6 attractive for use in general-purpose health surveys” [27]. In a recent systematic review (“Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic”), 6 (18%) of 34 cross-sectional studies used the K6 [28].
SPS-10 is a 10 items scale used to measure an individual's perceived social support. Answers go on Likert's scale from 1 (“Totally agree”) to 4 (“Totally disagree”) [29].
Five questions used numerical scale, going from 0 (“not at all”) to 10 (“very much”), to measure psychological distress, information level about available support systems, their need for support, quality of sleep, and whether they had experienced some form of hypomania. We grouped data in “low” (0–4), “moderate” (5–7), and “high” (8–10).
Two Yes/No questions were used to measure medical psychotropic drugs and non-medical psychotropic substances (alcohol, tobacco, cannabis,…) consumption.
Ethics
The questionnaires were collected anonymously, IP addresses were not recovered. Data were stored in an offline database for further analysis. Respondents were informed, and they gave their informed consent to participate. It respects European Data Protection Regulation. This study received agreement from the Paris Saclay Ethics and Research Committee (reference: CER-Paris-Saclay-2020-035).
Statistical Analysis
Descriptive information was provided as percentages. Statistical significance was tested in bivariate analyses using the Chi2 test and Fisher's exact test to compare between groups’ prevalence (on the one hand, students who have been in direct contact with patients, and on the other hand students who were in lockdown or the rearguard and were not in direct contact with the patients). Subsequently, logistic regression models adjusted for age and sex were performed for statistically significant associations in bivariate analyses. Statistical significance was evaluated using two-sided tests with an alpha risk set a priori at 0.05. Statistical analyses were performed using R software, version 1.4.869.
Results
Population
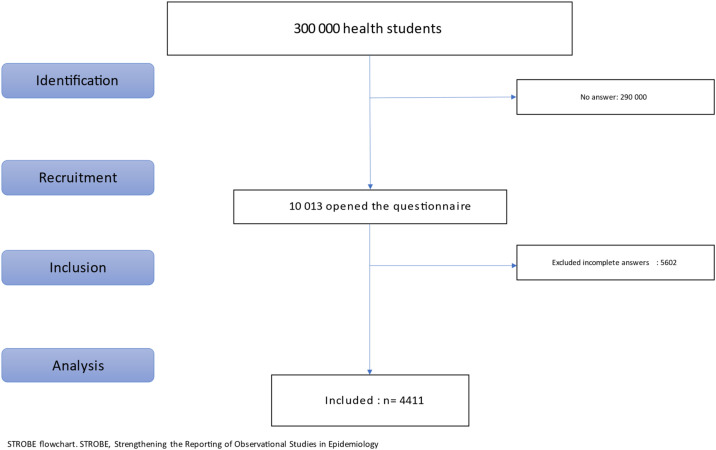
A total of 10,013 people opened the questionnaire. After excluding the respondents with too much missing data, which would impact the mode imputation, the results are based on 4411 answers (Fig. 1 ). According to government data, it represents about 1,5% of the approximately 300,000 French health students, with important discrepancies regarding their curriculum.
Fig. 1.
Flow chart.
Because there are very few answers from some specialities, we grouped them: audio prosthetist with orthoptists, psychomotricity, speech therapy physiotherapy, and ergotherapy in a group called “others”; midwife with dental and pharmacists.
Most of the students don’t live alone and can isolate themselves but also with discrepancies between groups. There are significative differences in the population: most nurses and other students are in the two first years of study versus 20% for medical or dental/pharmacists/midwife students (Table 1 ).
Table 1.
Population description by specialty.
| Characteristics/Number (percentage) | Overall, n = 4,411 |
Others n = 873 |
Medicine n = 1,712 |
Nurse n = 1,010 |
Dental-pharmacist-midwife n = 816 |
P-value* |
|---|---|---|---|---|---|---|
| Gender | ||||||
| Women | 3,510 (80%) | 797 (91%) | 1,198 (71%) | 892 (89%) | 623 (77%) | |
| Men | 859 (20%) | 74 (8.5%) | 490 (29%) | 111 (11%) | 184 (23%) | |
| Other | 11 (0.3%) | 1 (0.1%) | 8 (0.5%) | 1 (<0.1%) | 1 (0.1%) | |
| Unknown | 31 | 1 | 16 | 6 | 8 | |
| Age (years) | < 0.001 | |||||
| 19–21 | 729 (17%) | 137 (16%) | 296 (18%) | 231 (24%) | 65 (8.2%) | |
| 22–24 | 1,739 (40%) | 507 (59%) | 438 (26%) | 396 (41%) | 398 (50%) | |
| 25–27 | 994 (23%) | 158 (18%) | 466 (28%) | 116 (12%) | 254 (32%) | |
| 27 and more | 833 (19%) | 59 (6.9%) | 471 (28%) | 227 (23%) | 76 (9.6%) | |
| Unknown | 116% | 12 | 41 | 40 | 23 | |
| Years of study Numbers |
< 0.001 | |||||
| 1–3 | 2,674 (61%) | 759 (87%) | 618 (36%) | 974 (97%) | 323 (40%) | |
| 4–5 | 827 (19%) | 107 (12%) | 353 (21%) | 13 (1.3%) | 354 (44%) | |
| 6 and more | 896 (20%) | 4 (0.5%) | 739 (43%) | 21 (2.1%) | 132 (16%) | |
| Unknown | 14 | 3 | 2 | 2 | 7 | |
| Leave alone | < 0.001 | |||||
| Yes | 894 (20%) | 93 (11%) | 407 (24%) | 230 (23%) | 164 (20%) | |
| No | 3,458 (78%) | 771 (88%) | 1,275 (74%) | 768 (76%) | 644 (79%) | |
| N/A | 59 (1.3%) | 9 (1.0%) | 30 (1.8%) | 12 (1.2%) | 8 (1.0%) | |
| Ability to isolate | < 0.001 | |||||
| Yes | 3,385 (77%) | 746 (85%) | 1,316 (77%) | 665 (66%) | 658 (81%) | |
| No | 904 (20%) | 109 (12%) | 349 (20%) | 307 (30%) | 139 (17%) | |
| N/A | 122 (2.8%) | 18 (2.1%) | 47 (2.7%) | 38 (3.8%) | 19 (2.3%) |
Statistics presented: n (%).
Statistical tests performed: Chi2 test of independence.
Psychological distress, social support and information, and drugs.
Regarding the K6 scale, 39% of students have moderate and 21% a high level of distress. Psychological distress is more important in young students (19–21 years old), in nurse students, in students living alone, and in students who can’t isolate themselves (Table 2 ).
Table 2.
Population repartition regarding Kessler'score.
| Characteristic/Number (percentage) | Overall N = 4500a |
Low (≤ 7) n = 1816a |
Moderate (8–12) n = 1729a |
High (≥ 13) n = 955a |
P-value* |
|---|---|---|---|---|---|
| Gender | |||||
| Women | 3537 (80%) | 1350 (75%) | 1395 (83%) | 792 (84%) | |
| Men | 863 (20%) | 443 (25%) | 276 (16%) | 144 (15%) | |
| Other | 11 (0.2%) | 3 (0.2%) | 6 (0.4%) | 2 (0.2%) | |
| Unknown | 89 | 20 | 52 | 17 | |
| Age | < 0.001 | ||||
| 19–21 | 753 (17%) | 254 (14%) | 269 (16%) | 230 (25%) | |
| 22–24 | 1760 (40%) | 688 (39%) | 731 (44%) | 341 (37%) | |
| 25–27 | 1001 (23%) | 427 (24%) | 385 (23%) | 189 (20%) | |
| 27 years and more | 844 (19%) | 399 (23%) | 280 (17%) | 165 (18%) | |
| Unknown | 142 | 48 | 64 | 30 | |
| Year of study | 0.007 | ||||
| 1–3 | 900 (20%) | 355 (20%) | 333 (19%) | 212 (22%) | |
| 4–5 | 3483 (77%) | 1428 (79%) | 1335 (77%) | 720 (75%) | |
| 6 and more | 117 (2.6%) | 33 (1.8%) | 61 (3.5%) | 23 (2.4%) | |
| Unknown | < 0.001 | ||||
| Leave alone | 3409 (76%) | 1487 (82%) | 1285 (74%) | 637 (67%) | |
| Yes | 911 (20%) | 276 (15%) | 367 (21%) | 268 (28%) | |
| No | 180 (4.0%) | 53 (2.9%) | 77 (4.5%) | 50 (5.2%) | |
| Specialty | < 0.001 | ||||
| Others | 873 (20%) | 349 (19%) | 366 (22%) | 158 (17%) | |
| Medecine | 1712 (39%) | 729 (41%) | 611 (36%) | 372 (40%) | |
| Nurse | 1010 (23%) | 365 (20%) | 394 (23%) | 251 (27%) | |
| Dental-pharmacist-midwife | 816 (18%) | 351 (20%) | 310 (18%) | 155 (17%) | |
| Unknown | 89 | 22 | 48 | 19 |
Statistics presented: n (%).
Statistical tests performed: Chi2 test of independence.
Then, we did a logistic regression between students with moderate or high levels of distress and students without (Table 3 ). Risk factors of psychological distress are being a woman (P < 0.001), being between 19 and 21 years old (P < 0.001), living alone (P = 0.008), and not having the ability to isolate (P < 0.001).
Table 3.
Logistic regression with socio-demographic data using Kessler scale (presence or absence of psychological distress) as a dependent variable.
| Characteristic | K6 |
Univariate analysis |
Multivarate analysis |
|||||
|---|---|---|---|---|---|---|---|---|
| No distress (K6 ≤ 7) n = 1816a |
Moderate or High distress (K6 > 7) n = 2684a |
ORb | 95% CIb | P-value | ORb | 95% CIb | P-value | |
| Gender | < 0.001 | < 0.001 | ||||||
| Women | 1350 (38%) | 2187 (62%) | — | — | — | — | ||
| Men | 443 (51%) | 420 (49%) | 0.59 | 0.50, 0.68 | 0.59 | 0.51, 0.70 | ||
| Other | 3 (27%) | 8 (73%) | 1.65 | 0.48, 7.52 | 1.44 | 0.41, 6.66 | ||
| Unknown | 20 | 69 | ||||||
| Age | < 0.001 | < 0.001 | ||||||
| 19–21 | 254 (34%) | 499 (66%) | — | — | — | — | ||
| 22–24 | 688 (39%) | 1072 (61%) | 0.79 | 0.66, 0.95 | 0.78 | 0.65, 0.94 | ||
| 25–27 | 427 (43%) | 574 (57%) | 0.68 | 0.56, 0.83 | 0.67 | 0.55, 0.82 | ||
| 27 years and more | 399 (47%) | 445 (53%) | 0.57 | 0.46, 0.69 | 0.53 | 0.43, 0.66 | ||
| Unknown | 48 | 94 | ||||||
| Year of study | 0.015 | 0.008 | ||||||
| 1–3 | 355 (39%) | 545 (61%) | — | — | — | — | ||
| 4–5 | 1428 (41%) | 2055 (59%) | 0.94 | 0.81, 1.09 | 0.77 | 0.66, 0.91 | ||
| 6 and more | 33 (28%) | 84 (72%) | 1.66 | 1.09, 2.56 | 0.87 | 0.48, 1.59 | ||
| Unknown | < 0.001 | < 0.001 | ||||||
| Leave alone | 1487 (44%) | 1922 (56%) | — | — | — | — | ||
| Yes | 276 (30%) | 635 (70%) | 1.78 | 1.52, 2.08 | 1.93 | 1.63, 2.28 | ||
| No | 53 (29%) | 127 (71%) | 1.85 | 1.34, 2.59 | 1.57 | 1.05, 2.39 | ||
| Specialty | 0.004 | 0.75 | ||||||
| Others | 349 (40%) | 524 (60%) | — | — | — | — | ||
| Medecine | 729 (43%) | 983 (57%) | 0.90 | 0.76, 1.06 | 1.00 | 0.84, 1.20 | ||
| Nurse | 365 (36%) | 645 (64%) | 1.18 | 0.98, 1.42 | 1.07 | 0.88, 1.31 | ||
| Dental-pharmacist-midwife | 351 (43%) | 465 (57%) | 0.88 | 0.73, 1.07 | 0.96 | 0.79, 1.18 | ||
| Unknown | 22 | 67 | ||||||
Statistics presented: n (%).
OR: Odds Ratio; CI: Confidence Interval.
Regarding the numeric distress scale, one-third of the students have a moderate or high score; nurse and medical students have a higher score than dental/pharmacist/midwife and others health students and need more support (moderate/high need = 36% vs 26%). Medical students have better information on the support system. There is no difference at SPS 10 between groups: most students have a low score (Table 4 ).
Table 4.
Population repartition regarding numeric scales.
| Characteristic/Number (percentage) |
Overall n = 4411a |
Others n = 873a |
Medecine n = 1712a |
Nurse n = 1010a |
Dent-pharma-midwife n = 816a |
P-value* |
|---|---|---|---|---|---|---|
| Distress | 0.005 | |||||
| Low (0–4) | 3002 (68%) | 622 (72%) | 1140 (67%) | 662 (66%) | 578 (71%) | |
| Moderate (5–7) | 1209 (28%) | 228 (26%) | 488 (29%) | 288 (29%) | 205 (25%) | |
| High (8–10) | 175 (4.0%) | 18 (2.1%) | 78 (4.6%) | 49 (4.9%) | 30 (3.7%) | |
| Unknown | 25 | 5 | 6 | 11 | 3 | |
| Support information | < 0.001 | |||||
| Low (0–4) | 1291 (35%) | 287 (38%) | 382 (27%) | 384 (46%) | 238 (35%) | |
| Moderate (5–7) | 1510 (41%) | 299 (40%) | 623 (43%) | 301 (36%) | 287 (43%) | |
| High (8–10) | 896 (24%) | 160 (21%) | 430 (30%) | 157 (19%) | 149 (22%) | |
| Unknown | 714 | 127 | 277 | 168 | 142 | |
| Need for support | < 0.001 | |||||
| Low (0–4) | 2477 (67%) | 550 (73%) | 910 (63%) | 539 (64%) | 478 (71%) | |
| Moderate (5–7) | 907 (25%) | 157 (21%) | 387 (27%) | 209 (25%) | 154 (23%) | |
| High (8–10) | 315 (8.5%) | 45 (6.0%) | 137 (9.6%) | 94 (11%) | 39 (5.8%) | |
| Unknown | 712 | 121 | 278 | 168 | 145 | |
| Sleep quality | < 0.001 | |||||
| Low (0–4) | 1300 (35%) | 275 (37%) | 544 (38%) | 236 (28%) | 245 (36%) | |
| Moderate (5–7) | 1278 (34%) | 273 (36%) | 509 (35%) | 271 (32%) | 225 (33%) | |
| High (8–10) | 1148 (31%) | 203 (27%) | 392 (27%) | 347 (41%) | 206 (30%) | |
| Unknown | 685 | 122 | 267 | 156 | 140 | |
| SPS10 | 0.069 | |||||
| Low (≤ 20) | 2998 (83%) | 620 (85%) | 1187 (84%) | 643 (80%) | 548 (83%) | |
| Moderate (21–30) | 553 (15%) | 100 (14%) | 208 (15%) | 144 (18%) | 101 (15%) | |
| High (> 30) | 48 (1.3%) | 7 (1.0%) | 15 (1.1%) | 17 (2.1%) | 9 (1.4%) | |
| Unknown | 812 | 146 | 302 | 206 | 158 | |
| Substance use | < 0.001 | |||||
| No | 3094 (70%) | 666 (76%) | 1179 (69%) | 679 (67%) | 570 (70%) | |
| Yes | 592 (13%) | 80 (9.2%) | 250 (15%) | 164 (16%) | 98 (12%) | |
| Unknown | 725 (16%) | 127 (15%) | 283 (17%) | 167 (17%) | 148 (18%) | |
| Psychotropic treatments use | 0.2 | |||||
| No | 3361 (76%) | 693 (79%) | 1294 (76%) | 764 (76%) | 610 (75%) | |
| Yes | 323 (7.3%) | 53 (6.1%) | 139 (8.1%) | 71 (7.0%) | 60 (7.4%) | |
| Unknown | 727 (16%) | 127 (15%) | 279 (16%) | 175 (17%) | 146 (18%) |
Statistics presented: n (%).
Statistical tests performed: Chi2 test of independence.
Nurse and medical students used more non-medical psychotropic substances than other health students (15% vs 9.2%), and 7% used psychotropic drugs (Table 4).
Activity Restriction Impact
Two students’ groups can be distinguished: those who have direct contact with patients (“frontliners”) and those who don’t. Students without direct contact with patients can be divided into two subgroups: students in lockdown as the general population and without any clinical activity (45.7% of respondents) and students called “rearguard” (16% of respondents). These “rearguard” students were partially confined, but they maintained a certain clinical activity without direct contact with patients (by working on call centers, providing teleconsultations, helping social emergency rescue services) with patient control and contributing to clinical research).
The students in frontline had their care activity maintained in different sectors: medical emergency, intensive care, geriatrics (or residences for dependent seniors), in units dedicated (or not) to patients suffering from COVID-19, psychiatry, palliative care, as well as in outpatient facilities (doctors’ offices, pharmacies, laboratories,…). Students in the frontline are older (58% versus 30.1% have more than 25 years old, P < 0.001) and mainly medical students (47%) and nurses/midwife students (44%). They have less psychological distress (57 vs 62%, P = 0.003), better quality of sleep (34% vs 28% high quality, P < 0.001) but a higher consumption of medical (8.5% vs 6.5%, P = 0.044) and non-medical (18% vs 10%, P < 0.001) psychotropic drugs (Table 5 ).
Table 5.
Numeric scales regarding contact with patients.
| Characteristic/number (percentage) |
A, n = 2400a | B, n = 1969a | P-value* | Overall, n = 4369a |
|---|---|---|---|---|
| Gender | 0.10 | |||
| Women | 1927 (81%) | 1545 (79%) | 3472 (80%) | |
| Men | 450 (19%) | 406 (21%) | 856 (20%) | |
| Other | 8 (0.3%) | 2 (0.1%) | 10 (0.2%) | |
| Unknown | 15 | 16 | 31 | |
| Age | < 0.001 | |||
| 19–21 | 536 (23%) | 181 (9.5%) | 717 (17%) | |
| 22–24 | 1110 (47%) | 611 (32%) | 1721 (40%) | |
| 25–27 | 481 (21%) | 506 (26%) | 987 (23%) | |
| 27 years and more | 213 (9.1%) | 616 (32%) | 829 (19%) | |
| Unknown | 60 | 55 | 115 | |
| Specialty | < 0.001 | |||
| Others | 794 (33%) | 51 (2.6%) | 845 (19%) | |
| Medecine | 784 (33%) | 909 (47%) | 1693 (39%) | |
| Nurse | 237 (9.9%) | 760 (39%) | 997 (23%) | |
| Dent-pharma-midwife | 568 (24%) | 233 (12%) | 801 (18%) | |
| Unknown | 17 | 16 | 33 | |
| K6 Score | 0.002 | |||
| No distress (K6 ≤ 7) | 924 (38%) | 847 (43%) | 1771 (41%) | |
| Moderate or high distress (K6 > 7) | 1476 (62%) | 1122 (57%) | 2598 (59%) | |
| Distress | 0.7 | |||
| Low (0–4) | 1627 (68%) | 1343 (69%) | 2970 (68%) | |
| Moderate (5–7) | 670 (28%) | 531 (27%) | 1201 (28%) | |
| High (8–10) | 91 (3.8%) | 82 (4.2%) | 173 (4.0%) | |
| Unknown | 12 | 13 | 25 | |
| Support information | 0.006 | |||
| Low (0–4) | 847 (42%) | 648 (39%) | 1495 (41%) | |
| Moderate (5–7) | 502 (25%) | 385 (23%) | 887 (24%) | |
| High (8–10) | 657 (33%) | 629 (38%) | 1286 (35%) | |
| Unknown | 394 | 307 | 701 | |
| Need for support | > 0.9 | |||
| Low (0–4) | 1343 (67%) | 1107 (67%) | 2450 (67%) | |
| Moderate (5–7) | 498 (25%) | 410 (25%) | 908 (25%) | |
| High (8–10) | 167 (8.3%) | 144 (8.7%) | 311 (8.5%) | |
| Unknown | 392 | 308 | 700 | |
| Sleep quality | < 0.001 | |||
| Low (0–4) | 758 (37%) | 531 (32%) | 1289 (35%) | |
| Moderate (5–7) | 700 (35%) | 566 (34%) | 1266 (34%) | |
| High (8–10) | 568 (28%) | 572 (34%) | 1140 (31%) | |
| Unknown | 374 | 300 | 674 | |
| SPS10 | 0.10 | |||
| Low (≤ 20) | 1631 (83%) | 1340 (84%) | 2971 (83%) | |
| Moderate (21–30) | 316 (16%) | 235 (15%) | 551 (15%) | |
| High (> 30) | 20 (1.0%) | 28 (1.7%) | 48 (1.3%) | |
| Unknown | 433 | 366 | 799 | |
| Substance use | < 0.001 | |||
| No | 1761 (73%) | 1305 (66%) | 3066 (70%) | |
| Yes | 245 (10%) | 345 (18%) | 590 (14%) | |
| Unknown | 394 (16%) | 319 (16%) | 713 (16%) | |
| Psychotropic treatments use | 0.044 | |||
| No | 1850 (77%) | 1480 (75%) | 3330 (76%) | |
| Yes | 394 (16%) | 322 (16%) | 716 (16%) | |
| Unknown | 156 (6.5%) | 167 (8.5%) | 323 (7.4%) |
Statistics presented: n (%).
Statistical tests performed: Chi2 test of independence.
Discussion
Our study found significative differences between specialities with higher symptoms in nurse/midwife and medical students than in others health students. Nevertheless, a huge number of the students have elevated levels of stress on the K6 scale, bad quality of sleep and low information on the support system. The strength of our study is to look at all health students and not only medical and nurses, and to seek to understand the specificities of health students.
More than half of the students have been enlisted to work with patients during France's first wave of COVID-19. These students, who were in direct contact with patients, had an average score on Kessler's psychological distress scale, yet scored moderately but still significantly lower than students who were without clinical activity during lockdown (average scores are just below the threshold one what is considered as moderate psychological distress). However, frontline students reported quite significantly that their sleep quality decreased and their intake of psycho-stimulants (tobacco, alcohol) had increased. These results are in agreement with previous studies [30], [31].
Regarding students who were in lockdown, pedagogical reorganizations that allowed them to continue their curriculum online (online classes, digital…) were quickly proven to be limited regarding issues such as isolation, struggles with interactions and connections, risks of dropout and strong doubts regarding the quality of skills obtained through these methods. Regarding health care itself, care conditions have deteriorated dramatically, with departments that have been reorganized into makeshift intensive care wards, blurred responsibilities and roles, and sometimes faulty management, according to students. For midwife students, a French study found the importance for the mental health of work resources (work control and social support), interpersonal relationships and relationships with a clinical preceptor in training[32]. Many organizations have emphasized the importance of checking the well-being of health workers confronted with COVID-19 [22].
In addition to the psychological impact expected in this crisis context, half of them were directly involved with patients, thus fully experiencing the health crisis while also experiencing the impact on training or confinement experienced by any other student. This specific experience is expressed in particular by difficulties related to their mission as trainee carers: supervision is sometimes lacking due to teacher trainers who are themselves caught up in the pandemic and therefore even less available to support them (including on an academic level). Working in hospitals, they face death [31] and fear of contaminating their relatives, which is an additional risk factor for psychological disorders [33]. For some of them, however, this commitment seems to give meaning to their training, at least during the first wave, which might have contributed to some form of resilience for these future professionals and for some of them, this may have increased their motivation.
There are some limits to this study: the response rate was low, especially in some specialities. Sociodemographic characteristics were not similar to the general health student's population, with an over-representation of young health students and thus a risk of over-representation of students who were isolated during the first wave. Indeed, medical students who were the most advanced in their curriculum and residents were more frequently enlisted to work with patients. The estimated differences are small but indicative in this particular context of a health crisis of this magnitude. However, the specificity of students lies especially in the training objective they must complete besides their responsibilities as caregivers, which are exacerbated by the epidemic context.
Conclusion
COVID 19's crisis had multiple consequences for health students: psychological but also educational with the closure of universities, breaking the link with colleagues and teachers. However, their status as health professionals in training through their commitment to patient care also meant that they were affected by a deadly viral pandemic. Teachers themselves, overwhelmed by the demands of care, may not always have provided the necessary support, especially as they are also exposed to the impact on their own mental and physical health. We also know that a health crisis's physical and psychological effects on carers often take one to two years to reveal themselves. There is a risk of a deterioration in the motivation, training and commitment of health students to their course, with a likely increased dropout rate. There is an urgent need for psychological and pedagogical support for health students, even more in this pandemic crisis, with financial and human means.
Contribution of authors
All authors contributed equally to this work.
Disclosure of interest
Franck Rolland, Gilles Bertschy, Bertrand Diquet and Donata Marra are members of the executive committee of the National Support Center for the Quality of Life of Health Students. Ariel Frajerman is a psychiatric resident and a PhD student.
Acknowledgements
All health students and their representative associations (ANEMF, ANEP, ANEPF, ANESF, FFEO, FNEK, FNEO, FNESI, FNSIP-BM, ISNAR-IMG, ISNI, UNAEE, UNECD, FAGE, FNEA).
Eléonore Herscovici-Missistrano for English translation.
References
- 1.Schernhammer E.S., Colditz G.A. Suicide rates among physicians: a quantitative and gender assessment (Meta-Analysis) AJP. 2004;161:2295–2302. doi: 10.1176/appi.ajp.161.12.2295. [DOI] [PubMed] [Google Scholar]
- 2.Rotenstein L.S., Torre M., Ramos M.A., et al. Prevalence of burnout among physicians: a systematic review. JAMA. 2018;320:1131–1150. doi: 10.1001/jama.2018.12777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rotenstein L.S., Ramos M.A., Torre M., et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. JAMA. 2016;316:2214–2236. doi: 10.1001/jama.2016.17324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Frajerman A., Morvan Y., Krebs M.-O., et al. Burnout in medical students before residency: A systematic review and meta-analysis. European Psychiatry. 2019;55:36–42. doi: 10.1016/j.eurpsy.2018.08.006. [DOI] [PubMed] [Google Scholar]
- 5.Muniz F.W.M.G., Maurique L.S., Toniazzo M.P., et al. Self-reported depressive symptoms in dental students: systematic review with meta-analysis. J Dent Educ. 2021;85(2):135–147. doi: 10.1002/jdd.12408. [DOI] [PubMed] [Google Scholar]
- 6.Tung Y.-J., Lo K.K.H., Ho R.C.M., et al. Prevalence of depression among nursing students: a systematic review and meta-analysis. Nurse Educ Today. 2018;63:119–129. doi: 10.1016/j.nedt.2018.01.009. [DOI] [PubMed] [Google Scholar]
- 7.Oates J., Topping A., Arias T., et al. The mental health and wellbeing of midwifery students: an integrative review. Midwifery. 2019;72:80–89. doi: 10.1016/j.midw.2019.02.007. [DOI] [PubMed] [Google Scholar]
- 8.Enquête « Votre bien-être, parlons en ! » Union nationale des etudiants en chirurgie dentaire n.d. https://www.unecd.com/dossier_presse/enquete-votre-bien-etre-parlons-en/ [accessed June 28, 2021].
- 9.Résultats de l’enquête de l’ANEPF sur le bien-être des étudiants en pharmacie (Communiqué) – Toute La Veille Acteurs de Santé n.d. https://toute-la.veille-acteurs-sante.fr/139592/resultats-de-lenquete-bien-etre-des-etudiants-en-pharmacie-communique/ [accessed June 28, 2021].
- 10.Marra D. Ministère des solidarités et de la santé; 2018. Rapport sur la qualité de vie des étudiants en santé. [Google Scholar]
- 11.Cucinotta D., Vanelli M. WHO declares COVID-19 a pandemic. Acta Bio Medica Atenei Parmensis. 2020;91:157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Andersen K.G., Rambaut A., Lipkin W.I., et al. The proximal origin of SARS-CoV-2. Nat Med. 2020;26:450–452. doi: 10.1038/s41591-020-0820-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Salje H., Kiem C.T., Lefrancq N., et al. 2020. Estimating the burden of SARS-CoV-2 in France; p. 44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lai J., Ma S., Wang Y., et al. Factors associated with mental health outcomes among health care workers exposed to Coronavirus Disease 2019. JAMA Netw Open. 2020;3:e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Capdevila X. Pandémie au virus SARS-CoV-2 en France : l’histoire d’une adaptation hors normes des soignants. Anesth Reanim. 2020;6(3):281–282. doi: 10.1016/j.anrea.2020.05.001. [DOI] [Google Scholar]
- 16.Zhang W., Wang K., Yin L., et al. PPS; 2020. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China; pp. 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rossi R., Socci V., Pacitti F., et al. Mental health outcomes among front and second line health workers associated with the COVID-19 pandemic in Italy. MedRxiv. 2020 doi: 10.1101/2020.04.16.20067801. [2020.04.16.20067801] [DOI] [Google Scholar]
- 18.Saddik B., Hussein A., Sharif-Askari F.S., et al. Increased levels of anxiety among medical and non-medical university students during the COVID-19 pandemic in the United Arab Emirates. MedRxiv. 2020 doi: 10.1101/2020.05.10.20096933. [2020.05.10.20096933] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.El-Hage W., Hingray C., Lemogne C., et al. Les professionnels de santé face à la pandémie de la maladie à coronavirus (COVID-19) : quels risques pour leur santé mentale? L’Encéphale. 2021;46(3):s73–s80. doi: 10.1016/j.encep.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maunder R.G., Lancee W.J., Balderson K.E., et al. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg Infect Dis. 2006;12:1924–1932. doi: 10.3201/eid1212.060584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Greenberg N., Docherty M., Gnanapragasam S., et al. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ. 2020;368:m1211. doi: 10.1136/bmj.m1211. [DOI] [PubMed] [Google Scholar]
- 22.Mulin E., Trouillet I., Gellato C. N’oublions pas le moral des « troupes » ! La santé mentale des soignants et l’impact psychiatrique de la pandémie de covid-19. Encéphale. 2020;46(3):s125. doi: 10.1016/j.encep.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Australian Medical Association; 2020. Joint Statement - COVID-19 impact likely to lead to increased rates of suicide and mental illness. https://www.ama.com.au/media/joint-statement-covid-19-impact-likely-lead-increased-rates-suicide-and-mental-illness [accessed June 28, 2021] [Google Scholar]
- 24.Azoulay E., Cariou A., Bruneel F., et al. Symptoms of anxiety, depression, and peritraumatic dissociation in critical care clinicians managing patients with COVID-19. A Cross-Sectional Study. Am J Respir Crit Care Med. 2020;202:1388–1398. doi: 10.1164/rccm.202006-2568OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wathelet M., Duhem S., Vaiva G., et al. Factors associated with mental health disorders among university students in France confined during the COVID-19 Pandemic. JAMA Network Open. 2020;3:e2025591. doi: 10.1001/jamanetworkopen.2020.25591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kessler R.C., Green J.G., Gruber M.J., et al. Screening for serious mental illness in the general population with the K6 screening scale: results from the WHO World Mental Health (WMH) survey initiative. Int J Methods Psychiatr Res. 2010;19:4–22. doi: 10.1002/mpr.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kessler R.C., Andrews G., Colpe L.J., et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32:959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- 28.COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398(10312):1700–1712. doi: 10.1016/S0140-6736(21)02143-7. [S0140-6736(21)02143-7]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Caron J. [A validation of the Social Provisions Scale: the SPS-10 items] Sante Ment Que. 2013;38:297–318. doi: 10.7202/1019198ar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wathelet M., Duhem S., Vaiva G., et al. Factors associated with mental health disorders among university students in France confined during the COVID-19 pandemic. JAMA Network Open. 2020;3:e2025591. doi: 10.1001/jamanetworkopen.2020.25591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Serrano-Ripoll M.J., Meneses-Echavez J.F., Ricci-Cabello I., et al. Impact of viral epidemic outbreaks on mental health of healthcare workers: a rapid systematic review and meta-analysis. J Affect Disord. 2020;277:347–357. doi: 10.1016/j.jad.2020.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ferrand C., Courtois R., Martinent G., et al. Relationships between work-related characteristics, needs satisfaction, motivation and mental health in midwifery students. Psychol Health Med. 2017;22:711–718. doi: 10.1080/13548506.2016.1220597. [DOI] [PubMed] [Google Scholar]
- 33.El-Hage W., Hingray C., Lemogne C., et al. Les professionnels de santé face à la pandémie de la maladie à coronavirus (COVID-19) : quels risques pour leur santé mentale ? L’Encéphale. 2020;46:S73–S80. doi: 10.1016/j.encep.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]