Abstract
Purpose
The COVID-19 pandemic has heightened the need for mental healthcare that can be delivered remotely and at scale to college students. This study evaluated the efficacy of online self-help for stress among students during the pandemic.
Method
College students with moderate or higher stress (N = 585) were recruited between November 2020 and February 2021, when COVID-19 had a major impact on colleges. Participants were randomly assigned to receive either online self-help using cognitive-behavioral therapy and positive psychology principles to support resilience and coping with pandemic-related stressors (n = 301) or referral to usual care (n = 284). Stress (primary outcome), depression, and anxiety (secondary outcomes) were assessed at pretreatment, one-month post-treatment, and three-month follow-up.
Results
Participants in the online self-help condition experienced significantly larger reductions in stress (d = –0.18, p = .035) and depression (d = –0.20, p = .018) from pretreatment to post-treatment than participants in the referral group. Reductions in stress from pretreatment to follow-up were also larger in the treatment versus referral group (d = –0.23, p = .005). Groups did not differ in change in anxiety. More time using the self-help program predicted greater improvement in depression at post-treatment (d = –0.41, p = .001) and follow-up (d = –0.32, p = .007), although usage was unrelated to change in stress or anxiety.
Conclusion
Online self-help targeting resilience and coping during the pandemic appears efficacious for long-term alleviation of stress and short-term alleviation of depression symptoms among the college students.
Registration
Keywords: COVID-19, Stress, Self-help, Cognitive-behavioral therapy, Positive psychology
Implications and Contribution.
The COVID-19 pandemic heightened the need for remote and scalable mental health interventions, especially among students. Online self-help reduced stress and depression and could have a significant impact if provided at scale.
See Related Editorial on p.141
COVID-19 has caused over 260 million infections and over 7.7 million deaths worldwide as of December 2021. [1] The pandemic has also caused major economic disruption, and efforts to limit contagion have profoundly changed lifestyles. Consequently, research has indicated heightened mental health concerns among adolescents during the pandemic. [2] Despite these concerns, traditional mental healthcare services, such as in-person counseling, have posed infection risk. The pandemic has, therefore, caused a surge of need for mental health services that can be delivered remotely and at scale.
College students are a subsection of the adolescent population that is particularly in need of safe and scalable mental healthcare during the pandemic. Sawyer et al. have argued that adolescence should be defined as around ages 10–24 years, corresponding more closely to adolescent growth, and therefore, an age range of 18–24, the typical age of college students, maps onto this period of substantial social and neurological maturation. [3] Research has suggested heightened mental health vulnerability among college students, especially during the pandemic. For example, before the pandemic, 27% of college students reported moderate or higher stress. [4] Furthermore, students’ stress and mood disorder symptoms rose during the pandemic, suggesting deteriorating mental health among an already vulnerable group of adolescents. [5,6] Although many college counseling centers expanded teletherapy services during the pandemic, [7] such counseling centers have been historically overwhelmed by demand for services, [8] and the increase in mental health problems likely exacerbated this challenge. Furthermore, some counseling centers might not have been licensed to deliver teletherapy to students attending school remotely while living in different states. Evaluating alternative methods for providing care to college students is a public health priority.
Online self-help interventions, in which users guide themselves through therapeutic content delivered via the internet, could meet the need for remote and scalable mental healthcare among college students. Online self-help interventions are effective in addressing a range of child and adolescent mental health problems, [9] including among college students. [10] Accordingly, researchers have suggested using online self-help programs to support mental health during the pandemic, [11] and some college counseling centers have expanded online self-help resources offered to students. [12] However, arguments in favor of online self-help have relied exclusively on studies conducted before the pandemic. The few randomized controlled trials (RCTs) examining online self-help during the pandemic have provided inconclusive results. One large trial (N = 670) found that a cognitive-behavioral therapy (CBT)-based online intervention targeting worry caused improvements in pandemic-related anxiety relative to a waiting list control, [13] whereas one smaller trial (N = 120) found that an expressive writing intervention did not improve stress, depression, or anxiety relative to treatment as usual. [14] Furthermore, neither study targeted adolescents or college students, instead targeting the general adult population. Evaluating online self-help among students is important to support the use of these interventions among students during both the pandemic and future crises affecting entire campus populations (e.g., other pandemics, disasters).
Online interventions should use evidence-based techniques to support resilience and coping with pandemic-related stressors. Positive psychology approaches that help people develop a sense of purpose, harness strengths, and foster social connections may be beneficial for promoting resilience to stress. [15] Intervention studies have suggested that targeting these constructs can support mental health during times of stress, [16,17] and perceptions of purpose, strengths, and support have been associated with better mental health in studies conducted during the pandemic. [15] Additionally, traditional and third-wave CBT techniques such as relaxation, problem-solving, and mindfulness have substantial support as methods to provide online intervention for stress, anxiety, and depression, [18] and they are likely to benefit students during the pandemic. Finally, to aid with pandemic-specific stressors (e.g., isolation, illness risk), it is important to help students identify coping strategies that can be pursued without the risk of contracting COVID-19. [19] Because the pandemic’s effects on mental health likely vary across students, intervention components should be accessible at the pace and order of students’ choices.
The purpose of this study was to test the efficacy of online self-help for college students facing stress during the COVID-19 pandemic. U.S. students with moderate or higher stress during the pandemic were randomly assigned to receive (1) access to a CBT-based and positive psychology-based online self-help program designed to support resilience and coping with pandemic-related stressors or (2) referral for usual care. Stress, depression, and anxiety were assessed at pretreatment, one-month post-treatment, and three-month follow-up. We predicted that the treatment group would experience larger reductions across outcome measures than the referral group.
Method
Participants
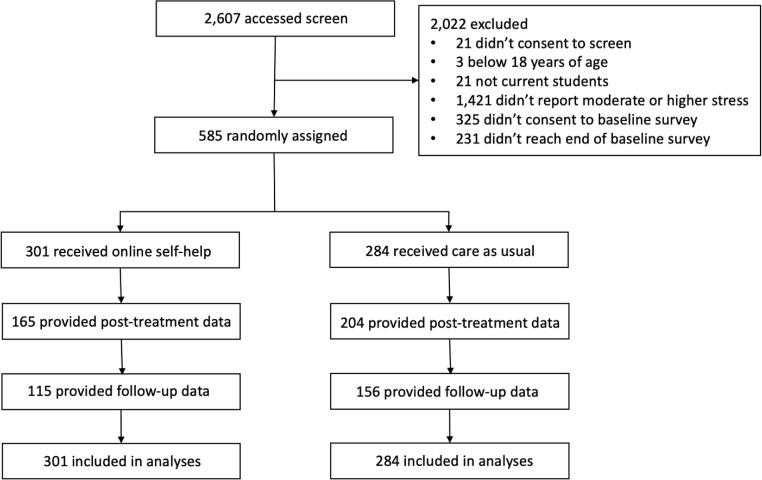
The sample included 585 college or university students who reported moderate or higher stress during the COVID-19 pandemic. There were participants from 25 U S. schools. Participants were randomly assigned to either online self-help (n = 301) or referral for usual care (n = 284).
Procedure
The study was registered on ClinicalTrials.gov (NCT04762173) and approved by the IRB of the corresponding author’s institution. Please see Figure 1 for a CONSORT diagram. Participants were recruited between November 2020 and February 2021. To be eligible, participants had to currently be a student at a U.S. college or university, 18 years or older, and score moderately or higher on the stress subscale of the Depression Anxiety Stress Scales-Short Form. [20,21] These criteria were assessed in an online Qualtrics screening survey that was emailed to students who had provided consent to be contacted regarding additional research opportunities while participating in a screening survey for another project (NCT04162847) and/or whose university administrators had approved survey invitations. In total, 56,939 students received invitations. Furthermore, advertisements for the study were posted in an online research participation bulletin, as well as Reddit forums for students at various colleges (54 forums total). Advertisements provided an email address that interested participants could contact to receive the screening survey. Recruitment materials informed potential participants that the researchers were studying student mental health during the pandemic and how online programs could be used to support mental health. Potential participants were informed that they would be asked to complete a survey that would indicate their eligibility for a second phase of the study involving assignment to one of two conditions designed to support mental health.
Figure 1.
Participant recruitment, randomization, assessment, and analysis summary.
The screening survey showed participants an informed consent document and then assessed eligibility for the RCT. Participants fulfilling screening criteria were informed of their eligibility for the RCT and invited to the online pretreatment survey for the RCT. The pretreatment survey began with an informed consent document, followed by demographic and mental health measures. At the end of the pretreatment survey, participants were informed of their condition. Simple, parallel (1:1) random assignment was performed automatically using Qualtrics’ randomizer; thus, experimenters were blind to allocation. Participants had to reach the end of the pretreatment survey to be randomized and included in the RCT. Participants were emailed the post-treatment survey one month after random assignment and emailed the follow-up survey three months after random assignment. Because all assessments were conducted with online surveys, assessors were blind to condition.
Self-help condition
Participants in the treatment condition were informed that they were selected to receive access to two programs to support mental health during the pandemic on SilverCloud Health. They were provided a link that they could use to create an account on SilverCloud Health and begin using the programs. Programs included several individual modules, each designed to take 20–30 minutes to complete. One program, “Space for Resilience,” used positive psychology principles to support mental health in the face of stress. The “Space for Resilience” program included seven modules: Building Resilience, Purpose, Self, Connection, Body, Mind, and Moving Forward. Modules are outlined in Table 1 . Each module closed with personal stories outlining ways people have put the content into practice, as well as a mindfulness exercise. The other program, “Space from COVID-19,” was guided by the mass trauma intervention principles proposed by Hobfoll and colleagues: [19] promoting a sense of safety, calming, self-efficacy and community-efficacy, connectedness, and hope. These goals were targeted using CBT and grief therapy techniques. The “Space from COVID-19” program included five modules: Challenging Times, Sleep Difficulties, Relaxation, Mindfulness, and Grief and Loss. Modules are outlined in Table 2 . Participants could access the modules at the pace and order of their choosing, and they could switch between the two programs at any time.
Table 1.
Description of Space for Resilience Program
| Module | Goals | Content |
|---|---|---|
| Building resilience | Orientation to the program |
|
| Purpose | Help users identify sources of purpose |
|
| Self | Promote positive sense of self |
|
| Connections | Enhance utilization of social network |
|
| Body | Build healthy habits |
|
| Mind | Promote balanced optimism |
|
| Moving forward | Summarizing and putting skills into action |
|
Note. Participants in the treatment condition had access to both the Space for Resilience and Space from COVID-19 programs.
Table 2.
Description of Space from COVID-19 Program
| Module | Goals | Content |
|---|---|---|
| Challenging times | Normalize and guide coping with pandemic-related stress |
|
| Sleep difficulties | Promote healthy sleep |
|
| Relaxation | Promote relaxation habits |
|
| Mindfulness | Introduce and train in mindfulness |
|
| Grief and loss | Promote coping with grief |
|
Note. Participants in the treatment condition had access to both the Space for Resilience and Space from COVID-19 programs.
Referral condition
Participants in the control condition were informed that they were selected to receive information about available counseling services. Participants were provided a link to the Substance Abuse and Mental Health Services Administration treatment locator, which provides a directory of mental healthcare providers for any zip code in the United States. Participants were also shown a list of college counseling centers that enabled students to find their school’s counseling center information. A phone number and/or website was provided for each school counseling center. All participants’ school counseling centers provided in-person and/or remote counseling services during the pandemic.
Measures
The screening and primary outcome measure was stress assessed using the stress subscale of the Depression Anxiety Stress Scales-Short Form (DASS). [20] The DASS stress subscale consists of seven statements about stress in the past week, rated from 0 (Did not apply to me at all) to 3 (Applied to me very much, or most of the time). Item scores were summed and doubled to correspond with the full-length DASS. Participants were eligible if they scored 20 or higher, indicating moderate or greater stress. [21] Secondary outcome measures included anxiety and depression, assessed with seven-item subscales on the DASS. The DASS possesses excellent construct validity. [20] Cronbach’s alpha was .76 for stress, .81 for anxiety, and .91 for depression. The pretreatment survey also collected the following background information: gender, racial/ethnic minority status, sexual orientation, age, year in school, school geographic region, school sector (private vs. public), whether students were living away from college during the pandemic, and perceived change in mental healthcare access due to the pandemic.
Planned analyses
As a preliminary analysis, we compared the treatment and control groups on all baseline symptoms and demographic characteristics using t-tests (for continuous variables) and chi-square tests (for categorical variables). We also computed rates of missing data at post-treatment and follow-up and tested if treatment condition or any baseline symptom or demographic characteristic predicted the probability of having missing data using logistic regression.
Symptom changes over time were compared across conditions using robust multilevel modeling in the R package robustlmm. [22] Robust multilevel modeling accounts for nonindependent repeated measurements and provides valid inferences in the presence of outliers. Models included main effects of time (pretreatment vs. post-treatment; pretreatment vs. follow-up) and condition (self-help vs. referral), as well as interactions between time and condition. Models also included fixed and random intercepts. Interactions were probed using simple slope analyses to examine symptom change over time in each condition. Missing data were handled using full information maximum likelihood estimation (FIML) under the missing at random assumption, which states that data are missing randomly after controlling for observed data. [23] This assumption is rendered feasible when background variables, termed “auxiliary variables,” are included in analytic models. [23] Therefore, models included fixed covariate effects of all background variables (gender, racial/ethnic minority status, sexual orientation, age, year in school, school geographic region, school sector, whether students were living away from college during the pandemic, and perceived change in mental healthcare access during the pandemic). Cohen’s d was calculated from Z statistics as: . [24] Analyses were intent-to-treat, incorporating every participant.
We conducted exploratory analyses to understand the usage of the self-help program within the treatment group. We computed descriptive statistics for the following usage characteristics: uptake, defined as the proportion of participants who created accounts on the program; the total number of visits to the program among those who created accounts; and total time spent on the program among those who created accounts. Additionally, to examine if the rate of program uptake affected results, we re-fit the main analysis models limited to treatment group participants who created accounts on the platform (and all control group participants). Finally, within the treatment group, to test how usage related to outcome, we fit robust multilevel models in which stress, depression, and anxiety were regressed on time (pretreatment to post-treatment; pretreatment to follow-up), usage characteristics (total time using the program; the number of logins to the program), and the interactions between the usage characteristics and time.
Power analysis
The study was designed to achieve 85% power to detect a difference in symptom change from pretreatment to post-treatment across conditions, assuming Cohen’s d of .35 with an alpha of .05. To accommodate the high proportion of missing data common in online self-help intervention studies, [25] we assumed 35% of data would be missing at post-treatment. A 5,000 simulation study suggested that 580 participants provided 86.4% power; recruitment stopped within one week of enrolling the 580th participant.
Results
Preliminary analyses
Please see Table 3 for participant background characteristics and Table 4 for symptom levels at pretreatment, post-treatment, and follow-up. The age range was 18–57, and 544 (93%) participants were in the typical college ages of 18–24. There were no significant differences across conditions on any symptom or demographic variable at pretreatment, except that fewer treatment participants lived away from college ( = 5.23, p = .022, 38.9% vs. 48.6%). Because this variable was included as a covariate, all analyses controlled for this pretreatment difference.
Table 3.
Participant Baseline Characteristics
| Treatment |
Control |
|||
|---|---|---|---|---|
| n | % | n | % | |
| Gender | ||||
| Male | 65 | 21.59 | 52 | 18.31 |
| Female | 216 | 71.76 | 217 | 76.41 |
| Gender minority | 20 | 6.64 | 15 | 5.28 |
| Sexual orientation | ||||
| Heterosexual | 188 | 62.5 | 182 | 64.1 |
| LGB+ | 113 | 37.5 | 102 | 35.9 |
| Racial/ethnic minority status | ||||
| Minority | 83 | 27.6 | 91 | 32.0 |
| Nonminority | 214 | 71.1 | 185 | 65.1 |
| Year in School | ||||
| Undergraduate year 1 | 116 | 38.5 | 96 | 33.8 |
| Undergraduate year 2 | 92 | 30.1 | 96 | 33.8 |
| Undergraduate year 3 | 57 | 18.9 | 50 | 17.6 |
| Undergraduate year 4 | 20 | 6.6 | 33 | 11.6 |
| Other | 16 | 5.3 | 9 | 3.2 |
| Living away from college | ||||
| Yes | 117 | 38.9 | 138 | 48.6 |
| No | 184 | 61.1 | 146 | 51.4 |
| School region | ||||
| Northeast | 197 | 65.4 | 171 | 60.2 |
| Midwest | 10 | 3.3 | 13 | 4.6 |
| South | 84 | 27.9 | 91 | 32.9 |
| West | 10 | 3.3 | 9 | 3.2 |
| School sector | ||||
| Public | 282 | 93.7 | 268 | 94.3 |
| Private | 19 | 6.3 | 16 | 5.6 |
| Change in mental healthcare access | ||||
| Much less limited access | 2 | 0.7 | 4 | 16.9 |
| Somewhat less limited access | 13 | 4.3 | 12 | 4.2 |
| No change | 76 | 25.2 | 85 | 29.9 |
| Somewhat more limited access | 112 | 37.2 | 97 | 34.2 |
| Much more limited access | 50 | 16.6 | 41 | 14.4 |
| Do not know | 48 | 15.9 | 45 | 15.8 |
| M | SD | M | SD | |
| Age | 20.24 | 4.13 | 20.65 | 4.88 |
Table 4.
Pretreatment, Post-treatment, and Follow-up Symptoms by Condition
| Measure | Treatment |
Control |
||||
|---|---|---|---|---|---|---|
| Pretreatment |
Post-treatment |
Follow-up |
Pretreatment |
Post-treatment |
Follow-up |
|
| M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | |
| Stress | 28.77 (6.12) | 22.98 (9.64) | 21.77 (9.87) | 28.04 (6.15) | 23.84 (9.18) | 23.57 (9.20) |
| Anxiety | 21.11 (9.26) | 15.82 (10.81) | 15.98 (10.46) | 19.84 (9.34) | 15.60 (10.17) | 15.63 (10.14) |
| Depression | 25.83 (10.34) | 19.90 (12.32) | 19.86 (12.08) | 24.31 (10.65) | 20.80 (11.98) | 20.71 (11.79) |
Note. N = 585. Stress, Anxiety, and Depression scores had a possible range of 0–42.
Survey completion rates were 63.0% at post-treatment and 46.1% at follow-up. Compared to participants in the referral condition, participants in the self-help condition were less likely to complete the post-treatment (Z = -4.32, p < .001; 71.8% vs. 54.8%) and follow-up (Z = -4.02, p < .001; 54.6% vs. 38.2%) assessments. We also found differences in rates of post-treatment and/or follow-up assessment completion as a function of gender, sexual orientation, school region, and perceived change in mental healthcare access due to the pandemic (outlined in Appendix A1). No baseline symptoms or background characteristics predicted the probability of missing post-treatment or follow-up data. Because the treatment group was a predictor in all models and all background characteristics were modeled as auxiliary variables, these patterns do not affect the validity of the analyses.
Main analyses
There was a significant interaction between pretreatment to post-treatment time and condition in the prediction of stress (ß = -1.84, SE = 0.87, Z = -2.11, p = .035, d = -0.18), showing that the self-help group improved significantly more during the acute treatment period than the control group. There was also a significant interaction between pretreatment to follow-up time and condition in the prediction of stress (ß = -2.78, SE = 0.99, Z = -2.82, p = .005, d = -0.23), showing that the self-help group also had greater long-term improvement than the control group. Simple slope analysis revealed that participants in the treatment condition experienced large reductions in stress from pretreatment to post-treatment (ß = –5.79, SE = 0.64, Z = –9.06, p < .001, d = –0.81) and pretreatment to follow-up (ß = –6.79, SE = 0.74, Z = –9.24, p < .001, d = –0.83), whereas participants in the referral condition experienced medium reductions in stress from pretreatment to post-treatment (ß = –3.95, SE = 0.59, Z = –6.66, p < .001, d = –0.57) and pretreatment to follow-up (ß = -4.01, SE = 0.66, Z = –6.12, p < .001, d = –0.52). Thus, online self-help was associated with larger stress reduction than referral for usual care during the acute treatment period, and these stress reductions were maintained at follow-up.
On secondary outcomes, there was also a significant interaction between pretreatment to post-treatment time and condition in the prediction of depression (ß = –2.26, SE = 0.96, Z = –2.36, p = .018, d = –0.20), showing greater improvement in the self-help condition, but no interaction between pretreatment to follow-up time and condition in the prediction of depression (ß = –0.96, SE = 1.09, Z = –0.88, p = .379, d = –0.07). Simple slope analysis revealed that participants in the treatment group experienced a medium to large reduction in depression from pretreatment to post-treatment (ß = –5.29, SE = 0.71, Z = –7.50, p < .001, d = –0.65), whereas participants in the control group experienced a small to medium reduction in depression (ß = –3.03, SE = 0.65, Z = –4.70, p < .001, d = –0.40). In predicting anxiety, there were not significant interactions between condition and pretreatment to post-treatment time (ß = –1.02, SE = 0.82, Z = –1.24, p = .215, d = –0.10) or pretreatment to follow-up time (ß = –0.89, SE = 0.93, Z = –0.96, p = .337, d = –0.08). Thus, online self-help recipients experienced a significantly larger reduction in depression during the acute treatment period, although depression improvements were not different across groups at follow-up. Moreover, groups did not differ in change in anxiety over time.
Exploratory analyses
Among the 301 participants in the treatment group, 158 accessed the self-help platform, indicating 52.5% uptake. Participants who accessed the platform averaged 2.04 total logins (SD = 2.57) and 13.58 total minutes logged in (SD = 33.50). Results from the analyses limited to treatment group participants who created accounts on the platform (and all control group participants) were identical to those from the main analyses (see Appendix A1). Within the treatment group, greater time using the program predicted greater reduction in depression from pretreatment to post-treatment (ß = –0.08, SE = 0.02, Z = –3.45, p = .001, d = –0.41), as well as greater reduction in depression from pretreatment to follow-up (ß = –0.06, SE = 0.02, Z = –2.72, p = .007, d = –0.32). No other usage characteristics predicted stress, depression, or anxiety changes (see Appendix A1). Thus, there was a dose-response relationship on depression but not on stress or anxiety, such that greater time using the self-help program was related to greater depression improvement.
Discussion
The results supported the efficacy of online self-help for stress in college students during the COVID-19 pandemic. Students who received access to online self-help experienced larger reductions in stress and depression during the acute treatment period than students who received referral information. The larger stress reductions in the treatment group were sustained at follow-up. Results did not favor the intervention for treating anxiety. Although effects sizes were small (0.18–0.23), they indicated potential for an important public health impact of self-help programs using positive psychology and CBT principles for students during the pandemic.
Online self-help was efficacious in treating stress and depression during the acute treatment period. The intervention group did not experience greater reductions in anxiety than the referral group, suggesting that the intervention might be less effective in treating anxiety. It is worth noting that anxiety was less elevated at pretreatment than stress and depression. Stress and depression may therefore be especially representative of mental health reactions during the pandemic and especially amenable to positive psychology and CBT-based stress management skills.
Stress reductions in the intervention group remained larger than those in the control group at three-month follow-up. Thus, the intervention appeared to promote durable improvements in stress. This finding suggests possible long-term benefits of providing online self-help programs to college students. Because the self-help programs emphasized building stress management habits, students might have continued to use the skills taught in the intervention after the one-month acute treatment period.
Within the self-help group, greater time spent using the program predicted a greater reduction in depression, indicating a dose-response relationship between usage time and depression improvement. This result converges with other findings that have suggested greater usage of online programs is associated with better depression outcomes. [26] Interestingly, there were no such dose-response relationships between usage metrics and improvement in stress or anxiety. Other trials have also found an absence of dose-response relationships between usage and outcome in online interventions for students, [27] suggesting that there is no single optimal usage profile. Further understanding the causes and consequences of online self-help usage is another important direction for future research.
Important limitations of this study deserve note. First, the control group received a referral, and we do not have data on how many of these students sought treatment. Although this control group allowed examining the efficacy of online self-help above and beyond available resources, it precluded addressing questions such as how online self-help compares to more intensive (yet potentially costly) interventions (e.g., teletherapy). Additionally, there was a high rate of missing post-treatment and follow-up data, and the rate of missing data differed across the treatment and control groups. Although both of these problems are common in internet intervention research, [25] and we used gold-standard methods for handling missing data, [23] collecting data from a greater proportion of the sample would strengthen generalizability.
In conclusion, the present study suggested that online self-help is an efficacious method for reducing stress and depression among college students during the COVID-19 pandemic. Providing widespread access to online self-help based on CBT and positive psychology principles could help alleviate widespread mental health symptoms in the student population during the pandemic and future campus-wide crises.
Acknowledgments
We thank Derek Richards, Angel Enrique, and SilverCloud Health for providing access to the online self-help programs evaluated in this study.
Contributions: Gavin N. Rackoff and Michelle G. Newman designed the study. Gavin N. Rackoff collected data, analyzed data, and drafted the manuscript under Michelle G. Newman’s supervision. Ellen E. Fitzsimmons-Craft, C. Barr Taylor, Daniel Eisenberg, Denise E. Wilfley, and Michelle G. Newman provided critical revisions.
Footnotes
Conflicts of interest: The authors have no conflicts of interest or financial disclosures.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.jadohealth.2022.01.227.
Funding Sources
This study was supported by National Institute of Mental Health grants R01MH115128 and K08MH120341, and the Department of Psychology, The Pennsylvania State University. The funding agencies are not responsible for any data collection, analysis, or interpretation in this manuscript. No author is being paid to write this article by a pharmaceutical company or other agency.
Supplementary Data
References
- 1.WHO WHO coronavirus disease (COVID-19) dashboard. World Health Organization. 2021. https://covid19.who.int/ Available at: [PubMed]
- 2.Guessoum S.B., Lachal J., Radjack R., et al. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 2020;291:113264. doi: 10.1016/j.psychres.2020.113264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sawyer S.M., Azzopardi P.S., Wickremarathne D., Patton G.C. The age of adolescence. Lancet Child Adolesc Health. 2018;2:223–228. doi: 10.1016/S2352-4642(18)30022-1. [DOI] [PubMed] [Google Scholar]
- 4.Bayram N., Bilgel N. The prevalence and socio-demographic correlations of depression, anxiety and stress among a group of university students. Soc Psychiatry Psychiatr Epidemiol. 2008;43:667–672. doi: 10.1007/s00127-008-0345-x. [DOI] [PubMed] [Google Scholar]
- 5.Charles N.E., Strong S.J., Burns L.C., et al. Increased mood disorder symptoms, perceived stress, and alcohol use among college students during the COVID-19 pandemic. Psychiatry Res. 2021;296:113706. doi: 10.1016/j.psychres.2021.113706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim H., Rackoff G.N., Fitzsimmons-Craft E.E., et al. College mental health before and during the COVID-19 pandemic: Results from a nationwide survey. Cognit Ther Res. 2021:1–10. doi: 10.1007/s10608-021-10241-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pierce B.S., Perrin P.B., Tyler C.M., et al. The COVID-19 telepsychology revolution: A national study of pandemic-based changes in U.S. Mental health care delivery. Am Psychol. 2021;76:14–25. doi: 10.1037/amp0000722. [DOI] [PubMed] [Google Scholar]
- 8.Brunner J.L., Wallace D.L., Reymann L.S., et al. College counseling Today: Contemporary students and how counseling centers meet their needs. J Coll Student Psychother. 2014;28:257–324. [Google Scholar]
- 9.Bennett S.D., Cuijpers P., Ebert D.D., et al. Practitioner review: Unguided and guided self-help interventions for common mental health disorders in children and adolescents: A systematic review and meta-analysis. J Child Psychol Psychiatry. 2019;60:828–847. doi: 10.1111/jcpp.13010. [DOI] [PubMed] [Google Scholar]
- 10.Harrer M., Adam S.H., Baumeister H., et al. Internet interventions for mental health in university students: A systematic review and meta-analysis. Int J Methods Psychiatr Res. 2019;28:e1759. doi: 10.1002/mpr.1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Razai M.S., Oakeshott P., Kankam H., et al. Mitigating the psychological effects of social isolation during the covid-19 pandemic. BMJ. 2020;369:m1904. doi: 10.1136/bmj.m1904. [DOI] [PubMed] [Google Scholar]
- 12.Petersen A. Colleges Brace for potential increased need for mental health services. Wall Street J. 2020 [Google Scholar]
- 13.Wahlund T., Mataix-Cols D., Olofsdotter Lauri K., et al. Brief online cognitive behavioural intervention for dysfunctional worry related to the COVID-19 pandemic: A randomised controlled trial. Psychother Psychosom. 2020:1–9. doi: 10.1159/000512843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Markovic M.V., Bjekic J., Priebe S. Effectiveness of expressive writing in the reduction of psychological distress during the COVID-19 pandemic: A randomized controlled trial. Front Psychol. 2020;11:1–11. doi: 10.3389/fpsyg.2020.587282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Waters L., Algoe S.B., Dutton J., et al. Positive psychology in a pandemic: Buffering, bolstering, and building mental health. J Posit Psychol. 2021 [Google Scholar]
- 16.Casellas-Grau A., Font A., Vives J. Positive psychology interventions in breast cancer. A systematic review. Psychooncology. 2014;23:9–19. doi: 10.1002/pon.3353. [DOI] [PubMed] [Google Scholar]
- 17.Enrique Roig A., Mooney O., Salamanca-Sanabria A., et al. Assessing the efficacy and acceptability of a web-based intervention for resilience among college students: Pilot randomized controlled trial. JMIR Form Res. 2020;4:e20167. doi: 10.2196/20167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Heber E., Ebert D.D., Lehr D., et al. The benefit of web- and computer-based interventions for stress: A systematic review and meta-analysis. J Med Internet Res. 2017;19:e32. doi: 10.2196/jmir.5774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hobfoll S.E., Watson P., Bell C.C., et al. Five essential elements of immediate and mid-term mass trauma intervention: Empirical evidence. Psychiatry. 2007;70:283–315. doi: 10.1521/psyc.2007.70.4.283. discussion 316-269. [DOI] [PubMed] [Google Scholar]
- 20.Antony M.M., Bieling P.J., Cox B.J., et al. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychol Assess. 1998;10:176–181. [Google Scholar]
- 21.Lovibond P.F., Lovibond S.H. Psychological Foundation of Australia, Inc.; Syndney, Australia: 1995. Manual for the depression anxiety stress scales. [Google Scholar]
- 22.Koller M. robustlmm: An R package for robust estimation of linear mixed-effects models. J Stat Softw. 2016;75:1–24. doi: 10.18637/jss.v075.i01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Graham J.W. Missing data analysis: Making it work in the real world. Annu Rev Psychol. 2009;60:549–576. doi: 10.1146/annurev.psych.58.110405.085530. [DOI] [PubMed] [Google Scholar]
- 24.Rosenthal R., DiMatteo M.R. Meta-analysis: Recent developments in quantitative methods for literature reviews. Annu Rev Psychol. 2001;52:59–82. doi: 10.1146/annurev.psych.52.1.59. [DOI] [PubMed] [Google Scholar]
- 25.Linardon J., Fuller-Tyszkiewicz M. Attrition and adherence in smartphone-delivered interventions for mental health problems: A systematic and meta-analytic review. J Consult Clin Psychol. 2020;88:1–13. doi: 10.1037/ccp0000459. [DOI] [PubMed] [Google Scholar]
- 26.Enrique A., Palacios J.E., Ryan H., Richards D. Exploring the relationship between usage and outcomes of an internet-based intervention for individuals with depressive symptoms: Secondary analysis of data from a randomized controlled trial. J Med Internet Res. 2019;21:e12775. doi: 10.2196/12775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Newman M.G., Jacobson N.C., Rackoff G.N., et al. A randomized controlled trial of a smartphone-based application for the treatment of anxiety. Psychother Res. 2021;31:443–454. doi: 10.1080/10503307.2020.1790688. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.