Abstract
There is no denying that the massive spread of COVID-19 around the world has worried everyone. The virus can cause mild to severe symptoms in various organs, especially the lungs. The virus affects oxidative stress in the cells. Reactive Oxygen Species modulator 1 (ROMO1) is one of the most important mitochondrial proteins that plays a critical regulatory role in the production of Reactive Oxygen Species (ROS). According to the studies, COVID-19 can promote oxidative stress through some important pathways, for instance, TNF-α and NF-κB routes. Furthermore, ROMO1 is closely related to these pathways and its dysfunction may affect these routes, then promote oxidative stress, and ultimately cause tissue damage, especially in the lungs. Another factor to consider is that the TNF-α and NF-κB pathways are associated with ROMO1, COVID-19, and oxidative stress. To summarize, it is hypothesized that COVID-19 may increase oxidative stress by affecting ROMO1. Understanding the exact molecular mechanisms of ROMO1 in the pathogenesis of COVID-19 can pave the way to find better therapeutic strategies.
Keywords: COVID-19, Reactive Oxygen Species, Reactive Oxygen Species Modulator 1, Oxidative Stress
INTRODUCTION
It is universally accepted that Corona Virus Disease-19 (COVID-19), also known as Acute Respiratory Disease-2019 or commonly known as Coronavirus (nCoV acute respiratory disease-2019), is an infectious disease, caused by Coronavirus Acute Respiratory Syndrome 2 (SARS-CoV-2).1 This disease is the cause of the recent pandemic.1 Common symptoms are fever, cough, shortness of breath, temporary loss of smell, muscle pain, sputum production, sore throat, nausea, and red eyes.2 Although, the majority of cases of the disease lead to mild symptoms, some cases progress to pneumonia and organ failure.2,3,4 Mortality rates are estimated at between 5% and 15%, however, this depends on age and other health conditions. The disease is mainly spread through tiny respiratory droplets to other people when people with COVID-19 cough or sneeze.3,4 The time between exposure to the disease and the onset of symptoms is about 2 to 14 days. It can be prevented by washing hands and other hygiene measures.4,5
One of the most important proteins that is involved in the production of Reactive Oxygen Species (ROS) is Reactive Oxygen Species modulator 1 (ROMO1).6,7 Also known as Glyrichin, it has 79 amino acids and is located in chromosomal locus of 20q11.22.6 ROMO1 is a mitochondrial protein that binds to some proteins of mitochondrial inner membrane and was first reported in various cancerous tissues which cause drug resistance.6 Furthermore, ROMO1, as an ROS-producing protein, has been observed in various cancers and has also been implicated in the invasion and progression of cancer cells.6 In addition to various neoplasms, ROMO1 is also involved in other diseases such as diabetes, respiratory diseases, and even infertility.6
ROSs are produced endogenously through the electron transfer pathway in mitochondria as well as in other metabolic pathways.6,8 External and environmental factors are also involved in the formation of ROS, including chemical intake and some types of radiation.6 Also, ROSs play a multiple part role in the normal cellular physiology processes, so certain levels of ROSs are required for normal cell function.6,8 Accumulation and changes in these molecules can play a dual role in cell function, which is related to the concentration of ROSs in a cell. Further, ROSs can over-activate certain signaling pathways, which may change a normal cell and cause mutations in the genes. As previous studies have shown, changed levels of ROS may cause cell damage, inflammation, and mutations in DNA, then can affect most organs and lead to various diseases.6,8
According to the significant effects of ROS, and the association of coronavirus and ROMO1 with oxidative stress, separately,5 it is possible that the virus may have an effect on this important mitochondrial protein, and increases ROSs and activate some critical pathways.5 As a consequence, the purpose of this article is to demonstrate the association between COVID-19 and ROMO1 with oxidative stress to understand the exact molecular mechanisms underlining of Coronavirus infection.
In this article, we used international databases such as Google Scholar, Web of Sciences, Scopus, and Pubmed, by using keywords including COVID-19, ROMO1, Oxidative Stress, ROS, Acute Respiratory Syndrome, and Diseases, and we found information about COVID-19, ROMO1, and their relationship to each other and oxidative stress.
COVID-19 AND OXIDATIVE STRESS
COVID-19 is rapidly spreading through the world and has affected almost very country.1 Most patients with SARS-CoV-2 have symptoms, but about 5% of these patients show severe lung damage and/or dysfunction of various organs such as the kidneys, and even they suffer from septic shock.9 Therefore, considering the country and its hospital facilities, the mortality rate is between 5% and 15%. In addition, patients with COVID-19, who are severely sick, often show severe clinical manifestations and a variety of metabolic disorders including poor peripheral pulses, metabolic acidosis, and impaired coagulation parameters (e.g., PT, INR, D.Dimer, FDP).5,10 There is however, strong evidence that this pandemic is declining in some countries due to the creation and distribution of several novel vaccines.
Recently, oxidative stress has been suggested as a crucial factor in COVID-19 and has many disturbing effects on the body.11,12 Furthermore, imbalance in the amount of oxidants and antioxidants has been observed in many medical afflictions, including, diabetes, cancer, infertility, and especially in lung diseases which causes increased oxidative stress and promotes tissue and cell damage in various organs.13 Anand et al.14 showed that the potent binding of SARS-CoV-2 to Angiotensin-Converting Enzyme 2 (ACE2) is about twice as high as in previous SARS-CoV viruses. This mechanism involves the activity of ACE2 on the octapeptide Angiotensin II (Ang II), which was previously triggered by ACE.15,16 Because Ang II is a vasoconstrictor and plays an important role in raising blood pressure, its processed by ACE2 dilates blood vessels and this process is highlighted by a vasodilator peptide called Angiotensin 1-7 (Ang 1-7).16,17 The binding of SARS-CoV-2 to ACE2 leads the virus to enter the cells and ultimately decreases the biological access of ACE2.17
Some previous studies have shown, when Ang II binds to Angiotensin Type 1 Receptor 1 (AT1R), it may affect and regulate Nicotinamide Adenine Dinucleotide Phosphate (NAD(P)H) Oxidase (NOX) activity.16,17,18,19,20 NOX activation is one of the most important factors in the production of ROS (including superoxide radical anion (O2.-) and hydrogen peroxide (H2O2)). Thus, a decrease in ACE2 bioavailability following SARS-CoV-2 connection allows Ang II to be accessible to interact with AT1R, which regulates to trigger NADPH oxidase, oxidative stress, and inflammatory responses14, which eventually leads to aggravate COVID-19.14 Other pathways have also been associated with ACE2 and oxidative stress in the pathogenesis of COVID-19 and include endothelial cell dysfunction that results in the production of ROS by NAD(P)H oxidase, which decreases the bioavailability of nitric oxide, and ultimately leads to redox imbalance, inflammation, vasoconstriction, and endothelial dysfunction. Accumulating this evidence has shown that when ACE2 function is impaired due to SARS-CoV-2 binding, the classic Renin-Angiotensin–Aldosterone System (RAAS), particularly the ACE2–Ang-(1-7) axis, causes a potent pro-oxidant system in vessels.10,17,20,21,22,23
On top of that the pathways mentioned, the virus can also play a role in the release of iron from red blood cells into the bloodstream, which in turn can trigger Fenton and Haber–Weiss reactions. In this mechanism, SARS-CoV-2 attacks hemoglobin, and releases Fe (III) ions from red blood cells, which ultimately increases ferritin levels.10 Iron dysmetabolism and hemoglobin disorders, caused by COVID-19, can eventually cause clinical symptoms such as mitochondrial and related protein damage, lipid peroxidation, Ferroptosis, and oxidative stress.23,24,25,26
According to a study that Wenzhong and Hualan27 conducted, COVID-19 can use its E protein to initiate a viral infection by binding to iron and haem, which results in attack haemoglobin and phagocytes. While E protein binds haem, produces free radicals such as superoxide anions, hydrogen peroxide, and hydroxyl radicals, leads to an increase in the amount of free radicals, and attacks different cells, especially the immune system cells, which eventually causes damage to the immune system.27
ROMO1 AND OXIDATIVE STRESS
One of the most critical proteins in the production of ROS is ROMO1. Structurally, this protein is associated with some critical proteins in the mitochondrial inner membrane,6 and has two membrane domains (TMDs). One of them consists of an alpha helix, and the other can be connected to the alpha helix by a base loop. Furthermore, TMD2 has some polar amino acids, for instance, K58, T59, Q62, S63, T66, and T69.6
Accumulated evidence has shown that ROMO1 is an ROS-producting protein in various cancer cells.28 It has also been implicated in the invasion and proliferation of neoplastic cells. In the same way, ROMO1-induced ROS can lead to a growth, proliferation, and metastasis of cancer cells through various signaling pathways.29 As a result, ROMO1-induced ROS triggers cell proliferation by various factors such as the Extracellular-signal-Regulated Kinase (ERK) pathway, Transforming Growth Factor-β (TGF-β) and their agents, which can include Smad 2/3 protein, Extra Cellular Matrix (ECM) and Epithelial-Mesenchymal Transporters (EMT). For this reason, ROMO1 may affect different signaling pathways in the cell.29,30
As previous mentioned, ROMO1 can affect other pathways, like NF-κB. Overexpression of ROMO1 can launch ROS production by activating NF-κB signaling pathway and degrading and controlling the κB kinase inhibitor, which eventually leads to metastasis, proliferation, and invasion.29,30 According to previous studies, the EMT signaling pathway leads to metastasis, invasion, and proliferation by impairing cell-cell interaction and loss of cell adhesion to the other factors. Thus, ROMO1 affects the growth of cancer cells by activating NF-κB-driven EMT factors.29 Besides, ROMO, by activating NF-κB pathway, can trigger NLRP3, Pro-IL1β, and inflammasome complex, which will ultimately increase oxidative stress, cytokine storm, and inflammation (Fig. 1).28
FIG. 1. This figure shows that COVID-19 can initiate oxidative stress by affecting ROMO1 as well as other factors such as NF-κB, TNF-α and NADPH oxidase, and eventually result in tissue damage and lung dysfunction.
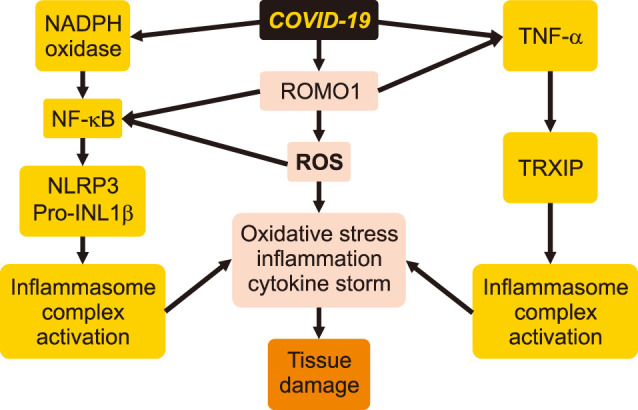
One of the most important factors in inflammation is Tumor Necrosis Factor-alpha (TNF-α).6,31 TNF-α has two critical pathways. One of these signaling pathways is inflammation that is called the complex 1 route, which stimulates Mitogen-Activated Protein Kinase (MAPK or MAP kinase) and NF-κB. Another route leads to apoptosis by launching of Complex 2, which includes the Cascade ROS route and mitochondrial function as the downstream mediators.6
Another point worth noting is that ROMO1 is involved in various cellular routes, especially TNF-α and NF-κB pathways.6,31 At the same time, when ROMO1 activity increases, these factors can trigger some pathways that are related to inflammation and oxidative stress in the cell.31 Increased oxidative stress and inflammation in the cells and mitochondria, in addition to mutations in the genomes, can lead to cell and tissue damage.7,32
COVID-19 AND ROMO1
There strong evidence that ROMO1 has been identified in different diseases, particularly lung diseases, stomach cancer, bladder cancer, diabetes, and some infertility problems.6,7 In 2020, Amini et al.7 conducted a study on ROMO1 and OMA1, and found that overexpression of ROMO1 in gastric cancer tissue promotes oxidative stress in patients with gastric cancer, which is an critical factor in aggravating and even the onset of this deadly cancer. At the same time, in 2020, Ghasemi et al.33 conducted a study on the mitochondrial protein and observed that overexpression of ROMO1 in bladder cancer tissue and also increased ROMO1 in the serum of people with bladder cancer may promote some parameters of oxidative stress in these patients.
Another point worth noting is that ROMO1 and its association with oxidative stress can affect various organs, particularly the lungs, and it has been observed that ROMO1 might cause some diseases related to this organ, namely lung cancer and some other respiratory diseases.6,33 In 2017, Lee et al.34 did a study on Lung Cancer-Related Malignant Effusion (LCRME), and observed that ROMO1 in the fluid isolated from the lungs is increased in the malignant state compared with the benign state, then, they introduced ROMO1 as a marker for lung cancer-related malignant effusion. Similarly, in 2020, Kong et al.35 carried out research on poor distant metastasis-free survival in patients with Non-Small Cell Lung Cancer and observed overexpression of ROMO1 in this type of lung disorder. In the same way, in 2018, Ye et al.36 conducted a study on people with Obstructive Sleep Apnea Syndrome (OSAS) and found that an increase of ROMO1 in their serum, compared to normal people, leads to an increase in oxidative stress and severity of the disease. Likewise, in 2019, Ye et al.37 conducted research on people with Chronic Obstructive Pulmonary Disease (COPD), and according to their results, they showed that overexpression of ROMO1 might increase inflammation and oxidative stress, which can ultimately affect lung function.
Most studies that have been done on ROMO1 are about non-viral diseases (cancer, diabetes…), and it is often said that its dysfunction will cause an increase and overproduction of ROS, which leads to damage different cells, tissues and organs, especially the immune system and finally aggravate or intitiate these diseases.6,7,33 In addition to non-viral diseases, this protein has also been studied in Human Immunodeficiency Virus (HIV).38 In 2021, Merlini et al.38 evaluated ROMO1 in the serum of patients with HIV and found that this protein has significantly increased and they introduced ROMO1 as a factor which increases the amount of oxidative stress in this viral disease.
According to these studies, ROMO1 dysfunction can be the cause of increased oxidative stress in various cells and tissues, especially the lungs that might ultimately promote oxidative stress which impairs lung function.6 Another factor to consider is the pathogenesis of COVID-19 in different cells, especially in lung cells.5 The association of COVID-19 and oxidative stress might have a direct or indirect relationship with this mitochondrial protein in the pathogenesis of COVID-19. As mentioned above, The TNF-α and NF-κB pathways increase oxidative stress and ROS within the lung cells, which are closely related to ROMO1 protein.5,6 To put it simply, overexpression and dysfunction of ROMO1 might launch these pathways, which ultimately promotes oxidative stress in the lung cells.
To sum up, there is the hypothesis that COVID-19 might have a direct or indirect association with this important mitochondrial protein through related molecules, which promote oxidative stress and ROS within the lung cells, and lead eventually to lung dysfunction (Fig. 1).
CONCLUSION
To summarize, TNF-α and NF-κB pathways play an important role in inflammation and oxidative stress, and, are also associated with ROMO1 and COVID-19. Consequently, it is hypothesized that COVID-19 might increase oxidative stress by affecting ROMO1 through activating these pathways. This strong implies the role of ROMO1 in the pathogenesis of COVID-19 and may help pave the way to the development of strategies for effective potential therapeutics.
Footnotes
CONFLICT OF INTEREST STATEMENT: None declared.
References
- 1.CDC COVID-19 Response Team. Severe outcomes among patients with coronavirus disease 2019 (COVID-19) - United States, February 12-March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:343–346. doi: 10.15585/mmwr.mm6912e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khamis F, Al Rashidi B, Al-Zakwani I, Al Wahaibi AH, Al Awaidy ST. Epidemiology of COVID-19 infection in Oman: analysis of the first 1304 cases. Oman Med J. 2020;35:e145. doi: 10.5001/omj.2020.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lippi G, Sanchis-Gomar F, Henry BM. Coronavirus disease 2019 (COVID-19): the portrait of a perfect storm. Ann Transl Med. 2020;8:497. doi: 10.21037/atm.2020.03.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jernigan DB CDC COVID-19 Response Team. Update: public health response to the coronavirus disease 2019 outbreak - United States, February 24, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:216–219. doi: 10.15585/mmwr.mm6908e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beltrán-García J, Osca-Verdegal R, Pallardó FV, Ferreres J, Rodríguez M, Mulet S, et al. Oxidative stress and inflammation in COVID-19-associated sepsis: the potential role of anti-oxidant therapy in avoiding disease progression. Antioxidants (Basel) 2020;9:936. doi: 10.3390/antiox9100936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Amini MA, Talebi SS, Karimi J. Reactive oxygen species modulator 1 (ROMO1), a new potential target for cancer diagnosis and treatment. Chonnam Med J. 2019;55:136–143. doi: 10.4068/cmj.2019.55.3.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Amini MA, Karimi J, Khodadadi I, Tavilani H, Talebi SS, Afshar B. Overexpression of ROMO1 and OMA1 are potentially biomarkers and predict unfavorable prognosis in gastric cancer. J Gastrointest Cancer. 2020;51:939–946. doi: 10.1007/s12029-019-00330-w. [DOI] [PubMed] [Google Scholar]
- 8.Lee S, Park YH, Chung JS, Yoo YD. Romo1 and the NF-κB pathway are involved in oxidative stress-induced tumor cell invasion. Int J Oncol. 2015;46:2021–2028. doi: 10.3892/ijo.2015.2889. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization. Coronavirus disease (COVID-19): situation report, 162. Geneva: World Health Organization; 2020. [Google Scholar]
- 10.Wu H, Wang Y, Zhang Y, Xu F, Chen J, Duan L, et al. Breaking the vicious loop between inflammation, oxidative stress and coagulation, a novel anti-thrombus insight of nattokinase by inhibiting LPS-induced inflammation and oxidative stress. Redox Biol. 2020;32:101500. doi: 10.1016/j.redox.2020.101500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Delgado-Roche L, Mesta F. Oxidative stress as key player in severe acute respiratory syndrome coronavirus (SARS-CoV) infection. Arch Med Res. 2020;51:384–387. doi: 10.1016/j.arcmed.2020.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cecchini R, Cecchini AL. SARS-CoV-2 infection pathogenesis is related to oxidative stress as a response to aggression. Med Hypotheses. 2020;143:110102. doi: 10.1016/j.mehy.2020.110102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Islam MMT, Shekhar HU. In: Free Radicals in Human Health and Disease. Rani V, Yadav U, editors. New Delhi: Springer; 2015. Impact of oxidative stress on human health; pp. 59–73. [Google Scholar]
- 14.Anand SP, Chen Y, Prévost J, Gasser R, Beaudoin-Bussières G, Abrams CF, et al. Interaction of human ACE2 to membrane-bound SARS-CoV-1 and SARS-CoV-2 S glycoproteins. Viruses. 2020;12:1104. doi: 10.3390/v12101104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Diep PT. Is there an underlying link between COVID-19, ACE2, oxytocin and vitamin D? Med Hypotheses. 2021;146:110360. doi: 10.1016/j.mehy.2020.110360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gan R, Rosoman NP, Henshaw DJE, Noble EP, Georgius P, Sommerfeld N. COVID-19 as a viral functional ACE2 deficiency disorder with ACE2 related multi-organ disease. Med Hypotheses. 2020;144:110024. doi: 10.1016/j.mehy.2020.110024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sawalha AH, Zhao M, Coit P, Lu Q. Epigenetic dysregulation of ACE2 and interferon-regulated genes might suggest increased COVID-19 susceptibility and severity in lupus patients. Clin Immunol. 2020;215:108410. doi: 10.1016/j.clim.2020.108410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dikalov SI, Nazarewicz RR. Angiotensin II-induced production of mitochondrial reactive oxygen species: potential mechanisms and relevance for cardiovascular disease. Antioxid Redox Signal. 2013;19:1085–1094. doi: 10.1089/ars.2012.4604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wei Y, Sowers JR, Clark SE, Li W, Ferrario CM, Stump CS. Angiotensin II-induced skeletal muscle insulin resistance mediated by NF-kappaB activation via NADPH oxidase. Am J Physiol Endocrinol Metab. 2008;294:E345–E351. doi: 10.1152/ajpendo.00456.2007. [DOI] [PubMed] [Google Scholar]
- 20.Oudit GY, Kassiri Z, Patel MP, Chappell M, Butany J, Backx PH, et al. Angiotensin II-mediated oxidative stress and inflammation mediate the age-dependent cardiomyopathy in ACE2 null mice. Cardiovasc Res. 2007;75:29–39. doi: 10.1016/j.cardiores.2007.04.007. [DOI] [PubMed] [Google Scholar]
- 21.Violi F, Oliva A, Cangemi R, Ceccarelli G, Pignatelli P, Carnevale R, et al. Nox2 activation in Covid-19. Redox Biol. 2020;36:101655. doi: 10.1016/j.redox.2020.101655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Libby P, Lüscher T. COVID-19 is, in the end, an endothelial disease. Eur Heart J. 2020;41:3038–3044. doi: 10.1093/eurheartj/ehaa623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rabelo LA, Alenina N, Bader M. ACE2-angiotensin-(1-7)-Mas axis and oxidative stress in cardiovascular disease. Hypertens Res. 2011;34:154–160. doi: 10.1038/hr.2010.235. [DOI] [PubMed] [Google Scholar]
- 24.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. Erratum in: Lancet 2020;395:1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cavezzi A, Troiani E, Corrao S. COVID-19: hemoglobin, iron, and hypoxia beyond inflammation. A narrative review. Clin Pract. 2020;10:1271. doi: 10.4081/cp.2020.1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Merad M, Martin JC. Pathological inflammation in patients with COVID-19: a key role for monocytes and macrophages. Nat Rev Immunol. 2020;20:355–362. doi: 10.1038/s41577-020-0331-4. Erratum in: Nat Rev Immunol 2020;20:448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wenzhong L, Hualan L. COVID-19: captures iron and generates reactive oxygen species to damage the human immune system. Autoimmunity. 2021;54:213–224. doi: 10.1080/08916934.2021.1913581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim IG, Kim SY, Kim HA, Kim JY, Lee JH, Choi SI, et al. Disturbance of DKK1 level is partly involved in survival of lung cancer cells via regulation of ROMO1 and γ-radiation sensitivity. Biochem Biophys Res Commun. 2014;443:49–55. doi: 10.1016/j.bbrc.2013.11.038. [DOI] [PubMed] [Google Scholar]
- 29.Shyamsunder P, Verma RS, Lyakhovich A. ROMO1 regulates RedOx states and serves as an inducer of NF-κB-driven EMT factors in Fanconi anemia. Cancer Lett. 2015;361:33–38. doi: 10.1016/j.canlet.2015.02.020. [DOI] [PubMed] [Google Scholar]
- 30.Lee SB, Kim JJ, Chung JS, Lee MS, Lee KH, Kim BS, et al. Romo1 is a negative-feedback regulator of Myc. J Cell Sci. 2011;124(Pt 11):1911–1924. doi: 10.1242/jcs.079996. Erratum in: J Cell Sci 2011;124(Pt 11):1911. [DOI] [PubMed] [Google Scholar]
- 31.Kim JJ, Lee SB, Park JK, Yoo YD. TNF-alpha-induced ROS production triggering apoptosis is directly linked to Romo1 and Bcl-X(L) Cell Death Differ. 2010;17:1420–1434. doi: 10.1038/cdd.2010.19. [DOI] [PubMed] [Google Scholar]
- 32.Norton M, Ng AC, Baird S, Dumoulin A, Shutt T, Mah N, et al. ROMO1 is an essential redox-dependent regulator of mitochondrial dynamics. Sci Signal. 2014;7:ra10. doi: 10.1126/scisignal.2004374. [DOI] [PubMed] [Google Scholar]
- 33.Ghasemi H, Amini MA, Pegah A, Azizi E, Tayebinia H, Khanverdilou S, et al. Overexpression of reactive oxygen species modulator 1 is associated with advanced grades of bladder cancer. Mol Biol Rep. 2020;47:6497–6505. doi: 10.1007/s11033-020-05702-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee SH, Park MJ, Choi SI, Lee EJ, Lee SY, In KH. Reactive oxygen species modulator 1 (Romo1) as a novel diagnostic marker for lung cancer-related malignant effusion. Medicine (Baltimore) 2017;96:e5975. doi: 10.1097/MD.0000000000005975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kong M, Sung JY, Lee SH. Reactive oxygen species modulator 1 is associated with poor survival in patients with non-small cell lung cancer after stereotactic fractionated radiosurgery: a retrospective pilot study. Onco Targets Ther. 2020;13:8173–8180. doi: 10.2147/OTT.S266344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ye L, Qian Y, Li Q, Fang S, Yang Z, Tan Y, et al. Serum Romo1 is significantly associated with disease severity in patients with obstructive sleep apnea syndrome. Sleep Breath. 2018;22:743–748. doi: 10.1007/s11325-017-1606-2. [DOI] [PubMed] [Google Scholar]
- 37.Ye L, Mao S, Fang S, Zhang J, Tan Y, Gu W. Increased serum Romo1 was correlated with lung function, inflammation, and oxidative stress in chronic obstructive pulmonary disease. Inflammation. 2019;42:1555–1560. doi: 10.1007/s10753-019-01017-x. [DOI] [PubMed] [Google Scholar]
- 38.Merlini E, Tincati C, Sacchi V, Augello M, Bono V, Cannizzo ES, et al. Predictors of low ovarian reserve in cART-treated women living with HIV. Medicine (Baltimore) 2021;100:e27157. doi: 10.1097/MD.0000000000027157. [DOI] [PMC free article] [PubMed] [Google Scholar]


