Abstract
COVID-19 vaccine hesitancy will likely increase in the unvaccinated general population because of several vaccine safety issues that arose during priority vaccination. To investigate the potential rate of COVID-19 vaccine hesitancy in the unvaccinated population and evaluate factors that affect the attitude towards vaccine acceptance, a cross-sectional survey was performed. A telephone survey was conducted in 1,357 people older than 18 years; 99 were excluded from the analysis because they had already been vaccinated (n=58) or hesitated (n=41) after an official call. The COVID-19 vaccine hesitancy rate was 21.9% and was highest among those aged under 30 years (33.4%) and lowest among those aged 65 years and over (8.7%). Age, occupation, and perceived confidence in vaccine safety and efficacy were associated with vaccine hesitancy. These findings suggest that public health authorities should strengthen the spread of correct information, especially in the younger population, to increase vaccination rates.
Keywords: COVID-19, Vaccine Hesitancy, Vaccination
INTRODUCTION
The public health crisis caused by the COVID-19 pandemic continues worldwide since the first COVID-19 cases were reported in Wuhan, China, in December 2019. As of the third week of December 2021, more than 273 million COVID-19 cases have been confirmed, and approximately 5.8 million COVID-19-related deaths have been reported worldwide.1 In Korea, more than 550,000 COVID-19 cases and 4,600 deaths from COVID-19 have occurred.2 To end this crisis, increasing the level of herd immunity via vaccination seems to be the most obvious “game changer” because there are few magic bullets in COVID-19 treatment.3 In December 2020, the United States Food and Drug Administration (FDA) first approved the COVID-19 vaccines and the mass vaccination program against COVID-19 started in Europe, United states, and Israel in early December 2020.4 As growing concerns about vaccine safety and adverse effects of COVID-19 vaccine sufaced, vaccine hesitancy has become an important issue in addressing the pandemic. However, although the occurrence of serious COVID-19 vaccine adverse effects varies by vaccine brands, ages, and vaccination numbers, these effects are generally evaluated as very rare.5
The first COVID-19 vaccinations in Korea were given on February 26, 2021. Vaccination of the first priority groups, including high-risk health care workers and older adults in overcrowded settings, and the second priority groups, including those aged over 65 years, health care workers, and individuals in various shelters, were initiated first. Since the first COVID-19 vaccination in Korea, more than forty million two dose vaccinations have been administered, and more than ten million people have completed booster vaccination, as of the third week of December 2021. Furthermore, vaccination of children between the ages of 12 and 17 has just begun. However, there are still more than 10 million unvaccinated peoples in all ages, and the vaccination rate of those over 80 years of age, the age group with the worst clinical prognosis, does not exceed 90% yet.2 Vaccination of the general population was scheduled for the second half of 2021.
The SAGE Working Group on Vaccine Hesitancy defined vaccine hesitancy as delayed acceptance, reluctance, or refusal of vaccination despite the availability of vaccination services.6 Before the COVID-19 pandemic began, the World Health Organization (WHO) identified vaccine hesitancy as one of the 10 current global public health threats in 2019. Even medical personnel have been known to exhibit vaccine hesitancy or skepticism. In an Israeli survey, the future COVID-19 vaccine acceptance rate was 78% in doctors and only 61% in nurses, compared with 75% in the general population.7
Therefore, it is important to establish tailored strategies to increase the potential acceptance rate of COVID-19 vaccination and decrease vaccine hesitancy. So, a cross-sectional survey for unvaccinated people to evaluate the current vaccine hesitancy status and identify the factors associated with vaccine hesitancy was conducted in Korea.
MATERIALS AND METHODS
A cross-sectional telephone survey was performed in March 2021 to estimate the intention to receive the COVID-19 vaccine in the future and to evaluate the factors associated with vaccine compliance among unvaccinated individuals who were not eligible for vaccination at the time of the investigation. To achieve the representative sample of general population, study subjects were selected from a pool of interviewees from a public polling institution to be included evenly by sex, age, and residence area. All study subjects gave their phone number and consent to participate in the telephone survey. Of the 1,357 people surveyed over the age of 18 years living in Metropolitan Gwangju, 99 were excluded from the analysis because they had already been vaccinated (n=58) or had shown hesitancy (n=41) after an official vaccination call. The analysis included 1,258 unvaccinated individuals who have not yet received an official call. IRB approval of this study was obtained (IRB no. CNUHH-2021-070). Ideal study sample size under condition of population size (1.5 million), 95% confidence interval, and margin of error (3%) is 1,067 individuals. Demographic data, such as sex, age, occupation, and region, was self-reported. All participants were asked whether they intend to undergo future COVID-19 vaccination. The answer choices were “Yes, as soon as the vaccine is available”, “Yes, if it is the vaccine I prefer”, “Yes, but only after learning more”, “No, I probably won’t receive the vaccine”, “No, I absolutely won’t receive the vaccine”, and “I have not decided yet”. These answers were categorized into three categories: “Yes”, the participants who will receive the vaccine as soon as possible, or as long as it is their preferred vaccine, or after learning more; “Wait”, the participants who have not yet decided; and “No”, the participants who have no intention of receiving the COVID-19 vaccine. Vaccine acceptance was defined as the category “Yes”, while vaccine hesitancy was defined as the categories “Wait” or “No”, according to the SAGE Working Group on Vaccine Hesitancy.6 Those who had no intention of getting vaccinated were asked “What are the reasons that you will not or are hesitant to receive the vaccine?”, and the seven possible answers were “Distrust efficacy and safety”, “No transparency of the information disclosed by the government”, “Don’t expect to be infected if I am not vaccinated”, “Anxiety over reported vaccine side effects”, “Poor health”, “History of adverse reactions to vaccines”, and “Other reasons”. Awareness of information about the vaccination plan, satisfaction with vaccination preparedness, confidence in vaccine safety and efficacy, and fairness regarding vaccine availability were assessed on a 10-point scale. They were also asked about their preference of COVID-19 vaccine manufacturer. Multivariate logistic regression was used to identify factors associated with COVID-19 vaccine hesitancy among the unvaccinated population. All analyses were conducted in R (v3.6.3), and statistical significance was based on a p-value of 0.05.
RESULTS
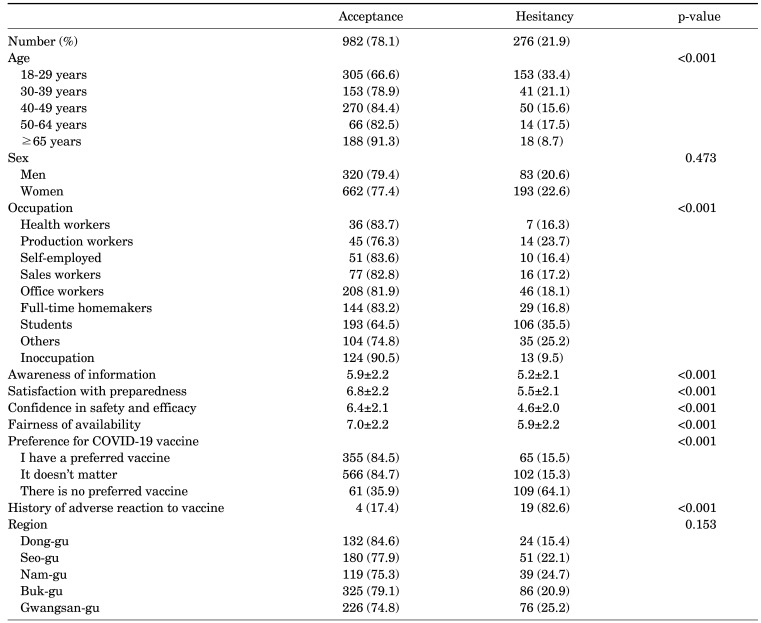
Table 1 shows the proportion intending to undergo COVID-19 vaccinated according to demographic factors. The vaccine hesitancy rate was 21.9% (‘Wait’ 13.8%, ‘No’ 8.1%) and vaccine acceptance rate was 78.1% (“Yes, as soon as the vaccine is available” 40.8%, “Yes, but only after learning more” 31.6%, “Yes, if it is the vaccine I prefer” 5.6%). There was no difference according to sex (men 20.6%, women 22.6%). The vaccine hesitancy rate was highest in individuals under 30 years of age (33.4%) and lowest in those 65 years or older (8.7%). Regarding occupation, health care workers had the highest acceptance rate (83.7%), and university students had the highest COVID-19 vaccine hesitancy rate (35.5%). The greater the awareness of vaccine information, satisfaction with vaccine preparedness, confidence in vaccine safety and efficacy, and fairness of vaccine availability, the lower the vaccine hesitancy rate (Table 1).
TABLE 1. Acceptance and hesitancy rates of COVID-19 vaccine by the demographic factors and subjective assessment for vaccine policy.
Values are number of individuals (percentage) or mean±standard deviation, as appropriately.
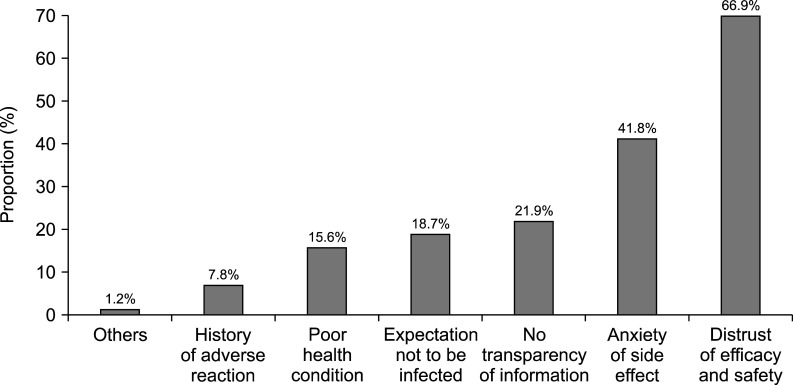
The most common reason for vaccine hesitancy was distrust of the efficacy and safety of the vaccine (66.9%), followed by anxiety caused by reported vaccine side effects (41.8%), belief that they will not be infected (18.7%), poor health (15.6%), adverse reaction after recent influenza vaccination (5.8%), and history of anaphylaxis (2.0%) (Fig. 1).
FIG. 1. Reasons for being unsure of taking COVID-19 vaccines.
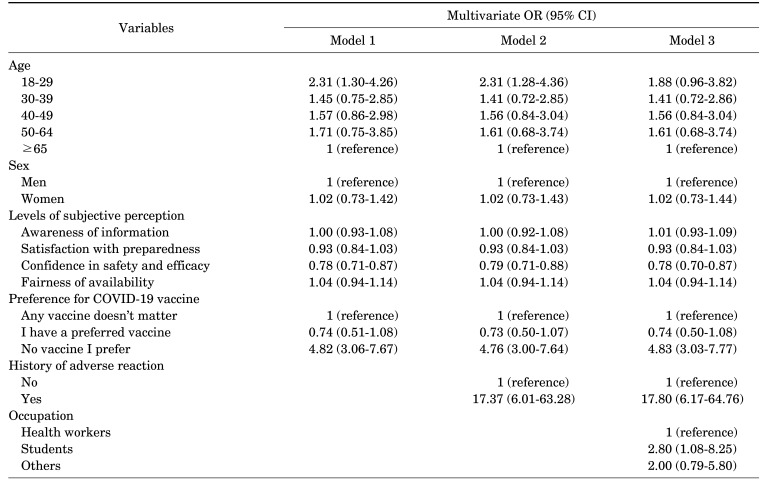
In the multivariate model, compared with subjects aged 65 years or over, the odds ratios (ORs) of vaccine hesitancy in those aged 18-29, 30-39, 40-49, and 50-65 years were 1.91 (95% confidence interval [CI] 0.82-4.81), 1.57 (95% CI 0.67-3.95), 1.60 (95% CI 0.69-4.00), and 1.83 (95% CI 0.67-5.14), respectively. Students had the highest risk of hesitancy (OR 2.53, 95% CI 1.07-6.77) compared with health care workers. Except for students, there was no occupation that showed a significant difference in the risk of hesitancy compared to health-care workers. When occupations were grouped into “others”, no difference was found. The individuals with confidence in the efficacy and safety of COVID-19 vaccine had lower risk of vaccine hesitancy as compared to individuals without confidence (OR 0.69, 95% CI 0.63-0.77). Vaccine preference and history of adverse reaction were also associated with the tendency of vaccine hesitancy. Compared to individuals who responded as no brand preference, individuals who didn’t prefer any vaccine showed higher vaccine hesitancy (OR 4.83, 95% CI 3.03-7.77). The OR (95% CI) of individuals with history of adverse reaction was 17.80 (6.17-64.76). No significant association was observed between vaccine hesitancy and sex, awareness, satisfaction, fairness, or residence area (Table 2).
TABLE 2. Factors associated with the risk of COVID-19 vaccine hesitancy among the unvaccinated population.
OR: odds’ ratio, CI: confidence interval.
DISCUSSION
Although the acceptance rate of the COVID-19 vaccine (78.1%) in this study was similar to that of previous reports,7,8 only 40.8% of unvaccinated individuals reported a definite intention for future COVID-19 vaccination. Similar to previous studies, a noticeable difference in COVID-19 vaccine acceptance was observed between the youngest and oldest populations.9 The difference in the vaccine acceptance rate according to age may be due to differences in disease severity or infectivity. The higher acceptance rate among the oldest may have resulted from their relatively serious concerns about COVID-19 infection. Note that the hesitancy rate was not lower in health care workers than in other occupational groups, except university students. Confidence in vaccine safety and efficacy was inversely associated with vaccine hesitancy. These findings are consistent with studies conducted in other countries.10 The perceived safety and efficacy of the vaccine have been the most common determinants of vaccine acceptance since the pre-COVID-19 era.11,12 During the COVID-19 pandemic, several publications have shown that the strongest predictors of COVID-19 vaccination intention are the safety of the potential vaccine13 and benefits versus risks.14 Preference for a particular vaccine manufacturer is a unique issue of the COVID-19 pandemic that has not been carefully considered with other diseases, such as influenza. In this study, only 33.4% of the participants responded that they did not have a vaccine preference, while 5.6% responded that they would be vaccinated only if given their preferred vaccine. Preference for a particular manufacturer may lead to skepticism regarding non-preferred COVID-19 vaccines and to a decrease in vaccination rates. In this study, the factor that had the biggest effect on vaccine hesitancy was the history of vaccine adverse reaction. Among the individuals having adverse reaction histories, the perceived benefits and actually expected benefits compared to the harm will be lower while the perceived and actual risk will be higher.
As a limitation of this study, since the investigation was conducted in the early stages of the national vaccination response for COVID-19, it may be different from the current ongoing situation, which is progressing up to the third vaccination schedule. Nevertheless, it provides information on the status of vaccination hesitancy and related factors at the early stage of vaccination launching as a response strategy against a pandemic.
In conclusion, to achieve a greater COVID-19 vaccine acceptance, public authorities should enhance perceptions of the efficacy and safety of vaccines and urgently address the hesitancy of the younger population. A successful COVID-19 vaccination program to decrease vaccine hesitancy should include the spread of clear, timely messages advocating the safety and efficacy of available COVID-19 vaccines.
ACKNOWLEDGEMENTS
This study was financially supported by the Gwangju Institute for Public Health and Equity and Gwangju Centers for Infectious Diseases Control and Prevention.
Footnotes
CONFLICT OF INTEREST STATEMENT: None declared.
References
- 1.European Centre for Disease Prevention and Control (ECDC) COVID-19 situation update worldwide, as of week 52 2021 [Internet] Solna: ECDC; 2021. [cited 2021 Dec 17]. Available from: https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases . [Google Scholar]
- 2.Central Disaster Management Headquarters. Coronavirus (COVID-19), Republic of Korea [Internet] Sejong: Ministry of Health and Welfare; 2021. [cited 2021 Dec 17]. Available from: http://ncov.mohw.go.kr/en/ [Google Scholar]
- 3.Kouznetsov VV. COVID-19 treatment: much research and testing, but far, few magic bullets against SARS-CoV-2 coronavirus. Eur J Med Chem. 2020;203:112647. doi: 10.1016/j.ejmech.2020.112647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hasan T, Beardsley J, Marais BJ, Nguyen TA, Fox GJ. The implementation of mass-vaccination against SARS-CoV-2: a systematic review of existing strategies and guidelines. Vaccines (Basel) 2021;9:326. doi: 10.3390/vaccines9040326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beatty AL, Peyser ND, Butcher XE, Cocohoba JM, Lin F, Olgin JE, et al. Analysis of COVID-19 vaccine type and adverse effects following vaccination. JAMA Netw Open. 2021;4:e2140364. doi: 10.1001/jamanetworkopen.2021.40364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.MacDonald NE SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33:4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 7.Dror AA, Eisenbach N, Taiber S, Morozov NG, Mizrachi M, Zigron A, et al. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35:775–779. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sallam M. COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines (Basel) 2021;9:160. doi: 10.3390/vaccines9020160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Coustasse A, Kimble C, Maxik K. COVID-19 and vaccine hesitancy: a challenge the United States must overcome. J Ambul Care Manage. 2021;44:71–75. doi: 10.1097/JAC.0000000000000360. [DOI] [PubMed] [Google Scholar]
- 10.Soares P, Rocha JV, Moniz M, Gama A, Laires PA, Pedro AR, et al. Factors associated with COVID-19 vaccine hesitancy. Vaccines (Basel) 2021;9:300. doi: 10.3390/vaccines9030300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Larson HJ, de Figueiredo A, Xiahong Z, Schulz WS, Verger P, Johnston IG, et al. The state of vaccine confidence 2016: global insights through a 67-country survey. EBioMedicine. 2016;12:295–301. doi: 10.1016/j.ebiom.2016.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Karafillakis E, Larson HJ ADVANCE consortium. The benefit of the doubt or doubts over benefits? A systematic literature review of perceived risks of vaccines in European populations. Vaccine. 2017;35:4840–4850. doi: 10.1016/j.vaccine.2017.07.061. [DOI] [PubMed] [Google Scholar]
- 13.Karlsson LC, Soveri A, Lewandowsky S, Karlsson L, Karlsson H, Nolvi S, et al. Fearing the disease or the vaccine: the case of COVID-19. Pers Individ Dif. 2021;172:110590. doi: 10.1016/j.paid.2020.110590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pogue K, Jensen JL, Stancil CK, Ferguson DG, Hughes SJ, Mello EJ, et al. Influences on attitudes regarding potential COVID-19 vaccination in the United States. Vaccines (Basel) 2020;8:582. doi: 10.3390/vaccines8040582. [DOI] [PMC free article] [PubMed] [Google Scholar]