Abstract
Coronavirus disease 2019 has created and amplified racial health disparities. This has been particularly noticeable in populations with asthma. There is no one simple reason for this occurrence, but rather a complex interaction of biological, structural, and socioeconomic factors. This article will highlight reasons why the coronavirus disease 2019 pandemic has been particularly impactful among minority populations throughout the world and will also offer potential solutions to help overcome health disparities.
Key words: COVID-19, Health disparities, Race, Minority populations, Asthma, Social determinants of health
Abbreviations used: COVID-19, coronavirus disease 2019
INFORMATION FOR CATEGORY 1 CME CREDIT.
Credit can now be obtained, free for a limited time, by reading the review articles in this issue. Please note the following instructions.
Method of Physician Participation in Learning Process: The core material for these activities can be read in this issue of the Journal or online at the JACI: In Practice Web site: www.jaci-inpractice.org/. The accompanying tests may only be submitted online at www.jaci-inpractice.org/. Fax or other copies will not be accepted.
Date of Original Release: April 1, 2022. Credit may be obtained for these courses until March 31, 2023.
Copyright Statement: Copyright © 2022-2024. All rights reserved.
Overall Purpose/Goal: To provide excellent reviews on key aspects of allergic disease to those who research, treat, or manage allergic disease.
Target Audience: Physicians and researchers within the field of allergic disease.
Accreditation/Provider Statements and Credit Designation: The American Academy of Allergy, Asthma & Immunology (AAAAI) is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians. The AAAAI designates this journal-based CME activity for 1.00 AMA PRA Category 1 Credit™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
List of Design Committee Members: Sara J. Willems, PhD, Mariana C. Castells, MD, PhD, and Alan P. Baptist, MD, MPH (authors); David A. Khan, MD (editor)
Learning objectives:
-
1.
To describe racial disparities in the incidence and outcomes of COVID-19.
-
2.
To provide an understanding in the underlying mechanisms explaining these disparities including inequity in health care.
-
3.
To identify how the COVID-19 pandemic worsened health disparities among those with asthma in the United States and how these can be addressed.
Recognition of Commercial Support: This CME has not received external commercial support.
Disclosure of Relevant Financial Relationships with Commercial Interests: All authors and reviewers reported no relevant financial relationships.
Global Coronavirus Disease 2019 Pandemic Disparities
Two sisters lived few miles from each other in a rural area. They were the breadwinners of their families selling produce in the open market. Both were married, in their 50s, and had children. They were Hispanic with low socioeconomic status and had limited access to information, health care, and resources. However, they were in good health: they did not smoke, did not have diabetes or hypertension, although one had mild asthma. They could not stop working during the pandemic, and vaccination for COVID-19 had not started. One sister acquired COVID-19 from one of her adolescent children, a few days before the family was reunited for a birthday party. Masks and social distancing were not enforced. Her symptoms worsened in the next week, with fever, cough, and shortness of breath. Her sister with whom she had close contact during the party started 5 days later with similar symptoms, which also worsened quickly. Access to medical care was difficult, the hospitals were overloaded, and they were treated at home with azithromycin, dexamethasone, inhaled corticosteroids, and bronchodilators. Oxygen became necessary, and the family searched for it. Attempts were made for transport of both sisters to the capital; however, oxygen became unavailable in and outside hospitals. The two sisters died within few days of each other gasping for air, within two weeks of becoming symptomatic. Their deaths had devastating impact in the family, destroying the sources of income and emotional support of the children and the entire family.
At the end of 2019, a novel coronavirus (severe acute respiratory syndrome coronavirus 2) emerged from an animal reservoir in Wuhan, China.1 , 2 In January 2020, the World Health Organization recognized the worldwide infection with the virus as a public health emergency of international concern. In March 2020, it was declared a pandemic for which a global coordinated effort is needed to stop the further spread of the virus.3 Globally, as of December 6, 2021, there have been 265,194,191 confirmed cases of coronavirus disease 2019 (COVID-19), including 5,254,116 deaths.4 Globally, the mortality rate is 57.833 deaths/100K population. However, the global COVID-19 incidence and mortality rates vary temporally (as the epidemic progresses) and spatially (among countries).5 Countries throughout the world have reported very different case-fatality ratios (the number of deaths divided by the number of confirmed cases), ranging from 7.6% in Mexico, 4.1% in Bulgaria, 1.6% in the United States, to 0.2% in Iceland.6 In addition to differences in the number of people tested and the way numbers are reported, the wide range of these figures can be explained by differences in the composition of the population (eg, a higher proportion of elderly), the scope of the measures taken to flatten the curve, and the organization of health care (eg, the organization of primary care, the testing abilities, the availability of medical oxygen, and the country-specific capacity to tackle a large number of patients requiring respiratory assistance and intensive care).5
Also, within countries, the health effects of COVID-19 have been unevenly distributed among and within regions and communities. The most recent findings on ethnic disparities are those of Mude et al,7 who conducted a systematic literature search of studies published between January 1, 2020, and April 15, 2021, reporting on prevalence, hospitalizations, and deaths from COVID-19 by race groups. The meta-analysis on the 72 included studies (with most from the United States) showed that COVID-19 significantly impacted Black people more across all the outcomes measured than White people. The prevalence ratios and hospitalization rates in Black people were 156% and 153% higher than in White people, and deaths in Black people were 105% higher than in White people. Although not as high as Black people, this study showed that Hispanic people also experienced a higher burden of disease than White people (154% higher incidence rates, 78% higher hospitalization rates, and 15% higher deaths).7 These results largely confirm the results of the 2 earlier reviews8 , 9 and 1 meta-analysis.10
Racial and ethnic disparities seem to have been amplified during the pandemic. For example, although more than 600,000 people have died in the United States from COVID-19, the death rate through March of 2021 among Black people was 1.4 times higher than that mong White people.11 In urban areas, the disparities were even more pronounced. In Chicago, Black individuals accounted for nearly 70% of deaths from COVID-19 despite representing only 30% of the population.12 The COVID-19 death rate among Hispanic individuals was significantly higher than that among non-Hispanic individuals in New York (74.3 vs 45.2 per 100,000, respectively).13 Disparities among those younger than 25 years in the United States were especially high during the first months of the pandemic (January-April 2020). Although disparities remained, they decreased the months after, mainly because of a greater increase in mortality in White people.14
Determinants of Health Disparities in Covid-19, with a Focus on Asthma
The identified racial disparities in prevalence, hospitalizations, and mortality ratio from COVID-19 could be attributed to several reasons, including biological, structural, and socioeconomic, and there is growing evidence for the relationship between ethnicity and the already known risk factors for poor clinical outcomes in COVID-19. Although there was initial significant concern that asthma was a significant risk factor for mortality from COVID-19, this generally has not been observed in studies.15 , 16 However, in a study comparing COVID-19 outcomes, the percent of Black patients with asthma who had COVID was significantly higher than the percent of Black patients without asthma who had COVID (35.5% vs 21.4%),17 and Black patients overall were more likely to require hospitalization. In addition, in another study of 1827 patients with asthma, those who required hospitalization were more likely to be Black than those who did not require hospitalization (19.1% vs 15.0%).18
To better understand the possible contributing factors of COVID-19 as an exacerbating factor of asthma health disparities, as well as to quantify the impact of the pandemic on patients with asthma, a survey was conducted among 1171 patients with asthma and 225 physicians from April to May 2020.19 Of the asthma survey respondents, a total of 10% of the subjects were considered minority individuals (Black or Hispanic). The results of the survey helped to delineate the unequal impact of COVID-19 and possible causes.
Table I summarizes how COVID-19 has worsened or magnified existing health inequities. First, racial minority populations experience disproportionately higher rates of underlying health conditions, of which it is known that they are associated with an increased vulnerability to COVID-19.20 For example, Native American populations have disproportionately higher heart disease and diabetes levels, which make them particularly at risk of complications from COVID-19.21 And in the most impoverished neighborhoods, Black people and Hispanic people are at greater risk for respectively hypertension and diabetes compared with White neighbors, resulting in a greater risk of death from a COVID-19 infection than their White counterparts.22 The reasons for increased comorbidities are complex and include social and structural determinants of health, racism (the belief that personality, behavior, and morals can be traced back to race, and the belief that one race is superior to another), discrimination (acting upon racist thoughts), economic and educational disadvantages, health care access and quality, individual behavior, and biology. Minority patients with asthma are more likely than White individuals to have medical comorbidities, observed in both adult and pediatric populations.23 , 24 These comorbidities include cardiac disease, diabetes, and obesity. The presence of medical comorbidities presented a particular impetus for worsening asthma disparities. Patients with medical comorbidities have worse outcomes on most asthma metrics than those without.25 Medical comorbidities (such as obesity and congestive heart failure) are a major risk factor for morbidity and mortality due to COVID-19.26 The additive effects of medical comorbidities during the pandemic amplify health disparities present for individuals with asthma.
Table I.
How COVID-19 has worsened or magnified disparities for underrepresented minority individuals
| General socioeconomic factors |
| Increased multidimensional poverty |
| More likely to become unemployed because of COVID-19 |
| Structural and institutional racism |
| Increased exposure |
| Jobs with higher likelihood for virus exposure (“essential workers”) and less opportunities to work remotely |
| Dependent on public transportation for work, leisure, and health care |
| Crowded clinics |
| More likely to live in communities with a high number of COVID-19 cases |
| More likely to live in enclosed and crowded housing with shared facilities |
| Personal factors |
| Genetic determinants |
| Angiotensin-converting enzyme 2 receptor expression |
| Interferon responses |
| Associated risk factors: diabetes, hypertension, obesity, chronic pulmonary diseases |
| Health care factors |
| More likely to have lost insurance coverage |
| Problems paying for medication and health care |
| Closure of primary care services |
| Language and cultural barriers forcing to use erroneous data sources for information on prevention and mitigation, treatment options, and shared decision making |
| Lower vaccination rates |
| Unavailable health care or barriers in access to health care |
| Increased likelihood for lower quality of care |
Second, the disproportionate impact of COVID-19 on ethnic minority communities might be attributable to higher exposure to the virus, leading to an increased infection rate among these communities.10 , 21 , 22 , 27, 28, 29, 30 Such factors were seen in the survey of patients with asthma as well, where minority individuals with asthma were more likely to have been diagnosed with COVID-19, were more likely to have become unemployed due to COVID-19, were more likely to have difficulties obtaining asthma medications during COVID-19, and were more likely to live in communities with a high number of COVID-19 cases.23 Because sustained close contact with someone who is infected with severe acute respiratory syndrome coronavirus 2 drives most new infections, the virus is much more efficiently spread in enclosed and crowded environments. In addition, individuals from ethnic minority communities are more likely to live in larger household sizes composed of multiple generations.8 Compared with their White counterparts, they are also more likely to experience various deprivations in their daily lives, such as poor health, lack of education, inadequate living standards, disempowerment, poor quality of work, and the threat of violence, among others (“multidimensional poverty”).28 They also more often live in overcrowded households or accommodations with shared facilities or communal areas.10 Ethnic minorities disproportionally make up “essential workers” such as retail grocery workers, public transit employees, health care workers, and custodial staff, are more exposed to the public, and are at a higher risk of getting infected.22 , 29 , 30 As it pertains to employment, social distancing is a privilege that requires the opportunity and digital access to work from home, and this is not distributed equally in society.
Third, one of the most effective tools against serious complications and death from COVID-19 is vaccination, but unfortunately this again is a significant contributor to health disparities because minorities and migrant populations are less likely to be vaccinated. When the mRNA vaccines received emergency approval in the United States, vaccine hesitancy rates were significantly higher among Black and Hispanic individuals as compared with White individuals. For example, a July 2020 survey in Arkansas among 1200 adults found that 50% of Black individuals reported significant vaccine hesitancy, compared with only 18% of White individuals.31 Reasons for vaccine hesitancy include mistrust of the medical establishment developed over centuries through racist exploitation by medical researchers and doctors.32 Minority individuals were underrepresented in the COVID-19 vaccine trials, further contributing to a communal sense that the vaccine was not designed for certain populations. In addition, minority individuals face language and cultural barriers limiting their access to accurate information on prevention and mitigation, compelling them to rely on social media or advice from friends, which may be erroneous.29 , 33
Similar to vaccine hesitancy, minority patients who contract COVID-19 are less likely to accept mAb therapy.34 In that study, patients who did not consent to mAb therapy were significantly more likely to subsequently require hospitalization. In addition, a large study of more than 12,000 patients with COVID-19 found that minority patients were far less likely to receive mAb therapy, though whether this was related to patient hesitancy or lack of access is unclear.35 No current data exist regarding COVID vaccine and/or mAb hesitancy rates among those with asthma, and additional research is needed to determine whether disparities in uptake are present in this population.
Together with the increased exposure, these health care–related variables are found to underlie COVID-19–related disparities even more than susceptibility (ie, comorbid conditions).8
Fourth, health care system characteristics also play a significant role in COVID-19–related disparities. Barriers in health care contribute to higher rates of comorbidities, which increase the risk of getting a COVID-19 infection and higher rates of bad COVID-19 outcomes.7 , 29 Despite ethnic minorities being at increased risk of exposure to the virus, they also experience increased barriers to testing such as the lack of transportation and co-payments. As a result, the only recourse for many ethnic minority patients is to seek testing in an emergency room.36 , 37 Individuals from ethnic minority groups also experience barriers in health care once they become ill with COVID-19. Sometimes health care is even not available. For example, in NYC, the borough of Bronx, with 58% of the population at or below “NYCgov Poverty threshold,” has half the rate of intensive care unit beds per 100,000 population of adults 60 years of age and older, compared with the borough of Manhattan, with 31% of the population at or below the poverty threshold.22 Among patients with asthma, minority individuals are more likely to seek care for an exacerbation at an emergency department rather than at a primary care physician office.38 Not only do racial minority groups have less access to care, but they are also more likely to receive the inappropriate diagnosis, treatment, or referrals compared with White people.20 In Europe, the PRICOV-19 study examines how primary care practices in 37 European countries and Israel organized care during the COVID-19 pandemic. Results show that practices actively reached out to patients. However, this was significantly more the case for patients with chronic conditions such as diabetes, than for socially vulnerable patients such as patients known as at risk for domestic violence or patients with limited social resources.39 Hence, health care services and systems are not always offered on the basis of health care need, which is often highest in materially disadvantaged groups or ethnic minority groups. And together with the increased exposure, these health care–related variables are found to underlie COVID-19–related disparities even more than susceptibility (ie, comorbid conditions).8
The US National Academy of Medicine notes that unconscious bias, stereotyping, and prejudice may play an important role in persisting health care disparities.40 For example, Black people are less likely to be detected with pressure ulcers.20 One of the root causes can be found in the medical training and in medical science: darker skin tones are significantly underrepresented and lighter skin tones overrepresented in dermatologic texts, general medical texts, and scientific literature.41 This example is one example of institutional (or systemic) racism: “the collective failure of an organization to provide an appropriate and professional service to people because of their color, culture or ethnic origin.” It does not necessarily have to be deliberate or overt, but rather manifest itself through unwitting prejudice, ignorance, thoughtlessness, and racist stereotyping.42
Institutional and structural racism are related and interconnected. Institutional racism relates to entities such as education and health care systems, whereas structural racism refers to wider political and social disadvantages within society, such as higher rates of poverty for indigenous people or higher COVID-19 mortality rates among Black people. Multiple examples of institutional and structural racism were identified in the survey of patients with asthma: minority individuals with asthma were more likely to have lost health insurance during COVID-19, to live in urban environments (where, as noted above, hospitals are often under significant financial constraints and are underresourced), to have difficulty affording asthma medications during COVID-19, and were less likely to have a primary care physician. Physicians also noted potential effects of structural racism, as nearly 30% of providers noted they encountered more obstacles when providing asthma care for Black patients than for White patients, and approximately 25% of physicians felt that during COVID-19, it was more challenging to care for Black patients.23 Although not explored in that study, institutional racism and individual physician implicit bias both may contribute to physician responses. For example, difficulties caring for minority patients may be related to factors such as perceived difficulties in affording medications, baseline health status, or attending office visits.
The COVID-19 pandemic crisis is expected to have unintended consequences in the most vulnerable individuals and households, amplifying disparities. For example, pregnant women and children are expected to have increased mortality due to collapsed health facilities, limited critical and intensive care beds, limited resources such as oxygen, and barriers to prenatal care and social services.43 , 44
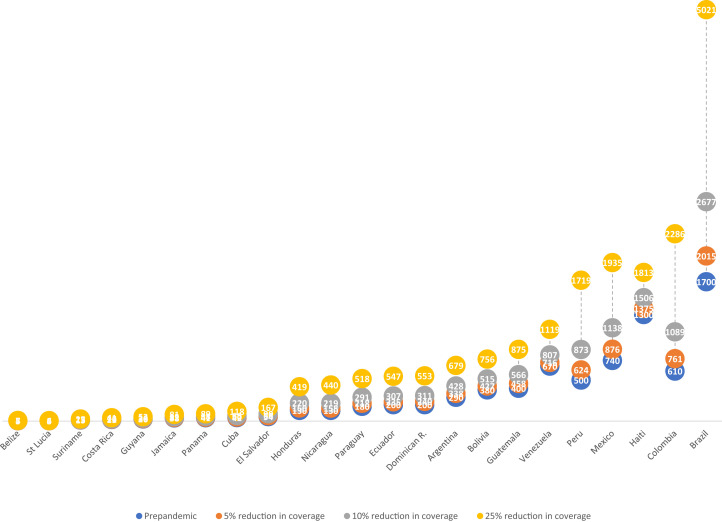
Figure 1 describes the number of excess deaths due to maternal causes due to the effect of the response to the pandemic in selected countries in Latin America and the Caribbean.45
Figure 1.
Estimate of the number of excess deaths due to maternal causes for each range of reduction of coverage (5%, 10%, or 25%) during 1 year due to the effect of the response to the pandemic in selected countries in Latin America and the Caribbean.
Urgent Priorities Oriented Toward Health Equity During and After the Pandemic
Table II gives an overview of the areas that can be identified to start assessing and correcting disparities during and after the pandemic.46, 47
Table II.
Areas to address regarding disparities during and after the pandemic
|
|
|
|
|
|
|
There is also a pressing need to decrease systemic racism throughout the medical establishment. Programs that have shown a positive impact include exposure to counterstereotypical exemplars and implicit bias training.47 Increasing public spending on health and social policies to favor social and economic reactivation and reconstruction would help decrease maternal and infant deaths and reestablish vaccination. Also, building strong primary and community health care is essential. Primary care units deliver the first line of care in communities during the acute phase of a pandemic while maintaining continuity of care for individuals with other diseases. By doing so, primary care also reduces pressure on the entire health system.29 , 48 Stronger involvement of patients in care can contribute to health care systems that address the needs of people whose lives are impacted most.48
Although vaccination is the primary component of the solution for the pandemic, low rates of vaccination and resistance to vaccination are high among underserved populations. In the United States, there has been a recent increase among minority populations regarding COVID-19 vaccination uptake. Some methods that appear to have helped include incentivization of COVID-19 vaccination as well as promotion through community leaders, churches, celebrities, and organizations embedded in the fabric of the underserved populations.
Collecting data on disparities and reporting success and failures of interventions are necessary to understand the true magnitude of the problem. Although we start to understand the impact of the pandemic, there is a need to maintain essential health services for all.
Conclusions
The evidence from the COVID-19 pandemic shows the impact of social determinants on the incidence of cases and on mortality. These inequities must be addressed to improve both overall health outcomes and COVID-19–related outcomes. The factors that predispose to these disparities include ones that are easier to address as well as ones that are achievable but will require significantly more effort. As Mude et al8 conclude, “Governments and policymakers have an opportunity to turn the course of health inequities in minority populations by investing in programs that facilitate equity in disadvantaged communities for improved health outcomes.”8
Footnotes
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest: S. J. Willems and M. C. Castells declare no relevant conflicts of interest and not to have any financial relationships for themselves and their immediate family/significant others. These include consultant arrangements, speakers’ bureau participation, stock or other equity ownership, patent licensing arrangements, and support such as financial or materials grants for research, employment, or expert witness testimony. A. P. Baptist received research funding from AstraZeneca, American Lung Association, and Novartis; acts as an advisor for GlaxoSmithKline, Novartis, and AstraZeneca; and declares not to have any other conflicts of interest or financial relationships for himself and his immediate family/significant others.
References
- 1.Zhou P., Yang X.L., Wang X.G., Hu B., Zhang L., Zhang W., et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization WHO Director-General’s opening remarks at the media briefing on COVID-19-11 March 2020. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 Accessed December 6, 2021.
- 4.World Health Organization WHO Coronavirus (COVID-19) Dashboard. https://covid19.who.int/
- 5.Sorci G., Faivre B., Morand S. Explaining among-country variation in COVID-19 case fatality rate. Sci Rep. 2020;10 doi: 10.1038/s41598-020-75848-2. Article no. 18909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.John Hopkins University & Medicine Corona Virus Resource Center: Mortality analyses. https://coronavirus.jhu.edu/data/mortality Accessed December 6, 2021.
- 7.Mude W., Oguoma V.M., Nyanhanda T., Mwanri L., Njue C. Racial disparities in COVID-19 pandemic cases, hospitalisations, and deaths: a systematic review and meta-analysis. J Glob Health. 2021;11:05015. doi: 10.7189/jogh.11.05015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mackey K., Ayers C.K., Kondo K.K., Saha S., Advani S.M., Young S., et al. Racial and ethnic disparities in COVID-19–related infections, hospitalizations, and deaths. Ann Intern Med. 2021;174:362–373. doi: 10.7326/M20-6306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pan D., Sze S., Minhas J.S., Bangash M.N., Pareek N., Divall P., et al. The impact of ethnicity on clinical outcomes in COVID-19: a systematic review. EClinicalMedicine. 2020;23:100404. doi: 10.1016/j.eclinm.2020.100404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sze S., Pan D., Nevill C.R., Gray L.J., Martin C.A., Nazareth J., et al. Ethnicity and clinical outcomes in COVID-19: a systematic review and meta-analysis. EClinicalMedicine. 2020;29:100630. doi: 10.1016/j.eclinm.2020.100630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.The Covid Tracking Project and Boston University Center for Antiracist Research The COVID Racial Data Tracker. COVID-19 is affecting Black, Indigenous, Latinx, and other people of color the most. https://covidtracking.com/race Accessed July 28, 2021.
- 12.Yancy C.W. COVID-19 and African Americans. JAMA. 1891;2020:323. doi: 10.1001/jama.2020.6548. [DOI] [PubMed] [Google Scholar]
- 13.Kirby T. Evidence mounts on the disproportionate effect of COVID-19 on ethnic minorities. Lancet Respir Med. 2020;8:547–548. doi: 10.1016/S2213-2600(20)30228-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Van Dyke ME, Mendoza MCB, Li W, Parker EM, Belay B, Davis EM, et al. Racial and ethnic disparities in COVID-19 incidence by age, sex, and period among persons aged <25 years—16 U.S. jurisdictions, January 1–December 31, 2020. MMWR Morb Mortal Wkly Rep 2021;70:382–8. [DOI] [PMC free article] [PubMed]
- 15.Lovinsky-Desir S., Deshpande D.R., De A., Murray L., Stingone J.A., Chan A., et al. Asthma among hospitalized patients with COVID-19 and related outcomes. J Allergy Clin Immunol. 2020;146:1027–1034. doi: 10.1016/j.jaci.2020.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lieberman-Cribbin W., Rapp J., Alpert N., Tuminello S., Taioli E. The impact of asthma on mortality in patients with COVID-19. Chest. 2020;158:2290–2291. doi: 10.1016/j.chest.2020.05.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chhiba K.D., Patel G.B., Huyen Vu T.T., Chen M.M., Guo A., Kudlaty E., et al. Prevalence and characterization of asthma in hospitalized and nonhospitalized patients with COVID-19. J Allergy Clin Immunol. 2020;146:307–314. doi: 10.1016/j.jaci.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang L., Foer D., Bates D.W., Boyce J.A., Zhou L. Letter to the editor: risk factors for hospitalization, intensive care, and mortality among patients with asthma and COVID-19. J Allergy Clin Immunol. 2020;146:808–812. doi: 10.1016/j.jaci.2020.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baptist A.P., Lowe D., Sarsour N., Jaffee H., Eftekhari S., Carpenter L.M., et al. Asthma disparities during the COVID-19 pandemic: a survey of patients and physicians. J Allergy Clin Immunol Pract. 2020;8:3371–3377.e1. doi: 10.1016/j.jaip.2020.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Piccardi C., Detollenaere J., Vanden Bussche P., Willems S. Social disparities in patient safety in primary care: a systematic review. Int J Equity Health. 2018;17:114. doi: 10.1186/s12939-018-0828-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dorn A., van Cooney R.E., Sabin M.L. COVID-19 exacerbating inequalities in the US. Lancet. 2020;395:1243–1244. doi: 10.1016/S0140-6736(20)30893-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Arasteh K. Prevalence of comorbidities and risks associated with COVID-19 among Black and Hispanic populations in New York City: an examination of the 2018 New York City Community Health Survey. J Racial Ethn Health Disparities. 2021;8:863–869. doi: 10.1007/s40615-020-00844-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cremer N.M., Baptist A.P. Race and asthma outcomes in older adults: results from the National Asthma Survey. J Allergy Clin Immunol Pract. 2020;8:1294–1301.e7. doi: 10.1016/j.jaip.2019.12.014. [DOI] [PubMed] [Google Scholar]
- 24.Stingone J.A., Ramirez O.F., Svensson K., Claudio L. Prevalence, demographics, and health outcomes of comorbid asthma and overweight in urban children. J Asthma. 2011;48:876–885. doi: 10.3109/02770903.2011.616615. [DOI] [PubMed] [Google Scholar]
- 25.Rogliani P., Sforza M., Calzetta L. The impact of comorbidities on severe asthma. Curr Opin Pulm Med. 2020;26:47–55. doi: 10.1097/MCP.0000000000000640. [DOI] [PubMed] [Google Scholar]
- 26.Booth A., Reed A.B., Ponzo S., Yassaee A., Aral M., Plans D., et al. Population risk factors for severe disease and mortality in COVID-19: a global systematic review and meta-analysis. PLoS One. 2021;16:e0247461. doi: 10.1371/journal.pone.0247461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Raharja A., Tamara A., Kok L.T. Association between ethnicity and severe COVID-19 disease: a systematic review and meta-analysis. J Racial Ethn Health Disparities. 2021;8:1563–1572. doi: 10.1007/s40615-020-00921-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reeves R., Rodrigue E., Kneebone E. The Brookings Institution; Washington, DC: 2016. Five Evils: Multidimensional Poverty and Race in America. [Google Scholar]
- 29.Shadmi E., Chen Y., Dourado I., Faran-Perach I., Furler J., Hangoma P., et al. Health equity and COVID-19: global perspectives. Int J Equity Health. 2020;19:104. doi: 10.1186/s12939-020-01218-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stringer S.M. Bureau of Policy & Research; New York: 2020. New York City’s Frontline Workers. Bureau of Policy & Research. [Google Scholar]
- 31.Willis D.E., Andersen J.A., Bryant-Moore K., Selig J.P., Long C.R., Felix H.C., et al. COVID-19 vaccine hesitancy: race/ethnicity, trust, and fear. Clin Trans Sci. 2021;14 doi: 10.1111/cts.13077. 2200-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kennedy B.R., Mathis C.C., Woods A.K. African Americans and their distrust of the health care system: healthcare for diverse populations. J Cult Divers. 2007;14:56–60. [PubMed] [Google Scholar]
- 33.Alsan M., Stantcheva S., Yang D., Cutler D. Disparities in coronavirus 2019 reported incidence, knowledge, and behavior among US adults. JAMA Network Open. 2020;3:e2012403. doi: 10.1001/jamanetworkopen.2020.12403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bierle D.M., Ganesh R., Wilker C.G., Hanson S.N., Moehnke D.E., Jackson T.A., et al. Influence of social and cultural factors on the decision to consent for monoclonal antibody treatment among high-risk patients with mild-moderate COVID-19. J Prim Care Community Health. 2021;12 doi: 10.1177/21501327211019282. 21501327211019282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cooper M.H., Christensen P.A., Salazar E., Perez K.K., Graviss E.A., Nguyen D., et al. Real-world assessment of 2879 COVID-19 patients treated with monoclonal antibody therapy: a propensity score–matched cohort study. Open Forum Infect Dis. 2021;8 doi: 10.1093/ofid/ofab512. ofab512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kim E.J., Marrast L., Conigliaro J. COVID-19: magnifying the effect of health disparities. J Gen Intern Med. 2020;35:2441–2442. doi: 10.1007/s11606-020-05881-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McElfish P.A., Purvis R., James L.P., Willis D.E., Andersen J.A. Perceived barriers to COVID-19 testing. Int J Environ Res Public Health. 2021;18:2278. doi: 10.3390/ijerph18052278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang Q., Lamichhane R., Diggs L.A. Disparities in emergency department visits in American children with asthma: 2006-2010. J Asthma. 2017;54:679–686. doi: 10.1080/02770903.2016.1263315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Van Poel E., Vanden Bussche P., Klemenc-Ketis Z., Willems S. How did general practices organize care during the COVID-19 pandemic: the protocol of the multi-country cross-sectional PRICOV-19 study. BMC Family Pract. 2022;23 doi: 10.1186/s12875-021-01587-6. Article no. 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Institute of Medicine (US) Committee on Institutional and Policy-Level Strategies for Increasing the Diversity of the U.S. Healthcare Workforce . National Academies Press; Washington, DC: 2004. In the Nation’s Compelling Interest: Ensuring Diversity in the Health-Care Workforce. [PubMed] [Google Scholar]
- 41.Kaundinya T., Kundu R.V. Diversity of skin images in medical texts: recommendations for student advocacy in medical education. J Med Educ Curric Dev. 2021:8. doi: 10.1177/23821205211025855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Esmail A. The prejudices of good people: leadership is needed to combat continued institutional racism. BMJ. 2004;328:1448–1449. doi: 10.1136/bmj.328.7454.1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.National Center for Immunization and Respiratory Diseases Health equity considerations and racial and ethnic minority groups. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html Accessed April 19, 2021.
- 44.Wortham JM, Lee JT, Althomsons S, Latash J, Davidson A, Guerra K. Characteristics of persons who died with COVID-19—United States, February 12–May 18, 2020. MMWR Morb Mortal Wkly Rep 2020;69:923–9. [DOI] [PubMed]
- 45.Castro A. United Nations Development Program and UNICEF; New York: 2020. Challenges posed by the COVID-19 pandemic in the health of women, children, and adolescents in Latin America and the Caribbean. COVID-19 Latin American and the Caribbean Policy Documents Series 19. [Google Scholar]
- 46.Bailey Z.D., Krieger N., Agénor M., Graves J., Linos N., Bassett M.T. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389:1453–1463. doi: 10.1016/S0140-6736(17)30569-X. [DOI] [PubMed] [Google Scholar]
- 47.FitzGerald C., Martin A., Berner D., Hurst S. Interventions designed to reduce implicit prejudices and implicit stereotypes in real world contexts: a systematic review. BMC Psychol. 2019;7:29. doi: 10.1186/s40359-019-0299-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Organization for Economic Co-operation and Development Strengthening the frontline: how primary health care helps health systems adapt during the COVID-19 pandemic. https://www.oecd.org/coronavirus/policy-responses/strengthening-the-frontline-how-primary-health-care-helps-health-systems-adapt-during-the-covid-19-pandemic-9a5ae6da/ Accessed February 10, 2021.