Abstract
Severe COVID-19 is associated with a systemic hyperinflammatory response leading to acute respiratory distress syndrome (ARDS), multi-organ failure, and death. Galectin-3 is a ß-galactoside binding lectin known to drive neutrophil infiltration and the release of pro-inflammatory cytokines contributing to airway inflammation. Thus, we aimed to investigate the potential of galectin-3 as a biomarker of severe COVID-19 outcomes. We prospectively included 156 patients with RT-PCR confirmed COVID-19. A severe outcome was defined as the requirement of invasive mechanical ventilation (IMV) and/or in-hospital death. A non-severe outcome was defined as discharge without IMV requirement. We used receiver operating characteristic (ROC) and multivariable logistic regression analysis to determine the prognostic ability of serum galectin-3 for a severe outcome. Galectin-3 levels discriminated well between severe and non-severe outcomes and correlated with markers of COVID-19 severity, (CRP, NLR, D-dimer, and neutrophil count). Using a forward-stepwise logistic regression analysis we identified galectin-3 [odds ratio (OR) 3.68 (95% CI 1.47–9.20), p < 0.01] to be an independent predictor of severe outcome. Furthermore, galectin-3 in combination with CRP, albumin and CT pulmonary affection > 50%, had significantly improved ability to predict severe outcomes [AUC 0.85 (95% CI 0.79–0.91, p < 0.0001)]. Based on the evidence presented here, we recommend clinicians measure galectin-3 levels upon admission to facilitate allocation of appropriate resources in a timely manner to COVID-19 patients at highest risk of severe outcome.
Subject terms: Predictive markers, Viral infection
Introduction
Coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection has afflicted tens of millions of people in a worldwide pandemic, straining health care systems across the world1,2. Prognostic biomarkers that can identify high-risk patients are needed to improve clinical management and allow appropriate allocation of healthcare resources. Moreover, the lack of current curative therapies emphasizes the need to get a better understanding of the pathophysiological process behind SARS-CoV-2 infection and its long-term consequences for the development of targeted therapeutic strategies.
Severe COVID-19 is associated with a systemic hyperinflammatory response characterized by high levels of circulating cytokines and chemokines3 and substantial lung infiltration of innate immune cells4 that can lead to acute respiratory distress syndrome (ARDS), multi-organ failure and death5,6. Among the inflammatory cytokines are those associated with the activation of monocyte/macrophages such as Interleukin 6 (IL-6), Tumor necrosis factor (TNF), and the CC-chemokine ligand 2 (CCL2)3,6,7.
Studies have shown that those inflammatory cytokines contribute to the recruitment of additional inflammatory cells that not only aggravate the lung damage, but also lead to pulmonary fibrosis8,9. Subsets of M2 macrophages expressing profibrogenic genes have been found in the bronchoalveolar lavage of COVID-19 patients4, reflecting that the pathological process of SARS-CoV-2 infection not only involves an acute inflammatory response in the lungs, but is also associated with fibrotic complications10.
Galectin-3 is a 29–35 kDa ß-galactoside binding lectin11 known to enhance the effects of viral infection by promoting host inflammatory responses12,13 and the release of several cytokines including IL-6 and TNF-α14, which are some of the major cytokines present in severe COVID-19 patients3. High levels of galectin-3 have been shown to drive neutrophil infiltration contributing to acute airway inflammation15–17, and are associated with disease severity and mortality in ARDS patients18. Galectin-3 is increasingly recognized as a potentially important diagnostic or prognostic biomarker for a variety of inflammatory and fibrotic diseases19–21 and has been found to be elevated in patients with idiopathic pulmonary fibrosis22,23 and more recently in COVID-19 patients24,25. Inflammation and fibrosis are key contributing mechanisms to the progression of severe COVID-19 and the development of its long-term consequences3,10,26 .
Given the known proinflammatory and profibrotic roles of galectin-3, the aim of this study was to analyze the prognostic value of serum galectin-3 upon hospital admission to predict patients at high-risk of progressing to a severe COVID-19 outcome resulting in invasive mechanical ventilation (IMV) and/or death.
Methods
Study design and population
This single-center, prospective observational study was performed in COVID-19 patients admitted to the Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán (INCMNSZ), one of the largest designated institutions in Mexico for the hospitalization of patients with COVID-19 between April and October 2020. The inclusion criteria were patients ≥ 18 years with laboratory confirmed COVID-19 by real-time reverse transcriptase-polymerase chain reaction (RT-PCR). We excluded pregnant women.
Primary outcome definition
Patients who required IMV and/or died during hospitalization were categorized as having a severe outcome. Patients who recovered and were discharged without requiring IMV were categorized as having a non-severe outcome.
Data collection
Clinical and laboratory data were extracted from the electronic medical records including: Demographics (age, gender, and comorbidities), clinical (days of hospital stay), radiological (chest CT findings), laboratory and patient outcome data (need for IMV and/or death). Laboratory data included, complete blood count, triglycerides, albumin, AST, International Normalized Ratio (INR), thrombo-inflammatory markers (D-dimer, fibrinogen and ferritin) and C-reactive protein (CRP). All information was recorded in a specific database. Data was independently reviewed by 2 investigators to verify the correct collection of the data.
Sample collection and Galectin-3 levels measurement
Blood samples were collected upon hospital admission from all COVID-19 patients fulfilling inclusion criteria. Samples were centrifuged at 3000 rpm for 10 min, and serum was aliquoted and stored at − 70 °C until further analysis. Galectin-3 was measured in the serum samples using a commercial enzyme-linked immunosorbent assay (ELISA) Kit (Invitrogen, #BMS 279-4, Carlsbad, CA, USA), according to the manufacturing instructions. The detection limit of this kit is 0.29 ng/mL and a mean recovery of 100% after spike recovery and linearity of dilution assessments is reported. All samples were evaluated in duplicate. The inter-assay coefficient of variation was 8.52% and the intra-assay 5.34%. Galectin-3 levels in COVID-19 patients were compared against those of age-matched healthy control subjects analyzed before the pandemic, between 2018 and 2019.
Statistical analysis
Data are expressed as frequencies for categorical variables and as mean with standard deviation (SD) or median with interquartile range (IQR) for continuous variables according to their normality as assessed by the Kolmogorov–Smirnov test. Student’s t-tests or Mann–Whitney U tests were used for univariate statistical comparisons, while correlation analyses were performed with Spearman's correlation coefficient for pairs of continuous variables. To determine the prognostic ability of galectin-3 and inflammatory markers for the primary outcome, receiver operating characteristic (ROC) curves were plotted, and cut-point values were chosen as those with the highest Youden’s J statistic. Comparisons between AUCs obtained were performed with DeLong's test for correlated ROC curves. Independent predictors of the primary outcome were determined after performing a multivariable logistic regression analysis with the forward-stepwise selection method. Analyzed variables were those with a p value < 0.20 after univariate analyses. Only those variables chosen by the stepwise procedure were reported in Table 3. Goodness of the fit was assessed with the Hosmer–Lemeshow test. The combined power of the identified independent predictors was evaluated with a ROC curve using the model selected by the stepwise logistic regression procedure. Statistical analyses were performed with SPSS (version 24.0, SPSS Inc., Chicago, IL, USA) and GraphPad Prism (version 8.00, GraphPad Software, La Jolla, CA, USA). A selected alpha level of 0.05 indicated statistical significance.
Table 3.
Univariate and multivariable logistic regression analyses for severe outcome.
| Variable | Univariate | Multivariable | p value (individual AUC vs. model AUC) | ||||
|---|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | p value | Odds ratio | 95% CI | p value | ||
| Galectin-3 (binary) | 7.94 | (3.75–16.82) | < 0.0001 | 3.68 | (1.47–9.20) | < 0.01 | < 0.001 |
| CRP | 1.11 | (1.07–1.16) | < 0.0001 | 1.05 | (1.00–1.11) | 0.04 | 0.03 |
| Albumin | 0.14 | (0.06–0.33) | < 0.0001 | 0.35 | (0.13–0.89) | 0.03 | 0.03 |
| Critical disease (CT pulmonary affection > 50%) | 7.86 | (3.25–19.03) | < 0.0001 | 4.04 | (1.17–13.97) | 0.03 | < 0.0001 |
| Gender (male) | 1.99 | (0.93–4.25) | 0.08 | ||||
| Age | 1.02 | (1.00–1.05) | 0.10 | ||||
| Diabetes | 1.62 | (0.74–3.57) | 0.23 | ||||
| Hypertension | 0.98 | (0.48–2.01) | 0.96 | ||||
| Obesity (BMI ≥ 30) | 1.14 | (0.59–2.21) | 0.71 | ||||
| NLR | 1.05 | (1.02–1.09) | < 0.01 | ||||
| Neutrophil count | 1.15 | (1.07–1.23) | < 0.001 | ||||
| Ferritin | 1.00 | (1.07–1.23) | < 0.01 | ||||
| Lymphocyte count | 0.63 | (0.28–1.42) | 0.27 | ||||
| Platelets | 1.00 | (1.00–1.00) | 0.89 | ||||
| D-Dimer | 1.00 | (1.00–1.00) | 0.03 | ||||
| Fibrinogen | 1.00 | (1.00–1.01) | < 0.01 | ||||
| INR | 2.06 | (1.01–4.24) | 0.05 | ||||
| Triglycerides | 1.01 | (1.00–1.01) | 0.02 | ||||
| AST | 1.01 | (1.00–1.02) | 0.03 | ||||
Galectin-3 was analyzed as a binary variable according to its non-linear relationship with severe outcomes (> 30.99 ng/mL = 1, < 30.99 ng/mL = 0). Only variables with a p value < 0.20 after univariate analyses were further evaluated in multivariable analyses. The AUC of the final model was compared against that of each independent predictor with DeLong’s test for correlated ROC curves. Bold values represent p < 0.05.
Ethics approval and consent to participate
This study was approved by INCMNSZ’s Research Ethics Committee (No. GAS-3385-20-20-1) and complied with the provisions of the Declaration of Helsinki. Informed written consent was obtained from all patients prior to blood sample collection.
Results
Demographic, clinical and laboratory characteristics
A total of 156 patients with RT-PCR-confirmed SARS-CoV-2 infection and CT findings were enrolled in the study. The mean age in the overall population was 53.24 ± 13.22 years, of which 107 (68.6%) were male and 49 (31.4%) females. Based on our primary outcome definition, 54 (34.6%) patients progressed to a severe outcome and 102 (65.4%) to a non-severe outcome (Supplementary Fig. S1).
There were no differences in age, gender, or body mass index (BMI) between patients with severe and non-severe outcome. The principal comorbidities among our cohort were obesity (44.2%), hypertension (30.1%) and diabetes (21.2%), all of which had been diagnosed prior to hospital admission.
Patients with a severe outcome had a significantly longer hospital stay compared to non-severe outcome patients (16 [6–26] vs. 7 [5–9], p < 0.0001). From the 54 patients with severe outcome, 47 (87%) had a critical disease with > 50% of lung damage, and only 7 (13%) presented a moderate disease with < 50% of lung damage. Whereas from the 102 patients with non-severe outcome, 47 (46.1%) had critical disease and 55 (53.9%) moderate disease. (Table 1).
Table 1.
Demographic, clinical and laboratory characteristics.
| Total (n = 156) | Severe outcome (n = 54) | Non-severe outcome (n = 102) | p value | |
|---|---|---|---|---|
| Age | 53.24 ± 13.22 | 54.63 ± 11.52 | 50.97 ± 13.92 | 0.10 |
| Gender, male | 107 (68.6%) | 42 (39.3%)* | 65 (60.7%)* | 0.07 |
| Gender, female | 49 (31.4%) | 12 (24.5%)* | 37 (75.5%)* | |
| BMI | 29.42 (26.74–33.78) | 29.35 (26.79–32.89) | 29.42 (26.80–33.40) | 0.77 |
| Normal | 21 (13.5%) | 4 (19.0%)* | 17 (81.0%)* | 0.14 |
| Overweight | 66 (42.3%) | 25 (37.9%)* | 41 (62.1%)* | 0.46 |
| Obesity | 69 (44.2%) | 25 (36.2%)* | 44 (63.8%)* | 0.71 |
| Hypertension | 47 (30.1%) | 17 (36.2%)* | 30 (63.8%)* | 0.96 |
| Diabetes | 33 (21.2%) | 15 (45.5%)* | 18 (54.5%)* | 0.23 |
| Alcohol consumption | 60 (38.5%) | 24 (40.0%)* | 36 (60.0%)* | 0.28 |
| Days of hospital stay | 7 (5–14) | 16.5 (6–26) | 7 (5–9) | < 0.0001 |
| IMV | 51 (32.7%) | 51 (94.4%) | 0 (0.0%) | < 0.0001 |
| Mortality | 21 (13.5%) | 21(38.9%) | 0 (0.0%) | < 0.0001 |
| CT pulmonary affection | ||||
| > 50%, critical disease | 94 (60.3%) | 47 (87.0%) | 47 (46.1%) | < 0.0001 |
| < 50%, moderate disease | 62 (39.7%) | 7 (13.0%) | 55 (53.9%) | |
| Laboratory tests | ||||
| Galectin-3 (ng/ml) | 28.77 (17.52–42.04) | 41.17 (29.71–52.25) | 23.76 (15.78–33.97) | < 0.0001 |
| Neutrophil count (× 103/µl) | 6.83 (4.13–10.61) | 9.4 (5.98–14.28) | 6 (3.54–9) | < 0.0001 |
| Lymphocyte count (× 103/µl) | 0.77 (0.53–1.05) | 0.7 (0.48–0.98) | 0.84 (0.57–1.09) | 0.09 |
| NLR | 8.43 (5.29–17.68) | 14.22 (7.94–23.32) | 6.97 (4.09–12.89) | < 0.0001 |
| Fibrinogen | 645 (482–772) | 682 (592.5–848.75) | 616.5 (455.5–738) | < 0.01 |
| Ferritin (ng/ml) | 500.47 (292.25–1020.5) | 722.7 (339.4–1167) | 376.4 (227.3–851.6) | < 0.01 |
| D-Dimer (ng/ml) | 698.5 (459.5–1178.5) | 1176 (528.8–2510) | 604.5 (400.8–928.8 ) | < 0.0001 |
| CRP (mg/dl) | 14 (6.13–23.01) | 20.96 (14.42–29.17) | 9.38 (4.48–19.1) | < 0.0001 |
| INR | 1.1 (1–1.2) | 1 (1.1–1.2) | 1.1 (1–1.2) | 0.03 |
| Platelets (K/μl) | 224.25 (191–288) | 220.7 (185.5–300) | 234 (193–290) | 0.66 |
| Albumin (g/dl) | 3.7 ± 0.54 | 3.44 ± 0.47 | 3.89 ± 0.49 | < 0.0001 |
| AST (U/L) | 36.25 (26.8–59.9) | 43.26 (33–65) | 31.62 (23.1–56.7) | < 0.001 |
| Triglycerides (mg/dL) | 152 (115.5–199.5) | 175 (127.8–224.8) | 137.5 (112–193.3) | 0.011 |
Data are reported as median (IQR), mean (± SD) and n (%).Comparisons were performed with Pearson’s Chi-squared test or Fisher’s exact test and either Student’s t-test or Mann–Whitney U test. Bold values represent p < 0.05.
BMI Body mass index.
Laboratory characteristics including complete blood count, inflammatory and thrombo-inflammatory markers, AST and coagulation tests for both groups are depicted in Table 1.
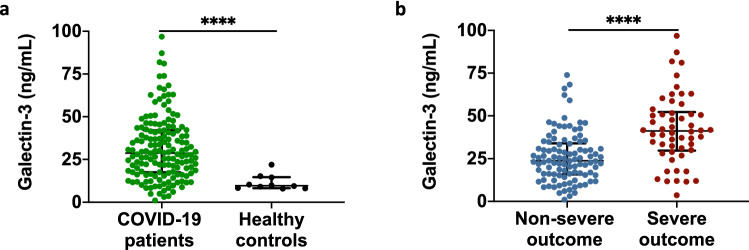
Galectin-3 serum levels are higher in COVID-19 patients with a severe outcome
To explore the possible role of galectin-3 as a biomarker of severity, circulating levels were measured in sera from COVID-19 patients using a commercial ELISA kit. We found that COVID-19 patients upon hospital admission had significantly elevated circulating levels of galectin-3 when compared to age-matched pre-pandemic healthy subjects (28.77 ng/mL [17.52–42.04] vs. 9.65 ng/mL [8.27–14.71], p < 0.0001) (Fig. 1a). Patients who developed a severe outcome, including IMV and/or in-hospital death, had significantly higher galectin-3 levels than those with a non-severe outcome (41.17 ng/mL [29.71–52.25] vs. 23.76 ng/mL [15.78–33.97], p < 0.0001) (Fig. 1b).
Figure 1.
Galectin-3 serum levels in COVID-19 patients. (a) Galectin-3 circulating levels upon hospital admission of COVID-19 patients (n = 156) and age-matched healthy pre-pandemic controls (n = 10). (b) Severe outcomes in COVID-19 patients were associated with elevated levels of galectin-3. Data in (a, b) are shown as median with IQR. ****p < 0.0001; two-tailed Mann–Whitney U test or two-tailed t-test. Samples were assessed in duplicate in ELISA assays.
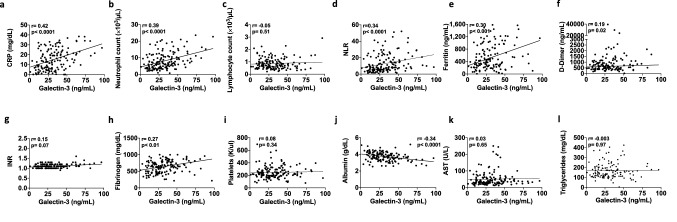
Galectin-3 correlates with other inflammatory biomarkers
Given that elevated galectin-3 levels were found in patients who progressed to a severe outcome, and considering its participation in the inflammatory response, correlations with inflammatory parameters previously studied in COVID-19 using the spearman correlation coefficient, in accordance with the non-normal distribution of the data were carried out. We found that galectin-3 correlates positively with CRP (r = 0.42, p < 0.0001), neutrophil count (r = 0.39, p < 0.0001), NLR (r = 0.34, p < 0.0001), ferritin (r = 0.30, p < 0.001), D-dimer (r = 0.19, p = 0.02) and fibrinogen (r = 0.27, p < 0.01), whereas a negative correlation was found with albumin (r = 0.35, p < 0.0001) (Fig. 2a–l).
Figure 2.
Galectin-3 correlates with inflammatory markers in COVID-19 patients. Spearman correlations show significant associations between galectin-3 and commonly measured inflammatory markers in SARS-CoV-2 infected patients. (a) CRP, (b) Neutrophil count, (c) Lymphocyte count, (d) NLR, (e) Ferritin, (f) D-dimer, (g) INR, (h) Fibrinogen, (i) Platelets, (j) Albumin, (k) AST and (l) Triglycerides.
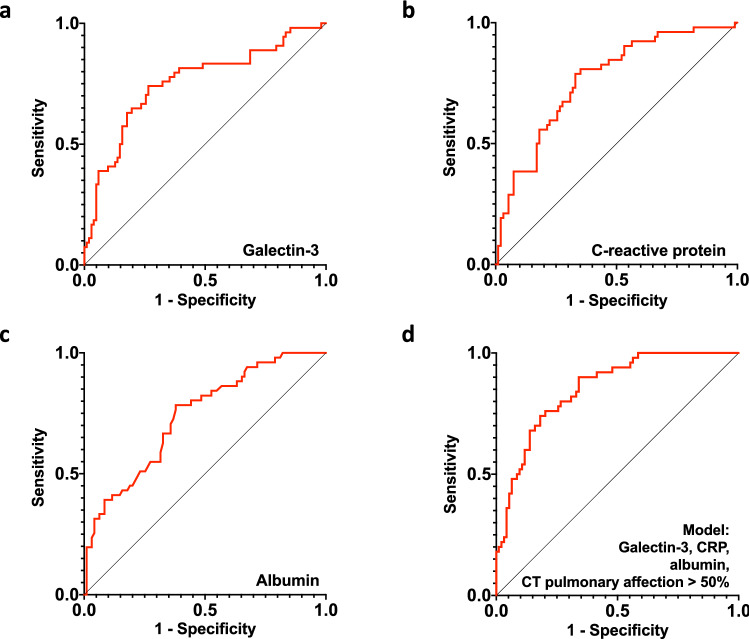
Galectin-3 in combination with CRP, albumin and CT pulmonary affection accurately predicts severity in COVID-19 patients
To assess the discriminative ability of galectin-3 as a predictor of severe outcome, ROC curves were plotted. Galectin-3 discriminates well between those with severe and non-severe outcome, with an AUC of 0.75 (95% CI 0.67–0.84, p < 0.0001), and a cut-point of 30.99 ng/mL (74.07% sensitivity, 73.53% specificity) (Fig. 3a). Other inflammatory and thromboinflammatory parameters studied in COVID-19 could also discriminate patients with severe outcome, except for lymphocyte count and platelets (Table 2).
Figure 3.
Galectin-3, CRP, albumin and CT pulmonary affection > 50% as independent predictors of severe outcome in COVID-19 patients. Receiver-operating characteristic curves (ROCs) of the independent predictors for the classification of binary outcomes (severe/non-severe) using (a) galectin-3, (b) CRP, (c) albumin and (d) the combined predicted probabilities of galectin-3, CRP albumin and CT pulmonary affection > 50%.
Table 2.
Discrimination power of other inflammatory and thromboinflammatory markers for severe outcome and comparison with galectin-3.
| Biomarker | AUC | 95% CI | p value | p value (comparison with galectin-3 AUC) |
|---|---|---|---|---|
| Galectin-3 | 0.75 | (0.67–0.84) | < 0.0001 | – |
| CRP | 0.76 | (0.68–0.85) | < 0.0001 | 0.70 |
| Albumin | 0.73 | (0.65–0.82) | < 0.0001 | 0.93 |
| NLR | 0.71 | (0.62–0.79) | < 0.0001 | 0.52 |
| Neutrophil count | 0.70 | (0.61–0.78) | < 0.0001 | 0.43 |
| Ferritin | 0.66 | (0.57–0.76) | < 0.01 | 0.19 |
| Lymphocyte count | 0.58 | (0.49–0.68) | 0.09 | 0.02 |
| Platelets | 0.48 | (0.38–0.58) | 0.66 | < 0.01 |
| D-Dimer | 0.69 | (0.60–0.79) | < 0.001 | 0.49 |
| Fibrinogen | 0.66 | (0.57–0.75) | < 0.01 | 0.16 |
| INR | 0.61 | (0.51–0.71) | 0.04 | 0.05 |
| Triglycerides | 0.64 | (0.54–0.74) | 0.01 | 0.12 |
| AST | 0.68 | (0.59–0.76) | < 0.001 | 0.27 |
ROC curves were performed to determine the discrimination power of each biomarker for severe outcome. The AUC obtained was compared against that of galectin-3 using DeLong’s test for correlated ROC curves. Bold values represent p < 0.05.
Based on the above, we performed a forward-stepwise logistic multivariate regression analysis to identify independent demographic and laboratory parameters that predict and strongly correlated with severe outcome, and thus with disease progression (i.e., IMV and/or death). A smoothing spline of galectin-3 showed a non-linear relationship with severe outcome; therefore, we used the Youden’s J statistic to determine the ideal binary cut-point of galectin-3 for classifying severe outcomes (Supplementary Fig. S2a). Variables assessed in univariate analyses included age, gender, comorbidities and inflammatory parameters (Table 3). The final model selected via the stepwise procedure included galectin-3 (odds ratio [OR] 3.68 [95% CI 1.47–9.20], p < 0.01), critical disease (CT pulmonary affection > 50%) (4.04 [95% CI 1.17–13.97], p = 0.03), CRP (OR 1.05 [95% CI 1.00–1.11], p = 0.04), and low albumin levels upon admission (OR 0.35 [95% CI 0.13–0.89], p = 0.03) when regressed on severe outcome (IMV and/or death; Hosmer–Lemeshow goodness of fit test p = 0.74; Table 3). Of note, CRP and albumin were entered as continuous variables according to their smoothing splines which showed linear relationships with severe outcome (Supplementary Fig. S2b,c). The equation fitted by this logistic regression model was the following, where : = 0.649 + [1.302 * binary galectin-3] + [1.396 * CT pulmonary affection] + [0.052 * CRP] − [1.062 * albumin], where galectin-3 is coded as binary (less than 30.99 ng/mL with 0 and above 30.99 ng/mL with 1) as well as CT pulmonary affection (< 50% or moderate disease with 0 and > 50% or critical disease with 1) and CRP and albumin as continuous variables. The obtained values were transformed into predicted probabilities with the formula exp ()/(1 + exp ()).
We also explored the binary cut-points of the other two biomarkers obtained from the model, (CRP and albumin), to classify severe outcomes (Fig. 3b,c, respectively). CRP had an AUC of 0.76 (95% CI 0.68–0.85, p < 0.0001) and a cut-point of 14.04 mg/dL (78.85% sensitivity, 67.02% specificity), while albumin had an AUC of 0.73 (95% CI 0.65–0.82, p < 0.0001) with a 3.74 g/dL cut-point (78.43% sensitivity, 62.11% specificity). We then assessed if the model proposed by the logistic regression analyses could better predict severe outcome in COVID-19 patients than either predictor on its own. To determine this, the predicted probabilities for this combination of values were computed and plotted in a ROC curve (Fig. 3d). Its AUC showed an enhanced ability to classify severe outcome (0.85 [95% CI 0.79–0.91], p < 0.0001) and was significantly higher compared to the individual AUC of each independent predictor (Table 3).
Discussion
In this prospective cohort of COVID-19 patients, we assessed the classification performance of circulating galectin-3 levels obtained upon hospitalization on the development of a severe outcome, defined as requirement of IMV and/or death. We hypothesized that this molecule could be associated with symptom severity due to its known involvement in the exacerbated inflammatory response, a feature that has been exhibited in COVID-19 patients3.
Evidence in the literature has implicated the cytokine release syndrome as the main factor responsible for the high mortality observed in COVID-19 patients27. Disease progression is associated with ARDS characterized by diffuse alveolar damage in the lung caused by the severe inflammatory process28. ARDS in COVID-19 leads to more severe outcomes than ARDS due to other causes29 with a general mortality of 26–61.5% in those admitted to the intensive care unit, and significantly higher in those requiring IMV (65.7% to 94%)29.
Galectin-3 has been shown to orchestrate the inflammatory response syndrome activating immune cells and triggering the release of inflammatory cytokines30,31.
This study presents for the first time an important connection between galectin-3 and the hyperinflammatory state in COVID-19 patients. Our observations reveal that higher galectin-3 levels upon admission are found in those patients with severe outcome. Values greater than 30.99 ng/mL have a high sensitivity and specificity to predict an adverse clinical course with the possibility of requiring IMV and/or death which might indicate its possible role in the pathophysiology of ARDS reflecting the excessive inflammatory response associated with this syndrome.
While IMV is intended to minimize the progression of lung injury32, it has also been demonstrated to induce or aggravate lung damage and in the long-run may contribute to lung fibrosis4,33. Chronic pulmonary fibrosis has been observed in recovered COVID-19 patients10,26. Galectin-3 is known to play a role in the pathogenesis of pulmonary fibrosis, and clinical trials testing galectin-3 inhibitors are currently underway for the treatment of idiopathic pulmonary fibrosis34. Targeting Galectin-3 has been suggested as treatment for COVID-19 not only due to its role in fibrosis and systemic inflammation, but also due to its potential involvement in the virus-host interaction mediated by the N-terminal domain of SARS-CoV-235,36. Given the known sequence and functional similarities between the N-acetylneuraminic acid binding domain on the spike protein of SARS-CoV-2 and human galectin-336, it is possible that by targeting galectin-3, we might also interfere with viral-host interactions, thus potentially decreasing viral load and the resulting inflammatory responses associated with the infection.
Galectin-3 significantly correlated with several inflammatory and thrombo-inflammatory biomarkers, indicating its pathophysiological implication in COVID-19’s inflammatory response. Many of the classic biomarkers used in COVID-19 including CRP, NLR, Ferritin, neutrophil count, D-dimer, among others, had a significant discriminating ability for severe outcome on their own, however after the selection of variables via forward stepwise in the multivariate, many were no longer significant, likely due to collinearity. However, galectin-3 remained an independent predictor of severe outcome even after adjusting for age, gender, comorbidities, and those other inflammatory parameters. CRP, an acute inflammatory biomarker with ability to predict mortality in COVID-1937,38, was also identified as an independent predictor of severe outcome in our cohort and had a positive correlation with galectin-3. This novel association between galectin-3 and CRP has not been reported in viral infection, much less in COVID-19 but it suggests the utility of this molecule in detecting the inflammatory state of patients upon hospital arrival. As both CRP and galectin-3 were identified as independent predictors, we sought to identify which one would perform better according to its association with patient outcome. The non-linear relationship of galectin-3, observed in a smoothing spline, demonstrated that higher levels of this lectin were a common characteristic of patients at high-risk of progressing to a severe COVID-19 outcome. We consider that inflammatory markers such as CRP which tend to show a linear relationship with outcome may not be suitable as efficient biomarkers given their inconsistency, which is reflected in the various cut-off values thus far reported. This may partially explain the fact that although numerous inflammatory biomarkers have been widely described as predictors of severity in COVID-19, their measurement and use in clinical practice is lacking. Measuring Galectin-3 may present an advantage given its accuracy and the simplicity of using a binary cut-point to classify patients as having low or high risk for severe outcomes due to its non-linear spline.
We also identified hypoalbuminemia as a common characteristic among critically ill patients which was negatively correlated with galectin-3. Albumin is an important biomarker that reflects the inflammatory state, as its production is decreased due to higher levels of IL-639. Observations carried out by Huang et al. in a large cohort of COVID-19 patients identified the decrease in albumin levels as a significant indicator of progression to a critical stage and death. They associated this pathologic finding with a reduced capacity of synthesis by hepatocytes as mild hepatic injury was evident40. Another aspect relevant to consider is that capillary leakage into the interstitial space increases in severe illness such as sepsis, leading to the sequestration of albumin41. As galectin-3 was found to reflect the hyperinflammatory state of patients, its predictive ability together with CRP, albumin and CT pulmonary affection > 50% was tested. Results revealed that when used jointly, severe outcomes can be more accurately classified upon hospital admission (AUC = 0.85), thus providing clinicians more resources to efficiently identify patients with higher odds of adverse progression.
There are some limitations to our study. First, since this is a single-center experience, data from different populations and a multicenter analysis will be needed for validation. Second, due to the small sample size, further clinical studies with larger sample sizes are required to confirm these findings before galectin-3 can definitively be recommended in the hospital setting. Despite these limitations, this study demonstrates in a prospective cohort of COVID-19 patients at one of the largest health institutes in Mexico that measurement of galectin-3 levels upon hospital admission could be helpful in predicting disease progression. Finally, the combined use of galectin-3, CRP, albumin and CT pulmonary affection > 50% showed strong predictive ability, and thus could aid to efficiently allocate medical resources before patients develop an adverse outcome.
Conclusion
We have offered evidence on the prognostic use of galectin-3 in SARS-CoV-2 infected patients which may extend to other critical diseases and propose its combined use with other inflammatory markers to guide the clinical rationale when assessing a hospitalized patient’s risk.
Supplementary Information
Abbreviations
- ARDS
Acute respiratory distress syndrome
- COVID-19
Coronavirus disease 2019
- CRP
C-Reactive protein
- CT
Computerized tomography
- IMV
Invasive mechanical ventilation
- SARS-CoV-2
Severe acute respiratory syndrome coronavirus 2
Author contributions
N.L.R., E.C.A. and N.N.A. conceived and designed the study. N.L.R., E.C.A., M.S.M., P.V.S., M.P.J., F.R.A., B.I.V.M., E.A.A., J.M.E.V., J.A., O.M.G., F.T.D., J.T.R., D.G.M., and N.N.A., collected clinical data. N.L.R., E.C.A. and N.N.A. contributed to data analysis. K.L.C. and O.M.G. provided input on statistical methods. N.L.R. and E.C.A. wrote the manuscript and generated tables and figures. N.N.A., C.A.H., D.K. and K.L.C. contributed to the manuscript review. All authors critically reviewed and approved the final version of the manuscript.
Funding
This work was supported by the Grant #312285 from Consejo Nacional de Ciencia y Tecnología (CONACYT)-México (N.N.A.) and University of Colorado Anschutz Medical Campus Department of Surgery Academic Enrichment Fund (C.A.H.)
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request. All data generated during this study are included in this published article.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Eduardo Cervantes-Alvarez and Nathaly Limon-de la Rosa.
Contributor Information
Christene A. Huang, Email: christene.huang@cuanschutz.edu
Nalu Navarro-Alvarez, Email: nalu.navarroa@incmnsz.mx.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-022-05968-4.
References
- 1.Zhou F, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/s0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. Int. J. Antimicrob. Agents. 2020;55:105924. doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Del Valle DM, et al. An inflammatory cytokine signature predicts COVID-19 severity and survival. Nat. Med. 2020;26:1636–1643. doi: 10.1038/s41591-020-1051-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liao M, et al. Single-cell landscape of bronchoalveolar immune cells in patients with COVID-19. Nat. Med. 2020;26:842–844. doi: 10.1038/s41591-020-0901-9. [DOI] [PubMed] [Google Scholar]
- 5.Baksh M, Ravat V, Zaidi A, Patel RS. A systematic review of cases of acute respiratory distress syndrome in the coronavirus disease 2019 pandemic. Cureus. 2020;12:e8188. doi: 10.7759/cureus.8188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang J, Jiang M, Chen X, Montaner LJ. Cytokine storm and leukocyte changes in mild versus severe SARS-CoV-2 infection: Review of 3939 COVID-19 patients in China and emerging pathogenesis and therapy concepts. J. Leukoc. Biol. 2020;108:17–41. doi: 10.1002/JLB.3COVR0520-272R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Merad M, Martin JC. Pathological inflammation in patients with COVID-19: A key role for monocytes and macrophages. Nat. Rev. Immunol. 2020;20:355–362. doi: 10.1038/s41577-020-0331-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Burnham EL, Janssen WJ, Riches DW, Moss M, Downey GP. The fibroproliferative response in acute respiratory distress syndrome: Mechanisms and clinical significance. Eur. Respir. J. 2014;43:276–285. doi: 10.1183/09031936.00196412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schupp JC, et al. Macrophage activation in acute exacerbation of idiopathic pulmonary fibrosis. PLoS ONE. 2015;10:e0116775. doi: 10.1371/journal.pone.0116775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Spagnolo P, et al. Pulmonary fibrosis secondary to COVID-19: A call to arms? Lancet Respir. Med. 2020;8:750–752. doi: 10.1016/S2213-2600(20)30222-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barondes SH, Cooper DN, Gitt MA, Leffler H. Galectins. Structure and function of a large family of animal lectins. J. Biol. Chem. 1994;269:20807–20810. doi: 10.1016/S0021-9258(17)31891-4. [DOI] [PubMed] [Google Scholar]
- 12.Henderson NC, Sethi T. The regulation of inflammation by galectin-3. Immunol. Rev. 2009;230:160–171. doi: 10.1111/j.1600-065X.2009.00794.x. [DOI] [PubMed] [Google Scholar]
- 13.Chen YJ, et al. Galectin-3 enhances avian H5N1 influenza a virus-induced pulmonary inflammation by promoting NLRP3 inflammasome activation. Am. J. Pathol. 2018;188:1031–1042. doi: 10.1016/j.ajpath.2017.12.014. [DOI] [PubMed] [Google Scholar]
- 14.Filer A, et al. Galectin 3 induces a distinctive pattern of cytokine and chemokine production in rheumatoid synovial fibroblasts via selective signaling pathways. Arthritis Rheumatol. 2009;60:1604–1614. doi: 10.1002/art.24574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kuwabara I, Liu FT. Galectin-3 promotes adhesion of human neutrophils to laminin. J. Immunol. 1996;156:3939–3944. [PubMed] [Google Scholar]
- 16.Sano H, et al. Human galectin-3 is a novel chemoattractant for monocytes and macrophages. J. Immunol. 2000;165:2156–2164. doi: 10.4049/jimmunol.165.4.2156. [DOI] [PubMed] [Google Scholar]
- 17.Frigeri LG, Zuberi RI, Liu FT. Epsilon BP, a beta-galactoside-binding animal lectin, recognizes IgE receptor (Fc epsilon RI) and activates mast cells. Biochemistry. 1993;32:7644–7649. doi: 10.1021/bi00081a007. [DOI] [PubMed] [Google Scholar]
- 18.Xu Z, et al. The predictive value of plasma galectin-3 for ARDS severity and clinical outcome. Shock. 2017;47:331–336. doi: 10.1097/SHK.0000000000000757. [DOI] [PubMed] [Google Scholar]
- 19.de Boer RA, et al. The fibrosis marker galectin-3 and outcome in the general population. J. Intern. Med. 2012;272:55–64. doi: 10.1111/j.1365-2796.2011.02476.x. [DOI] [PubMed] [Google Scholar]
- 20.Hara A, et al. Galectin-3 as a next-generation biomarker for detecting early stage of various diseases. Biomolecules. 2020 doi: 10.3390/biom10030389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lok DJ, et al. Prognostic value of galectin-3, a novel marker of fibrosis, in patients with chronic heart failure: Data from the DEAL-HF study. Clin. Res. Cardiol. 2010;99:323–328. doi: 10.1007/s00392-010-0125-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mackinnon AC, et al. Regulation of transforming growth factor-beta1-driven lung fibrosis by galectin-3. Am. J. Respir. Crit. Care Med. 2012;185:537–546. doi: 10.1164/rccm.201106-0965OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nishi Y, et al. Role of galectin-3 in human pulmonary fibrosis. Allergol. Int. 2007;56:57–65. doi: 10.2332/allergolint.O-06-449. [DOI] [PubMed] [Google Scholar]
- 24.De Biasi S, et al. Marked T cell activation, senescence, exhaustion and skewing towards TH17 in patients with COVID-19 pneumonia. Nat. Commun. 2020;11:3434. doi: 10.1038/s41467-020-17292-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kalfaoglu B, Almeida-Santos J, Tye CA, Satou Y, Ono M. T-cell hyperactivation and paralysis in severe COVID-19 infection revealed by single-cell analysis. Front. Immunol. 2020;11:589380. doi: 10.3389/fimmu.2020.589380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.George PM, Wells AU, Jenkins RG. Pulmonary fibrosis and COVID-19: The potential role for antifibrotic therapy. Lancet Respir. Med. 2020;8:807–815. doi: 10.1016/S2213-2600(20)30225-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moore JB, June CH. Cytokine release syndrome in severe COVID-19. Science. 2020;368:473–474. doi: 10.1126/science.abb8925. [DOI] [PubMed] [Google Scholar]
- 28.Pierrakos C, Karanikolas M, Scolletta S, Karamouzos V, Velissaris D. Acute respiratory distress syndrome: Pathophysiology and therapeutic options. J. Clin. Med. Res. 2012;4:7–16. doi: 10.4021/jocmr761w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wu C, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern. Med. 2020;180:934–943. doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nieminen J, St-Pierre C, Sato S. Galectin-3 interacts with naive and primed neutrophils, inducing innate immune responses. J. Leukoc. Biol. 2005;78:1127–1135. doi: 10.1189/jlb.1204702. [DOI] [PubMed] [Google Scholar]
- 31.Mishra BB, et al. Galectin-3 functions as an alarmin: Pathogenic role for sepsis development in murine respiratory tularemia. PLoS ONE. 2013;8:e59616. doi: 10.1371/journal.pone.0059616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bonnesen B, et al. Early improvements in pulmonary function after severe COVID-19 requiring mechanical ventilation. Infect. Dis. (Lond.) 2020 doi: 10.1080/23744235.2020.1857432. [DOI] [PubMed] [Google Scholar]
- 33.Cabrera-Benitez NE, et al. Mechanical ventilation-associated lung fibrosis in acute respiratory distress syndrome: A significant contributor to poor outcome. Anesthesiology. 2014;121:189–198. doi: 10.1097/ALN.0000000000000264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hirani N, et al. Target-inhibition of galectin-3 by inhaled TD139 in patients with idiopathic pulmonary fibrosis. Eur. Respir. J. 2020 doi: 10.1183/13993003.02559-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Caniglia JL, Asuthkar S, Tsung AJ, Guda MR, Velpula KK. Immunopathology of galectin-3: An increasingly promising target in COVID-19. F1000Res. 2020;9:1078. doi: 10.12688/f1000research.25979.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Aminpour M, et al. Computational study of potential galectin-3 inhibitors in the treatment of COVID-19. Biomedicines. 2021 doi: 10.3390/biomedicines9091208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Luo X, et al. Prognostic value of C-reactive protein in patients with COVID-19. Clin. Infect. Dis. 2020 doi: 10.1093/cid/ciaa641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang L. C-reactive protein levels in the early stage of COVID-19. Med. Mal. Infect. 2020;50:332–334. doi: 10.1016/j.medmal.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tanaka T, Narazaki M, Kishimoto T. IL-6 in inflammation, immunity, and disease. Cold Spring Harb. Perspect. Biol. 2014;6:a016295. doi: 10.1101/cshperspect.a016295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Huang W, et al. Decreased serum albumin level indicates poor prognosis of COVID-19 patients: Hepatic injury analysis from 2,623 hospitalized cases. Sci. China Life Sci. 2020;63:1678–1687. doi: 10.1007/s11427-020-1733-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nicholson JP, Wolmarans MR, Park GR. The role of albumin in critical illness. Br. J. Anaesth. 2000;85:599–610. doi: 10.1093/bja/85.4.599. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request. All data generated during this study are included in this published article.