Abstract
Objective:
The purpose of the current study was to use network analysis techniques to parse relations between attention-deficit/hyperactivity disorder’s (ADHD) symptom domains, domains of executive function, and temperament traits.
Method:
Participants were 420 children aged 6–17 years (55% boys). The majority of participants were Caucasian (72.86%) and 50% of the sample met diagnostic criteria for ADHD. Both parents and teachers provided ratings of participants’ ADHD symptom severity. Parents completed questionnaires pertaining to participants’ temperament traits, and participants completed well-validated laboratory measures of executive function.
Results:
Results suggested effortful control as demonstrating the strongest relations with ADHD, particularly the parent-reported inattentive symptom domain. Additionally, negative affect appeared to demonstrate weaker but still notable relations primarily with the parent-reported hyperactive/impulsive symptom domain. Measures of executive function did not appear to demonstrate relations with any measures of ADHD symptoms or temperament traits. Results were generally replicated in a distinct sample (n = 732, 7–13 years, 63% boys, 81% White), although differences emerged pertaining to the role of surgency (i.e., related to the hyperactive/impulsive symptom domain in the replication but not primary sample).
Conclusions:
Overall, findings provided support for the primary role of effortful control, as well as secondary roles for negative affect and surgency, as key risk markers for the characterization of ADHD. Additional exploration of the overlap between temperament and executive function, as pertaining to ADHD, may help clarify heterogeneity in phenotypes and suggest priorities for targeted interventions outside of traditional symptoms.
Keywords: ADHD, temperament, executive function, risk markers, network analysis
Attention-deficit/hyperactivity disorder (ADHD) is a neurodevelopmental disorder that affects about 5% of children (American Psychiatric Association, 2013; Polanczyk, de Lima, Horta, Biederman, & Rohde, 2007) and contributes to functional impairment in academic, social/relational, physical health, and work domains (Barkley, 2015; Pelham, Foster, & Robb, 2007). Past studies have highlighted ADHD as a disorder characterized by significant heterogeneity, with diagnoses typically determined by a clinician based on the number, severity, and duration of inattentive and hyperactive/impulsive symptoms observed by parents/caregivers and teachers (Luo, Weibman, Halperin, & Li, 2019). Although this diagnostic classification system has been well-supported (Willcutt et al., 2012), the reliance on symptoms for characterizing those with ADHD is subject to serious limitations, including unclear relations between symptoms and neurobiological or psychological mechanisms involving emotion regulation and cognition. This issue may also have contributed to a lack of effectiveness in ADHD-related interventions potentially as a result of target misspecification, as studies have suggested low correspondence between reductions in ADHD symptoms and reductions in impairment (Karpenko, Owens, Evangelista, & Dodds, 2009; O’Connor, Garner, Peugh, Simon, & Epstein, 2015; Owens, Johannes, & Karpenko, 2009). Given these limitations, a targeted focus on empirically supported risk markers that indicate vulnerability for ADHD symptom domains may be critical for highlighting those most indicative of ADHD, while also linking these key risk markers with the disorder in a clearer and more integrated manner.
Temperament and Executive Function as Risk Markers
One such risk marker is executive function (i.e., a set of processes that enable engagement in goal-directed behavior, such as working memory, planning, inhibition, and cognitive flexibility; Lezak, Howieson, Bigler, & Tranel, 2012; Miyake & Friedman, 2012). Well-established theories have linked ADHD, particularly inattentive symptoms, to deficits in executive function (Coghill, Seth, & Matthews, 2014). Additionally, recent findings have suggested heterogeneity in executive dysfunction phenotypes in children with ADHD, particularly as pertaining to inhibitory control, working memory, and set shifting domains (Kofler, Irwin, Soto, Groves, Harmon, & Sarver, 2019), with an accounting of this heterogeneity needed to fully understand the nature of executive dysfunction in children with ADHD.
A second risk marker that has shown promise for helping to characterize the nature of ADHD is temperament (i.e., individual differences in reactivity and self-regulation; Rothbart & Bates, 2006). Importantly, despite conceptual overlap between ADHD and temperament, prior empirical work examining associations between these constructs has suggested that temperament may be best conceptualized as playing an etiological role in the development of ADHD symptoms (i.e., vulnerability hypothesis), rather than being a part of the disorder (i.e., continuum hypothesis; Gagne & Goldsmith, 2011; Martel et al., 2009; Wichstrøm, Penelo, Viddal, de la Osa, & Ezpeleta, 2018). Although various temperament taxonomies have been proposed, three higher-order traits have consistently been identified and are thought to be moderately stable across childhood and adolescence (see Kopala-Sibley, Olino, Durbin, Dyson, & Klein, 2018). Effortful control connotes the ability to suppress a prepotent response and purposefully resist interference, or suppress a dominant response in favor of a goal, and it has been frequently linked to the inattentive symptom domain in particular (Martel, 2009; Nigg, 2017). Negative affect connotes a predisposition to frequently experience negative emotions like sadness, anhedonia, and anger, of possible relevance to emotional dysregulation that has been associated with the hyperactive/impulsive symptom domain in those with ADHD (Forbes et al., 2017). Surgency is characterized by high activity level, high-intensity pleasure seeking, low shyness, and impulsivity; it is associated with positive affect and has been suggested to connote positive associations with ADHD (Martel, 2009).
A Need for Simultaneous Examination of Relations Among Risk Markers and ADHD
It should be noted that executive function and temperament traits, particularly effortful control, show conceptual overlap and similar neurobiological underpinnings, with some work suggesting that these two constructs may be best integrated into a single theory of self-regulation (Whittle, Allen, Lubman, & Yucel, 2006; Zhou, Chen, & Main, 2012). Yet, other studies have supported the continued differentiation of temperament and executive function by identifying weaker correlations between the two constructs, with one idea being that effortful control may be narrower in scope and more relevant for emotion regulation compared to executive function (Eisenberg, 2017). Further, working memory has been recognized as a key component of executive function, but less so effortful control, with a recently proposed developmental sequence being that high emotionality may disrupt the development of effortful control which, in turn, subsequently contributes to weakened executive functioning (Nigg, Sibley, Thapar, & Karalunas, 2020).
Given this ambiguity regarding the interplay/overlap of executive function and temperament traits, additional work examining these risk markers’ unique relations with ADHD is needed. This work may be particularly important in childhood and adolescence, given past work suggesting these periods as corresponding with peak risk for hyperactive/impulsive and inattentive symptoms, respectively (Cherkasova, Sulla, Dalena, Ponde, & Hechtman, 2013). Some limited prior work examining temperament and executive function simultaneously has identified relations between these risk markers and inattentive or both ADHD symptom domains (Martel, 2016). Additionally, other studies have identified working memory, cognitive inhibition, effortful control, and surgency-related constructs (e.g., positive emotionality) as uniquely related to both inattention and hyperactive/impulsive symptoms (Brocki, Forslund, Frick, & Bohlin, 2019; Forslund, Brocki, Bohlin, Granqvist, & Eninger, 2016; Frick & Brocki, 2019; Krieger, Amador-Campos, & Gallardo-Pujol, 2019; Sjowall, Bohlin, Rydell, & Thorell, 2017). Yet, almost all studies in this area have been conducted using small-to-moderately sized samples (ns ≤ 184). Only one study, to our knowledge, has been conducted examining trait-executive function overlap in a relatively large and well-characterized sample of children with ADHD, with results suggesting executive function accounted for some unique heterogeneity in primarily trait-based subgroups (Goh, Lee, Martel, Karalunas, & Nigg, 2020). Hence, additional research is needed to identify temperament trait and executive function domains most uniquely related to and hence most likely to represent key risk markers that best indicate vulnerability for certain ADHD symptom profiles (e.g., effortful control and executive function uniquely related to inattentive symptoms; negative affect and surgency related to hyperactive/impulsive symptoms). Such research could be important for conceptualizing the overlap between temperament and executive function, as well as clarifying their unique roles as risk markers for ADHD.
Network Analysis
Network analysis represents a novel technique that can accommodate of simultaneous examination of risk markers’ unique relations with ADHD symptom domains. This set of techniques is based on a “network theory” of psychopathology, which conceptualizes elements of disorders (i.e., symptoms, symptom domains) and their risk markers as demonstrating direct and potentially reciprocal relations with one another (Borsboom & Cramer, 2013). As a complement to structural equation modeling techniques, network analysis readily accommodates the differentiation of relations among elements; in structural equation modeling, these relations would be conflated within latent constructs (i.e., differential relations among various executive function domains, both with each other and ADHD symptom domains, being conflated within a single relationship between one executive function composite and one ADHD composite). Further, through the use of regularized partial correlations, network analysis provides a means to highlight the strongest unique relations between disorders and their risk markers. Such an analysis would be somewhat analogous to numerous multiple regression analyses conducted at once, with the accessible depiction of resulting networks and the use of regularization techniques to reduce risk for false positives differentiating it from other multivariate methodologies. Although the vast majority of network analytic work has investigated relations solely among symptoms of disorders, network analysis has also shown potential for clarifying relationships among risk markers of disorders and highlighting those that may be particularly important in disorders’ development (Elliott, Jones, & Schmidt, 2019; Olatunji, Levinson, & Calebs, 2018).
There are at least two primary ways that network analysis may facilitate novel insights into the differential relations between risk markers and ADHD symptom domains. First, network analysis could help parse associations among ADHD and its risk markers simultaneously, providing a means to explore risk markers’ unique relations with ADHD symptom domains. This may be particularly useful in the context of past studies described above suggesting aspects of temperament and cognition may be related and potentially exhibit overlapping relations with ADHD symptom domains. The identification of the strongest relations between risk markers and ADHD may be a crucial step in identifying key vulnerabilities that may serve as the best early indicators of ADHD symptoms (e.g., deficits in effortful control), as well as exploring the interplay among traits and executive function in the context of ADHD. For instance, while accounting for direct relations between ADHD and its risk markers, network analysis could also accommodate a preliminary and theory-driven examination of indirect effects of risk markers on ADHD, as has been proposed in prior work (Krieger et al., 2019; Nigg et al., 2020). Second, the use of network analysis could accommodate an identification of relevant “bridge risk markers” that demonstrate the strongest unique relations with ADHD symptom domains while accounting for overlap among other elements in a network. Such work may be important for identifying key risk markers that demonstrate the strongest unique relations with ADHD symptom domains overall, facilitate insights into early vulnerability for ADHD, and have the most potential for linking ADHD symptoms with psychological and neurobiological mechanisms.
The Current Study
The current study was the first to utilize network analysis to examine ADHD symptom domains’ relations with measures of executive functioning and temperament traits through two primary aims. First, networks were created including parent- and teacher-reported ADHD symptom domains, temperament traits, and executive function measures in a sample including participants with and without ADHD (i.e., primary sample). It was hypothesized that a relation would emerge between effortful control and the inattentive symptom domain, with surgency and temperament being more related to the hyperactive/impulsive symptom domain. Additionally, it was hypothesized that executive function domains would be more closely related to inattentive, rather than hyperactive/impulsive, symptoms. Next, we conducted a sensitivity analysis of results using a distinct and more recently collected sample of similarly aged youth (i.e., replication sample). Replicability and generalizability remain key issues for complex models involving network analysis (Borsboom et al., 2017; Forbes, Wright, Markon, & Krueger, 2019). Several studies have provided support for the robustness of network structure (Fried et al., 2018; Goh, Lee, Martel, Derefinko, & Lynam, 2020), yet most of this work has been conducted across networks only including symptoms. Hence, there remains a need for additional testing of networks’ replicability, particularly in those including disorders and their risk markers. Thus, we sought to contribute to this work by looking for reproducibility in a distinct sample. It was hypothesized that network structure would be generally robust across samples.
Methods
Participants
Primary sample.
Demographic information is available in Table 1. In both samples, all parents and children completed informed consent and assent in conformity with local IRB, NIH, and APA ethical guidelines and the 1964 Helsinki declaration. Participants in the primary sample were 420 children (231 boys) between the ages of six and 17 years (M = 10.75, SD = 2.35), with this age range being chosen given that most ADHD diagnoses occur during school age and continue to cause impairment into adolescence (Cherkasova et al., 2013). Participants were recruited from a metropolitan area in the Upper Midwest region of the United States, with efforts being made to obtain the broadest sample that, except for ADHD prevalence, was representative of the region (and to avoid potential biases inherent in a purely clinic-referred sample). The majority of participants were White (72.86%). About 50% of the sample met diagnostic criteria for ADHD, with ADHD sum scores ranging from 0 to 54 (M = 16.70, SD = 13.51). Among the parent raters, 97% identified themselves as the participant’s mother. Informant information was not available on teachers.
Table 1.
Sample Demographic Information
| Primary Sample | Replication Sample | |
|---|---|---|
|
| ||
| N | 420 | 732 |
| Gender [n (%) Female] | 191 (45.00) | 273 (37.30) |
| Age [M(SD)] | 10.75 (2.35) | 9.74 (1.56) |
| Race [n (%) white] | 306 (72.86) | 627 (85.66) |
| ADHD Diagnosis [n (%) Positive] | 210 (50.00) | 440 (60.11) |
| FSIQ | 104.49 (14.64) | 111.12 (13.54) |
| Family Income [n (%)] a 0 – 50,000 50,001 – 100,000 100,001 – 150,000 > 150,001 |
114 (27.14) 156 (37.14) 39 (9.29) 13 (3.10) |
161 (21.99) 305 (41.67) 150 (20.49) 65 (8.88) |
Note.
Family income was measured as a continuous variable in the primary sample and as a categorical variable (with categories corresponding to those listed in the Table) in the replication sample. We report categorical results across samples for consistency. 98 participants in the primary sample and 51 participants in the replication did not report family income.
Replication sample.
Data from the replication sample was obtained following the primary sample, with participant recruitment and assessment being generally consistent with the primary sample. This sample was recruited from within the geographic radius of 50 miles from a Northwest University in the United States. The final sample included 732 children (459 boys; aged 7–13 years, M = 9.74, SD = 11.56). In this sample, 81.1% participants identified as White. About 60% of the sample met diagnostic criteria for ADHD. Among the parent raters, 79% were women in the primary caregiving role, and most were biological mothers who chose to participate due to availability. Informant demographic information was not available on teachers.
Recruitment and identification.
A broad community-based recruitment strategy was used, with mass mailings to parents in local school districts, public advertisements, and fliers at local clinics. Families were initially recruited and then passed through a standard multi-gate screening process to establish diagnostic status. At Stage 1, all families were screened by phone to rule out youth prescribed long-acting psychotropic medication (e.g., antidepressants), neurological impairments, seizure history, head injury with loss of consciousness, other major medical conditions, or a prior diagnosis of intellectual disability or autism.
At Stage 2, parents and teachers of remaining eligible youth completed the following standardized rating scales: Child Behavior Checklist/Teacher Report Form (CBCL/TRF; Achenbach, 1999), Conners Rating Scales-Revised, (Conners, 1997), and the ADHD Rating Scale (ADHD-RS; DuPaul et al., 1998). In addition, parents completed a structured clinical interview to ascertain symptom presence, duration, and impairment. Parents and teachers were instructed to rate children’s behavior while off medication. At this visit, a four-subtest short form of the WISC-IV (Wechsler, 2003) was administered; estimated full scale IQ over 75 was required for inclusion. All parents and youth that met criteria attended a second laboratory visit a few weeks later during which parents completed temperament ratings and children completed neuropsychological testing. All materials were scored and presented to a clinical diagnostic team comprising a board-certified child psychiatrist and a licensed child neuropsychologist. Implementing a best estimate procedure (Kosten & Rounsaville, 1992), each clinician independently assigned diagnoses, masked to one another’s ratings and to subsequent cognitive or temperament ratings. Disagreements were conferenced to consensus or excluded. Participants and informants were paid for participation.
Measures
ADHD symptoms.
Parent and teacher report on ADHD symptoms was obtained using the ADHD-RS (DuPaul et al., 1998), a common method used by researchers and clinicians. Each ADHD symptom was rated using a four-point scale ranging from 0 (“never, or rarely”) to 3 (“very often”) (detailed response options are available in the Supplemental Material). Each informant provided ratings for all of the 18 DSM–IV symptoms (i.e., nine inattentive and nine hyperactive/impulsive symptoms; data was collected before the creation of DSM-5). Item responses were then aggregated into inattentive and hyperactive/impulsive sum scores, with a two-symptom domain model being chosen to be consistent with DSM-IV and DSM-5, as well as current clinical practices. Analyses were conducted including parent- and teacher-reported inattentive and hyperactive/impulsive symptom domains as separate sum scores (αs > .80).
Executive function.
All children completed a neuropsychological testing battery after a minimum washout period of 24 hours for short-acting medications and 48 hours for long-acting medications (washout range 24–152 hours, M = 58 hours). The testing battery included tasks that produce scores chosen to assess a variety of neuropsychological domains deemed especially relevant to children and adolescents with ADHD (Nigg et al., 2018). Detailed information regarding the neuropsychological battery and its factor analysis is available elsewhere (Nikolas & Nigg, 2013). Tests were administered in a fixed order as follows:
Memory span and working memory: digit span.
Youth completed the WISC-IV Digit Span task to assess verbal span (forward) and working memory (backward) (Wechsler, 2003), with these scores being combined into a total standard score. Higher standardized score composites indicated better average performance across both.
Response suppression/inhibition: stop task.
The stop task was administered to assess response inhibition (Logan, 1994); it requires the suppression of a prepotent motor response. Higher Stop Signal Reaction Time (SSRT) scores indicated worse performance. For the current study, SSRT was calculated using a “mean” method. It should be noted that a recent consensus guide suggested an “integration method” (i.e., replacing go omissions with the maximum RT in order to compensate for the lacking response), rather than the mean value, as a more reliable method for measuring SSRT (Verbruggen et al., 2019). However, the correlation between SSRT using the “mean” method and the integration method is usually high. Thus, to be consistent with prior work in ADHD (Goh et al., 2020; Karalunas, Gustafsson, Fair, Musser, & Nigg, 2019; Nigg et al., 2018), the “mean” method was used in the current study.
Processing speed and set shifting: trail making test.
Participants completed the Trail Making Test parts A (connecting numbers in sequential order) and B (connecting numbers and letters in alternative sequential order) as an assessment of processing speed and set shifting abilities, respectively (Lezak, Howieson, Loring, Hannay, & Fischer, 2004). Higher scores indicated a longer time to complete the tasks and hence, worse performance. In the replication sample, participants completed the Trail Making Test from the Delis-Kaplan Executive Function System (DKEFS; Delis et al., 2001), with the times to complete the Number Sequencing and Number-Letter Switching conditions (i.e., conditions 2 and 4) included in networks. These tasks directly correspond to Trails A and Trails B from the older task.
Temperament traits.
Parents in the primary sample completed the short form version of the Early Adolescent Temperament Questionnaire-Revised (EATQ-R; Ellis & Rothbart, 2011). The EATQ-R consists of 62 item-statements describing child temperament characteristics. Instructions consist of asking the parent to rate how well the statements describe their child on a scale from 1 (“almost always untrue of the child”) to 5 (“almost always true of the child”), with responses being combined to form activation control, affiliation, attention, fear, frustration, high intensity pleasure/surgency, inhibitory control, shyness, aggression, and depressed mood. Scores on these scales were, in turn, averaged into effortful control (EATQ-R: Attention, Inhibitory Control, Activation Control; TMCQ: Attention, Inhibitory Control, Low Intensity Pleasure, Perceptual Sensitivity, and Activation Control), negative affect (EATQ-R: Frustration, Depressive Mood, Aggression; TMCQ: Anger/Frustration, Discomfort, Fear, Sadness, Soothability), and surgency (EATQ-R: High Intensity Pleasure, Fear, Shyness; TMCQ: Activity Level, High Intensity Pleasure, Impulsivity, Shyness) (response options are available in the Supplemental Material). Higher scores on negative affect and surgency, along with lower scores on effortful control, indicated greater impairment. In the replication sample, parents completed the Temperament in Middle Childhood Questionnaire (TMCQ; Simonds & Rothbart, 2004), which is a 157-item analogous measure similar in administration and conceptual interpretation to the EATQ-R. In both samples, all scales demonstrated adequate internal consistency (Cronbach αs ≥ .8). Scores on the TMCQ and EATQ-R have been shown to be related to ADHD severity, with recent studies also linking traits to symptom trajectories as well (Forbes et al., 2017; Karalunas et al., 2019; Martel & Nigg, 2006; Lawson, Atherton, & Robins, 2021).
Statistical Analyses
Network construction and interpretation.
Given that data consisted of ordinal and non-normal variables, we estimated Mixed Graphical Models (MGMs) using the R package bootnet, with the qgraph package being used for network visualization (Epskamp, Cramer, Waldorp, Schmittmann, & Borsboom, 2012; Epskamp & Fried, 2018; Haslbeck & Waldorp, 2015). All networks were estimated using the least absolute shrinkage and selection operator (LASSO; Tibshirani, 1996) in combination with extended Bayesian Information Criterion (EBIC) model selection (Foygel & Drton, 2010), resulting in sparse networks containing only the strongest partial correlations (gamma hyperparameter was set to 0.5).1 Within network visualizations, elements were positioned based on Fruchterman and Reingold’s (1991) algorithm, such that strongly connected elements were depicted as closer together and elements in the center of the network demonstrated the strongest connections to other elements. Three networks were created: the first included parent- and teacher-reported ADHD symptom domains, temperament traits, and executive function, the second only included parent-reported ADHD symptom domains, and the third only included teacher-reported ADHD symptom domains. The second and third networks were created to account for and explore potential effects of relations between parent- and teacher-reported ADHD symptom domains on network structure, as well as examine structural differences in the network based on reporter.
Identifying bridge elements.
Bridge strength, or the absolute sum of the edge weights attached to an element from elements of another community (i.e., ADHD versus risk markers), was used to determine risk markers most related to ADHD symptom domains (Jones, Ma, & McNally, 2019). Higher values suggested greater potential relevance with respect to ADHD symptom domain scores. To determine bridge risk markers, we conducted bootstrapped difference tests statistically comparing the bridge strength of all variables within networks. Detailed information regarding these tests is available in the Supplemental Material.
Results2,3,4
Missing Data
The primary sample originally consisted of 498 participants, but data for 78 were listwise deleted because of missing data (network analysis requires complete data). Chi square and ANOVA tests suggested no differences between participants with and without missing data as pertaining to age (p = .77), gender (p = .98), race/ethnicity (p = .85), parent- and teacher-reported ADHD sum scores (ps ≥ .68), effortful control (p = .57), negative affect (p = .40), surgency (p = .48), digit span (p = .42), and Trail-Making B (p = .54) scores. Those with complete data had significantly higher stop signal and Trail-Making A scores, although the effect sizes of these scores were negligible (ps ≤ .02; partial η2s = .02). In the replication sample, data for 117 (out of 849) participants were deleted. Participants with complete data were significantly older than those with missing data (p < .001, partial η2 = .02). Those with missing data had significantly higher negative affect (p = .047, partial η2 = .01), digit span (p = .03, partial η2 = .01), and Trail Making scores (ps < .001, partial η2s ≤ .02). However, effect sizes of these differences were small. No other differences were identified (ps > .05).
Network Interpretation
See Supplemental Material for detailed description of tests assessing network reliability and accuracy, regularized correlation matrices, and tests statistically comparing the bridge strength of elements in networks. With respect to the primary sample, resulting networks are depicted in Figure 1, with the bridge strength of elements within networks shown in Figure 2. Preliminary tests suggested significant differences in primary and replication samples based on overlapping ADHD-RS, temperament trait, and executive function scores (ps ≤ .08, partial η2s ≤ .06). However, effect sizes of these differences were small and likely not meaningful.
Figure 1.
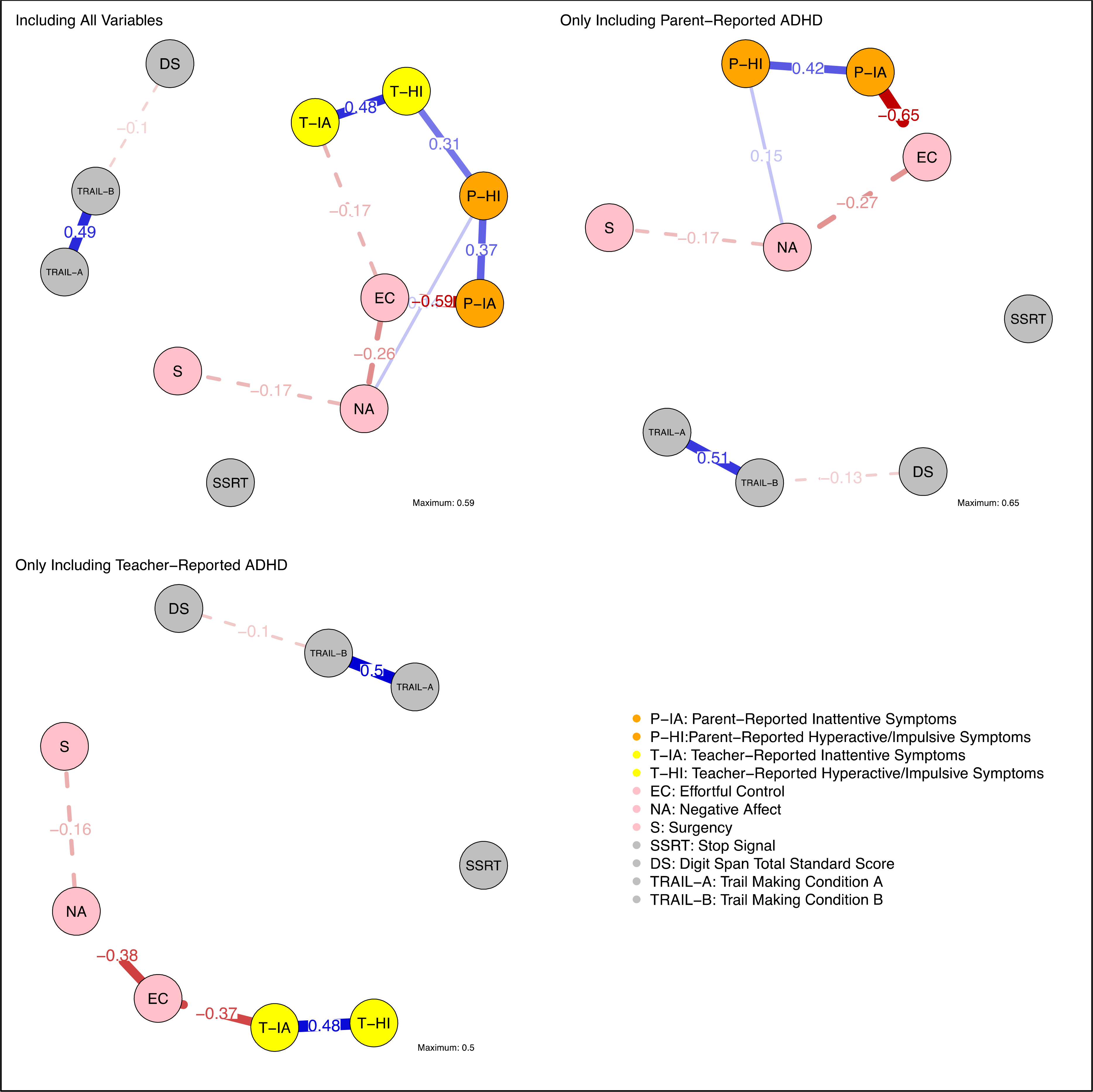
Primary Sample Networks Depicting Regularized Partial Correlations Among Parent-Reported ADHD Symptoms, Teacher-Reported ADHD Symptoms, Executive Function Domains, and Temperament Traits
Note. Solid lines indicate positive correlations and broken lines indicate negative correlations. Line thickness indicates the strength of the relation. Listed edge weights correspond with regularized partial correlations.
Figure 2.
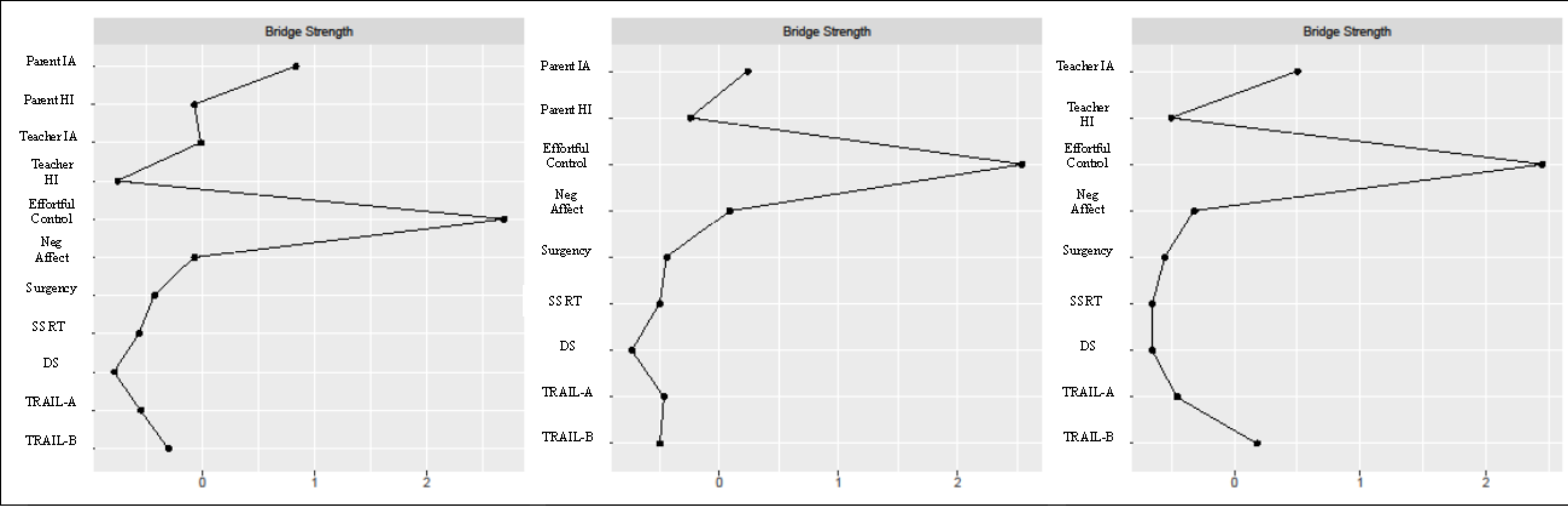
Bridge Strength Values for Variables in (from left to right) Complete Networks, Networks Including Only Parent-Reported ADHD Symptoms, and Networks Only Including Teacher-Reported ADHD Symptoms in the Primary Sample
Note. Nodes are listed on the y-axis, with bridge strength values listed on the x-axis. Values farther to the right indicate greater bridge centrality. IA = Inattentive Symptom Domain, HI = Hyperactive/Impulsive Symptom Domain, SSRT = stop signal reaction time, DS = digit span, TRAIL-A = trail making test condition A, TRAIL-B = trail making test condition B.
Examination of the network including both parent- and teacher-reported ADHD symptom domains, temperament traits, and executive function measures suggested effortful control was related to both parent- and teacher-rated inattentive symptom domain scores (regularized |rs| ≥ .17). Negative affect was positively related to the parent-reported hyperactive/impulsive symptom domain (regularized r = .14), as well as negatively related to effortful control (regularized r = −.26) and surgency (regularized r = −.17). Parent- and teacher-reported ADHD symptom domains did not exhibit relations with any measures of executive function. Assessment of bridge strength suggested effortful control as a bridge risk marker that demonstrated the strongest overall relationship with ADHD, primarily the parent-reported inattentive symptom domain. In sum, effortful control emerged as a bridge risk marker primarily via its relation with the parent-reported inattentive symptom domain. Negative affect also appeared to demonstrate a relation with the parent-reported hyperactive/impulsive symptom domain and other temperament traits. No relations emerged involving executive function domains.
Networks Including Just Parent- or Teacher-reported ADHD Symptoms
When networks were rerun using just parent- or just teacher-rated ADHD symptoms as a follow-up test assessing the effect of redundancy between parent- and teacher-report, the prominent role of the inattentive symptom domain was highlighted. That is, in networks only including parent-reported ADHD, the inattentive symptom domain was related to effortful control (regularized |r| = .63), and the hyperactive/impulsive symptom domain was related to negative affect (regularized r = .15). In networks including teacher-reported ADHD, effortful control was related to the inattentive symptom domain (regularized |r| = .37). Effortful control still emerged as the most clinically relevant bridge marker, overall, via its relation with the inattentive symptom domain, regardless of reporter.
Replication Sample Network Interpretation
Results suggested a notable relation between effortful control and the parent-reported inattentive symptom domain (regularized |r| = .47). All temperament traits, particularly negative affect (regularized r = .31) and surgency (regularized r = .42), were related to the parent-reported hyperactive/impulsive symptom domain. Surgency was related to the teacher-reported hyperactive/impulsive symptom domain (regularized r = .11), but no traits were related to teacher-reported inattentive symptom domain. No measures of executive function were uniquely related to any ADHD symptom domains or temperament traits. Assessment of bridge strength suggested effortful control as demonstrating the strongest relations with ADHD symptom domains in general, particularly the parent-reported inattentive symptom domain. Both negative affect and surgency emerged as secondary bridge risk markers. Results pertaining to trait-disorder relations generally persisted even when only one reporter of ADHD was included in networks, although a relation emerged between digit span and inattentive symptoms when only teacher-reported ADHD was included in networks. In sum, the etiological network in the replication sample broadly suggested consistent results compared to the primary sample, although some differences emerged pertaining to the relation between teacher-reported inattention and effortful control as well as the relevance of surgency as a bridge risk marker.
Supplemental Analysis: Comparison of Network Structure Across Age Ranges
As a post-hoc supplemental analysis, we examined whether network structure differed between older and younger participants in both primary and replication samples, given prior work suggesting developmental changes in ADHD symptom domains’ prominence and the structure of executive function across childhood and adolescence (Cherkasova et al., 2013; Zelazo & Carlson, 2012). Participants were separated based on a mean split to ensure statistical power (i.e., 11 years in the primary sample, we also used this cut-off in the replication sample for consistency), with network comparison tests being conducted as described above. Omnibus tests comparing network structure (i.e., the maximum difference in any of the corresponding edge weights in younger versus older subsample networks) suggested no significant differences (ps ≥ .41), with corresponding relations among variables being highly correlated (rs ≥ .95). Overall, results suggested no differences in network structure between the two age groups.
Discussion
Using network analysis techniques in two distinct samples, the current study investigated unique relations among parent- and teacher-reported ADHD symptom domains and measures of executive function and temperament traits. In line with hypotheses, results suggested effortful control as the risk marker that demonstrated the strongest relations with parent- and teacher-reported inattentive symptom domain scores. Additionally, negative affect appeared to demonstrate a weaker relation with the parent-reported hyperactive/impulsive symptom domain. Conversely, and in contrast to hypotheses, executive function measures appeared to demonstrate little to no relations with ADHD symptom domains. Results were largely replicated in a distinct sample, although some differences emerged pertaining to the role of surgency and teacher-reported inattention. Supplemental tests suggested findings did not appear to change between older and younger age ranges. Lastly, results also persisted when accounting for overlap between ADHD and effortful control, were consistent regardless of ADHD diagnosis, and generally replicated when including more distal risk markers of ADHD that were collected as part of the larger study (i.e., genetics and marital conflict; See Footnotes 2–4).
Effortful Control and (secondarily) Negative Affect as Risk Markers for ADHD
Results suggested effortful control, overall, as the risk marker most related to ADHD symptom domains, particularly inattentive, even when only including one reporter (i.e., parent or teacher) of ADHD. Findings were consistent with prior work conceptualizing ADHD as a disorder largely characterized by deficits in effortful control (Atherton, Lawson, Ferrer, & Robins, 2020; Frick & Brocki, 2019; Martel & Nigg, 2006), and suggested early screening of effortful control may facilitate the most insight into vulnerability for ADHD symptoms, particularly inattentive. Additionally, negative affect appeared to demonstrate relations primarily with the parent-reported hyperactive/impulsive symptom domain, although these relations were not as strong as those involving effortful control. These findings were consistent with prior work suggesting an affective component to the hyperactive/impulsive symptom domain (vs. inattentive; Martel, 2009), and provided additional support for temperament-based multiple-pathway models of ADHD (Martel & Nigg, 2006). That is, low levels of top-down control and high levels of reactivity may potentially contribute to inattentive and hyperactive/impulsive symptom domains, respectively, with effortful control (primarily) and negative affect (secondarily) being particular areas of focus to explore these effects.
It should also be noted that given the interconnectivity of parent- and teacher-reported ADHD symptom domains and temperament traits, it is likely that all traits and ADHD symptom domains were related in some manner. However, through the use of partial correlations and regularization, network analysis facilitated a highlighting of the strongest relations among these constructs. More concretely, effortful control and, secondarily, negative affect may be particularly key for indicating risk for inattentive and hyperactive/impulsive symptom domains, respectively, with trait-disorder relations involving surgency being better conceptualized as tertiary compared to the other traits. Such findings are in line with studies suggesting many children with ADHD experience difficulties with negative affect or negative emotional reactivity (Goh et al., 2020; Karalunas et al., 2019). Additionally, a relation emerging between negative affect and effortful control is consistent with the idea that high levels of negative affect may be associated with disruptions in the consolidation of effortful control, which, in turn, contribute to deficits in self-regulation in those with ADHD (Gagne & Goldsmith, 2011; Miller, Hane, Degnan, Fox, & Chronis-Tuscano, 2019; Nigg, 2017; Nigg et al., 2020). Yet, given the cross-sectional nature of networks, such ideas remain speculative pending future longitudinal work.
Absent Relations Between Executive Function and ADHD Symptom Domains
Interestingly, measures of executive function did not appear to demonstrate unique relations with any measures of ADHD symptoms or temperament traits. These results, in part, may have been due to shared source variance between parent-reported ADHD symptoms and temperament (versus objective measures of executive function). However, they differed from prior work that used similar measures (i.e., questionnaire for traits and objective tasks for executive function) to suggest executive function and temperament as both demonstrating unique relations with ADHD (Frick & Brocki, 2019). It should be noted that in this past study, the relationship or contribution of executive function to the characterization of ADHD, while notable, was substantially weaker than that involving temperament traits. Hence, it is possible that weaker relations between executive function domains and ADHD symptom domains were eliminated in the current study due to regularization.
Overall, results suggested temperament traits as more strongly related to ADHD symptom domains than executive function, likely due in part to differences and similarities in reporting methodology. Additionally, given that temperament traits and executive function domains were only somewhat related in our samples (non-regularized bivariate |rs| ranged from .01-.23, with correlations involving effortful control, in general, being the strongest), results provided mixed support for the idea that these risk markers may conceptually overlap (Nigg, 2017; Whittle et al., 2006; Zhou et al., 2012). Further work is needed applying the network approach and other analogous approaches to parse relations among executive function domains, temperament, traits, and ADHD symptom domains, perhaps using different combinations of objective and subjective measures for both temperament traits and executive function, to confirm findings and provide a better understanding of core risk markers’ unique roles the development, characterization, and treatment of ADHD.
Generally Consistent Findings Across Two Distinct Samples
The attempted replication in a distinct sample suggested mostly similar findings, in that effortful control emerged as a primary bridge risk marker via a relation with the parent-reported inattentive symptom domain (although not with teacher-reported inattention, likely due to the use of partial correlations), whereas negative affect demonstrated a relation primarily with parent-reported hyperactive/impulsive symptom domain scores. Additionally, measures of executive function appeared disconnected from ADHD symptom domains and temperament traits. Such findings appeared to provide support for the replicability of the network approach, in general, for conceptualizing relations among disorders and their risk markers.
However, some differences also emerged pertaining to the role of surgency in particular, as this trait emerged as a bridge risk marker via relations with the parent-, and secondarily, teacher-reported hyperactive/impulsive symptom domain in replication analyses. Further exploration of this finding suggested it was not necessarily driven by instability in the network approach, but instead by differences in the way that surgency was defined in the TMCQ versus the EATQ-R. That is, only one subscale involved in the calculation of surgency (out of three on the EATQ-R and four on the TMCQ) was found to be overlapping. Conversely, higher numbers of overlapping subscales were utilized in the calculation of effortful control and negative affect across samples, which may explain why their roles in the etiological network remained relatively consistent between primary and replication samples. Past work using different measures of surgency to examine its relation with ADHD has suggested mixed results (see Krieger et al., 2019), and results of the current study provided additional support for the idea that surgency’s convergent validity may be reliant on how it is defined and measured. Given these findings, clarification of surgency scores’ validity across different measures may be needed to clarify their utility with respect to ADHD-related risk markers and outcomes.
Clinical Implications
Results of the current study suggested that early assessment of temperament traits, particularly effortful control, may provide key insights into risk for specific ADHD phenotypes, as well as link these phenotypes more clearly with neurobiological and psychological mechanisms to facilitate further targeted screening and guide early interventions (Whittle et al., 2006). On the other hand, information gleaned from measures of executive function may be somewhat redundant with that pertaining to traits, with the nature of this overlap changing based on the methodology used to measure these constructs. Pertaining to treatment more specifically, findings suggested that in clinical settings, interventions aimed at effortful control (e.g., enhancing self-regulation) may provide benefits primarily to inattentive symptoms, whereas those aimed at negative affect and surgency (e.g., increasing soothability) may help reduce the severity of hyperactive/impulsive symptoms. Conversely, though interventions aimed at improving executive function (e.g., goal setting, increasing flexibility) may provide additional avenues to reduce the severity of ADHD symptoms, benefits of these interventions may overlap with those aimed at temperament traits, particularly effortful control. Critically, additional work in this area may facilitate a personalized approach to temperament-based interventions, where the environment can be adjusted based on a child’s own strengths and weaknesses (e.g., adjusting caregiver management strategies). This approach is commonly used to address cognitive deficits in children with ADHD (e.g., school accommodations), with temperament potentially providing another avenue for consideration. Further work is needed to examine this idea and parse the unique utility of temperament- and executive function-based interventions to clarify their overlap and maximize effectiveness and efficiency in treatment.
Limitations and Future Directions
There were some limitations in the current study. Although the use of bridge centrality facilitated a valuable examination of relations between ADHD and its risk markers, further work is needed to examine the utility of central nodes for highlighting intervention targets. Additionally, supplemental tests suggested robustness in network structure between younger and older participants, but an in-depth examination of whether networks change in structure throughout development remains a crucial future direction. We were also unable to conduct any analyses pertaining to effect sizes or confidence intervals as these analyses have yet to be developed for network analysis. Symptom and temperament trait scales contained several items that used similar wording, which could have inflated correlation estimates. Yet, this issue is not unique to network models (i.e., CFA models may be biased due to this overlap as well), and follow-up analyses exploring this overlap suggested it did not majorly impact results. A minority of participants (~23%) fell outside the recommended age ranges for administration as pertaining to the EATQ-R (9–15 years) and TMCQ (7–10 years). These participants were still included to preserve statistical power, and recent work has provided some support for the validity of the EATQ-R in adolescence (Lawson et al., 2021). Yet, future studies should seek to validate results in samples falling in recommended age ranges or using appropriate measures (as well as current DSM-5 ADHD symptoms). Our samples were also relatively high functioning (average FSIQ: primary sample = 104.49; replication sample = 111.12), underrepresented groups identifying as minorities, and had a higher reported median household income ($64,000) compared to the U.S. 2010 Census (http://www.census.gov). Future studies should seek to replicate results using larger nationally representative samples to ensure generalizability of results. Relatedly, although the robustness of network structure across parent- and teacher-report was notable, future examination of more nuanced differences between reporters (i.e., reporter age, sex, race/ethnicity) is likely to be important. Supplemental analyses suggested results held when including externally-oriented variables in primary sample networks (i.e., marital conflict, genetics), yet further work is needed assessing other environmental risk factors (e.g., prenatal stress and low birth weight) to further explore the nature of ADHD. Lastly, recent work has suggested limited construct validity in some tasks measuring executive function (Snyder, Miyake, & Hankin, 2015). Additional research is thus needed to ensure the validity of these measures to ensure accurate conceptualization of ADHD-executive function relations.
Conclusion
Despite these limitations, the findings of the current study extend the literature by examining the unique associations between ADHD and its relevant risk markers via network analysis. Results suggested effortful control as a primary bridge risk marker via a strong relation with ADHD symptom domains, particularly the parent-reported inattentive symptom domain. Further, network results provided some additional support for temperament-focused multiple-pathway models of ADHD highlighting surgency and negative affect’s relations with the hyperactive/impulsive symptom domain. Conversely, domains of executive function appeared to demonstrate little to no relation with ADHD symptom domains after accounting for the effects of temperament traits, supporting the importance of accounting for risk markers’ overlap when conceptualizing the nature of ADHD. Ultimately, further exploration of these findings may facilitate nuanced insights into risk markers that contribute most to heterogeneity in ADHD and aide in refining assessment and intervention procedures.
Supplementary Material
Acknowledgments
The authors have no conflicts of interest to disclose. Support was provided by NIH R37-MH-59105–12 and R01-MH59105. The authors thank all participants for making this work possible. The data that support the findings of this study are available from the corresponding author upon reasonable request.
Footnotes
Partial correlations range from −1 to 1 and correspond with the remaining association between two elements within a network after controlling for all other relations among elements. This contrasts with bivariate correlations which do not account for these other relations. However, spurious or false positive relations are still possible in networks given the high number of parameters that are estimated. Hence, regularization techniques apply a “penalty” to the strength of all relations within a network, decreasing their strength and removing weaker edges. Together, these two techniques are thought to increase the likelihood of creating a network structure that minimizes the number of spurious relations while highlighting the strongest relations (see Epskamp & Fried, 2018).
To test for redundancy between variables, we utilized the Goldbricker function in the R package networktools (Jones, 2018). This package identified variable pairs that were correlated (r > .50) with each other and in highly similar patterns with other variables (less than 25% of overlapping correlations with other items being significantly different [p < .05]). Results suggested no cross-construct redundancy between traits, executive function domains, and ADHD symptom domains. As a secondary test, we replicated analyses removing the Attention scale from Effortful Control scores to reduce item overlap, and results were generally consistent with analyses presented in the manuscript. Detailed results related to these “non-overlapping” analyses are available in the Supplemental Material. Further, we replicated analyses after removing effortful control from analyses completely. Results suggested general consistency with those presented in the main body of the text, as no measures of executive function emerged as bridge risk markers. Detailed results of these analyses are available upon request to the corresponding author.
To test the validity of findings in clinical versus non-clinical samples, we compared network structure in those diagnosed with versus without ADHD. Results suggested robustness in network structure regardless of ADHD diagnosis (see Supplemental Material).
Lastly, we added two other variables to the primary sample’s networks that have been found to be relevant to the development of ADHD: behavioral genetics and martial conflict. Results were consistent with those presented in the manuscript, with genetic markers and marital conflict not appearing to exhibit meaningful relations with ADHD symptom domains. Detailed results are available in the Supplemental Material.
References
- Achenbach TM (1999). The Child Behavior Checklist and related instruments. In Maruish ME (Ed.), The use of psychological testing for treatment planning and outcomes assessment (pp. 429–466). Mahwah, NJ, US: Lawrence Erlbaum Associates Publishers. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington, VA: American Psychiatric Association. [Google Scholar]
- Atherton OE, Lawson KM, Ferrer E, & Robins RW (2020). The role of effortful control in the development of ADHD, ODD, and CD symptoms. Journal of Personality and Social Psychology, 118(6), 1226–1246. doi: 10.1037/pspp0000243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barkley RA (2015). Attention-deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.). New York, NY: The Guilford Press. [Google Scholar]
- Borsboom D, & Cramer AO (2013). Network analysis: an integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology, 9, 91–121. doi: 10.1146/annurev-clinpsy-050212-185608 [DOI] [PubMed] [Google Scholar]
- Borsboom D, Fried EI, Epskamp S, Waldorp LJ, van Borkulo CD, van der Maas HLJ, & Cramer AOJ (2017). False alarm? A comprehensive reanalysis of “Evidence that psychopathology symptom networks have limited replicability” by Forbes, Wright, Markon, and Krueger (2017). Journal of Abnormal Psychology, 126(7), 989–999. doi: 10.1037/abn0000306 [DOI] [PubMed] [Google Scholar]
- Brocki KC, Forslund T, Frick M, & Bohlin G (2019). Do individual differences in early affective and cognitive self-regulation predict developmental change in ADHD symptoms from preschool to adolescence? Journal of Attention Disorders, 23(13), 1656–1666. doi: 10.1177/1087054717693372 [DOI] [PubMed] [Google Scholar]
- Cherkasova M, Sulla EM, Dalena KL, Pondé MP, & Hechtman L (2013). Developmental course of attention deficit hyperactivity disorder and its predictors. Journal of the Canadian Academy of Child and Adolescent Psychiatry, 22(1), 47–54. [PMC free article] [PubMed] [Google Scholar]
- Coghill DR, Seth S, & Matthews K (2014). A comprehensive assessment of memory, delay aversion, timing, inhibition, decision making and variability in attention deficit hyperactivity disorder: Advancing beyond the three-pathway models. Psychological Medicine, 44(9), 1989–2001. doi: 10.1017/S0033291713002547 [DOI] [PubMed] [Google Scholar]
- Conners CK (1997). Conners’ rating scales-revised: Technical manual. North Tonawanda, NY: Multi-Health Systems. [Google Scholar]
- Delis DC, Kaplan E, Kramer JH (2001). Delis-Kaplan executive function system (D-KEFS). San Antonio, TX: Psychological Corporation. [Google Scholar]
- DuPaul GJ, Power TJ, Anastopoulos AD, & Reid R (1998). ADHD Rating Scale—IV: Checklists, norms, and clinical interpretation. New York, NY: Guilford Press. [Google Scholar]
- Eisenberg N (2017). Commentary: What’s in a word (or words) - on the relations among self-regulation, self-control, executive functioning, effortful control, cognitive control, impulsivity, risk-taking, and inhibition for developmental psychopathology - reflections on Nigg (2017). Journal of Child Psychology and Psychiatry, 58(4), 384–386. doi: 10.1111/jcpp.12707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott H, Jones PJ, & Schmidt U (2019). Central symptoms predict posttreatment outcomes and clinical impairment in anorexia nervosa: A network analysis. Clinical Psychological Science, 8(1), 139–154. doi: 10.1177/2167702619865958 [DOI] [Google Scholar]
- Ellis LK, & Rothbart MK (2001). Revision of the Early Adolescent Temperament Questionnaire. Poster presented at the Biennial Meeting of the Society for Research in Child Development, Minneapolis, Minnesota. [Google Scholar]
- Epskamp S, Cramer AOJ, Waldorp LJ, Schmittmann VD, & Borsboom D (2012). qgraph: Network visualizations of relationships in psychometric data. Journal of Statistical Software, 48(4), 1–18. doi: 10.18637/jss.v048.i04 [DOI] [Google Scholar]
- Epskamp S, & Fried EI (2018). A tutorial on regularized partial correlation networks. Psychological Methods, 23(4), 617–634. doi: 10.1037/met0000167 [DOI] [PubMed] [Google Scholar]
- Forbes MK, Rapee RM, Camberis AL, & McMahon CA (2017). Unique associations between childhood temperament characteristics and subsequent psychopathology symptom trajectories from childhood to early adolescence. Journal of Abnormal Child Psychology, 45(6), 1221–1233. doi: 10.1007/s10802-016-0236-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes MK, Wright AGC, Markon KE, & Krueger RF (2019). Quantifying the reliability and replicability of psychopathology network characteristics. Multivariate Behavioral Research. Advance online publication. doi: 10.1080/00273171.2019.1616526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forslund T, Brocki KC, Bohlin G, Granqvist P, & Eninger L (2016). The heterogeneity of attention-deficit/hyperactivity disorder symptoms and conduct problems: Cognitive inhibition, emotion regulation, emotionality, and disorganized attachment. British Journal of Developmental Psychology, 34(3), 371–387. doi: 10.1111/bjdp.12136 [DOI] [PubMed] [Google Scholar]
- Foygel R, & Drton M (2010). Extended bayesian information criteria for gaussian graphical models. Advances in Neural Information Processing Systems, 23, 2020–2028. [Google Scholar]
- Frick MA, & Brocki KC (2019). A multi-factorial perspective on ADHD and ODD in school-aged children: What is the role of cognitive regulation, temperament, and parental support? Journal of Clinical and Experimental Neuropsychology, 41(9), 933–945. 10.1080/13803395.2019.1641185 [DOI] [PubMed] [Google Scholar]
- Fried EI, Eidhof MB, Palic S, Costantini G, Huisman-van Dijk HM, Bockting CLH, . . . Karstoft KI (2018). Replicability and generalizability of posttraumatic stress disorder (PTSD) networks: A cross-cultural multisite study of PTSD symptoms in four trauma patient samples. Clinical Psychological Science, 6(3), 335–351. doi: 10.1177/2167702617745092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fruchterman TM, & Reingold EM (1991). Graph drawing by force-directed placement. Software: Practice and Experience, 21(11), 1129–1164. doi: 10.1002/spe.4380211102 [DOI] [Google Scholar]
- Gagne JR, & Goldsmith HH (2011). A longitudinal analysis of anger and inhibitory control in twins from 12 to 36 months of age. Developmental Science, 14(1), 112–124. doi: 10.1111/j.1467-7687.2010.00969.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goh PK, Lee CA, Martel MM, Fillmore MT, Derefinko KJ, & Lynam DR (2020). Conceptualizing the UPPS-P model of impulsive personality through network analysis: Key dimensions and general robustness across young adulthood. Journal of Personality, 88(6), 1302–1314. doi: 10.1111/jopy.12572 [DOI] [PubMed] [Google Scholar]
- Goh PK, Lee CA, Martel MM, Karalunas SL, & Nigg JT (2020). Subgroups of childhood ADHD based on temperament traits and cognition: concurrent and predictive validity. Journal of Abnormal Child Psychology, 48(10), 1251–1264. doi: 10.1007/s10802-020-00668-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goth-Owens TL, Martinez-Torteya C, Martel MM, & Nigg JT (2010). Processing speed weakness in children and adolescents with non-hyperactive but inattentive ADHD (ADD). Child Neuropsychology, 16(6), 577–591. doi: 10.1080/09297049.2010.485126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haslbeck J, & Waldorp LJ (2015). mgm: Estimating time-varying mixed graphical models in high-dimensional data. arXiv:1510.06871. [Google Scholar]
- Jones P (2018). Networktools: Tools for identifying important nodes in networks. R package version 1.2.1. Retrieved from https://CRAN.R-project.org/package=networktools [Google Scholar]
- Jones PJ, Ma R, & McNally RJ (2019). Bridge centrality: A network approach to understanding comorbidity. Multivariate Behavioral Research. Advance online publication. doi: 10.1080/00273171.2019.1614898 [DOI] [PubMed] [Google Scholar]
- Karalunas SL, Gustafsson HC, Fair D, Musser ED, & Nigg JT (2019). Do we need an irritable subtype of ADHD? Replication and extension of a promising temperament profile approach to ADHD subtyping. Psychological Assessment, 31(2), 236–247. doi: 10.1037/pas0000664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karpenko V, Owens JS, Evangelista NM, & Dodds C (2009). Clinically significant symptom change in children with attention-deficit/hyperactivity disorder: Does it correspond with reliable improvement in functioning? Journal of Clinical Psychology, 65(1), 76–93. doi: 10.1002/jclp.20549 [DOI] [PubMed] [Google Scholar]
- Kofler MJ, Irwin LN, Soto EF, Groves NB, Harmon SL, & Sarver DE (2019). Executive Functioning Heterogeneity in Pediatric ADHD. Journal of Abnormal Child Psychology, 47(2), 273–286. 10.1007/s10802-018-0438-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kopala-Sibley DC, Olino T, Durbin E, Dyson MW, & Klein DN (2018). The stability of temperament from early childhood to early adolescence: A multi-method, multi-informant examination. European Journal of Personality, 32(2), 128–145. doi: 10.1002/per.2151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosten TA, & Rounsaville BJ (1992). Sensitivity of psychiatric diagnosis based on the best estimate procedure. American Journal of Psychiatry, 149(9), 1225–1227. doi: 10.1176/ajp.149.9.1225 [DOI] [PubMed] [Google Scholar]
- Krieger V, Amador-Campos JA, & Gallardo-Pujol D (2019). Temperament, executive function, and attention-deficit/hyperactivity disorder (ADHD) in adolescents: The mediating role of effortful control. Journal of Clinical and Experimental Neuropsychology, 41(6), 615–633. doi: 10.1080/13803395.2019.1599824 [DOI] [PubMed] [Google Scholar]
- Lawson KM, Atherton OE, & Robins RW (2021). The structure of adolescent temperament and associations with psychological functioning: A replication and extension of Snyder et al. (2015). Journal of Personality and Social Psychology, Advance online publication. doi: 10.1037/pspp0000380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lezak MD, Howieson DB, Loring DW, Hannay HJ, & Fischer JS (2004). Neuropsychological assessment (4th ed.). New York, NY: Oxford University Press. [Google Scholar]
- Logan GD (1994). On the ability to inhibit thought and action: A users’ guide to the stop signal paradigm. In Dagenbach D & Carr TH (Eds.), Inhibitory processes in attention, memory, and language (pp. 189–239). San Diego, CA: Academic Press. [Google Scholar]
- Luo Y, Weibman D, Halperin JM, & Li X (2019). A review of heterogeneity in attention deficit/hyperactivity disorder (ADHD). Frontiers in Human Neuroscience, 13, Article 42. doi: 10.3389/fnhum.2019.00042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martel MM (2009). Research review: a new perspective on attention-deficit/hyperactivity disorder: Emotion dysregulation and trait models. Journal of Child Psychology and Psychiatry and Allied Disciplines, 50(9), 1042–1051. doi: 10.1111/j.1469-7610.2009.02105.x [DOI] [PubMed] [Google Scholar]
- Martel MM (2016). Dispositional trait types of ADHD in young children. Journal of Attention Disorders, 20(1), 43–52. doi: 10.1177/1087054712466915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martel M, Nikolas M, & Nigg JT (2007). Executive function in adolescents with ADHD. Journal of the American Academy of Child & Adolescent Psychiatry, 46(11), 1437–1444. doi: 10.1097/chi.0b013e31814cf953 [DOI] [PubMed] [Google Scholar]
- Martel MM, & Nigg JT (2006). Child ADHD and personality/temperament traits of reactive and effortful control, resiliency, and emotionality. Journal of Child Psycholology and Psychiatry, 47(11), 1175–1183. doi: 10.1111/j.1469-7610.2006.01629.x [DOI] [PubMed] [Google Scholar]
- Miller NV, Hane AA, Degnan KA, Fox NA, & Chronis-Tuscano A (2019). Investigation of a developmental pathway from infant anger reactivity to childhood inhibitory control and ADHD symptoms: Interactive effects of early maternal caregiving. Journal of Child Psychology and Psychiatry, 60(7), 762–772. doi: 10.1111/jcpp.13047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyake A, & Friedman NP (2012). The nature and organization of individual differences in executive functions: Four general conclusions. Current Directions in Psychological Science, 21(1), 8–14. doi: 10.1177/0963721411429458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nigg JT (2017). Annual research review: On the relations among self-regulation, self-control, executive functioning, effortful control, cognitive control, impulsivity, risk-taking, and inhibition for developmental psychopathology. Journal of Child Psychology and Psychiatry and Allied Disciplines, 58(4), 361–383. doi: 10.1111/jcpp.12675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nigg JT, Gustafsson HC, Karalunas SL, Ryabinin P, McWeeney SK, Faraone SV, . . . Wilmot B. (2018). Working memory and vigilance as multivariate endophenotypes related to common genetic risk for attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 57(3), 175–182. doi: 10.1016/j.jaac.2017.12.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nigg JT, Sibley MH, Thapar A, & Karalunas SL (2020). Development of ADHD: Etiology, heterogeneity, and early life course. Annual Review of Developmental Psychology, 2(1), 559–583. doi: 10.1146/annurev-devpsych-060320-093413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikolas MA, & Nigg JT (2013). Neuropsychological performance and attention-deficit hyperactivity disorder subtypes and symptom dimensions. Neuropsychology, 27(1), 107–120. doi: 10.1037/a0030685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor BC, Garner AA, Peugh JL, Simon J, & Epstein JN (2015). Improved but still impaired: Symptom-impairment correspondence among youth with attention-deficit hyperactivity disorder receiving community-based care. Journal of Developmental and Behavioral Pediatrics, 36(2), 106–114. doi: 10.1097/DBP.0000000000000124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olatunji BO, Levinson C, & Calebs B (2018). A network analysis of eating disorder symptoms and characteristics in an inpatient sample. Psychiatry Research, 262, 270–281. doi: 10.1016/j.psychres.2018.02.027 [DOI] [PubMed] [Google Scholar]
- Owens JS, Johannes LM, & Karpenko V (2009). The relation between change in symptoms and functioning in children with ADHD receiving school-based mental health services. School Mental Health, 1(4), 183–195. doi: 10.1007/s12310-009-9020-y [DOI] [Google Scholar]
- Pelham WE, Foster EM, & Robb JA (2007). The economic impact of attention-deficit/hyperactivity disorder in children and adolescents. Journal of Pediatric Psychology, 32(6), 711–727. doi: 10.1093/jpepsy/jsm022 [DOI] [PubMed] [Google Scholar]
- Polanczyk G, de Lima MS, Horta BL, Biederman J, & Rohde LA (2007). The worldwide prevalence of ADHD: a systematic review and metaregression analysis. American Journal of Psychiatry, 164(6), 942–948. doi: 10.1176/ajp.2007.164.6.942 [DOI] [PubMed] [Google Scholar]
- Rothbart MK, & Bates JE (2006). Temperament. In Eisenberg N, Damon W, & Lerner RM (Eds.), Handbook of child psychology: Social, emotional, and personality development (p. 99–166). Hoboken, NJ: John Wiley & Sons, Inc. [Google Scholar]
- Simonds J, & Rothbart MK (2004). The temperament in middle childhood questionnaire (TMCQ): A computerized self-report measure of temperament for ages 7–10. Poster session presented at the Occasional Temperament Conference, October, Athens, GA. [Google Scholar]
- Sjowall D, Bohlin G, Rydell AM, & Thorell LB (2017). Neuropsychological deficits in preschool as predictors of ADHD symptoms and academic achievement in late adolescence. Child Neuropsychology, 23(1), 111–128. doi: 10.1080/09297049.2015.1063595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder HR, Miyake A, & Hankin BL (2015). Advancing understanding of executive function impairments and psychopathology: Bridging the gap between clinical and cognitive approaches. Frontiers in Psychology, 6, Article 328. doi: 10.3389/fpsyg.2015.00328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tibshirani R (1996). Regression shrinkage and selection via the lasso. Journal of the Royal Statistical Society: Series B (Methodological), 58(1), 267–288. doi: 10.1111/j.2517-6161.1996.tb02080.x [DOI] [Google Scholar]
- Verbruggen F, Aron AR, Band GP, Beste C, Bissett PG, Brockett AT, . . . Boehler CN (2019). A consensus guide to capturing the ability to inhibit actions and impulsive behaviors in the stop-signal task. Elife, 8, e46323. doi: 10.7554/eLife.46323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D (2003). Wechsler intelligence scale for children (4th ed.). San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Whittle S, Allen NB, Lubman DI, & Yucel M (2006). The neurobiological basis of temperament: Towards a better understanding of psychopathology. Neuroscience & Biobehavioral Reviews, 30(4), 511–525. doi: 10.1016/j.neubiorev.2005.09.003 [DOI] [PubMed] [Google Scholar]
- Wichstrøm L, Penelo E, Viddal KR, de la Osa N, & Ezpeleta L(2018). Explaining the relationship between temperament andsymptoms of psychiatric disorders from preschool to middle child-hood: hybrid fixed and random effects models of Norwegian and Spanish children. Journal of Child Psychology and Psychiatry, 59(3), 285–295. doi: 10.1111/jcpp.1277 [DOI] [PubMed] [Google Scholar]
- Willcutt EG, Nigg JT, Pennington BF, Solanto MV, Rohde LA, Tannock R, . . . Lahey BB. (2012). Validity of DSM-IV attention deficit/hyperactivity disorder symptom dimensions and subtypes. Journal of Abnormal Psychology, 121(4), 991–1010. doi: 10.1037/a0027347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zelazo PD, & Carlson SM (2012). Hot and cool executive function in childhood and adolescence: Development and plasticity. Child Development Perspectives, 6(4), 354–360. doi: 10.1111/j.1750-8606.2012.00246.x [DOI] [Google Scholar]
- Zhou Q, Chen SH, & Main A (2012). Commonalities and differences in the research on children’s effortful control and executive function: A call for an integrated model of self-regulation. Child Development Perspectives, 6(2), 112–121. doi: 10.1111/j.1750-8606.2011.00176.x [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


