Abstract
Problem
At present, formal training in adult learning principles, educational theories, and educational methods is not a core objective of most medical school curricula. As academic medical centers aim to develop the next generation of medical educators, students must be provided an opportunity to learn educational principles, engage in supervised teaching activities, and develop experiences in academic medicine to foster interest early in their development as educators.
Intervention
We developed a longitudinal medical education elective for fourth-year medical students, which was comprised of attending five seminars, leading 15 teaching sessions, formulating a medical education project, and writing a reflective essay. The seminars covered the history of medical education in the USA, adult learning theory and teaching principles, use of various teaching strategies and formats, construction and organization of curricula, effective models of evaluation and feedback provision, and principles of educational research.
Context
This exploratory quasi-experiment incorporated a concurrent mixed methods data collection approach via pre- and post-seminar surveys and narrative reflection essay document analyses.
Impact
Learners revealed favorable changes in their self-efficacy and self-perceived knowledge and attitudes towards medical education. A qualitative analysis of the reflective essays revealed five thematic categories (learning impacts, medical educator growth, leadership growth, medical school reflections, and future professional plans) and thirteen sub-categories. Students found many opportunities to implement high-quality educational projects, expressed commitment to pursuing teaching careers, and felt better equipped to assume a leadership role as change agents in academic medicine.
Lessons Learned
Findings are likely relevant to critical stakeholders who advocate for the inclusion of formal educational skills training into medical education curricula.
Keywords: Academic medicine, Medical teaching, Leadership, Educational skills, Senior elective
Introduction
The role of clinician-educators has been widely recognized as pivotal to the educational objectives and clinical functions of academic medical centers [1, 2]. This awareness has led to a steady growth of clinical-educator tracks provided to faculty and graduate trainees at medical schools in recent years. Although trainee instruction in teaching skills has become a core requirement for many residency programs, this is not so for medical students and therefore not included in most medical school required curricula [3]. Many schools do offer a range of 1–8-week elective opportunities or have the option of a medical education pathway of emphasis which can offer students opportunities to teach and complete curricular projects [4–9].
Accordingly, medical students may benefit from formal training in foundational medical educational principles and theories, effective feedback provision, utilization of evidence-based diverse teaching modalities, and opportunities to connect with medical education mentors, practice teaching skills in a supervised setting, and develop and present scholarly work through professional conferences and academic journals. Exposure to such opportunities under the guidance of influential mentors early in the development of medical trainees has been shown to increase interest in careers in academic medicine, further serving the mission of the academic medical center [10].
Yoon et al. [11] performed a qualitative analysis of narrative reflections from students who experienced a medical educator course. In their prior study, students indicated themes such as using teaching strategies for adult learning, preparing for class, modeling professionalism, incorporating clinical correlations, exceeding course requirements, giving and receiving feedback, providing mentoring, creating a positive learning climate, and growing as educators [11]. Students are clearly highly engaged parties in improving medical education and are eager to be involved. Burk-Rafel et al. [12] noted that they are “untapped educational change agents.”
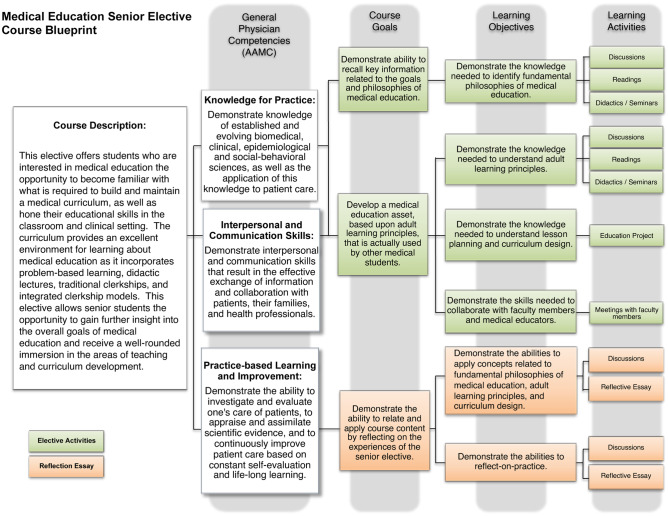
At our institution, we developed a longitudinal medical education elective for fourth-year medical students, comprised of attending five seminars, leading 15 teaching sessions, formulating a curricular project, and ultimately writing a reflective essay (Fig. 1). In this study, we analyzed student survey data from this elective and a qualitative analysis of their end-of-course reflective essays. Our research questions were as follows:
To what degree did the senior elective influence self-efficacy and self-perception of abilities as a medical educator?
How did the education curricular project promote reflection on management and leadership growth of 4th-year medical students?
To what extent did 4th-year medical students use the reflective essay to help inform their future professional plans as medical educators and change agents in academic medicine?
Fig. 1.
Course blueprint that visually describes the alignment of general physician competencies with primary course goals, learning objectives, and learning activities. Green boxes represent activities conducted as part of the elective. Orange boxes represent course components specifically aligned with the student reflection essay
Methods
Curricular Intervention
We developed and offered a medical education senior elective to approximately 10–15 fourth-year medical students per year. Students began the course by attending five seminars at the beginning of the academic year. These seminars covered the history of medical education in the United States, principles of adult learning and educational theories, small group and problem-based learning facilitation, case vignette writing, principles of team-based learning, clinical and bedside teaching, the microskills of teaching, running teaching rounds, writing learning objectives, designing exam questions, designing an Objective Structured Clinical Exam (OSCE), provision of effective feedback, the RIME evaluation model, mentoring students with difficulties, and principles of educational research.
Students were responsible for reading all assigned materials and being prepared to discuss pertinent topics at each seminar. Surveys assessing self-perceived medical education knowledge, skills, and attitudes were completed by students before and after participating in the seminars. Students were then required to lead at least 15 supervised teaching sessions over the course of the academic year. Opportunities for leading teaching sessions included, but were not limited to, problem-based learning (PBL) small groups, team-based learning (TBL) sessions, patient-oriented problem solving (POPS) sessions, skills labs (anatomy, surgical, obstetrics), clinical teaching (bedside, free clinics), lectures, bedside teaching rounds, and medical education journal club facilitation. Students also formulated a curricular medical education project, and ultimately wrote a reflective essay describing lessons learned and their potential interests in academic medicine as a career. Upon the successful completion of the elective, students received two weeks of elective credit and a certificate of completion.
Organization and Setting
The five seminar sessions required a small learning space that could accommodate up to 20 students and was equipped with audio-visual equipment to present material. Student participation in the fifteen separate teaching sessions did not require particular materials and were specific to the chosen activity. Likewise, physical space and materials required for completion of student curricular projects were specific to each chosen project. The university’s learning management system facilitated course organization and was used to post the course syllabus, readings, and other digital course materials.
The course faculty are both medical education deans and general internists (Associate Dean of Curriculum and Regional Dean for Medical Education). They provided all the seminars. The Associate Dean of Curriculum had oversight of all the projects but there are individual faculty mentors for each curricular project. The class size for this elective ranged from 6 to 15 per class. During the timeframe of this study, we collected 34 survey responses and 33 essays from the participants. Informal peer and faculty feedback was provided during teaching sessions, but no standardized rubrics were used. Additionally, medical students were not assigned teaching sessions. Rather, they had a choice of clinical bedside sessions, problem-based learning in courses, case-based or team-based learning sessions in clerkships, leading a medical education journal club, or facilitating other small group sessions. They kept logs of their teaching sessions and hours. Any growth in knowledge was self-assessed because there were no formal rubrics of teaching abilities that were assessed by faculty. Students made adjustments based on informal feedback. Education projects were monitored by the course director and by the individual faculty mentor. A summary of seminar topics is provided within Appendix 1. And examples of some educational projects that our medical students completed is located within Appendix 2.
Data Collection and Analysis
Our exploratory quasi-experiment used a concurrent mixed methods data collection approach to analyze student reflections and perceptions of their longitudinal learning experiences. Thirty-four students completed pre-/post-surveys with Likert-style prompts and then submitted final essay assignments that were coded retrospectively to help identify emergent themes and patterns. The research team repurposed an existing survey with free-response items (personal communication with Dr. Donna Jeffe at Washington University School of Medicine), which was distributed to students via a hard copy. This was completed at the beginning (pre) and end (post) of the seminars. The surveys focused on items related to medical educator growth, which included learners’ self-efficacy (eight prompts with a five-point scale) and self-perception of their abilities (ten prompts with a six-point scale). Survey data was transposed into an Excel workbook and then cleaned for quality assurance. Descriptive statistics (% of responses, medians, and modes) were then calculated to help explain the survey data.
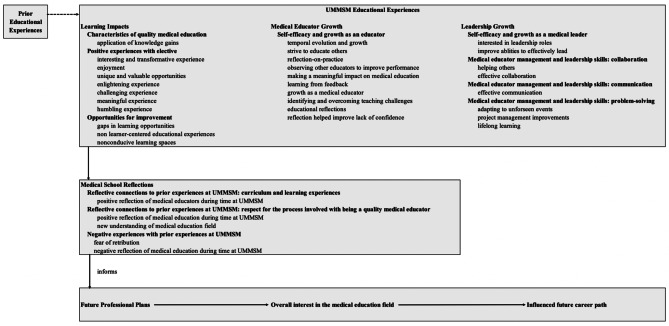
Emergent themes and patterns were revealed through multiple coding procedures of the qualitative data [13–15]. During the document analysis, student essays were read thoroughly by an independent educator (who was not affiliated with the senior elective in any way). Initial themes were highlighted through an open coding process using ATLAS.ti qualitative data analysis and research software. When generating the codebook, these initial umbrella themes were renamed as categories, and then transferred to an MS Excel spreadsheet. Each reflective essay was individually coded to establish emergent sub-categories. To complete the codebook, we paraphrased the sub-categories and aligned each with an umbrella category. For each sub-category code, we calculated frequencies and percentage of students who reported. These data informed the creation of a concept map that summarized and explained the qualitative dataset (Fig. 2). To ensure credibility and trustworthiness of our qualitative data analysis, we shared the summary concept map with several former students who anonymously provided feedback via a member checking process.
Fig. 2.
The visual map summarizes and explains emergent themes from our document analysis. Themes are grouped within categories and subcategories, which demonstrate the evolutionary growth of physicians in-training throughout their entire educational journey, both before and during their medical school training. These learner reflections helped to inform their future professional plans, including their future career paths
Results
Our document analysis (spanning four years of this elective and 33 student reflection essays) revealed five thematic categories and thirteen sub-categories (Table 1). Emergent patterns revealed that during their written reflections, students primarily highlighted learning impacts, medical educator growth, leadership growth, medical school reflections, and future professional plans. Self-efficacy and growth as an educator was a consistent sub-category that appeared in 100% of student essays. Nearly 88% of students specifically addressed how the elective helped them gain both collaboration and problem-solving skills, which they felt would help them as medical educators/leaders. Students also reflected on pre-medical school educational experiences that helped shape their identities as medical educators.
Table 1.
Summary of patterns that resulted from the qualitative document analysis. Five thematic categories emerged, which are listed and formatted in bold font. For each sub-category listed, the frequency of times with which this appeared across the entire dataset is included, and the percentage of students who included this within their reflective essay is presented
| Category | Frequency | % of students |
|---|---|---|
| Learning impacts | ||
| Characteristics of quality medical education | 46 | 75 |
| Positive experiences with elective | 73 | 78.12 |
| Opportunities for improvement | 15 | 25 |
| Medical educator growth | ||
| Self-efficacy and growth as an educator | 286 | 100 |
| Leadership growth | ||
| Personal educational reflections | 51 | 75 |
| Self-efficacy and growth as a medical leader | 36 | 65.625 |
| Medical educator management and leadership skills: collaboration | 70 | 87.5 |
| Medical educator management and leadership skills: communication | 45 | 71.875 |
| Medical educator management and leadership skills: problem-solving | 66 | 87.5 |
| Medical school reflections | ||
| Reflective connections to prior experiences at UMMSM: curriculum and learning experiences | 24 | 46.875 |
| Reflective connections to prior experiences at UMMSM: respect for the process involved with being a quality medical educator | 47 | 68.75 |
| Negative experiences with prior experiences at UMMSM | 7 | 9.375 |
| Future professional plans | ||
| Overall interest in the medical education field | 35 | 65.625 |
Additionally, students consistently stated their positive experiences with both the elective and with the impact of their medical education projects. Similarly, patterns revealed that students felt strongly that this elective helped increase their perceptions of self-efficacy and growth as a medical leader, respect for the process involved with being a quality medical educator, and overall interest in the medical education field for future professional plans. While some students mentioned negative items related to their prior medical school experiences (9.375%) and included specific opportunities for improvement (25%), these patterns emerged at a much lower frequency when compared with the other emergent themes.
Given the inherent complexities involved with explaining medical educator growth, the survey prompts compartmentalized key factors associated with self-efficacy (Table 2a) and with self-perception of abilities (Table 2b). Before the elective (pre-survey), medical students were most confident in their abilities to provide effective feedback (%PRE Strongly Agree and Agree = 41.31%) and that they would ultimately work in an academic environment (%PRE Strongly Agree and Agree = 43.48%). Incoming students were most unsure about their abilities to do the following: utilize the 1-min preceptor model in teaching a student (26.47% unsure), design an OSCE (8.82% unsure), assign a RIME classification to a learner (20.59% unsure), and conduct a curricular educational project (11.76% unsure).
Table 2.
Pre-/post-survey data with descriptive statistics (% of responses, median, and mode are reported). (a) Medical student self-efficacy and (b) medical student self-perception of abilities
| (a) Self-efficacy (n = 34 students; percentages reported) | Pre | Post | |||||||||||||||||||
| Strongly disagree | Disagree | Neutral | Agree | Strongly agree | Median | Mode | Strongly disagree | Disagree | Neutral | Agree | Strongly agree | Median | Mode | ||||||||
| I am confident that I have acquired the skills to teach medical students | 0 | 8.70 | 28.26 | 34.78 | 2.17 | 3.5 | 4 | 0 | 0 | 4.35 | 50.00 | 19.57 | 4 | 4 | |||||||
| I am confident in my understanding of adult learning principles | 2.17 | 21.74 | 36.96 | 10.87 | 2.17 | 3 | 3 | 0 | 0 | 4.35 | 50.00 | 19.57 | 4 | 4 | |||||||
| I am confident in my ability to work with challenging learners in a small group session | 0 | 15.22 | 30.43 | 26.09 | 2.17 | 3 | 3 | 0 | 0 | 6.52 | 56.52 | 10.87 | 4 | 4 | |||||||
| I am confident in my understanding of methods to develop clinical reasoning abilities | 0 | 21.74 | 19.57 | 30.43 | 2.17 | 3 | 4 | 0 | 0 | 4.35 | 56.52 | 13.04 | 4 | 4 | |||||||
| I am confident in my ability to provide effective feedback | 0 | 13.04 | 19.57 | 36.96 | 4.35 | 4 | 4 | 0 | 0 | 4.35 | 34.78 | 34.78 | 4 | 5 | |||||||
| I am confident in my ability to work with students facing academic or nonacademic difficulties | 0 | 8.70 | 30.43 | 28.26 | 6.52 | 3 | 3 | 0 | 0 | 13.04 | 39.13 | 21.74 | 4 | 4 | |||||||
| I am confident in my understanding of principles of educational research | 2.17 | 43.48 | 21.74 | 4.35 | 2.17 | 2 | 2 | 0 | 0 | 21.74 | 39.13 | 13.04 | 4 | 4 | |||||||
| I am confident that I will ultimately work in an academic environment | 2.17 | 4.35 | 23.91 | 32.61 | 10.87 | 4 | 4 | 0 | 2.17 | 13.04 | 30.43 | 28.26 | 4 | 4 | |||||||
| (b) Self-perception of abilities (n = 34 students; percentages reported) | Pre | Post | |||||||||||||||||||
| Unable to do | A lot of supervision | Some supervision | Minimal supervision | Do independently | Unsure | Median | Mode | Unable to do | A lot of supervision | Some supervision | Minimal supervision | Do independently | Unsure | Median | Mode | ||||||
| Facilitate a small group session | 0 | 5.88 | 44.12 | 32.35 | 14.71 | 0 | 3 | 3 | 0 | 0 | 8.82 | 44.12 | 47.06 | 0 | 4 | 5 | |||||
| Facilitate a problem-based learning session | 0 | 17.65 | 38.24 | 41.18 | 2.94 | 0 | 3 | 4 | 0 | 0 | 5.88 | 61.76 | 32.35 | 0 | 4 | 4 | |||||
| Facilitate a team-based learning session | 0 | 29.41 | 35.29 | 23.53 | 8.82 | 2.94 | 3 | 3 | 0 | 2.94 | 11.76 | 67.65 | 17.65 | 0 | 4 | 4 | |||||
| Conduct bedside clinical teaching | 5.88 | 23.53 | 35.29 | 29.41 | 5.88 | 0 | 3 | 3 | 0 | 0 | 17.65 | 55.88 | 26.47 | 0 | 4 | 4 | |||||
| Utilize the 1-min preceptor model in teaching a student | 14.71 | 17.65 | 26.47 | 8.82 | 5.88 | 26.47 | 2 | 0 | 0 | 0 | 14.71 | 26.47 | 58.82 | 0 | 5 | 5 | |||||
| Write learning objectives for an educational session | 5.88 | 26.47 | 29.41 | 20.59 | 14.71 | 2.94 | 3 | 3 | 0 | 0 | 8.82 | 41.18 | 50.00 | 0 | 4.5 | 5 | |||||
| Write clinical vignette exam questions | 0 | 38.24 | 32.35 | 20.59 | 8.82 | 0 | 3 | 2 | 0 | 5.88 | 11.76 | 50.00 | 32.35 | 0 | 4 | 4 | |||||
| Design an objective structured clinical examination | 17.65 | 38.24 | 23.53 | 5.88 | 5.88 | 8.82 | 2 | 2 | 0 | 2.94 | 29.41 | 50.00 | 17.65 | 0 | 4 | 4 | |||||
| Assign a RIME classification to a learner | 2.94 | 26.47 | 26.47 | 11.76 | 11.76 | 20.59 | 2.5 | 3 | 0 | 0 | 11.76 | 44.12 | 44.12 | 0 | 4 | 4 | |||||
| Conduct a curricular educational project | 2.94 | 23.53 | 32.35 | 26.47 | 2.94 | 11.76 | 3 | 3 | 0 | 0 | 14.71 | 38.24 | 47.06 | 0 | 4 | 5 | |||||
Post-survey data revealed that student self-efficacy increased across all categories. The largest increase related to student confidence with understanding of adult learning principles (%PRE Strongly Agree and Agree = 13.04%; %POST Strongly Agree and Agree = 69.57%). Similarly, students self-reported increased confidence with their understanding of principles of educational research (%PRE Strongly Agree and Agree = 6.52%; %POST Strongly Agree and Agree = 52.17%). Medical student self-perceptions of their abilities to effectively serve as a medical educator also increased in all categories. The majority of students reported they could do most tasks independently or with minimal supervision. Conducting bedside clinical teaching, writing clinical exam vignettes questions, and designing an OSCE were the three categories for which students felt they could still use supervision.
Our mixed methods analysis found that students felt more confident in their knowledge of foundational educational principles and with their abilities to implement newly acquired teaching methods. Importantly, high interest in pursuing careers in academic medicine was maintained, though it is important to keep in mind the self-selected nature of these participants. Students enjoyed the flexibility afforded by the course’s longitudinal nature and expressed satisfaction with having the opportunity to work directly with faculty mentors during teaching sessions, while getting a “behind-the-scenes” experience of their own training. All enrolled students completed educational curricular projects in congruence with their own interests, and importantly, several of these have persisted as permanent and valuable components of the current medical curriculum. Essays completed by students reflecting on their experiences in the course mirrored survey data, indicating that students felt better equipped to engage in their future teaching roles as residents.
Integrating results from the document analysis and pre-/post-surveys helped explain how our next generation of academic medicine leaders evolved their personal leadership philosophies throughout their medical education training (Table 3). Positive pre-medical school educational experiences begin shaping their views on what quality teaching is. During medical school, being provided opportunities to apply their learning was a key characteristic of quality medical education. Students reflected positively on their experiences with the elective itself (enjoyment, challenging, interesting, and transformative) as they were able to observe effective teaching practices from mentors and then create their own learning experience for others to use. The elective appeared to help motivate students (strive to educate others, helped improve lack of confidence, make a meaningful impact) and provided them opportunities to grow as professionals (temporal evolution and growth, observing other educators to improve performance, learning from feedback, and identifying and overcoming teaching challenges). Students reflected on their self-efficacy and growth as leaders (interested in leadership roles and improved abilities to effectively lead). Students also highlighted three specific medical educator management and leadership skills: collaboration, communication, and problem-solving (adapting to unforeseen events, project management, and lifelong learning).
Table 3.
Representative student quotations aligned with each of the five emergent patterns
| Emergent patterns from the qualitative analysis | Representative student reflection |
|---|---|
| Learning impacts | “The five seminars served as a safe space to learn from master teachers and open mentorship between faculty and my peers.” |
| Medical educator growth | “I was surprised by the complexity behind methods of teaching (i.e., PBL, TBL) that I have taken for granted during my time in medical school. My knowledge on methods of education and philosophy behind approaches to education were expanded.” |
| Leadership growth | “I learned more how to guide students so that they made connections for themselves. This was rewarding when a particular concept would click for a student.” |
| Medical school reflections | “It made me have significantly greater appreciation for faculty who work to expand our medical education curriculum.” |
| Future professional plans | “This course solidified my desire to pursue a career in medical education. Looking back on my medical school experience, I can clearly identify those individuals who were good teachers and those who were not. Now, rather than merely accepting that distinction, I can critically analyze what made them good teachers and how I can adopt their teaching styles.” |
Discussion
Medical school faculty and leadership benefit when engaging with students in a collaborative manner during curricular renewal and enhancement processes [12, 16]. Expanding intentional opportunities empowers students and fosters collaboration [16]. Furthermore, involving students in values-based curricular enhancement initiatives builds community and stimulates interest in academic medicine as a viable career option 17. These kinds of empowerment efforts can promote mentor–mentee relationships, generate inclusive educational experiences, and increase diversity in academic medicine [18, 19].
This senior elective provided students with opportunities to reflect on their entire medical school journey. Their reflections revealed how they gained new understandings of the medical education field, increased self-efficacy, and developed critical skills. This augmented their respect for the process involved with being a quality medical educator and helped inform their future professional plans. For some students, the elective alongside their past educational experiences, served to influence their future career paths, as they transition into the next phases of their professional journeys to become medical educators and leaders.
Based on our analysis, we recommend that medical schools incorporate longitudinal paths for students where they can develop their educator and leadership skills. Not only can students be involved in evaluation processes, but they can also serve as important liaisons for faculty members. For example, during the design and development of new and technologically enhanced curricular assets, students-as-partners can provide valuable knowledge, skills, and insight. Senior electives can serve as significant capstone experiences, where students may reflect on their learning paths and begin their transitions into academic medicine leadership roles. Student reflections can also help inform data-driven decision-making processes that can drive continuous quality improvements at the institutional level [20, 21].
This exploratory study of 4th-year medical students’ reflection-on-practice was limited to a single institution with a relatively small number of participants, which may impact its generalizability to other situational contexts. A future opportunity for research is to identify whether or not our learners actually pursued a career in academic medicine. Additionally, learners’ self-assessments of their own competencies may present inaccuracies [22]. That said, learner experiences within this senior elective are consistent with previously reported results from similar reflective opportunities. For example, Yoon et al. [11] identified nine themes that described practical medical educator skills. While our study did not intentionally code for their exact themes, our learners did relay similar feedback in terms of their self-efficacy and growth as an educator (Table 4). Taken together, these studies help illustrate the importance of formally including foundational training in academic medicine within the modern medical school curriculum.
Table 4.
Comparison/alignment of this study’s emergent educator-focused patterns against themes from the Yoon et al. [11] article. Two themes did not quite align across studies and are indicated with a blank space in their respective columns
| Yoon et al. (2017) themes | This paper’s educator-focused patterns: self-efficacy and growth as an educator |
|---|---|
| Using teaching strategies for adult learning | Identifying characteristics of quality medical education |
| Preparing for class | Evolving and growing temporally (in how to prepare as a medical educator) |
| Modeling professionalism | Observing other educators to improve performance |
| Providing mentoring | Striving to educate others |
| Exceeding course requirements | Identifying and overcoming teaching challenges |
| Giving and receiving feedback | Learning from feedback |
| Growing as educators | Growing as a medical educator |
| Creating a positive learning climate | Making a meaningful impact on medical education |
| Incorporating clinical correlations. | Reflecting-on-practice helped improve lack of confidence. |
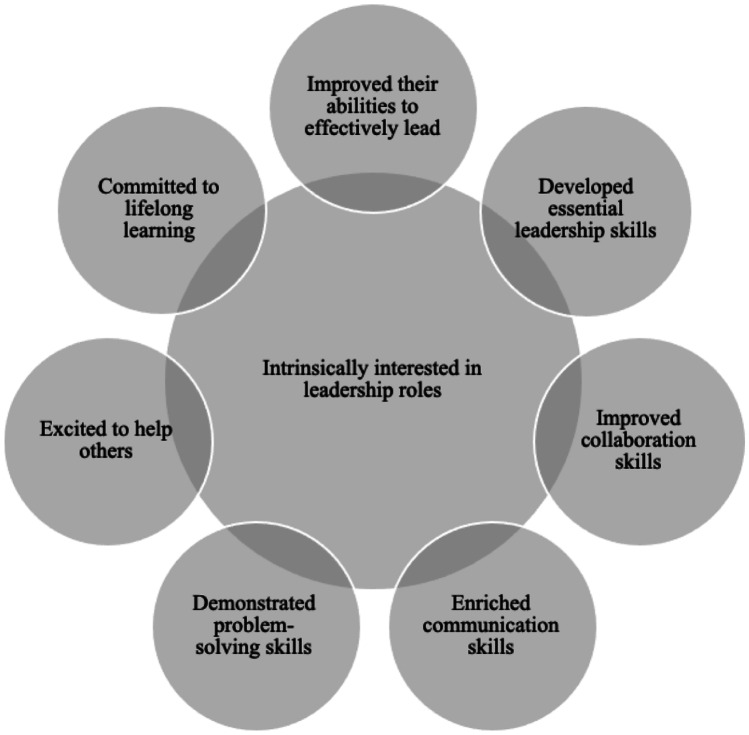
This is particularly true if we want our future leaders in academic medicine to have profound experiences with incorporating adult learning theory into practice, confidence in their abilities to lead, and capacity to contribute to the scholarship of teaching and learning [12, 23]. After all, our medical students are our agents of change for the future of academic medicine and are characterized by key attributes that we can help them nurture (Table 5). Developing effective medical educators of the future relies on sound educational experience and institutional support for curricular innovations [24–27]. A consideration that arises from our quasi-experiment is for medical schools to evaluate their responsibilities of intentionally providing experiential opportunities for medical educator and leadership skills development within our curricula (Fig. 3).
Table 5.
Leadership growth outcomes from the senior elective that help define characteristics of an academic medicine change agent
| Outcomes from senior elective | Representative student reflections from essays |
|---|---|
| Intrinsically interested in leadership roles | “The medical education elective was something I wanted to take part in from my very first year of medical school. I thought it was fascinating that my older medical student colleagues had amassed so much knowledge through med school and had the opportunity to embed that knowledge upon us. Continued education and teaching is such a special quality of medicine and I wanted to have the skills to know how to educate others as I progressed through the field.” |
| Improved their abilities to effectively lead | “These teaching sessions and discussions not only gave me the opportunity to hone my leadership skills, but to get to know the students and bond with them. I believe that a valuable aspect of education is relationship-building. A respectful relationship between teacher and student encourages healthy and enjoyable education for all involved individuals.” |
| Developed essential leadership skills | “I felt like it gave me the freedom to create my own project and let that project evolve and grow. At first, I thought my idea was relatively simple: create a learning module to teach sub-interns how to sign-out effectively. I noticed a gap in our medical school education and felt I could make an impactful change. Once I began, I realized that this project had the potential to be a much larger initiative, and with the assistance of several faculty members, it has.” |
| Improved collaboration skills | “My project for this elective made me realize first-hand that with teaching comes the need for flexibility and open-mindedness, especially when partnering with others to make the curriculum.” |
| Enriched communication skills | “Learning how to effectively give and receive feedback was a particularly useful tool, as I have found that receiving constructive feedback has been vital for my learning and development thus far and learning to implement effective feedback with peers and junior students/residents will undoubtedly be a useful skill during residency. … This is a skill that I enjoyed developing, and I think I was able to improve on as I got more teaching experience. I felt a great sense of gratification every time I was able to ask questions to allow for students to reach answers on their own, or at least identify a specific gap in knowledge to encourage more discussion.” |
| Demonstrated problem-solving skills | “There was not enough curricular time in the clerkship to add another separate teaching session, so I was left with a maximum of 5 slides to teach a very novel topic. I approached the problem knowing that this limit would not be enough, so I decided to add a few questions intermingled throughout the rest of the review to help solidify what was presented. Oddly enough, it took me nearly twice as long to design these questions than it did to research and prepare the original 5 slides. This experience, however, was quite unique. One of the skills that I have nearly perfected over the past 4 years is that of presenting just about anything in 5 slides or less. But designing questions was a whole other animal. It really allowed me to appreciate all the work that goes into making a test question. It also ensured that I had to have a much deeper knowledge of the subject matter so that the questions would be adequate to test and challenge the students. In the end, the short review not only allowed me to help others prepare to be successful on their shelf examination, but also pushed me to stretch myself beyond my normal comfort level.” |
| Excited to help others | “I not only hope to give back at least a fraction of the teaching I have received as a student, but also serve as a role model for future (pre-)medical students in their journeys towards physicianship.” |
| Committed to lifelong learning | “This career is a never-ending journey of lifelong learning and we should be motivated by our desire for personal growth and our duty to do right by our patients. In the future when I am an attending on clinical teams or facilitating TBL sessions, I hope to highlight the importance of self-directed learning and the need for all students of medicine, including fully qualified physicians, to keep up with new knowledge and fully indulge our curiosities.” |
Fig. 3.
Our Senior Elective analysis revealed consistencies in the characteristics that help define an academic medicine change agent. Future leaders in academic medicine will master critical skills and abilities that complement their intrinsic interest in academic medicine leadership roles. Medical schools can facilitate their educator growth and leadership evolution by intentionally including and assessing medical education “touch-points” longitudinally throughout the modern curricula
Acknowledgements
The authors are grateful for the organizational and curricular support provided by Latha Chandran, Alex Mechaber, Laurence Gardner, Paul Mendes, S. Barry Issenberg, and Henri Ford. The authors are also indebted to Dr. Chandran for the helpful reviews and feedback. Countless faculty, staff, and students at both the Miami campus and the regional campus helped with logistical support. Finally, the authors would like to highlight the contributions from the Division of Innovations in Medical Education within the Educational Development Office (EDO) at the University of Miami Miller School of Medicine (UMMSM). This research was conducted when the lead author (Green) was still with the EDO at UMMSM.
Appendix 1
Summary of seminar topics.
Seminar 1: History of medical education, characteristics of good teachers, small group teaching, problem-based learning
Seminar 2: Team-based learning, clinical teaching
Seminar 3: Writing learning objectives, writing multiple choice clinical vignette questions, developing an OSCE
Seminar 4: Providing feedback, mentorship, RIME model
Seminar 5: Educational scholarship and group discussion of planned curricular projects with peer feedback
Appendix 2
Examples of educational projects.
Creation of TBL session on developmental and child psychiatry
PBL case revision
Procedure lab on Suturing/knot tying and IUD insertion for OB clerkship
Website developed to assist students with use of medical interpreters: https://medical-student-language-access-training.webnode.com/
Student developed pressure injury curriculum in Geriatrics clerkship
Student developed and implemented Video Based Empathy small group communication skills lab
Student developed video guide for formal oral case presentations
Team based learning session on nutrition counseling for Family medicine clerkship
Pregnancy options counseling session for the OB-GYN clerkship that included discussions about options for termination of pregnancy
Communication lab on responding to pages as an intern for the Senior Bootcamp Course
Guide to the surgical correlates to anatomy dissection for the Anatomy course.
PPT and skills session on the ophthalmologic exam for Academic Societies trainers.
Team based learning session on pediatrics surgery for the Surgery clerkship
Guide and teaching session for the oral exam topics in the Obstetrics and Gynecology clerkship
“Racial Disparities in Pediatrics” session implemented in Pediatrics clerkship
“Racial Disparities in Obstetrics-Gynecology” session implemented in Obstetrics-Gynecology clerkship
“Contraception” session in Obstetrics-Gynecology clerkship
“Cultural Competency OSCE” submitted to Racial Justice Task Force as proposal
POCUS session on “Right upper quadrant ultrasound imaging”
“Telehealth visit guidelines education and physical exam via telehealth” guidelines
IPE workshop session
Peer mentoring on “Writing a case report”
“Gynecologic Malignancies” session in Obstetrics-Gynecology
Workshop on “Maternal Health Outcomes with Every Mother Counts”
“AKI/Hyponatremia” Team Based learning
OSCE on “Opioid-use disorder”
TBL session on “Healthcare policy education”
TBL on “Eating Disorders”
CBL on “Postpartum hemorrhage”
Declarations
Ethical Approval
University of Miami’s IRB ID: 20190045 and was approved on 1/14/2019.
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Barchi RL, Lowery BJ. Scholarship in the medical faculty from the university perspective: retaining academic values. Acad Med. 2000;75(9):899–905. doi: 10.1097/00001888-200009000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Levinson W, Rubenstein A. Integrating clinician-educators into Academic Medical Centers: challenges and potential solutions. Acad Med. 2000;75(9):906–912. doi: 10.1097/00001888-200009000-00012. [DOI] [PubMed] [Google Scholar]
- 3.Pasquinelli LM, Greenberg LW. A review of medical school programs that train medical students as teachers (MED-SATS) Teach Learn Med. 2008;20(1):73–81. doi: 10.1080/10401330701798337. [DOI] [PubMed] [Google Scholar]
- 4.Alger EA. A fourth-year elective in medical education. Acad Med. 1998;73(5):581. doi: 10.1097/00001888-199805000-00043. [DOI] [PubMed] [Google Scholar]
- 5.Pasquale SJ, Pugnaire MP. Preparing medical students to teach. Acad Med. 2002;77(11):1175–1176. doi: 10.1097/00001888-200211000-00046. [DOI] [PubMed] [Google Scholar]
- 6.Pasquale SJ, Cukor J. Collaboration of junior students and residents in a teacher course for senior medical students. Med Teach. 2007;29(6):572–576. doi: 10.1080/01421590701468737. [DOI] [PubMed] [Google Scholar]
- 7.ten Cate O. A teaching rotation and a student teaching qualification for senior medical students. Med Teach. 2007;29(6):566–571. doi: 10.1080/01421590701468729. [DOI] [PubMed] [Google Scholar]
- 8.Song C, Davis BJ, Lambert DR. The Medical Education Pathway: description and early outcomes of a student-as-teacher program. Acad Med. 2015;90(4):458–461. doi: 10.1097/ACM.0000000000000548. [DOI] [PubMed] [Google Scholar]
- 9.Milburn S, Fried M, Risley M, Schlair S. Student-as-teacher: the creation of a medical student-driven education elective. Med Educ. 2016;50(11):1156. doi: 10.1111/medu.13172. [DOI] [PubMed] [Google Scholar]
- 10.Greenberg RB, Ziegler CH, Borges NJ, Elam CL, Stratton TD, Woods S. Medical student interest in academic medical careers: a multi-institutional study. Perspect Med Educ. 2013;2(5–6):298–316. doi: 10.1007/s40037-013-0051-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yoon MH, Blatt BC, Greenberg LW. Medical students’ professional development as educators revealed through reflections on their teaching following a students-as-teachers course. Teach Learn Med. 2017;29(4):411–419. doi: 10.1080/10401334.2017.1302801. [DOI] [PubMed] [Google Scholar]
- 12.Burk-Rafel J, Jones RL, Farlow JL. Engaging learners to advance medical education. Acad Med. 2017;92(4):437–440. doi: 10.1097/ACM.0000000000001602. [DOI] [PubMed] [Google Scholar]
- 13.Harding J. Qualitative data analysis from start to finish. London: Sage Publications; 2013. [Google Scholar]
- 14.Creswell JW. Research design: qualitative, quantitative, and mixed methods approaches. Thousand Oaks (CA): Sage Publications; 2014. [Google Scholar]
- 15.Creswell JW. A concise introduction to mixed methods research. Thousand Oaks (CA): Sage Publications; 2015. [Google Scholar]
- 16.Fetterman DM, Deitz J, Gesundheit N. MPH empowerment evaluation: a collaborative approach to evaluating and transforming a medical school curriculum. Acad Med. 2010;85(5):813–820. doi: 10.1097/ACM.0b013e3181d74269. [DOI] [PubMed] [Google Scholar]
- 17.Geraghty JR, Young AN, Berkel TDM. Empowering medical students as agents of curricular change: a value-added approach to student engagement in medical education. Perspect Med Educ. 2020;9:60–65. doi: 10.1007/s40037-019-00547-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Farkas AH, Bonifacino E, Turner R, Tilstra SA, Corbelli JA. Mentorship of women in academic medicine: a systematic review. Journ gen int. 2019;1:1–8. doi: 10.1007/s11606-019-04955-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fernandez A, Chen V, Quan J, Martinez A, Flowers L, Aronson L. Evaluation of a medical student research and career development program to increase diversity in academic medicine. Acad Med. 2019;94(8):1220–1228. doi: 10.1097/ACM.0000000000002760. [DOI] [PubMed] [Google Scholar]
- 20.Blouin D, Tekian A. Accreditation of medical education programs: moving from student outcomes to continuous quality improvement measures. Acad Med. 2018;93(3):377–383. doi: 10.1097/ACM.0000000000001835. [DOI] [PubMed] [Google Scholar]
- 21.Hedrick JS, Cottrell S, Stark D, Brownfield E, Stoddard HA, Angle SM, Buckley LA, Clinch CR, Esposito K, Krane NK, Park V. A review of continuous quality improvement processes at ten medical schools. Med Sci Educ. 2019;29(1):285–290. doi: 10.1007/s40670-019-00694-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Davis DA, Mazmanian PE, Fordis M, Van Harrison R, Thorpe KE, Perrier L. Accuracy of physician self-assessment compared with observed measures of competence: a systematic review. JAMA. 2006;296(9):1094–1102. doi: 10.1001/jama.296.9.1094. [DOI] [PubMed] [Google Scholar]
- 23.Wagenschutz H, McKean EL, Mangrulkar R, Zurales K, Santen S. A first-year leadership programme for medical students. Clin Tea. 2019;16(6):623–629. doi: 10.1111/tct.13005. [DOI] [PubMed] [Google Scholar]
- 24.den Bakker CR, Hendriks RA, Houtlosser M, Dekker FW, Norbart AF. Twelve tips for fostering the next generation of medical teachers. Med Teach. 2021:1–5. 10.1080/0142159X.2021.1912311 [DOI] [PubMed]
- 25.Baker L, Shing LK, Wright S, Mylopoulos M, Kulasegaram K, Ng S. Aligning and applying the paradigms and practices of education. Acad Med. 2019;94(7):1060. doi: 10.1097/ACM.0000000000002693. [DOI] [PubMed] [Google Scholar]
- 26.Geraghty JR, Young AN, Berkel TDM, Wallbruch E, Mann J, Park YS, Hirshfield LE, Hyderi A. Empowering medical students as agents of curricular change: a value-added approach to student engagement in medical education. Perspect Med Educ. 2020;9(1):60–65. doi: 10.1007/s40037-019-00547-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goh PS. Medical educator roles of the future. Med Si Edu 2020;1:5–7. [DOI] [PMC free article] [PubMed]