Abstract
Introduction
This study investigated the perspectives of medical students on the factors influencing empathy development during their undergraduate training.
Methodology
A descriptive phenomenological approach was used to generate illustrations of empathy development and decline that had educational significance and applicability. Individual online semi-structured interviews were conducted to elicit experiential details from twelve final-year medical students. The interview recordings were transcribed verbatim, and data were analysed employing Braun and Clarke’s thematic analysis method.
Results
The self-reported empathic behavior of medical students seemed to have improved with time in medical school. Students attributed their empathy development to real patient encounters, positive role-modelling by teachers, and attainment of confidence and personal maturity. They identified exams, academic overload, time constraints, personal stresses, negative role models, unconducive learning environments, and lack of formal empathy training as barriers to empathy development.
Conclusion
Medical institutes should identify and address the barriers to empathy development and encourage the holistic development of medical students. Furthermore, medical educators should model their behavior accurately for their increasing roles and responsibilities and support the students in their empathic expressions with patients.
Keywords: Empathy, Medical education, Medical students, Empathy development, Phenomenological approach
Introduction
Empathy is an essential element of a trustful patient-physician relationship [1] and a crucial component of quality healthcare [2]. Empathic responses by healthcare professionals are associated with improved clinical outcomes, higher patient satisfaction [1, 3], fewer malpractice complaints, greater professional fulfilment, and enhanced physical and mental well-being of the physicians [4, 5]. Research reveals that empathic communications empower patients to address their health problems [6]. Patient’s perception of the physician’s empathic concern and trust improves the effectiveness of medical care [7, 8]. Studies have confirmed the positive health outcomes of patients’ perceptions of empathic care in some patients with diabetes, high cholesterol, and even the common cold [9, 10]
Greater empathy and professionalism have been reported to be associated with physicians’ well-being [11]. Physicians who are empathic with patients experience more professional satisfaction and lesser burnout than those who maintain a distance from patients [12]. Several professional organizations and medical education associations in various countries accept that empathy is a necessary attribute of a physician that needs to be fostered in medical students [11]. The General Medical Council UK [13] and Association of American Medical Colleges [14] have accepted incorporating empathy development in both undergraduate and postgraduate medical curricula to promote professionalism in medical students [15].
However, many studies have reported an empathy erosion in medical students during their undergraduate education [16, 17]. Conversely, some studies have reported no change [18, 19], and some have instead shown an increase in medical students’ empathy [8, 20]. The results of these studies are conflicting; furthermore, most of these studies had adopted a quantitative approach employing self-report tools [21–23]. Researchers have argued against the accuracy of the results reported by self-reported empathy instruments [24–26]. Furthermore, these quantitative studies have failed to explain the logic of empathy changes in medical students [27]. The quantitative studies on students’ empathy suggest that the factors that might affect the alleged empathy erosion need to be understood by qualitative studies [22, 28, 29].
Researchers have recommended exploring medical students' perspectives on the elements of medical education that promote or deter empathy [16, 30]. However, exploratory studies considering students’ views are limited, and quantitative studies employing self-administered questionnaires have not furnished a profound conceptualization of students’ experiences regarding empathy in the context of patient care. In order to design “intended” and “evidence-based interventions” for fostering empathy in medical students, a deeper understanding of determinants of empathy is exceptionally crucial [11].
This exploratory research was conducted to gain a comprehensive conception of empathy development in medical students. The study objectives were to (i) identify the factors influencing empathy development, (ii) explore if there were any significant changes in empathic behavior of medical students with time in their undergraduate medical training, and (iii) conceptualize the ways to enhance empathy in medical students.
Methodology
Settings
This study was carried out at SSR Medical college in Mauritius. The 5-year MBBS course at SSR Medical College is divided into ten semesters, and clinical teaching starts from the fourth semester. Teaching in clinical subjects is based primarily on clinical ward rotations and community visits, including peripheral healthcare organizations. No formal training to promote empathy development in medical students is in practice. Students learn to empathize by observing their teachers. This study was devised to understand how students experience empathy and how the factors described in the literature influence empathy development in medical students. The approval to conduct the study was obtained from the Institutional Research Ethics Committee. Medical students’ perspectives were gained through a qualitative descriptive phenomenological approach [31, 32].
Participant Recruitment and Sampling
Inclusion Criteria
Tenth semester (final year), medical students (n = 40) who had ample experience with patients were invited to participate in the study. The aim of the study was announced in class. Participation in the study was not compulsory, and to eliminate potential bias, it was explained to the students that their participation would not affect their academic careers in any way. Of the respondents, the first twelve students were initially included to participate in the study.
Exclusion Criteria
Medical students of the other semesters who did not have sufficient exposure with patients were not included in the study.
The invitation letters and study details were sent to the selected participants through emails. Written informed consent was obtained, and an interview was scheduled with each of the twelve participants. Maintaining the participants’ anonymity in online interviews was not possible; nevertheless, the confidentiality of their personal information was ensured.
Data Collection
Semi-structured online interviews were conducted, and each interview lasted for about 68 min. Before commencing the research interviews, a pilot run of the entire interview process was held with a senior colleague. The purpose of the pilot run was to ensure the relevance of questions and test the effectiveness of the recording and data-collection processes. The data collected from that interview were discarded.
Permission to audiotape interview details and transcribe verbatim was obtained from all the participants. An interview guideline was used (Table 1); however, the participants had the freedom to guide the discussion. The study participants were encouraged to communicate freely about their personal beliefs, views, and experiences. The researcher had the opportunity to contemplate the diverse ways in which things were interpreted. Leading questions were avoided. Throughout the interviews, the researcher maintained the ethical aspects of consent, confidentiality, and respect for the student [8]. The individual interviews helped gain insight into participants' perspectives and assisted in dealing with sensitive matters that the participants might have failed to deliberate in a group [33].
Table 1.
Interview guideline
| Q.N. | Question |
|---|---|
| 1 | Can you please explain what it means to be an empathic physician? |
| 2 | Can you explain your own empathy in context with patient care? |
| 3 | Have you ever encountered any situation when it was difficult to be empathic with the patient? Can you describe that situation? |
| 4 | Can you describe any situation when it was easier to deal with patients’ emotions and expectations? |
| 5 |
Have you ever felt that your empathic behavior with patients has changed through your experiences of the M.B.B.S Course until now in your last year? Can you please describe it? |
| 6 | Can you please specify which aspects of your curriculum have helped you to develop empathy? |
| 7 | Can you explain which aspects of your curriculum have negatively influenced or hindered the development of your empathy? |
| 8. | Do you think teachers can contribute to empathy development in medical students? Can you please take a few moments to describe any instance when you felt motivated or even demotivated by a teacher’s attitude? |
| 9. | Can you suggest how empathy be enhanced in medical students? |
| 10. | Can you add something to the concept of the importance of the development of empathy in medical students? |
Data Management
The recorded interviews were accurately transcribed. The recordings and transcripts were transferred securely by compression and encryption. The backup of the data was kept in portable devices, as well as in the password-protected files. All the portable devices and paper data were stored safely in a locked cabinet.
Data Analysis
The data were analyzed using the thematic analysis method of Braun and Clarke [34]. The thematic analysis aims to understand participants’ illustrations of lived experiences related to the research question in interviews [32]. An inductive rather than a deductive approach was used during the data analysis process [31]. Data collection and analysis were carried out simultaneously to include additional sampling plans and new interview questions after profoundly understanding the evolving themes [35]. However, no further participants were recruited, as after the interviews with twelve participants, no new information was uncovered, and data saturation for the research question was assumed.
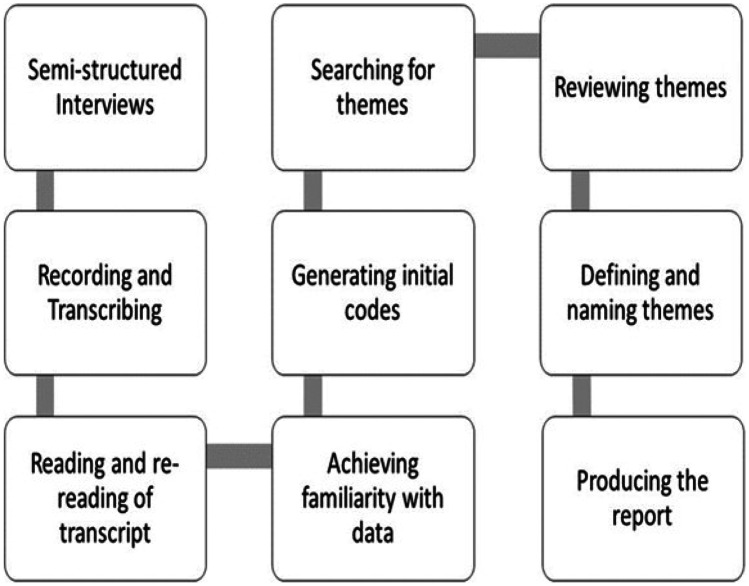
The thematic analysis procedure included six steps [34: pg 87]. The summary of the data analysis process is shown in Fig. 1.
Fig. 1.
Steps of data analysis
Familiarizing with Data
All the narrative data were thoroughly and repeatedly read with an open mind to gain familiarity with the data [36]. The objective was to explore the meanings of the experiences expressed in the data to extract new information instead of confirming what is already known [32].
Generating Initial Codes
Initial meanings (codes) were generated across all the data. The codes were marked manually by making notes in the transcript and highlighting and labeling text sections [36]. There was continuous focus on the research question, thus ensuring the relevance of the information to the research question. A coding framework was generated from the data. The transcripts were reviewed to identify emerging patterns and themes.
Searching for Themes
In exploring the relationship between codes, themes were developed to illustrate the process being studied [35–37].
Reviewing Themes
A thematic map was developed after relating the themes to the generated codes [31].
Defining and Naming Themes
The themes were named and clearly described. Finally, a report on the analyses related to the research question and relevant literature was produced [31].
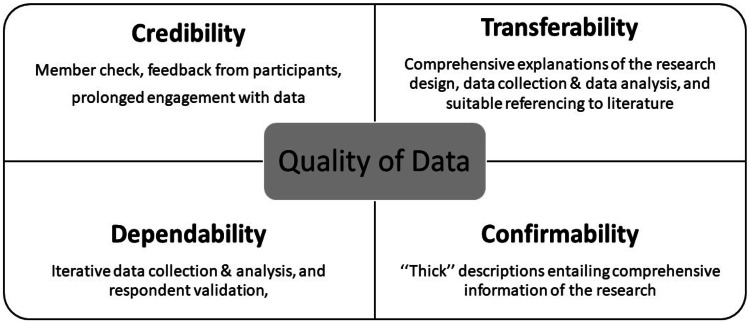
Quality of Data
The Standards for Reporting Qualitative Research (SRQR) were used as a checklist to ensure that the essential elements of the study were illustrated [38]. In addition, the following quality parameters were addressed (Fig. 2): credibility, transferability, dependability, and confirmability to ensure quality in qualitative research [35, 39].
Fig. 2.
Quality of data
Results
The participants expressed their views on the factors that affected their empathic behavior with patients and suggested diverse ways to enhance empathy. The themes and sub-themes that emerged from the students’ narratives have been described. Individual themes have been supported by the direct quotations provided from the data. The grammatical structure of the sentences has been left unchanged for the sake of authenticity. A summary of the themes and subthemes is shown in Table 2.
Table 2.
Summary of themes and subthemes
| Themes | Influences on empathy | Empathy changes | Enhancing empathy |
|---|---|---|---|
| Subtheme 1 | Workplace culture | Real patient encounters | Curriculum remodelling |
| Patient contact | Patient contact | ||
| Patients’ attributes | Local language | ||
| Hierarchy | Workshops | ||
| Language barriers | Roleplaying | ||
| Physical environment | Simulation-based learning | ||
| Stories and narratives | |||
| Case and problem-based assessments | |||
| Medical humanities | |||
| Subtheme 2 | Institutional culture | Self-confidence | Stress management |
| Positive and negative role models | |||
| Curriculum | |||
| Examinations and assessments | |||
| Strict discipline | |||
| Lack of student support | |||
| Positive encouragement | |||
| Subtheme 3 | Students’ characteristics | Personal maturity | Faculty development |
| Personal upbringing | |||
| Stress | |||
| Resilience | |||
| Mood changes |
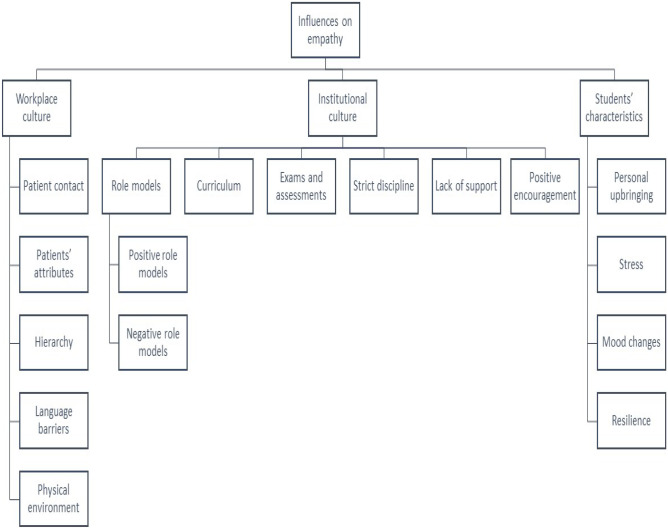
Theme 1—Influences on Empathy
Students described several factors that affected their empathic expressions with patients. Negative and positive effects have been described under three subthemes: workplace culture, institutional culture, and students’ characteristics (Fig. 3).
Fig. 3.
Influences on empathy
Workplace Culture
All the students agreed that they had fostered their skills to empathize with patients through face-to-face encounters with patients. However, they felt visiting the same wards and the same patients repeatedly hampered their empathy. Some students talked about hierarchy and felt that patients did not take them seriously. They further reported that occasionally, they failed to express empathic behavior due to rude, abusive, uncooperative, or fearful patients. A few students felt that the overcrowded and noisy clinics hampered their empathic expressions with patients. Some students identified language as the primary barrier in expressing empathy. International students who were not fluent in the local language failed to express empathy.
“It is challenging to empathise with those patients who do not understand your language. You can extract some factual information; however, you cannot build up an empathetic relationship with the patient.” (Participant 10, p. 3).
Institutional Culture
Almost all the students agreed that most of their teachers had been highly instrumental in making them learn the correct empathic behavior towards patients. The students admired their passion, humility, and humanity. However, students described that a few teachers, especially the junior ones, were rude and impolite to patients. They felt distressed when teachers were less empathic with patients.
Students felt that their curriculum mainly emphasized the biomedical aspect and lacked psychosocial elements in patient management. They described that the pre- and para-clinical subjects were primarily theoretical.
“With all theoretical knowledge, I might become a good teacher but never a practitioner.” (Participant 7, p. 4).
Additionally, they indicated that the time constraints and academic load made them feel stressed. They expressed that they were less empathic during case presentations or examinations. They felt rushed and stressed and preferred to spend lesser time with patients. Some felt low and less empathetic owing to strict discipline and lack of student support at school. However, most of the students felt motivated when encouraged by senior faculty members.
Students’ Characteristics
Most of the students contended that they were less empathic when stressed due to personal reasons, academic load, time constraints, burnout, and sleep deprivation. They reported that their mood changes due to several reasons affected their empathic behavior; however, that empathy decline was transient:
“If you’re having a bad day with your family, then that might come out on your patients because we’re more affected by our personal lives than our professional lives.” (Participant 6, p. 5).
Some students felt that the coping strategies learned during their childhood helped them develop resilience and empathic expressions with patients.
Theme 2—Empathy Changes
All the students noted that their empathic behavior had improved with time. In addition, most of the students agreed that they were more comfortable interacting with patients. The subthemes identified have been shown in Table 2.
Real Patient Encounters
Students agreed that it was through real patient encounters that they could improve their skills to express empathy towards patients: “I compare myself at the beginning of the second year, and now as a final-year student. When I interact with the patient, I’m a lot more confident and comfortable.” (Participant 5, p. 3).
Self-confidence
Students also related empathy with self-confidence: “In the beginning, when I had to speak to patients, it was exceedingly difficult, mainly because I was incredibly nervous speaking to patients, and it was difficult to create that environment that was comfortable for both the patient and me. As the years went on, it was easier to relate to the patients, and it was easier for me to speak to them.” (Participant 3, p. 4).
Personal Maturity
Some students related empathy to their maturity level. One of the students commented: “It takes time to develop emotionally. You develop empathy over some time when you start realising the need for it. When you see the situation of a patient, you realise the worth of it.” (Participant 7, p. 3).
Positive Role Modelling
Students felt that their empathy had improved only because of the positive role modelling by senior teachers. They mentioned that they learned empathy by observing them.
One of the students commented:
“I have no doctors in the family, so I came with zero knowledge, and whatever I came to know was because of our teachers and what I observed in the hospital through whatever they taught us. So, we only learn from them.” (Participant 6, p. 3).
Theme 3—Enhancing Empathy
Almost all the students felt that empathy could be enhanced by appropriate training. The subthemes identified from the narratives are shown in Fig. 4.
Fig. 4.

Enhancing empathy
Curriculum Remodelling
Students suggested curricular remodelling to incorporate empathy as an essential skill to be developed in medical students. They suggested early clinical exposure, extended hours in the hospitals, exposure to diverse patients, and inclusion of regional language as a special module in the official curriculum.
Students recommended that the institution should hold special workshops to impart empathy training. Some students suggested that such workshops should be held before the actual encounters with patients. Some suggested including role-playing, and some felt that the stories and narratives could also develop students’ empathy.
Most of the students were against simulation-based learning. One of the students commented: “You can understand the situation, but you can’t imagine or feel the patients' perspectives through simulations.” (Participant 7, p. 5).
Students talked about the assessment of empathic skills. They suggested that assessments would motivate students to develop their skills. They recommended using case scenarios to assess empathic skills. Some students recommended introducing medical humanities in the curriculum.
Stress Management
Some students suggested that the institution should organize activities to destress students. Some students expressed that the teachers should encourage empathy development through their behavior and interaction with students and other staff members.
Faculty Development
Some of the students indicated that their teachers should also be given training on enhancing empathy in medical students:
“Sometimes, teachers don’t know that the students are observing them. I think there should be counselling for teachers also. They should learn what are the things to be done in front of the students to increase their empathy with patients.” (Participant 8, p. 5).
Thus, the students recommended early patient contact, experiential learning methods, formal empathy training, and faculty development to enhance medical students' empathy.
Discussion
A large number of factors that influence medical students’ empathic behavior with patients were identified. Students’ views have illuminated several facets of the medical curricula that demand the attention of medical educators.
All the students agreed that they learned the skills to empathize with patients through direct encounters with patients. Studies have reported that the innate ability to empathize improves with learning experiences [24] and real-life patient encounters [40, 41]. For developing a deeper level of empathy, face-to-face interactions and real patient contact are exceptionally crucial [42]. Although students acknowledged that they developed their empathy by interacting with patients, they felt visiting the same wards and patients repeatedly hampered their empathy. Studies reveal that empathy declines when medical students start regarding patients as cases rather than human beings [24].
Students reported that sometimes, they failed to express empathic behavior due to rude, abusive, uncooperative, or fearful patients. Similar results have been reported by several researchers [8, 16, 24]. Literature reveals that empathic behavior is promoted by appreciative, cooperative, good-natured, compliant, and positive-minded patients. In contrast, empathic expressions become more challenging with insulting, demanding, irritating, ungrateful non-compliant patients [16].
Students talked about hierarchy; they found themselves at a lower level in the hierarchical culture of the hospital [40, 43]. Studies have reported that students fail to empathize with patients who are non-responsive because of hierarchical differences [24, 41]. Empathy is perceived as a cooperative process that necessitates the equal collaboration of both individuals [44]. Therefore, a lack of reciprocal response from complex, critical, insulting, or uncooperative patients can cause empathy decline in medical students.
Students identified language as the primary barrier in expressing empathy with patients. Researchers believe that the inability to understand the patient’s perspective or communicate the concerns due to the language barrier can cause failure to establish empathy [45]. Some students identified the unconducive local physical environment as a barrier to expressing empathy. Several studies have confirmed that in crowded clinics, students fail to express empathy with patients [16]. Empathy in clinical settings necessitates both endeavor and a conducive environment to achieve the best results [46].
Almost all the students agreed that they learned to empathize effectively with patients from positive and caring role models [41, 47]. They felt distressed when owing to a shortage of time, or otherwise, some consultants paid less attention to the emotive state of the patient. These findings are congruent with many studies [16, 24]. Inappropriate role models either invoke cautionary responses or enhance empathy erosion [48]. Nevertheless, most of the students appreciated the role of teachers in making them understand the value of empathy. They felt motivated to express better behavior with patients when encouraged by their teachers.
Students felt their curriculum emphasized mainly biomedical knowledge. They reported that the psychosocial aspects were never considered; teachers emphasized theoretical knowledge and clinical skills. These findings concur with several studies [24, 49, 50]. The greater emphasis on theoretical knowledge and high curriculum load demotivates students from engaging in bedside learning; hence, they fail to empathize with patients [16]. Like the results of some studies [40, 43], a few students noted that the pre- and para-clinical subjects were mainly theoretical. The lack of adequate patient contact in those years was a lost opportunity to learn empathic skills.
Some students, however, identified the interrelatedness of empathy with academic skills. They determined that an empathic expression without factual knowledge was a futile attempt to help patients. Studies have shown that empathy is essential for accurate diagnosis and effective management. Empathy enables physicians to understand more of a patient’s condition [27].
Students also described that they felt rushed and stressed during case presentations and examinations and preferred to spend less time with patients. Many researchers have described lack of time as a barrier to establishing empathic relations with patients [24, 40, 50]. Most of the students expressed that several personal factors influenced their empathic behavior. Some felt that the coping strategies learned during their childhood helped them to develop empathic expressions with patients. Literature supports these opinions; studies have shown that upbringing affects the development of empathy [51]. Students described that the workload, time constraints, burnout, sleep deprivation, examinations, and assessments made them feel stressed and less empathic. These results concur with the literature [30, 52]. Although transiently, mood changes affecting empathic behavior were also described by some students. Researchers suggest that to provide empathic care, students should be in a positive state of mind [53]. They should adopt effective personal-care strategies and resolve stress to maintain their physical and mental well-being [54].
Several researchers have reported a decline in medical students’ empathy during their undergraduate education [16, 17, 21, 55, 56]; however, our students noted that their empathic skills had improved with time. They agreed that they could improve their empathic skills through real patient encounters and positive role modelling by teachers. Some students attributed empathy development to the attainment of self-confidence and personal maturity. These results agree with reports of several qualitative studies that also noted an increase in medical students’ empathy [8, 18, 20].
Almost all the students felt that empathy could be enhanced by appropriate training. They suggested curricular changes and addressing the barriers to empathy. Students felt that empathy should be taught like a skill [24]. Relating the significance of communication skills in expressing empathy, students recommended that the institution should hold special workshops and seminars to improve their communication skills [57]. They suggested including role-playing in the training of students. Studies have reported improvement in the empathic skills of students through role-playing, case-based learning, problem-based learning, and simulations [24]. They also suggested including clinical scenarios to learn the practice of empathy in a stress-free environment [16]. However, some students felt that case-based presentations would promote the concept of patients as ‘cases and not human beings. Alternatively, they recommended introducing medical humanities in the curriculum [8, 58]. Some students felt that stories and narratives could also be used to train students. Students said they enjoyed listening to teachers’ personal experiences of dealing with patients.
Most of the students reported that the only way to promote genuine empathy could be by increasing contact hours with patients. They suggested early clinical exposure, extended hours in hospitals, and exposure to various patients. Students identified that they mainly developed empathy through real encounters with patients and that the other learning strategies were not significantly helpful [24].
Students talked about the assessment of empathic skills. They suggested that the assessment of empathic skills would motivate them to develop such skills. These views of students concur with some authors' opinions who recommended increasing the number of assessments of students’ empathic skills to counteract empathy decline in medical students [59].
Some students suggested that the institute should organize activities to destress students. Stress as a barrier to empathy has been reported by several studies [24, 50]. Students recommended conducting workshops on regulating negative emotions, handling demanding patients, and neutralizing the negative influences on stress and burnout on empathy in medical students [44].
Some students indicated that teachers should also be given training on enhancing empathy in medical students. They felt that teachers should be encouraged to treat students and patients empathically and respectfully [60]. They also suggested that teachers should model their behavior with patients accurately to motivate and inspire medical students [24].
Students identified language as one of the barriers to their empathic behavior with patients; therefore, they suggested including teaching the local language as a special module in the official curriculum.
Strengths and Limitations of the Study
Strengths
This research has identified several factors that hinder or facilitate empathic development in medical students. The study results will enable medical educators to plan evidence-based interventions to encourage empathy development in medical students.
Limitations
The opinions of medical educators regarding the influences on empathy development in medical students and their bedside behaviors could have been sought to gain a deeper understanding of empathy. In addition, large-scale, mixed-methods studies involving students and faculty might help explore empathy and its determinants in greater detail.
Conclusion
This study aimed to gain insight into medical students’ perspectives on the development and influences of empathy during their undergraduate training. The facilitators of empathy development are factors such as real encounters with patients, positive role-modelling and encouragement by teachers, self-confidence, personal maturity, and adequate time. At the same time, crowded clinics, the lower position in the hierarchical environment of the hospital, lack of proficiency in the local language, encounters with uncooperative and abusive patients, and negative role modelling by junior consultants hamper empathic expressions. Students’ views have illuminated several facets of the medical curricula that demand the attention of medical educators. Lack of formal teaching of empathy in the official curriculum, greater emphasis on biomedical aspects than psychosocial skills, lack of assessment of empathic skills, late clinical encounters with real patients, academic load, and negative role modelling by certain teachers are the institutional barriers to empathy development.
The contextual issues identified in this research need to be addressed. Interventions to improve empathy should include early patient contact, removing barriers, providing student support, and incorporating formal empathy training in the curriculum.
Recommendations for Future Research
Longitudinal studies investigating the impact of personal development, institutional culture, and workplace culture on the empathic behavior of medical students during their undergraduate training can be conducted. In addition, qualitative studies exploring patients’ experiences and perspectives on the empathic behavior of medical students can also help to conceptualize empathy from a broader perspective.
Acknowledgements
We are thankful to the twelve study participants for their patience, interest, and commitment to the research.
Author Contribution
Namrata Chhabra planned and conducted the study, analyzed and interpreted the data, and wrote the manuscript. Sahil Chhabra assisted in transcription, data analysis and interpretation, and developing the manuscript. All authors critically reviewed the manuscript and approved the final version. Elize Archer guided and supervised the study, reviewed the contents critically, assisted in analyzing and interpreting the data, and helped write the manuscript.
Declarations
Ethics Approval
The approval to conduct the study was obtained from the Institutional research ethics committee.
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Derksen F, Bensing J, Lagro-Janssen A. Effectiveness of empathy in general practice: a systematic review. Br J Gen Pract. 2013;63(606):e76–e84. doi: 10.3399/bjgp13X660814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Decety J, Fotopoulou A. Why empathy has a beneficial impact on others in medicine: unifying theories. Front Behav Neurosci. 2015;8:457. doi: 10.3389/fnbeh.2014.00457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Azim Majumder MA, Ojeh N, Rahman S, Sa B. Empathy in medical education: can 'kindness' be taught, learned, and assessed? Adv Hum Biol. 2020;10:38–40. [Google Scholar]
- 4.Halpern J. What is clinical empathy? J Gen Intern Med. 2003;18(8):670–674. doi: 10.1046/j.1525-1497.2003.21017.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gleichgerrcht E, Decety J. Empathy in clinical practice: how individual dispositions, gender and experience moderate empathic concern, burnout and emotional distress in physicians. PLoS One. 2013;8(4):e61526. [DOI] [PMC free article] [PubMed]
- 6.Halpern J. From idealized clinical empathy to empathic communication in medical care. Med Health Care Philos. 2014;17(2):301–311. doi: 10.1007/s11019-013-9510-4. [DOI] [PubMed] [Google Scholar]
- 7.Halpern J. Gathering the patient’s story and clinical empathy. Perm J. 2012;16(1):52–54. doi: 10.7812/tpp/11-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jeffrey D. Exploring empathy with medical students: a qualitative longitudinal phenomenological study [Ph.D. Thesis]. 2018. Edinburgh: University of Edinburgh.
- 9.Rakel DP, Hoeft TJ, Barrett BP, Chewning BA, Craig BM, Niu N. Practitioner empathy and the duration of the common cold. Fam Med. 2009;41(7):494–501. [PMC free article] [PubMed] [Google Scholar]
- 10.Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz C, Gonnella JS. Physicians’ empathy and clinical outcomes for diabetic patients. Acad Med. 2011;86(3):359–364. doi: 10.1097/ACM.0b013e3182086fe1. [DOI] [PubMed] [Google Scholar]
- 11.Ahrweiler F, Neumann M, Goldblatt H, Hahn EG, Scheffer C. Determinants of physician empathy during medical education: hypothetical conclusions from an exploratory qualitative survey of practicing physicians. BMC Med Educ. 2014;14:122. doi: 10.1186/1472-6920-14-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Samra R. Empathy and Burnout in Medicine—Acknowledging Risks and Opportunities. J Gen Intern Med. 2018;33:991–993. doi: 10.1007/s11606-018-4443-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.General Medical Council . Professional behaviour and fitness to practice: guidance for medical schools and their students. London: General Medical Council; Medical Schools Council; 2016. [Google Scholar]
- 14.Association of American Medical Colleges. Learning objectives for medical student education: guidelines for medical schools. Medical School Objectives Project, January 1998. Washington, DC: AAMC. [DOI] [PubMed]
- 15.O’Tuathaigh CMP, Nadhirah Idris A, Duggan E, Costa P, Costa MJ. Medical students’ empathy and attitudes towards professionalism: relationship with personality, specialty preference, and medical programme. PLoS ONE. 2019;14(5):e0215675. doi: 10.1371/journal.pone.0215675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pohontsch NJ, Stark A, Ehrhardt M, Kötter T, Scherer M. Influences on students' empathy in medical education: an exploratory interview study with medical students in their third and last year. BMC Med Educ. 2018;18(1):231. doi: 10.1186/s12909-018-1335-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Krishnasamy C, Ong SY, Loo ME, Thistlethwaite J. How does medical education affect empathy and compassion in medical students? A meta-ethnography: BEME Guide No. 57. Med Teach. 2019;41(11):1220–1231. doi: 10.1080/0142159X.2019.1630731. [DOI] [PubMed] [Google Scholar]
- 18.Costa P, Magalhães E, Costa MJ. A latent growth model suggests that the empathy of medical students does not decline over time. Adv Health Sci Educ Theory Pract. 2013;18(3):509–522. doi: 10.1007/s10459-012-9390-z. [DOI] [PubMed] [Google Scholar]
- 19.Paro HMS, Silveira PSP, Perotta B, Gannam S, Enns SC, Giaxa RRB, Bonito RF, Martins MA, TempskI PZ. Empathy among medical students: is there a relation with quality of life and burnout? PLoS ONE. 2014;9(4):e94133. doi: 10.1371/journal.pone.0094133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tavakol S, Dennick R, Tavakol M. Empathy in UK medical students: differences by gender, medical year and specialty interest. Educ Prim Care. 2011;22(5):297–303. doi: 10.1080/14739879.2011.11494022. [DOI] [PubMed] [Google Scholar]
- 21.Hojat M, Vergare MJ, Maxwell K, Brainard G, Herrine SK, Isenberg GA, Veloski J, Gonnella JS. The devil is in the third year: a longitudinal study of erosion of empathy in medical school. Acad Med. 2009;84(9):1182–1191. doi: 10.1097/ACM.0b013e3181b17e55. [DOI] [PubMed] [Google Scholar]
- 22.Pedersen R. Empathy development in medical education – a critical review. Med Teach. 2010;32(7):593–600. doi: 10.3109/01421590903544702. [DOI] [PubMed] [Google Scholar]
- 23.Hojat M, LaNoue M. Exploration, and confirmation of the latent variable structure of the Jefferson scale of empathy. Int J Med Educ. 2014;5:73–81. doi: 10.5116/ijme.533f.0c41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tavakol S, Dennick R, Tavakol M. Medical students’ understanding of empathy: a phenomenological study. Med Educ. 2012;46(3):306–316. doi: 10.1111/j.1365-2923.2011.04152.x. [DOI] [PubMed] [Google Scholar]
- 25.Hooker C. Understanding empathy: why phenomenology and hermeneutics can help medical education and practice. Med Health Care Philos. 2015;18(4):541–552. doi: 10.1007/s11019-015-9631-z. [DOI] [PubMed] [Google Scholar]
- 26.Smith KE, Norman GJ, Decety J. The complexity of empathy during medical school training: evidence for positive changes. Med Educ. 2017;51(11):1146–1159. doi: 10.1111/medu.13398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jeffrey D. A meta-ethnography of interview-based qualitative research studies on medical students’ views and experiences of empathy. Med Teach. 2016;38(12):1214–1220. doi: 10.1080/0142159X.2016.1210110. [DOI] [PubMed] [Google Scholar]
- 28.Sulzer SH, Feinstein NW, Wendland CL. Assessing empathy development in medical education: A systematic review. Med Educ. 2016;50(3):300–310. doi: 10.1111/medu.12806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Spatoula V, Panagopoulou E, Montgomery A. Does empathy change during undergraduate medical education? A meta-analysis. Med Teach. 2019;41(8):895–904. doi: 10.1080/0142159X.2019.1584275. [DOI] [PubMed] [Google Scholar]
- 30.Elayyan M, Rankin J, Chaarani MW. Factors affecting empathetic patient care behaviour among medical doctors and nurses: an integrative literature review. East Mediterr Health J. 2018;24(3):311–318. doi: 10.26719/2018.24.3.311. [DOI] [PubMed] [Google Scholar]
- 31.Vaismoradi M, Turunen H, Bondas T. Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nurs Health Sci. 2013;15(3):398–405. doi: 10.1111/nhs.12048. [DOI] [PubMed] [Google Scholar]
- 32.Sundler AJ, Lindberg E, Nilsson C, Palmér L. Qualitative thematic analysis based on descriptive phenomenology. Nurs Open. 2019;6(3):733–739. doi: 10.1002/nop2.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shrivastava S, Ramasamy J. Use of in-depth interviews in medical education research [letter to the editor] Muller J Med Sci Res. 2018;9(1):41–42. [Google Scholar]
- 34.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. [Google Scholar]
- 35.Ramani S, Mann K. Introducing medical educators to qualitative study design: twelve tips from inception to completion. Med Teach. 2016;38(5):456–463. doi: 10.3109/0142159X.2015.1035244. [DOI] [PubMed] [Google Scholar]
- 36.Sutton J, Austin Z. Qualitative research: data collection, analysis, and management. Can J Hosp Pharm. 2015;68(3):226–231. doi: 10.4212/cjhp.v68i3.1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tavakol M, Sandars J. Quantitative and qualitative methods in medical education research: AMEE Guide No. 90: Part I. Med Teach. 2014;36(9):746–756. doi: 10.3109/0142159X.2014.915298. [DOI] [PubMed] [Google Scholar]
- 38.O'Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245–1251. doi: 10.1097/ACM.0000000000000388. [DOI] [PubMed] [Google Scholar]
- 39.Stalmeijer RE, Mcnaughton N, Van Mook WN. Using focus groups in medical education research: AMEE Guide No. 91. Med Teach. 2014;36(11):923–939. doi: 10.3109/0142159X.2014.917165. [DOI] [PubMed] [Google Scholar]
- 40.Ratanawongsa N, Teherani A, Hauer KE. Third-year medical students’ experiences with dying patients during the internal medicine clerkship: a qualitative study of the informal curriculum. Acad Med. 2005;80(7):641–647. doi: 10.1097/00001888-200507000-00006. [DOI] [PubMed] [Google Scholar]
- 41.Cutler JL, Harding KJ, Mozian SA, Wright LL, Pica AG, Masters SR, Graham MJ. Discrediting the notion “working with ‘crazies’ will make you ‘crazy’”: addressing stigma and enhancing empathy in medical student education. Adv Health Sci Educ. 2009;14:487–502. doi: 10.1007/s10459-008-9132-4. [DOI] [PubMed] [Google Scholar]
- 42.Norfolk T, Birdi K, Walsh D. The role of empathy in establishing rapport in the consultation: a new model. Med Educ. 2007;41(7):690–697. doi: 10.1111/j.1365-2923.2007.02789.x. [DOI] [PubMed] [Google Scholar]
- 43.Lempp H, Seale C. The hidden curriculum in undergraduate medical education: qualitative study of medical students’ perceptions of teaching. Brit Med J. 2004;329(7469):770–773. doi: 10.1136/bmj.329.7469.770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Barrett-Lennard GT. The phases and focus of empathy. Br J Med Psychol. 1993;66(1):3–14. doi: 10.1111/j.2044-8341.1993.tb01722.x. [DOI] [PubMed] [Google Scholar]
- 45.Hashim MJ, Major S, Mirza DM, Prinsloo EA, Osman O, Amiri L, McLean M. Medical students learning communication skills in a second language: empathy and expectations. Sultan Qaboos Univ Med J. 2013;13(1):100–106. doi: 10.12816/0003202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Riess H. The impact of clinical empathy on patients and clinicians: understanding empathy's side effects. AJOB Neurosci. 2015;6(3):51–53. [Google Scholar]
- 47.Nogueira-Martins MC, Nogueira-Martins LA, Turato ER. Medical students’ perceptions of their learning about the doctor-patient relationship: a qualitative study. Med Educ. 2006;40(4):322–328. doi: 10.1111/j.1365-2929.2006.02411.x. [DOI] [PubMed] [Google Scholar]
- 48.Brazeau CM, Schroeder R, Rovi S, Boyd L. Relationships between medical student burnout, empathy, and professionalism climate. Acad Med. 2010;85(Suppl. 10):S33–36. doi: 10.1097/ACM.0b013e3181ed4c47. [DOI] [PubMed] [Google Scholar]
- 49.Michalec B. Learning to cure, but learning to care? Adv Health Sci Educ Theory Pract. 2011;16(1):109–130. doi: 10.1007/s10459-010-9249-0. [DOI] [PubMed] [Google Scholar]
- 50.Eikeland HL, Ørnes K, Finset A, Pedersen R. The physician's role and empathy – a qualitative study of third-year medical students. BMC Med Educ. 2014;14:165. doi: 10.1186/1472-6920-14-165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Neumann M, Edelhäuser F, Tauschel D, Fischer MR, Wirtz M, Woopen C, Haramati A, Scheffer C. Empathy decline and its reasons: a systematic review of studies with medical students and residents. Acad Med. 2011;86(8):996–1009. doi: 10.1097/ACM.0b013e318221e615. [DOI] [PubMed] [Google Scholar]
- 52.Bayne H, Neukrug E, Hays D, Britton B. A comprehensive model for optimizing empathy in person-centered care. Patient Educ Couns. 2013;93(2):209–215. doi: 10.1016/j.pec.2013.05.016. [DOI] [PubMed] [Google Scholar]
- 53.Zenasni F, Boujut E, Woerner A, Sultan S. Burnout and empathy in primary care: three hypotheses. Br J Gen Pract. 2012;62(600):346–347. doi: 10.3399/bjgp12X652193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kerasidou A, Horn R. Making space for empathy: Supporting doctors in the emotional labour of clinical care. BMC Med Ethics. 2016;17(1):1–5. doi: 10.1186/s12910-016-0091-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hamed OA, Alahwal AM, Basri AH, Bukhari BM. Personal, cultural, and academic factors affecting empathy score in third-year medical students. Int J Educ Res. 2015;3(3):727–740. [Google Scholar]
- 56.Costa P, de Carvalho-Filho MA, Schweller M, Thiemann P, Salgueira A, Benson J, Costa MJ, Quince T. Measuring medical students’ empathy: exploring the underlying constructs of and associations between two widely used self-report instruments in five countries. Acad Med. 2017;92(6):860–867. doi: 10.1097/ACM.0000000000001449. [DOI] [PubMed] [Google Scholar]
- 57.Bayne HB. Training medical students in empathic communication. J Spec Group Work. 2011;36(4):316–329. [Google Scholar]
- 58.Batt-Rawden SA, Chisolm M, Anton B, Flickinger TE. Teaching empathy to medical students: an updated, systematic review. Acad Med. 2013;88(8):1171–1177. doi: 10.1097/ACM.0b013e318299f3e3. [DOI] [PubMed] [Google Scholar]
- 59.Larsen DP, Butler AC, Lawson AL, Roediger HL. The importance of seeing the patient: Test-enhanced learning with standardized patients and written tests improves clinical application of knowledge. Adv Health Sci Educ Theory Pract. 2013;18(3):409–425. doi: 10.1007/s10459-012-9379-7. [DOI] [PubMed] [Google Scholar]
- 60.Halpern J. Empathy and patient-physician conflicts. J Gen Intern Med. 2007;22(5):696–700. doi: 10.1007/s11606-006-0102-3. [DOI] [PMC free article] [PubMed] [Google Scholar]