Abstract
The creation of developmentally appropriate and meaningfully complex clinical reasoning exercises in the pre-clerkship curriculum is a common challenge for many medical schools. We provide an overview of one component of the pre-clerkship clinical reasoning curriculum at Case Western Reserve University School of Medicine, and present evidence that inclusion of Health Systems Science in this exercise facilitates integrated thinking in a Problem-Based Learning curriculum.
Keywords: Problem-Based Learning (PBL), Health Systems Science (HSS), Social Determinants of Health (SDH), Clinical reasoning pre-clerkship education
Background
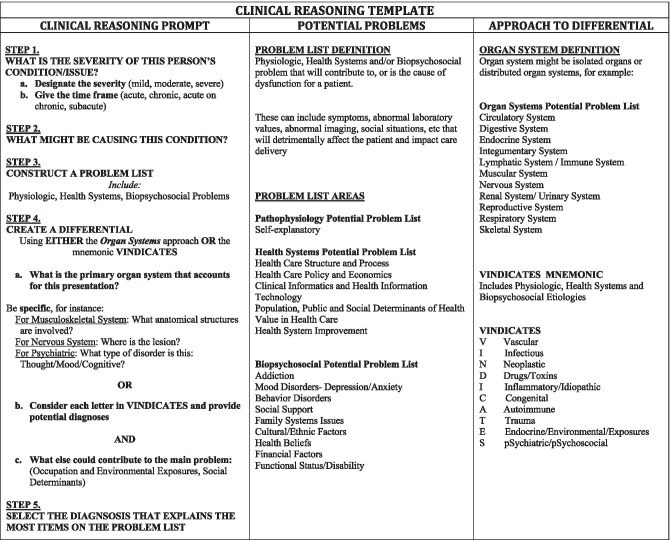
The Western Reserve2 (WR2) Curriculum at Case Western Reserve University School of Medicine (CWRU SOM) features Problem-Based Learning (PBL) as a primary learning approach during the pre-clerkship phase [1, 2]. The curriculum introduces health promotion and population health as a foundation for understanding the pathophysiology of medicine [3]. An important feature of the pre-clerkship curriculum is a pedagogical approach that intertwines basic, clinical, and health systems sciences throughout the educational program. To formally address the curricular challenge of teaching pre-clerkship clinical reasoning skills [4, 5], we created and implemented a developmentally appropriate [6] and increasingly advancing template that provides a scaffold, including basic science and health systems science (HSS), upon which students can build their clinical reasoning (Fig. 1).
Fig. 1.
Prompting questions that guide the development of clinical reasoning skills and the scaffolding upon which students build differentials
Activity
Starting in the early months of the pre-clerkship curriculum, students initially are presented with only the introductory paragraph of the PBL case, including the presenting complaint and basic background of a patient. Students are then asked to determine the severity and acuity of the patient’s presenting concern, (Step 1; Fig. 1) and what might be the potential cause for their condition (Step 2; Fig. 1). In particular, when discussing potential causes, students are prompted to consider occupational exposures, environmental triggers, and social determinants of health (SDH) [7]. As the students proceed through the curriculum, after completing the first part of the exercise, they add the creation of a problem list (Step 2; Fig. 1). Students are encouraged to be comprehensive and include problems using the following constructs: physiologic, health systems science, and biopsychosocial issues (Fig. 1).
During the second half of the pre-clerkship curriculum, students complete the first parts of the exercise (Steps 1, 2, 3; Fig. 1) and also practice different methods of creating a differential diagnosis for the PBL cases (Step 4 a, b; Fig. 1). They are first asked to use the problem list (Step 3; Fig. 1) to create an organ systems approach (Step 4a; Fig. 1) to understanding the patient’s condition. Later, they are given the mnemonic VINDICATES (Step 4b; Fig. 1) to help elaborate their working differential. In the final months of their pre-clerkship training, they are given the opportunity to choose between the two approaches to create differential diagnoses. The Clinical Reasoning Template provides a framework for students to organize their thinking.
Students are trained in the use of the Clinical Reasoning Template early in the curriculum and at four subsequent times throughout their pre-clerkship curriculum so that they receive stepwise preparation equipping them to approach the increasing complexity of the PBL clinical reasoning exercise [8]. These training sessions are recorded so that students have ongoing access to the instructional lectures that explain the use of this tool. PBL facilitators are similarly trained using this tool and are provided with sample responses, with the expectation that facilitators will guide students as they grapple with the probing questions of the tool.
Given the importance of health systems science in clinical care, we have integrated topics from the six AMA Health Systems Science core domains [9] into our Clinical Reasoning Template. These core domains are as follows: (1) Health Care Structures and Processes, (2) Health Care Policy and Economics, (3) Clinical Informatics and Health Information Technology, (4) Population, Public, and Social Determinants of Health, (5) Value in Health Care, and 6) Health System Improvement (Fig. 1). This early inclusion of HSS as part of clinical thinking is designed to set the stage for the more developmentally mature reasoning that students will need to demonstrate during core clinical rotations.
Because of the emphasis on health systems science in our curriculum, we were interested whether this template created a “habit of mind” of including HSS issues on the problem lists students created for PBL cases. The CWRU PBL curriculum consists of 94 cases over the course of the 2-year curriculum. Our study focused on the 21 PBL cases in the Homeostasis Block of the curriculum (Cardiovascular, Pulmonary, Renal, Cell Physiology, Principles of Pharmacology, and Bio-Ethics) that spans the last 4 months of the first year. All the students in their first year of medical school participated in the use of this clinical reasoning template. The CWRU Institutional Review Board deemed this study EXEMPT. The response rate of the PBL student groups varied from 68 to 91% depending upon the case. We scored the problem lists generated by students to quantify the frequency of inclusion of problems which would fall into one of the six HSS core domains. Faculty with HSS content expertise (MKS and ARS) reviewed the same cases and similarly delineated within which cases there were HSS issues. Faculty and student results were then compared.
Results and Discussion
The overall frequency with which respondents identified HSS as a problem was 88/357 or 25% of possible identifications for PBL cases included in the study. One or more student groups identified HSS issues in 85.7% of PBL cases (18/21). Table 1 describes the percentage of total cases identified as having issues that fell within each HSS core domain. Upon review by faculty, similar numbers of cases were identified as having problems that fell within each specific HSS core domain. Although the student to expert comparison did not yield exact case matches in all domains, it is striking that within the Health Care Structures and Process domain, faculty and student problem identification did match exactly.
Table 1.
Percentage of PBL cases with identified with HSS Domains
|
Health Systems Science Domain |
Raw number of cases identified by students (of 21) | Percentage of cases identified by students | Raw number of cases identified by HSS faculty (of 21) | Percentage of cases identified by HSS faculty |
|---|---|---|---|---|
| Health Care Structure and Process | 10 | 47.62% | 10 | 47.62% |
| Health Care Policy and Economics | 0 | 0% | 0 | 0% |
| Clinical Informatics and Health Information Technology | 1 | 4.76% | 2 | 9.52% |
| Population, Public, and Social Determinants of Health | 17 | 80.95% | 14 | 66.67% |
| Value in Health Care | 1 | 4.76% | 0 | 0% |
| Health System Improvement | 1 | 4.76% | 2 | 9.52% |
Students more readily identified problems within the Population, Public, and Social Determinants of Health domain than did faculty (81% compared to 67%) and were less likely to identify problems in the Clinical Informatics and Health Information Technology, and the Health System Improvement domains (4.76% vs. 9.52%). The Health Care Policy and Economics domain was not represented on any of the problem lists created by students and faculty alike.
It is notable that students included HSS issues on the problem list with no specific intent on our part to add explicit HSS learning objectives to any of the PBL cases. The primary focus of each PBL case is the underlying mechanism of disease, as such health care delivery problems are not typically written into the opening paragraph of any case. This study suggests that PBL can aid in teaching and reinforcing HSS thinking when students have been primed to consider these issues (see Fig. 1). Use of the tool provided in Fig. 1 may offer the opportunity to identify HSS issues in any PBL case or patient-based vignette.
In reviewing the first paragraph (initial patient presentation) of each PBL case, we identified three cases in which HSS concerns were very obvious to the students. In the remaining eighteen cases, HSS topics were not as obvious. Table 2 shows example opening paragraphs from four distinct cases, along with the notation of whether HSS domains were identified by students and faculty. It appears minimal narrative prompting was required to activate students to think about HSS issues in the context of a PBL case opening paragraph.
Table 2.
Examples of PBL case verbiage leading to identification of Health Systems Science Domains
| Cases where HSS issues identified on student problem list | Cases where HSS issues NOT identified on student problem list | |
|---|---|---|
|
Acuity of complaint: SUB-ACUTE |
Maria Gomez is a 67-year-old woman who presented to her primary care physician with 2 months of progressive dyspnea on exertion and 2 days of nocturnal dyspnea. Spanish is her primary languagei but speaks English well enough to function on her own | Ann Neiman is a 54-year-old woman with a past medical history significant for borderline hypertension, chronic anemia, and heavy cigarette smoking. She has been seen by her primary care physicianii for a 2-month history of coughing up blood-streaked sputum (hemoptysis). She notes progressive shortness of breath, decreased appetite, and a 10-lb weight loss over the last month |
| Identified by student |
HSS Domain: iPopulation, Public, and Social Determinants of Health |
HSS Domain: None |
| Identified by faculty |
HSS Domain: iPopulation, Public, and Social Determinants of Health |
HSS Domain: iiHealth Care Structure and Process |
|
Acuity of complaint: ACUTE ON CHRONIC |
James Randolph is a 45-year-old male with a 15-year history of type 2 diabetesi. He goes to see a new primary care doctor, Dr. Sick, because of “frothy” urine. Mr. Randolph is not regularly screenedii, iii for complications of diabetes; but 5 years ago he visited a clinic and tested negative for microalbuminuriaiv | Bernice Matthews is a 61-year-old woman admitted to the general medicine service for vomiting and diarrhea. She was in her usual state of health until 2 days ago when she began to complain of nausea, which rapidly developed into frequent vomiting and diarrhea several times a day. She has been unable to keep anything down and is now lightheaded and too weak to walk without help |
| Identified by student |
HSS Domain: iiHealth Care Structure and Process |
HSS Domain: None |
| Identified by faculty |
HSS Domains: iPopulation, Public, and Social Determinants of Health iiHealth Care Structure and Process iiiHealth System Improvement ivValue in Health Care |
HSS Domain: None |
Notably, simply mentioning English as a second language, and the lack of regular screening was sufficient for our students to extrapolate the potential presence of health care delivery concerns and include such issues on their problem list. Two of the cases that were not identified by students as having any HSS domains are noted above in Table 2. When reviewed by our HSS Faculty, one of these cases did indeed have an HSS domain that could be identified. It is possible that this was not, however, picked up by the students because the HSS domain was actually a protective factor for the patient. We presume this case was not identified because our students consider gaps in care and do not focus on HSS protective factors when compiling problem lists. In the other case, HSS faculty agreed with students that the initial paragraph did not indicate any issues that could be perceived as pertaining to HSS domains.
Using this tool in our curriculum, we were successful in making students explicitly list HSS issues as clinical concerns that require consideration. In trying to understand why CWRU students readily include HSS in the problem list, it is important to distinguish that these students are longitudinally taught public health and HSS issues beginning early in medical school during their first 5-week course called “Becoming a Doctor” that emphasizes HSS, with specific attention to the Health Care Structures and Processes domain [10]. It is likely that students emphasized inclusion of Health Care Structures and Processes, and Population, Public, and Social Determinants of Health in their choice of HSS domains more frequently than did our HSS faculty because of the early and immersive emphasis on these HSS domains in our curriculum. Many of the other HSS domains are more extensively explored when students reach their clerkships. Finally, it would be interesting to assess HSS inclusion in clinical thinking as students progress through the rest of the CWRU curriculum, to see whether they include a wider variety of HSS domains as they advance in their training.
From our findings, it appears that early exposure to HSS may sensitize students to consider potential issues of health care delivery, even when these are not the explicit intended educational focus. Given the increasing inclusion of HSS in pre-clerkship US medical school curricula, we suggest that this tool may be of use for other schools that utilize PBL or other forms of case-based learning. We believe that inclusion of HSS as part of a clinical reasoning exercise can allow students to answer the call to build broad and holistic problem lists [11] and demonstrate the beginnings of integrated clinical reasoning.
Declarations
Ethical Approval
The CWRU Institutional Review Board (IRB) deemed the above protocol EXEMPT under 45 Code of Federal Regulations (CFR) part 46.101(b)(1). The IRB protocol number is IRB-2015–1105.
Informed Consent
Not applicable.
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Neville AJ, Norman GR. PBL in the Undergraduate MD Program at McMaster University: three iterations in three decades. Acad Med. 2007;82(4):370–374. doi: 10.1097/ACM.0b013e318033385d. [DOI] [PubMed] [Google Scholar]
- 2.Margolius SW, Papp KK, Altose MD, Wilson-Delfosse AL. Students perceive skills learned in pre-clerkship PBL valuable in core clinical rotations. Med Teach. 2020 doi: 10.1080/0142159X.2020.1762031. [DOI] [PubMed] [Google Scholar]
- 3.Wolpaw TM, Hull Al, Wilson-Delfosse AL, Dannefer EF, Wolpaw DR, Isaacson JH, Papp KK, Bierer SB, Ornt DB. Case Western Reserve University School of Medicine and Cleveland Clinic. Acad Med. 2010;85(9S);S439–45. 10.1097/ACM.0b013e3181ea37d6. [DOI] [PubMed]
- 4.Keemink Y, Custers EJFM, van Dijk S, Ten Cate O. Illness script development in pre-clinical education through case-based clinical reasoning training. Int J Med Educ. 2018;9:35–41. Published 9 Feb 2018. 10.5116/ijme.5a5b.24a9. [DOI] [PMC free article] [PubMed]
- 5.Kelekar A, Afonso N. Evaluation of the effect of a new clinical reasoning curriculum in a pre-clerkship clinical skills course. Perspectives Medical Education. 2020;9(2):123–127. doi: 10.1007/s40037-020-00566-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kassirer JP. Teaching clinical reasoning: case-based and coached. Acad Med. 2010;85(7):1118–1124. doi: 10.1097/acm.0b013e3181d5dd0d. [DOI] [PubMed] [Google Scholar]
- 7.Mangold KA, Bartell TR, Doobat-Persaud AA, Adler MD, Sheehan KM. Expert consensus on inclusion of the social determinants of health in undergraduate medical education curricula. Acad Med. 2019;94:1355–1360. doi: 10.1097/ACM.0000000000002593. [DOI] [PubMed] [Google Scholar]
- 8.Schmidt HG, Mamede S. How to improve the teaching of clinical reasoning: a narrative review and a proposal. Med Educ. 2015;49:961–973. doi: 10.1111/medu.12775. [DOI] [PubMed] [Google Scholar]
- 9.Gonzalo JD, Dekhtyar M, Starr SR, Borkan J, Brunett P, Fancher T, Green J, Grethlein SJ, Lai C, Lawson L, Monrad S, O'Sullivan P, Schwartz MD, Skochelak S. Health systems science curricula in undergraduate medical education: identifying and defining a potential curricular framework. Acad Med. 2017;92(1):123–131. doi: 10.1097/ACM.0000000000001177. [DOI] [PubMed] [Google Scholar]
- 10.Ornt DB, Aron DC, King NB, Clementz LM, Frank S, Wolpaw T, Wilson-Delfosse A, Wolpaw D, Allan TM, Carroll M, Thompson-Shaheen K, Altose MD, Horwitz. RI. Population medicine in a curricular revision at Case Western Reserve. Acad Med. 2008;83:327–331. 10.1097/ACM.0b013e318166ab8a. [DOI] [PubMed]
- 11.Borkan JM, Hammoud MM, Nelson E, Oyler J, Lawson L, Starr SR, Gonzalo JD. Health systems science education: the new post-Flexner professionalism for the 21st century. Med Teach. 2021;43(sup2):S25–S31. doi: 10.1080/0142159X.2021.1924366. [DOI] [PubMed] [Google Scholar]