Abstract
Panchgavya represents milk, urine, dung, ghee, and curd, derived from cow and serves irreplaceable medicinal importance in Ayurveda and traditional Indian clinical practices. In Ayurveda,Panchgavya treatment is termed as ‘Cowpathy’. In India, the cow is worshipped as a god called ‘Gaumata,’ indicating its nourishing nature like a mother. Ayurveda recommends Panchagavya to treat diseases of multiple systems, including severe conditions, with almost no side-effects. It can help build a healthy population, alternative sources of energy, complete nutritional requirements, eradicate poverty, pollution-free environment, organic farming, etc. Panchgavya can also give back to mother nature by promoting soil fertility, earthworm production, protecting crops from bacterial and fungal infections, etc. Scientific efforts shall be taken to build evidence for the clinical application of Cowpathy. The present review aims to summarize the health and medicinal benefits of Panchgavya.
Keywords: Ayurveda, Cowpathy, Cow products, Indian cow, Panchgavya
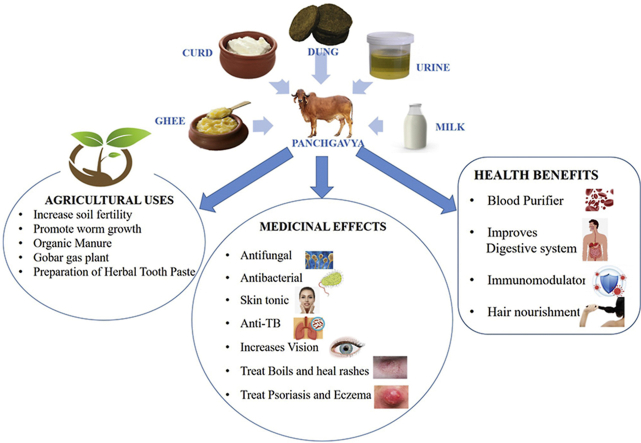
Graphical abstract
1. Introduction
India is the land of traditions with its roots in ancient science directly linking social rituals and scientific reasons behind them. In India, a cow is called ‘Gaumata’ or ‘Kamadhenu’ due to its nourishing nature like a mother [1]. Kamadhenu is the name of the sacred cow who believed to accomplish desired things. Panchgavya is a treasure of health benefits and medicinal properties. The Ayurvedic system of medicine has described the significance of using cow milk, ghee, urine, dung, and curd, each of which is termed ‘gavya’ (i.e., obtained from ‘Gau’ means cow) for the treatment of various diseases. Each product possesses different components and uses for human health, agriculture, and other purposes. ‘Panchgavya’ has been derived from two words, ‘Panch’ meaning five and ‘gavya’ meaning obtained from ‘Gau’ means cow [2], which in-toto represents five products obtained from a cow (Fig. 1). Each of the ‘gavya’ exerts a different medicinal impact against various diseases. Panchgavya therapy or treatment is called ‘Cowpathy’, similar to other pathies (allopathy, homeopathy, and naturopathy). Each ‘gavya’ can be used as a single therapy or in combination with other products or with other treatments. Also, all five products can be used alone or combined or any other synthetic, herbal, or mineral origin [3,4].
Fig. 1.
Components of Panchgavya
Panchgavya therapy is recommended for a variety of diseases viz., asthma, flu, allergies, cardiovascular diseases, renal disorders, rheumatoid arthritis, leucoderma, wound healing, leucorrhoea, hepatitis, dietary and gastrointestinal tract disorders, obesity, tuberculosis, ulcer, chemical intoxication, other bacterial, fungal and viral infections. The therapy has also demonstrated its therapeutic potential against severe pathological conditions like cancer, AIDS, and diabetes [2,5,6].
Panchgavya plays a crucial role in organic farming practices as the most favourable organic manure for agricultural fields. Its application ensures zero usage of harmful synthetic fertilizers, pesticides, insecticides, and antibiotics. No other manure can be as cost-effective and beneficial as Panchgavya. It can enhance soil fertility, improve the quality of earthworms, and promote crop health by acting as an organic fertilizer. Additionally, cow dung and cow urine are excellent sources of energy to generate biogas and electricity [2,7,8].
Traditional Indian literature cites numerous medicinal effects of Panchgavya; however, scientific evidence supporting ancient literature is very little. Scientific Validation and Research on Panchgavya (SVAROP) is a national program announced by the Ministry of Science and Technology, Government of India, for scientific validation of Panchgavya products. The program includes studies on the activity, efficacy, safety profile, toxicity, and acceptability of Panchgavya and other products obtained from the cow. The present review focuses on the composition of each Panchgavya product and its health benefits and medicinal properties based on available scientific evidence [9,10].
2. Cow-derived products
2.1. Curd
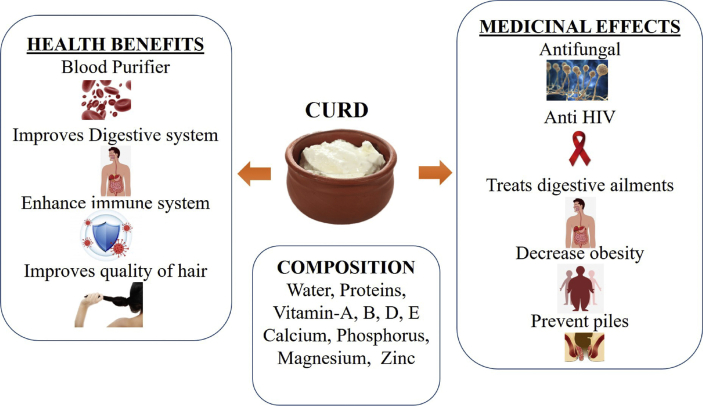
Curd also called ‘yogurt’ or “Dahi”, is consumed worldwide due to its high nutritional value and health benefits. It is prepared by fermenting cow milk using micro-organisms viz., Streptococcus, Acidophilus, and Lactobacillus [11]. Curd is a rich source of probiotics (beneficial living micro-organisms) that exert various beneficial effects upon oral administration. Lactic acid-producing bacteria form metabolites like cyclic dipeptides, phenyl lactic acid, and anti-fungal effects. These bacteria also include proteinous compounds in nature and a 3-hydroxylated fatty acid [2,5]. Ayurveda prescribes certain precautions carefully considering the health of an individual, environmental and climatic conditions for consumption of curd.
Curd contains several nutrients and micronutrients, including water, proteins, vitamins like A, B, D, and E; minerals like calcium, phosphorous, magnesium, zinc, etc. Probiotics present in curd help in strengthening the immune system and digestive system, whereas various minerals, vitamins, and proteins in curd help fight against multiple pathogens, including HIV [11]. It is used to treat digestive ailments as it can resist the growth of harmful micro-organisms and promote good gut flora to improve digestion [5]. Curd also acts as a blood purifier [12] and helps in lowering the total cholesterol, and low-density lipoproteins, thus, preventing the risk of obesity [13], anti-fungal effect for treating dandruff from hair [11], and treating piles [14]. Curd should be taken with green gram or moong for Vata Prakruti, sugar for Pitta Prakruti, and cumin powder for Kapha Prakruti individuals. Curd consumption with all the recommended precautions prescribed by Ayurveda may significantly benefit health [15]. The composition of curd, its health benefits, and its medicinal effects are depicted in Fig. 2.
Fig. 2.
Composition and uses of cow curd. TB: Tuberculosis; HIV: Human Immunodeficiency Virus.
2.2. Cow dung
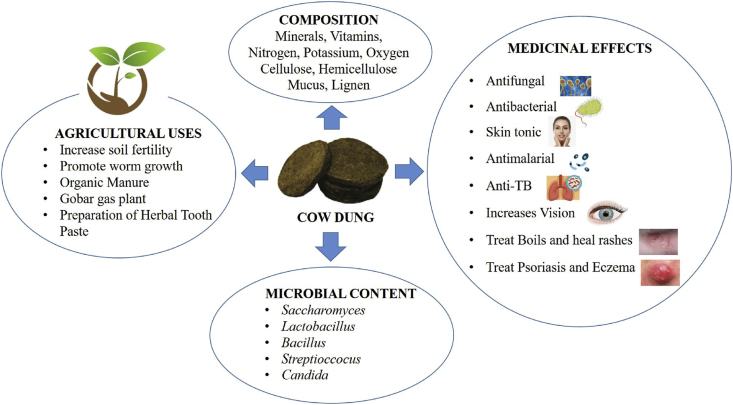
Cow dung is rich in several beneficial microbes like Saccharomyces, Lactobacillus, Bacillus, Streptococcus, Candida, etc. It also contains various nutritional components, including minerals, vitamins, potassium, nitrogen, oxygen, carbon, cellulose, hemicellulose, mucus, lignin. Cow dung is used to degrade waste generated from the city and hospitals due to the abundance of different micro-organisms beneficial for waste degradation [16].
In rural areas of India, a dried cow dung cake is used as a source of energy for cooking food, decreasing the dependency on other sources of energy and is entirely environment-friendly [17], and ensures air purification by killing the microbes in the surrounding air. ‘Gobar’ gas (biogas) plants also serve as a significant energy source. They convert cow dung into methane gas, which is used as a source of energy for cooking and generation of electricity [2]. Furthermore, the remaining residue is the best organic manure after converting most cow dung into methane gas.
Fibrous material obtained from cow dung is used for the preparation of papers [17]. Recently, cow dung-based mosquito repellents have been among the best alternatives for synthetic mosquito repellants [18]. Also, cow dung-based toothpaste protects against oral pathogens and improves oral health. The use of cow dung ensures more environment-friendly and cost-effective human activities [5,[19], [20], [21]].
The use of cow dung in agriculture is essential to maintain soil quality. Cow dung helps increase the population of earthworms, and also promotes and manages fertile soil with the presence of Eisenia andrei species of earthworm, showing an enhancement in the nitrification process [22]. Fungal diseases are among the major problem in agricultural fields. The use of cow dung can restrict the development of such fungal issues due to Fusarium oxysporum, Fusarium solani, and Sclerotinia sclerotiorum [23]. The use of pesticides, fertilizers, weedicides, and antibiotics in farming practices is hazardous to humans and animals, and leads to severe diseases such as immunosuppression, hypersensitivity reaction, and auto-immune disorders. Therefore, products obtained from organic farming have more demand as organic farming practices are devoid of harmful chemicals for crop production. High microbial count and nutritional value led the cow dung as manure for farming practices in organic farms. Cow dung serves as the best replacement for these chemicals and ensures human and animal health [[24], [25], [26]].
Cow dung has also demonstrated anti-bacterial and anti-fungal effects [2]. It serves as a skin tonic and is found effective in treating psoriasis and eczema. The mixtures of crushed neem leaves and cow dung helps against boils and heat rashes. Cow dung has demonstrated that it can kill the malarial parasite and Mycobacterium tuberculosis. The anti-fungal activity can be observed against Corprophilous fungi [20,21]. Smoke liberated on burning of cow dung causes eye irritation and tears, which can help vision enhancement [27]. The composition of cow dung, along with its uses, is summarized in Fig. 3.
Fig. 3.
Composition, health benefits, and medicinal effects of dung.
2.3. Cow ghee
Cow ghee prepared by traditional method possesses high nutritional value, medicinal benefits, and helps to promote good health. Ghee is prepared by heating the butter obtained from cow milk, and heating must be continued at high temperature until the moisture is completely lost [28].
2.3.1. Traditional methods of ghee preparation
Ghee can be prepared using four different methods and are explained as follows:
2.3.1.1. Method 1: Preparation of creamery butter ghee
In this method, cream from the milk is separated and stored to obtain the desired acidity. This cream is then churned to get the butter. After churning, buttermilk and creamery butter are separated. The butter is then heated at the desired temperature, and molten ghee is obtained. The ghee is then decanted and filled in containers [29].
2.3.1.2. Method 2: Preparation of desi ghee
The milk is first boiled, cooled at room temperature, followed by the addition of lactic acid culture and incubation for 10 to 16 h to prepare curd. Water is added to the curd and churned to obtained the butter called ‘desi butter’. The butter is heated at the desired temperature, and molten desi ghee is obtained. The ghee must be decanted while hot and filled in a container [30].
2.3.1.3. Method 3: Preparation of ghee directly from cream
Cream from milk is separated and heated to remove the moisture by maintaining the desired temperature. Molten ghee is obtained, allowed to settle, further decanted, and stored in containers [29].
2.3.1.4. Method 4: Preparation of ghee by pre-stratification
In this method, milk is processed to obtain creamery butter or desi butter. Butter is then heated at about 80 °C and allow to stand for 30 min. The bottom layer is discarded, and the remaining material is heated at the desired temperature to obtain the ghee. Molten ghee obtained must be decanted hot and filled in a container [31].
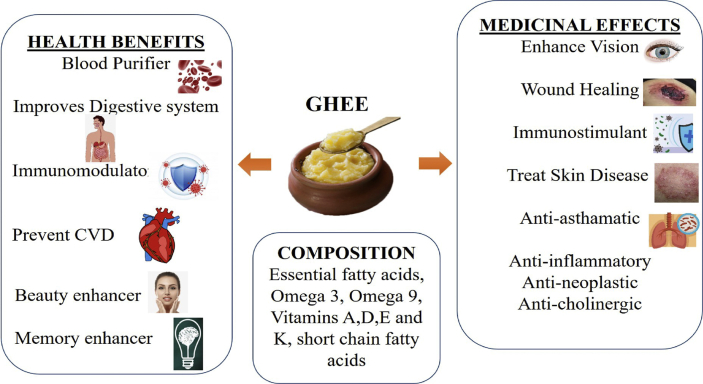
Ghee prepared using milk obtained from ‘deshi’ cow or Indian breed is more beneficial for health than ghee obtained from the milk of other exotic cow species. Due to ghee's high fatty acid content, people believed that ghee consumption could increase the risk of dyslipidemia and cause cardiovascular diseases. Such beliefs were responsible for the widespread avoidance of ghee in India [32]. Even though Ayurveda has given enormous benefits of consuming ghee, various scientific studies were conducted, and ghee's health benefits were re-established [33,34]. In the Ayurvedic system of medicine, ghee plays a vital role, both as a vehicle to deliver the active constituent and a base for incorporating active components to formulate the dosage forms. Ayurveda also supports the co-administration of ghee along with other remedial treatments. Ghee-based formulations, i.e., Ghrita, are developed for targeted delivery and enhanced bioavailability of hydrophobic botanicals. For example, Brahmi ghrita for cognitive function; Vasa ghrita for the respiratory system; Shatadhauta ghrita for skin diseases, Bhallatakadi ghrita for wound healing and Kaamdev ghrita for sexual disorders, etc. [[35], [36], [37], [38]]., Saleem et al. have performed molecular characterization studies on desi ghee. The study revealed that desi ghee is a rich source of essential fatty acids (omega 3 and omega 9), vitamins like A, D, E, and K [39]. The health benefits of cow ghee are memory enhancement, lowering bad cholesterol, preventing skin and cardiovascular diseases, promoting skin health, maintaining the digestion process, generating energy, purifying the blood, protecting the liver, etc. [35]. Ghee has demonstrated various medicinal properties such as anti-inflammatory, antineoplastic, vision enhancing, and fasten wound healing [40,41]. It helps treat skin and gastrointestinal diseases and has beneficial effects, including immunostimulant, anti-cholinergic activity, anti-asthmatic effect, helps against paralysis, etc. [12,17]. The composition, health benefits, and medicinal potential of cow ghee are shown in Fig. 4.
Fig. 4.
Composition, health benefits, and medicinal effects of cow ghee. CVD: Cardiovascular diseases.
2.4. Cow urine
Cow urine or “Gaumutra” is a non-toxic liquid waste discharged from the cow. Cow urine or its distillate is known to have several health benefits to improve the quality of life and prolong survival rates in patients with severe diseases [42]. When the Council of Scientific and Industrial Research (CSIR), India, and other scientists in India demonstrated antineoplastic, anti-fungal, antibiotic, and bio-enhancing effects of cow urine distillate, the modern world started to believe in the medicinal properties of cow urine [35,43]. A wide range of medicinal uses of cow urine is already in the public domain, but scientific data is minimal to support its consumption. More such studies shall be carried out to promote the traditional methods of treatment having less severe side-effects.
In the Ayurvedic system of medicine, cow urine is used for the preparation of several formulations. Numerous health benefits and medicinal effects of cow urine are revealed in the textbooks of Ayurveda. Cow urine is known to induce diuretic action and also acts as a nephroprotective agent. It can also help in weight loss, digestive issues, edema, reversal effect against various cardiovascular and kidney diseases [6]. It can also treat diarrhea, GIT infections, jaundice, piles, anemias, and skin diseases like vitiligo. Indian literature has described numerous benefits of cow urine, but supporting scientific evidence is missing [44,45].
2.4.1. Cow urine composition and their medicinal effects
Cow urine contains 95% water, 2.5% of urea, and the rest 2.5% include components like enzymes, hormones, salts, and minerals [46]. Various components of cow urine and its uses are described in Table 1.
Table 1.
Composition and medicinal effects of cow urine.
| Constituent | Formula | Health benefits and medicinal effects |
|---|---|---|
| Iron | Fe | Formation of RBCs and hemoglobin |
| Calcium | Ca | Blood purification; maintains bone strength |
| Copper | Cu | Prevent deposition of fats |
| Phosphate | P | Prevent formation of stones in the urinary tract |
| Manganese | Mn | Germicidal effects; prevent gangrene |
| Potassium | K | Increase appetite; reduce muscle weakness; cures hereditary rheumatism. |
| Sulphur | S | Blood cleanser; improve bowel movement |
| Nitrogen | N2, NH2 | Regulates kidney function; prevent abnormalities in the blood; diuresis |
| Sodium | Na | Blood purification; antacid |
| Ammonia | NH3 | Enhance blood formation; maintains bile and mucus |
| Carbolic acid | HCOOH | Germicidal effects; prevent gangrene |
| Aurum Hydroxide | AuOH | Improves immunity system; antibiotic; anti-toxic |
| Creatinine | C4HgN2O2 | Germicidal action |
| Hipuric acid | Helps in the excretion of toxins in urine | |
| Lactose | C6H12O6 | Reduce nervousness; strengthen the heart |
| Urea | CO(NH2)2 | Increase urine formation; germicidal effect |
| Uric Acid | C5H4N4O3 | Diuretic effect; help to maintain good heart health |
| Water | H2O | Maintains fluidity of blood and body temperature |
Besides this, cow urine also contains various enzymes to improve the digestive system and build a robust immune system. Vitamins including A, B, C, D, and E are also present in cow urine [43].
2.5. Cow milk
Traditional Indian systems of medicine had described the medicinal effects of cow milk in ancient literature. Milk is used for its health-protecting, health-promoting, and wide range of therapeutic effects [47]. Indian breed of cows delivers A2 type of milk, whereas A1 type of milk is given by crossbreed or exotic cow species. A1 type of milk contains a devil constituent, i.e., b-casomorphin-7 (BCM-7), a seven-membered peptide obtained from Bos taurus cow, particularly HeF cows. BCM-7 is a digestive by-product of beta-casein generated due to substituting a proline residue by histidine in polypeptide chains. BCM-7 has several adverse effects on the body. In patients with the leaky gut syndrome, BCM-7 in the bloodstream can cause schizophrenia and atherosclerosis. In nursing infants, it can cause type-1 diabetes and autism due to binding BCM-7 with opioid receptors and inhibiting endorphins' normal binding and function. Endorphins cannot perform their function, leading to autism in infants and schizophrenia in adults. Activation of opioid receptors by BCM-7 also causes damages to the immune system and leads to type-1 diabetes. Consumption of A1 milk also causes asthma, heart diseases, and allergic reactions [48].
On the other hand, milk obtained from the Indian cow breed is an A2 type of milk with numerous benefits on human health and various medicinal activities. In Ayurveda, a traditional practice prescribed cow's milk with medications to enhance the efficacy/toxicity ratio [49,50]. Indian cow milk is rich in nutrients, containing about 4.6% lactose, 4.65% fat, 0.54% minerals, 3.4% proteins, and 86% water. Cow milk proteins contain 27% β-casein, 9% κ-casein, 36% α-casein, and 27% peptides [17]. Casein is present in a colloidal state, and it constitutes about 3% of milk, while pigments like xanthophyll, carotene, and riboflavin are also present. Milk also contains essential fatty acids and is a rich source of calcium and phosphorous. Phospholipids including cephalin, lecithin, and sphingomyelin, and vitamins including A, B2, B3, and K are also found in milk [17,51].
Consumption of cow milk shows various health benefits. Cow milk is used as a replacement for breast milk for infants. It is essential for the growth of teeth, bones [52], and heart activities management. The low cholesterol fat of milk is vital for mental and physical development, while milk helps maintain the digestive system, immune system, and brain functions. Lactose serves as an essential source of energy. Milk also enhances vision because of vitamin A whereas vitamin K regulates the blood clotting process.
Milk serves as a gold mine of medicinal effects. Anemia in infants can be treated by consuming milk. Cow milk restricts the growth of harmful gut bacteria and promotes beneficial gut flora [53]. Milk enzymes (xanthine oxidase, lactoperoxidase, and lysozyme) play an anti-bacterial role, whereas peptides (β-casomorphins, exorphin, and serorphin) exert anti-diarrhoeal activity. Regular milk consumption is suggested for patients suffering from gall bladder diseases, diabetes, and hyperlipidemia [54].
Cis-isomer of linoleic acid present in milk has demonstrated antineoplastic activity. It was found to restrict cancerous growth. Milk has anti-cancer activity against skin, colon, and breast cancer [55]. Considering all these beneficial effects of A2 type milk, the Government of India announced the ‘Rashtriya Gokul Mission’ in 2014 in order to increase the indigenous breeds of cow and get more A2 type of milk [50].
3. Method of preparation of Panchagavya ghrita and its variants
Classic Ayurvedic textbooks (Acharya Charak and Vagbhatacharya) have quoted the traditional methods of preparing Panchgavya Ghrita (PGG). This ancient literature has suggested the preparation of PGG with all five Panchgavya components (Fig. 1) in equal proportion [56].
Recent literature, prepared and published by the Government of India, explained a pre-preparation of cow dung juice. Ayurvedic Formulary of India (AFI) suggested the preparation and filtration of cow dung and cow urine before its use in PGG formulation. Further, all the Panchgavya products should be thoroughly mixed in equal quantities and heated at a low flame till the formulation achieved all parameters prescribed by AFI [57].
3.1. Variants of PGG
Ayurvedic literature also mentions variants of PGG formulation and revealed that PGG could be used as single or in combination with other herbs. Examples of such combinations and single-use are Swalpa-Panchgavya ghrita, PGG, and Mahapanchgavya ghrita. Such mixing of herbs in the PGG may increase the therapeutic profile of the formulation. The composition of different variants is shown in Table 2.
Table 2.
The Composition of different Panchgavya variants.
| Sr. No | Name of Variant | Composition | Reference |
|---|---|---|---|
| 1 | SwalpaPanchgavya Ghrita | All five Panchgavya components in equal quantities | [58] |
| 2 | Maha Panchgavya Ghrita | Kwatha dravya- 24 herbs in 2 pala quantity Kalka dravya- 18 herbs in 1 karsha quantity And each Panchgavya component in equal quantities. | [58] |
| 3 | Panchgavya Ghrita | Cow ghee 768 g and other four components are taken in 3.07 kg. | [58] |
4. Therapeutic effects of Panchagavya
4.1. Analgesic effect
Cow urine (2 ml, oral) and its distillate (2 ml, oral) were analyzed for analgesic activity in rats of both sexes (150–200 g) using the rat tail immersion test and Diclofenac Sodium (50 mg/kg, oral) as a reference standard. In the tail immersion test, the time taken for reflex action was recorded at 0th, 30th, 60th, and 90th minute after administration indicated analgesic effect. The intensity of analgesic activity of cow urine (7.63 ± 0.008, 8.25 ± 0.06, 8.36 ± 0.37) and distillate (8.36 ± 0.37, 8.28 ± 0.09, 9.34 ± 0.09) was observed to be comparable with the group receiving Diclofenac Sodium (9.07 ± 0.02, 10.55 ± 0.02, 11.22 ± 0.02) (P < 0.01). The analgesic effect was due to steroidal constituents and volatile fatty acids, which were confirmed using sophisticated analytical techniques in other studies. Ayurveda recommends using cow urine in pain relief, and the study served as scientific evidence for its acceptance in the modern world [59].
4.2. Hepatoprotective effect
PGG demonstrated hepatoprotective potential at a dose of 150–300 mg/kg, p.o. against carbon tetrachloride (CCl4)-induced hepatotoxicity in males albino rats of Sprague Dawley strain. Serum marker enzymes, i.e., serum glutamate oxaloacetate transaminase (SGOT), serum glutamate pyruvate transaminase (SGPT), alkaline phosphatase (ALP), acid phosphatase (ACP) were estimated to assess the liver function by taking Silymarin as a reference standard. PGG formulation was significantly active against CCl4-induced elevation in SGOT, SGPT, ALP, and ACP, preventing the elevation of these enzymes comparable with Silymarin [39]. Phospholipids influence the repair mechanisms with elevated thymidylate synthetase and thymidine kinase levels in the liver, reaching a peak at 72 h demonstrating liver regeneration [60,61].
4.3. Anti-haemorroid activity
Hemorrhoids are symptomatic enlargement and distal displacement of the anal mucosa. Treatment of 250 mg of gaumutra-ghana (extract of cow urine) along with the water was given twice daily for 30 days to patients of both sexes diagnosed with hemorrhoids of grade I and II. Consumption of cow urine exerted positive effects on the large intestine. Clinical evaluation supported cow urine as oral supplementation to relieve pain, ease defecation, prevent itching, and bleeding [[62], [63], [64]].
4.4. Wound healing activity
Cow ghee has demonstrated potential wound healing activity. High saturated and unsaturated fatty acid content is supposed to have participated in wound healing [65]. A study was conducted to examine the healing ability of cow ghee in combination with Aegle marmelos leaves extract and evaluated for the various parameters, i.e., decrease in the area of the wound, wound closure, wound contraction, and tissue regeneration at the damaged area. The combination demonstrated rapid wound healing within eight days [65,66].
Cow ghee was also evaluated with Aloe vera for wound healing potential by topical application 0.5 g of formulated gel. Wound contraction ceased between 21 and 24 days, increasing epithelization, providing tensile strength, and promoting collagen formation. The therapeutic intensity of wound healing was comparable with 0.5 g Framycetin sulphate cream (1% w/w) [67].
Cow urine was examined for wound healing activity using the Wistar albino rat's excision wound model of both sexes. Nitrofurazone was used as a reference standard. The experiment revealed the significant wound healing ability of cow urine. External application of cow urine for 14 days on the damaged area exhibited 50% wound healing compared to 50.3% healing of nitrofurazone, showing cow urine was more effective than nitrofurazone [68].
4.5. Effect on eyes
Computer Vision Syndrome (CVS) is a common problem across the globe, characterized by drying of eyes, burning sensation, itching, and redness. Lubricating eye drops are used for the treatment, and their regular use can cause damage to the eyes due to preservatives. Cow ghee has a lubricating property that can be used to treat CVS without any harmful effects. Cow ghee has Vitamin A which helps maintain moisture in the outer lining of the eyeball and prevents dryness and blindness [69].
4.6. Anti-microbial activity
Anti-microbial activity of cow urine and cow urine distillate was tested against pathogens like Bacillus subtilis, Salmonella typhi, Klebsiella pneumonia, and Pseudomonas aeruginosa [70]. Cow urine distillate (at 5, 10 and 15 μl) demonstrated maximum activity (zone of inhibition) against P. aeruginosa (7.06 ± 0.05, 8.08 ± 0.18 and 10.4 ± 1.23, mm in diameter, respectively) and S. typhi (6.3 ± 1.23, 8.06 ± 0.17 and 10.4 ± 1.2, mm in diameter, respectively) [1]. Cow urine and distillate also demonstrated free radical scavenging activity. Fresh cow urine was comparatively more effective than distillate. Ofloxacin was considered the standard, and the anti-microbial activity of fresh cow urine was comparable with Ofloxacin [71].
4.7. Anti-epileptic effect
PGG was examined for anti-epileptic activity using a rat model of maximal electroshock (MES) induced convulsions. PGG demonstrated anti-convulsant activity by increasing the motor activity of rats. The formulation also successfully inhibited the phenobarbitone-induced sleep time. The PGG is recommended as adjuvant therapy in treating epilepsy [72].
4.8. Nootropic effect
PGG was evaluated for nootropic activity using a model of diazepam-induced (1 mg/kg, i.p.) amnesia against piracetam (270 mg/kg) as a reference standard. Elevated Plus Maze (EPM) and Morris Water Maze (MWM) tests considering transfer latency and scape transfer latency as assessment parameters respectively was performed to confirm the activity. The PGG was administered at three different doses 2.5 g/kg, 5 g/kg and 10 /kg in Swiss albino mice (18-30 g) and 1.75 g/kg, 3.5 g /kg and 7.0 g/kg in Wistar rats (160-200 g). The therapeutic intensity in the group receiving 5 g/kg and 3.5 g/kg of the formulation was comparable to the standard in EPM and MWM tests. PGG demonstrated significant memory-enhancing and memory retention activity [73].
4.9. Anti-cancer effect
A comparative evaluation of cow ghee and soyabean oil in a rat model of 7,12-dimethylbenz(a)-anthracene (DMBA) induced mammary carcinogenesis revealed the anti-cancer potential of cow ghee by expressing cox-2 and peroxisome proliferators activated receptors-γ(PPAR-γ) in mammary glands. The group receiving cow ghee had lower tumour incidences (26.6%), low tumour weight (1.67 g), and volume (1925 mm3) compared to the group receiving soyabean oil (65.4%,6.18 g, 6285 mm3) [74]. Cow urine has also demonstrated its potential as an antineoplastic agent [75,76].
5. Role of Panchagavya in agriculture
The application of Panchgavya in agricultural fields demonstrated several benefits.
5.1. Effect on soil
Panchgavya improves soil fertility by increasing organic matter, macro and micronutrient levels, and the uptake of nutrients in plants, promoting the growth and reproduction of micro-organisms and maintaining good soil health. It also progresses the physical properties of soil by increasing the porosity and balancing the soil aggregate stability, regulating soil pH and the soil's nutrient profile. Beaulah, in his study confirmed the application of Panchgavya in agricultural fields dramatically influences the growth and crop yield by promoting the beneficial soil microorganisms around the roots [77].
5.2. Effect on different parts of plants and crops
The spraying of Panchgavya on leaves results in the production of invariably bigger leaves and denser canopy; enhances photosynthetic material, which results in maximum production of metabolites and photosynthates [78]. It also develops side shoots from the trunk carrying the maximum number of fruits to maturity; rich and high branching; rich and dense roots grow in deeper soil layers. Furthermore, it helps plants and crops remain fresh for a longer time with a high intake of nutrients and water [79].
5.3. Role in organic farming
Pacnhgavya helps in the production of synthetic pesticide-free food. It also maintains and restores crop production levels when the field changes from inorganic to organic farming practices within a year. It enhances the shelf-life, taste of fruits, grains, and vegetables and yields better and safe quality food products. Moreover, it improves crop harvest by 15 days and reduces crop production costs by decreasing the expenses on chemicals, thereby increasing profit margin.
6. Panchagavya-based nanotechnology
Nanoparticles are the fundamental building blocks in nanotechnology, and they consist of macromolecular materials in which drug (active ingredient, biologically active compound) is dissolved, entrapped, encapsulated, adsorbed, or attached. Nanotechnologies have a diverse range of applications and have become one of the functional areas of research in drug delivery due to their capacity to deliver drugs to the right place, at the correct time, and in the proper dosage [80].
Arumugam et al. synthesized Panchgavya mediated copper nanoparticles using Panchgavya filtrate and copper sulphate solution (25 mM) as substrate. Copper nanoparticles were characterized using various techniques; Ultraviolet spectrophotometer, Fourier transmission infrared spectroscopy, X-ray diffraction analysis, Dynamic light scattering, Scanning electron microscope, High-resolution transmission electron microscope, X-ray fluorescent microscopy. Moreover, they have been evaluated for their antioxidant and cytotoxic potential [81].
Govarthanan et al. synthesized silver nanoparticles using 4 ml of Panchgavya filtrate in 96 ml of 1 mM AgNO3 solution. The prepared nanoparticles were characterized and demonstrated concentration-dependent anti-microbial activity against antibiotic-resistant bacterial species (sp) such as Aeromonas sp., Acinetobacter sp., and Citrobacter sp [82].
7. Conclusion
Panchgavya has demonstrated its potential to serve humankind and is a promising therapy against various human ailments. The effects of Panchgavya must not be limited only to ancient literature although, scientific efforts are needed to validate biological activities and safety and establish the standards. Detailed experimentations are required for each product to validate composition, chemical behaviour, pharmacological activity, safety, toxicity profile, and the mechanism of action of the active components. It is equally important to educate the people and promote Panchgavya products to seek the world's attention towards India's rich traditional practice and literature.
Source(s) of Funding
None.
Conflict of interest
None.
Author Contributions
Komal Bajaj: Data curation, Resources, Methodology, Roles/Writing- original draft; Vishal Chavan: Data curation, Resources, Roles/Writing- original draft; Nishikant Raut: Conceptualization, Investigation, Resources, Validation; Shailendra S. Gurav: Supervision, Validation, Formal analysis, Writing - review & editing.
Footnotes
Peer review under responsibility of Transdisciplinary University, Bangalore.
References
- 1.Shah C.P., Patel D.M., Dhami P.D., Kakadia J., Bhavsar D., Vachhani U.D., et al. In vitro screening of antibacterial activity of cow urine against pathogenic human bacterial strains. Int J Curr Pharmaceut Res. 2011;3:91–92. [Google Scholar]
- 2.Dhama K., Rathore R., Chauhan R.S., Tomar S. Panchgavya (cowpathy): an overview. Int J Cow Sci. 2005;1:1–15. [Google Scholar]
- 3.Khan M.Y., Roy M., Saroj B.K., Dubey S., Sharma V.K. A Review-Benefits of Panchgavya therapy (Cowpathy) for health of humans. Asian J Res Pharm Sci. 2015;5:115. doi: 10.5958/2231-5659.2015.00019.3. [DOI] [Google Scholar]
- 4.Chauhan R.S. Cowpathy: a new version of ancient science. Indian Cow Sci Econ J. 2008;5:39–40. [Google Scholar]
- 5.Schnürer J., Magnusson J. Antifungal lactic acid bacteria as biopreservatives. Trends Food Sci Technol. 2005;16:70–78. doi: 10.1016/j.tifs.2004.02.014. [DOI] [Google Scholar]
- 6.Chauhan R.S. Panchgavya therapy (Cowpathy): current status and future directions. Indian Cow Sci Econ J. 2004;1:3–7. [Google Scholar]
- 7.Tharmaraj K., Ganesh P., Kumar R.S., Anandan A., Kolanjinathan K. A critical review on Panchagavya-a boon plant growth. Int J Pharm Biol Arch. 2011;2:1611–1614. [Google Scholar]
- 8.Pathak R.K., Ram R.A. Bio-enhancers: a potential tool to improve soil fertility, plant health in organic production of horticultural crops. Progress Hortic. 2013;45:237–254. [Google Scholar]
- 9.Blaser M.J. NY Henry Holt Co; New York: 2014. Missing microbes. [Google Scholar]
- 10.Kuldeep D., Sandip C., Ruchi T. Panchgavya therapy (Cowpathy) in safeguarding health of animals and humans-a review. Res Opin Anim Vet Sci. 2013;3:170–178. [Google Scholar]
- 11.Irvine S.L., Hummelen R., Hekmat S., Looman C W.N., Habbema J.D.F., Reid G. Probiotic yogurt consumption is associated with an increase of CD4 count among people living with HIV/AIDS. J Clin Gastroenterol. 2010;44 doi: 10.1097/mcg.0b013e3181d8fba8. [DOI] [PubMed] [Google Scholar]
- 12.Dhama K., Khurana S.K., Karthik K., Tiwari R., Malik Y.P.S., Chauhan R.S. Panchgavya: immune-enhancing and therapeutic perspectives. J Immunol Immunopathol. 2014;16:1. doi: 10.5958/0973-9149.2014.01071.5. [DOI] [Google Scholar]
- 13.Kadooka Y., Sato M., Imaizumi K., Ogawa A., Ikuyama K., Akai Y., et al. Regulation of abdominal adiposity by probiotics (Lactobacillus gasseri SBT2055) in adults with obese tendencies in a randomized controlled trial. Eur J Clin Nutr. 2010;64:636–643. doi: 10.1038/ejcn.2010.19. [DOI] [PubMed] [Google Scholar]
- 14.Singh B.P., Chauhan R.S. Cow Dahi (curd) or Matha (Butter Milk): as probiotic to control animal diseases. Indian Cow Sci Econ J. 2004;1:6–10. [Google Scholar]
- 15.Godse C.S., Paradkar P.H., Loke V.M., Udipi S.A., Vaidya R.A., Vaidya A.D.B. Cow's milk: nutritional relevance beyond its intolerance and allergies. Indian Pract. 2017;70:29–34. [Google Scholar]
- 16.Umanu G., Nwachukwu S.C.U., Olasode O.K. Effects of cow dung on microbial degradation of motor oil in lagoon water. GJBB. 2013;2:542548. [Google Scholar]
- 17.Ananno A.A., Masud M.H., Mahjabeen M., Dabnichki P. In: Sustainable bioconversion of waste to value added products. Advances in science, technology & innovation (IEREK Interdisciplinary Series for Sustainable Development) Inamuddin, Khan A., editors. Springer; Cham: 2021. Multi-utilisation of cow dung as biomass. [DOI] [Google Scholar]
- 18.Palanisami S., Natarajan E., Rajamma R. Development of eco-friendly herbal mosquito repellent. J Innov Biol. 2014;1:132–136. [Google Scholar]
- 19.Chauhan R.S., Dhama K. Panchgavya (cowpathy): an ancient wisdom & modern science. Indian Cow Sci Econ J. 2010;6:1–25. [Google Scholar]
- 20.Tuthill D.E., Frisvad J.C. Eupenicillium bovifimosum, a new species from dry cow manure in Wyoming. Mycologia. 2002;94:240. doi: 10.2307/3761800. [DOI] [PubMed] [Google Scholar]
- 21.Lehr N.-A., Meffert A., Antelo L., Sterner O., Anke H., Weber R.W.S. Antiamoebins, myrocin B and the basis of antifungal antibiosis in the coprophilous fungus Stilbella erythrocephala (syn. S. fimetaria) FEMS Microbiol Ecol. 2006;55:105–112. doi: 10.1111/j.1574-6941.2005.00007.x. [DOI] [PubMed] [Google Scholar]
- 22.Hand P., Hayes W.A., Satchell J.E., Frankland J.C. earthworms waste environ manage by Clive A Edwards Edward F Neuhauser. 1988. Vermicomposting of cow slurry. [Google Scholar]
- 23.Basak A.B., Lee M.W., Lee T.S. In vitro inhibitory activity of cow urine and dung to fusarium solani f. sp. cucurbitae. MYCOBIOLOGY. 2002;30:51–54. [Google Scholar]
- 24.Geetha M., Fulekar M.H. Bioremediation of pesticides in surface soil treatment unit using microbial consortia. Afr J Environ Sci Technol. 2008;2:36–45. [Google Scholar]
- 25.Singh D., Fulekar M.H. Benzene bioremediation using cow dung microflora in two phase partitioning bioreactor. J Hazard Mater. 2010;175:336–343. doi: 10.1016/j.jhazmat.2009.10.008. [DOI] [PubMed] [Google Scholar]
- 26.Chauhan R.S., Singhal L. Harmful effects of pesticides and their control through cowpathy. Int J Cow Sci. 2006;2:61–70. [Google Scholar]
- 27.Kulkarni S.K. Vallabh prakashan; 1987. Hand book of experimental pharmacology. [Google Scholar]
- 28.Joshi K.S. Docosahexaenoic acid content is significantly higher in ghrita prepared by traditional Ayurvedic method. J Ayurveda Integr Med. 2014;5:85–88. doi: 10.4103/0975-9476.131730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ganguli N.C., Jain M.K. Ghee: its chemistry, processing and technology. J Dairy Sci. 1973;56:19–25. [Google Scholar]
- 30.Lamsal B., Bhandari T.R., Panta P., Saiter J.M., Pokhrel S., Katuwal T.B., et al. Preparation and physicochemical characterization of ghee and mūrcchita ghrta. J Ayurveda Integr Med. 2020;11:256–260. doi: 10.1016/j.jaim.2020.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ray S.C. Pre-stratification method ghee making. 1960. Pre-stratification method of ghee making. [Google Scholar]
- 32.Singh R.B., Niaz M.A., Ghosh S., Beegom R., Rastogi V., Sharma J.P., et al. Association of trans fatty acids (vegetable ghee) and clarified butter (Indian ghee) intake with higher risk of coronary artery disease in rural and urban populations with low fat consumption. Int J Cardiol. 1996;56:289–298. doi: 10.1016/0167-5273(96)02760-x. [DOI] [PubMed] [Google Scholar]
- 33.Malhotra A., Redberg R.F., Meier P. Saturated fat does not clog the arteries: coronary heart disease is a chronic inflammatory condition, the risk of which can be effectively reduced from healthy lifestyle interventions. Br J Sports Med. 2017;51:1111–1112. doi: 10.1136/bjsports-2016-097285. [DOI] [PubMed] [Google Scholar]
- 34.Chinnadurai K., Kanwal H.K., Tyagi A.K., Stanton C., Ross P. High conjugated linoleic acid enriched ghee (clarified butter) increases the antioxidant and antiatherogenic potency in female Wistar rats. Lipids Health Dis. 2013;12:121. doi: 10.1186/1476-511X-12-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gurav N., Gurav S., Wanjari M., Prasad S., Wayal S., Rarokar N. Development and evaluation of aphrodisiac potential of a classical ayurvedic formulation,‘Kaamdev ghrita’in rat model. J Ayurveda Integr Med. 2021;12(2):294–301. doi: 10.1016/j.jaim.2020.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gurav N.S., Gurav S.S., Sakharwade S.N. Studies on Ashwagandha Ghrita with reference to murcchana process and storage conditions. J Ayurveda Integr Med. 2020;11(3):243–249. doi: 10.1016/j.jaim.2019.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wayal S.R., Gurav S.S. Bhallatakadi ghrita: development and evaluation with reference to murcchana and shata-dhauta process. J Ayurveda Integr Med. 2020;11(3):261–269. doi: 10.1016/j.jaim.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wayal S.R., Gurav S.S. Evaluation of wound healing potential of Bhallatakadi Ghrita–cow ghee based polyherbal formulation: in-vivo excision and incision wound model. J Compl Integr Med. 2021 doi: 10.1515/jcim-2020-0179. [DOI] [PubMed] [Google Scholar]
- 39.Ahmad N., Saleem M., Atta B.M., Mahmood S. Characterization of desi ghee extracted by different methods using fluorescence spectroscopy. J Fluoresc. 2019;29:1411–1421. doi: 10.1007/s10895-019-02453-6. [DOI] [PubMed] [Google Scholar]
- 40.Chunekar K.C. Chaukhamba Vidya Bhavan; Banaras, India: 1960. Bhav Prakasa Nighantu (Hindi translation) p. 86. [Google Scholar]
- 41.Simon A., Traynor K., Santos K., Blaser G., Bode U., Molan P. Medical honey for wound care--still the “latest resort”? Evid Based Complement Alternat Med. 2009;6:165–173. doi: 10.1093/ecam/nem175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mohanty I., Senapati M.R., Jena D., Palai S. Diversified uses of cow urine. Int J Pharm Pharmaceut Sci. 2014;6:20–22. [Google Scholar]
- 43.Khanuja S.P.S., Kumar S., Shasany A.K., Arya J.S., Darokar M.P., Singh M., et al. 2005. Use of bioactive fraction from cow urine distillate (‘go-mutra’) as a bio-enhancer of anti-infective, anti-cancer agents and nutrients. [Google Scholar]
- 44.Khan A., Srivastava V.K. Antitoxic and bioenhancing role of kamdhenu ark (cow urine distillate) on fertility rate of male mice (Mus musculus) affected by cadmium chloride toxicity. Int J Cow Sci. 2005;1:43–46. [Google Scholar]
- 45.Krishnamurthi K., Dutta D., Sivanesan S.D., Chakrabarti T. Protective effect of distillate and redistillate of cow's urine in human polymorphonuclear leukocytes challenged with established genotoxic chemicals. Biomed Environ Sci. 2004;17:247–256. [PubMed] [Google Scholar]
- 46.Minocheherhomji F.P. Bio enhancing properties of cow urine–A Review. Int J Innov Res Sci Eng Technol. 2016;5:16283–16287. [Google Scholar]
- 47.Gopalan S., Puri R.K., hps Sachdev. 1993. Adequacy of vegetarian diets for optimal nutrition of motker and child. [PubMed] [Google Scholar]
- 48.Woodford K.B. Chelsea Green Publishing; 2009. Devil in the milk: illness, health and politics of A1 and A2 milk. [Google Scholar]
- 49.Raut A.A. Bharatiya Vidya Bhavan; 2010. Vaidya Antarkar memorial volume. [Google Scholar]
- 50.Kimpel F., Schmitt J.J. Review: milk proteins as nanocarrier systems for hydrophobic nutraceuticals. J Food Sci. 2015;80:R2361–R2366. doi: 10.1111/1750-3841.13096. [DOI] [PubMed] [Google Scholar]
- 51.Singh A., Agrawal D.K. Quality milk from Indian cows. Indian Cow Sci Econ J. 2004;1:39–49. [Google Scholar]
- 52.Raut A., Bichile L., Chopra A., Patwardhan B., Vaidya A. Comparative study of amrutbhallataka and glucosamine sulphate in osteoarthritis: six months open label randomized controlled clinical trial. J Ayurveda Integr Med. 2013;4:229–236. doi: 10.4103/0975-9476.123708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Nautiyal C.S. Cow's milk a novel source of microbial wealth. Indian Cow Sci Econ J. 2011;8:41–45. [Google Scholar]
- 54.Bettiol W. Effectiveness of cow's milk against zucchini squash powdery mildew (Sphaerotheca fuliginea) in greenhouse conditions. Crop Protect. 1999;18:489–492. doi: 10.1016/s0261-2194(99)00046-0. [DOI] [Google Scholar]
- 55.Singh B.P., Chauhan R.S. Cow Dahi (curd) or Matha (butter milk): as probiotic to control animal diseases. Indian Cow Sci Econ J. 2008;4:42–45. [Google Scholar]
- 56.Shukla, Tripathi . Chikitsa Sthan Ch10; 2006. Charak Samhita. Chaukhamba Sanskrit Prakashan; p. p251. Verse17. [Google Scholar]
- 57.Committee AP The ayurvedic formulary of India. Partisans. 2000;1:367. [Google Scholar]
- 58.Pandey A., Pawar M. Panchagavya and Panchagavya Ghrita a conceptual study. 2016;1:24–28. [Google Scholar]
- 59.Wate S.P., Duragkar N.J., Tajne M.R., Jadhav S.S. Study of analgesic activity of cow urine and its distillate by rat-tail immersion method. Indian J Pharm Chem Sci Jan Mar. 2012;1:95–96. [Google Scholar]
- 60.Dobrynina O.V., Migushina V.L., Shatinina S.Z., Boldanova N.B. Use of phospholipids to repair rat liver membranes during carbon tetrachloride poisoning. Biulleten’eksperimental’noi Biol i Meditsiny. 1987;104:301–303. [PubMed] [Google Scholar]
- 61.Devarshi P., Kanase A., Kanase R., Mane S., Patil S., Varute A.T. Effect of mandur bhasma on lipolytic activities of liver, kidney and adipose tissue of albino rat during CCl 4 induced hepatic injury. J Biosci. 1986;10:227–234. [Google Scholar]
- 62.Lohsiriwat V. Hemorrhoids: from basic pathophysiology to clinical management. World J Gastroenterol. 2012;18:2009–2017. doi: 10.3748/wjg.v18.i17.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sushruta Samhita (the compendium of Sushruta) Lancet. 1912;180:1025–1026. doi: 10.1016/s0140-6736(01)57200-1. [DOI] [Google Scholar]
- 64.Talokar O.W., Belge A.R., Belge R.S. Clinical evaluation of cow-urine extract special reference to Arsha (Hemmorrhoids) Int J Pharm Sci Invent. 2013;2 [Google Scholar]
- 65.Biyani D.M., Verma P.R.P., Dorle A.K., Boxey V. Wound healing activity of cow ghee: a veterinary case report. Int J Ayurvedic Med. 2011;2 doi: 10.47552/ijam.v2i3.71. [DOI] [Google Scholar]
- 66.Shaikh S.S., Ukande M.D., Murthy K., Shete R.V., Solunke R.S. Traditional remedies for wound healing: a review. J Drug Deliv Therapeut. 2019;9:761–764. doi: 10.22270/jddt.v9i4-s.3263. [DOI] [Google Scholar]
- 67.Nandanwar R., Gurjar H., Sahu V.K., Saraf H. Studies on wound healing activity of gel formulation containing cow ghee and Aloe vera. Int J Pharma Sci Res. 2010;1:50–54. [Google Scholar]
- 68.Sanganal J., JayakumarK J., GM J., Tikare V.P., R P. Effect of cow urine on wound healing property in Wister Albino Rats. Vet World. 2011;317 doi: 10.5455/vetworld.4.317. [DOI] [Google Scholar]
- 69.Mulik S.S., Bhusari D.P. Conceptual study of goghrita eye drops (aschyotana) in computer vision syndrome. Asian J Multidiscip Stud Octane. 2013;1:1–6. [Google Scholar]
- 70.Ahuja A., Kumar P., Verma A., Tanwar R. Antimicrobial activities of cow urine against various bacterial strains. Int J Recent Adv Pharm Res. 2012;2:84–87. [Google Scholar]
- 71.Jarald E., Edwin S., Tiwari V., Garg R., Toppo E. Antioxidant and antimicrobial activities of cow urine. Global J Pharmacol. 2008;2:20–22. [Google Scholar]
- 72.Gosavi D., Jhon S. Effect of Panchagavya Ghritra on some neurological parameters in albino rats. Asian J Pharm Sci Clin Res. 2012;5:154–156. [Google Scholar]
- 73.Pandey A., Pawar M.S. Assessment of nootropic activity of Panchagavya ghrita in animal models. Int J Sci Res Publica. 2015;5:1–5. [Google Scholar]
- 74.Rani R., Kansal V.K. Study on cow ghee versus soybean oil on 7, 12-dimethylbenz (a)-anthracene induced mammary carcinogenesis & expression of cyclooxygenase-2 & peroxisome proliferators activated receptor-γ in rats. Indian J Med Res. 2011;133:497. [PMC free article] [PubMed] [Google Scholar]
- 75.Rani R., Kansal V.K. Effects of cow ghee (clarified butter oil) & soybean oil on carcinogen-metabolizing enzymes in rats. Indian J Med Res. 2012;136:460. [PMC free article] [PubMed] [Google Scholar]
- 76.Jain N.K., Gupta V.B., Garg R., Silawat N. Efficacy of cow urine therapy on various cancer patients in Mandsaur District, India - a survey. Int J Green Pharm. 2010;4:29. doi: 10.4103/0973-8258.62163. [DOI] [Google Scholar]
- 77.Beaulah A. 2001. Growth and development of moringa (Moringa oleifera Lam.) under organic and inorganic systems of culture. [Google Scholar]
- 78.Katyal V., Gangwar K.S., Gangwar B. Long-term effect of fertiliser use on yield sustainability and soil fertility in rice-wheat system in sub-tropical India. Fertil News. 2003;48:43–48. [Google Scholar]
- 79.Kaushik S.K., Gautam R.C. Response of rainfed pearl millet (Pennisetum glaucum) to water harvesting, moisture conservation and plant population in light soils. Indian J Agric Sci. 1994;64:858–860. [Google Scholar]
- 80.Swaminathan C. 1st ed. International Book Distributing Co.; Lucknow U.P. India: 2007. Panchagavya: boon to organic farming. [Google Scholar]
- 81.Arumugam D.G., Sivaji S., Dhandapani K.V., Nookala S., Ranganathan B. Panchagavya mediated copper nanoparticles synthesis, characterization and evaluating cytotoxicity in brine shrimp. Biocatal Agric Biotechnol. 2019;19:101132. doi: 10.1016/j.bcab.2019.101132. [DOI] [Google Scholar]
- 82.Govarthanan M., Selvankumar T., Manoharan K., Rathika R., Shanthi K., Lee K.J., et al. Biosynthesis and characterization of silver nanoparticles using panchakavya, an Indian traditional farming formulating agent. Int J Nanomed. 2014;9:1593–1599. doi: 10.2147/IJN.S58932. [DOI] [PMC free article] [PubMed] [Google Scholar]