Abstract
Background
Inferior alveolar nerve block (IANB) is known to have a lower success rate for anesthesia in patients with irreversible pulpitis. This calls for supplementary techniques to effectively anesthetize such patients. This systematic review aimed to evaluate the published literature for determining the success rate of anesthesia induction using post-IANB intraligamentary (IL) injection in the mandibular teeth of patients with symptomatic irreversible pulpitis. The review question was, “What is the success rate of IL injection in the mandibular teeth of patients with irreversible pulpitis as a supplementary technique for endodontic treatment?”
Methods
A thorough search of electronic databases and manual searches were performed. The protocol of the review was framed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist and was registered in the International Prospective Register of Ongoing Systematic Reviews (PROSPERO) with a proper criterion for inclusion and exclusion of studies. The included studies were analyzed using the Cochrane Collaboration ‘‘Risk of Bias’’ tool. A meta-analysis that included a comparison of primary nerve block and supplemental IL injection was performed. The success rate was evaluated using the combined risk ratio (RR) with a random risk model. A funnel plot was created to measure publication bias.
Results
After all analyses, four studies were included. In the forest plot representation, RRs were 3.56 (95% CI: 2.86, 4.44), which were in favor of the supplemental IL injections. Statistical heterogeneity was found to be 0%. These values suggest that supplemental IL injections provide better success rates for anesthesia.
Conclusion
According to the pooled qualitative and quantitative analyses, supplemental IL injections increased anesthetic efficacy.
Keywords: Intraligamentary Injection, Irreversible Pulpitis, Local Anesthesia, Mandible, Tooth
INTRODUCTION
The most common method of anesthetizing the mandibular teeth is inferior alveolar nerve block (IANB) [1]; however, the failure rate is high [2,3]. According to previous studies, IANB has a success rate of < 30% in cases of symptomatic irreversible pulpitis [4,5]. This may be due to the inflammation-related activation of certain receptors, such as tetrodotoxin-resistant receptors and capsaicin-sensitive transient receptor potential vanilloid type 1. These receptors resist local anesthetic agents and reduce their efficacy [6,7,8]. Various studies have suggested alternative methods to reduce the pain and discomfort experienced during root canal treatment, including the application of supplemental injections such as periodontal ligament (PDL) or IL, intraosseous (IO), and intrapulpal injections as well as buccal infiltrations (BIs) [9,10]. Additionally, evidence suggests that the administration of pre-medications, such as non-steroidal anti-inflammatory drugs, potentiates pre-treatment analgesia [11]. Furthermore, BI with 4% articaine shows an improved but inconsistent success rate [12,13,14,15]. It was also found that BI successfully anesthetized maxillary teeth subjected to dental treatment; however, its efficacy was hindered by the thickness of the buccal cortical bone [16].
Intrapulpal injections have a reportedly high success rate and are often regarded as the final option for inducing anesthesia. These injections have an immediate onset but short duration of action. For proper deposition of the anesthetic solution, the pulpal space must be properly and adequately exposed [9]. On the other hand, IL and IO injections are also common supplemental anesthetic techniques [8,9,14,17,18,19,20]. The solution is injected directly into the bone around the tooth. IO injections have a good success rate as a supplemental injection [18]; however, special equipment may be needed, which could lead to adverse effects [9,17].
According to an investigative survey by members of the American Association of Endodontists, patients with symptomatic irreversible pulpitis require supplemental anesthetic injections. In such cases, an IL injection is frequently administered [10]. This technique involves forcefully injecting the agent into the bone adjacent to the affected tooth root and periodontal ligament [10,17]. In 1982, Malamed recommended IL as an alternative to IANB. In endodontics, IL injections have been studied as both primary and supplemental injections [20,21]. Supplemental IL injections have a success rate of 50-96% for painless endodontic treatment [18,22,23,24,25,26,27].
The efficacy of supplemental injections may be influenced by the volume of the solution. However, evidence regarding its required volume for administration remains scarce. Various studies report a volume range of 0.2 to 0.9 mL per root [17,22,24,26,28]; injecting 0.2 mL of the solution into the PDL space was advised by Malamed [17]. However, successful IL injections have no clearly defined volume. Another factor that may affect its efficacy is the mode of delivery. The IL technique can be applied using standardized, specialized mechanical, or computer-operated syringes [21,22,24]. Following a failed nerve block in mandibular teeth with irreversible pulpitis, a computerized local anesthetic delivery system was used for its delivery, with a success rate of approximately 56% [22].
Many investigations have attempted to determine the most optimal local anesthetic agent in association with the IL technique. By comparing 4% articaine with 1:100,000 epinephrine and 2% lidocaine with 1:100,000 epinephrine, no significant difference in pain elimination during anesthetic induction was observed [10]. Therefore, there is ambiguity regarding the type of solution used for IL injection.
As a result, the present review focuses on the success rate of IL injection as a supplementary technique in symptomatic irreversible pulpitis in human mandibular teeth; conflicting variables such as volume, type, and mode of delivery were excluded.
METHODS
1. Registration
The review protocol was prepared following the established Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist and was registered on International Prospective Register of Ongoing Systematic Reviews (PROSPERO) under the number, CRD42020201534 [28].
2. Eligibility criteria
The PICO framework was applied to frame the question as, “What is the success rate of IL injection in the mandibular teeth of patients with irreversible pulpitis as a supplementary technique for endodontic treatment?”
The framework included:
P: Human mandibular teeth with irreversible pulpits
I: Anesthesia with IANB
C: Anesthesia with IANB + supplementary intraligamentary injection
O: Successful anesthesia and painless root canal treatment procedure
3. Search strategy
A thorough manual search was carried out in electronic databases (PubMed, Scopus, and Ebsco). A combination of keywords was prepared using the Boolean operators “AND” and “OR” for a systematic search for studies published until December 2020 (Table 1). Duplicates were identified and excluded.
Table 1. Lists of combination of keywords for electronic database search strategy.
| Database | Search strategy (2020) | n (search results as on Dec 2020) |
|---|---|---|
| PubMed | (“Intraligamentary Injection” [All fields] OR “Periodontal Ligament Injection” [All fields] AND “Irreversible Pulipitis” [All fields] OR “Symptomatic Irreversible Pulpitis” [All fields] OR “Asymptomatic Irreversible Pulpitis” [All fields] AND “Systematic Review” [All fields]) | 38 |
| SCOPUS | (“Intraligamentary Injection” [All fields] OR “Periodontal Ligament Injection” [All fields] AND “Irreversible Pulipitis” [All fields] OR “Symptomatic Irreversible Pulpitis” [All fields] OR “Asymptomatic Irreversible Pulpitis” [All fields] AND “Systematic Review” [All fields]) | 132 |
| EbscoHost | (“Intraligamentary Injection” [All fields] OR “Periodontal Ligament Injection” [All fields] AND “Irreversible Pulipitis” [All fields] OR “Symptomatic Irreversible Pulpitis” [All fields] OR “Asymptomatic Irreversible Pulpitis” [All fields] AND “Systematic Review” [All fields]) | 27 |
4. Inclusion criteria
The following inclusion criteria were established and used for screening:
• Clinical studies published in English between 1960 and December 2020
• Studies with adult human patients planned for root canal treatment
• Studies of symptomatic irreversible pulpitis in mandibular teeth
• Studies with supplemental IL techniques after failed primary IANB injections
• Studies reporting the success of IL injection either in percentages or numbers
• Performed access preparation and pulp extirpation to check for pulpal anesthesia
• Patients able to understand pain scales
5. Exclusion criteria
The following exclusion criteria were established and used for screening:
• Studies evaluating other techniques such as infiltration, IO, and any pre-medication;
• Patients with systemic diseases
• Patients who received analgesics on the same day as the treatment
• Case reports and case series
• Studies evaluating the influence of any medication on the success of an anesthetic technique
• Studies in pediatric patients
• Patients with a known allergic response to local anesthesia
6. Data extraction
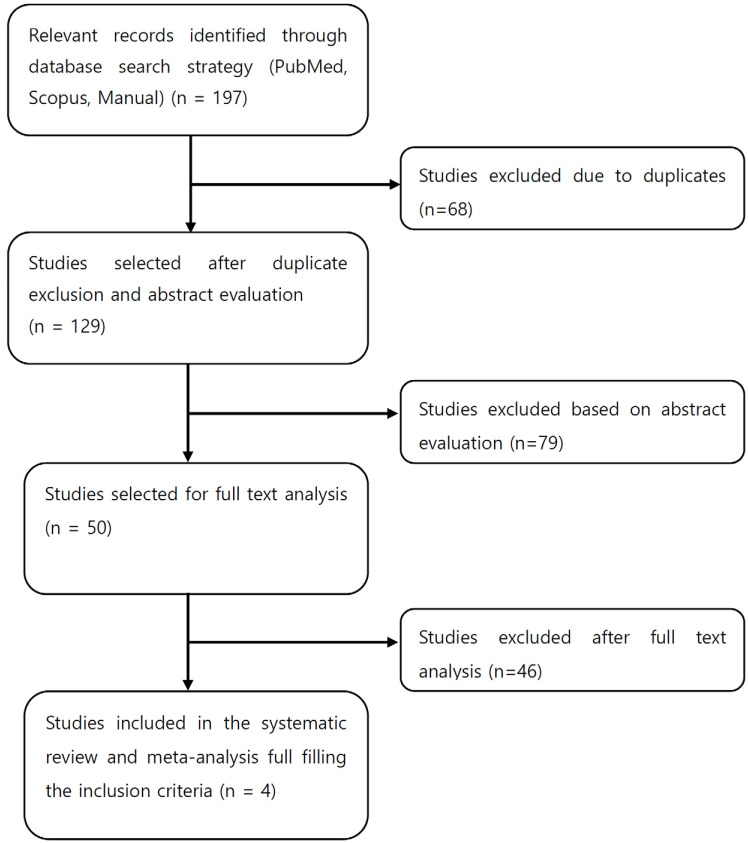
All articles were manually searched along with a thorough analysis of their bibliography to extract relevant data, which was then framed as a PRISMA flowchart (Fig. 1). Each study was examined according to multiple parameters, such as authors, language of publication, sample size, and information of participants as well as their evaluation of pain presented as scales and success rates with statistical values.
Fig. 1. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart.
RESULTS
After thorough evaluation, 197 articles were found to be relevant; 129 abstracts were screened. Proper inclusion and exclusion criteria were followed to include only four articles in the final analysis.
1. Study characteristics
Four articles studied the effect of IL injection as a supplemental technique after a failed nerve block in irreversible pulpitis in mandibular teeth [24,26,27,29]. Individual study characteristics are presented in Table 2.
Table 2. Summary of the included studies.
| Author/Country | Year & journal of publication (language) | Tooth type, number of subjects and group wise division | Primary or supplemental injection type | Case/study type | Pain evaluation | Success rate with statistical result |
|---|---|---|---|---|---|---|
| Aggarwal, et al./India [27] | 2019, J Endod (English) | Mandibular 1st & 2nd molars Total patients: 82 in the age group 21-44years Group 1= 24 males and 17 females 1st Molars-30 2nd Molars-11 Group 2= 24 males and 14 females 1st Molars-34, 2nd Molars-7 |
1°–IANB 1.8 ml of 2% lidocaine with 1:100000 epinephrine Supplemental Group 1 IL – 0.6 ml of 4% articaine with 1 : 100000 epinephrine Group 2 IL - 2% Lidocaine with 1 : 80000 epinephrine |
Symptomatic irreversible pulpitis Randomised double blind study |
Heft parker VAS | Group 1 = 66% Group 2 = 78% (No significant difference among groups) |
| Aggarwal, et al./India [26] | 2018, Int End J (English) | Mandibular Molars Total patients= 78 Group 1 - Age group 19-35 years 16 males and 23 females Group 2 - Age group 21-43 years 24 males and 15 females |
1°– IANB Supplemental Group 1 - IL - 0.2 ml of 2% Lidocaine with 1 : 80000 epinephrine Group 2 IL - 0.6 ml of 2% Lidocaine with 1 : 80000 epinephrine |
Symptomatic irreversible pulpitis Randomised double blind study |
Heft parker VAS | Group 1= 64% Group 2= 84% sig diff |
| Zarei, et al./Iran [24] | 2012 Int End J (English) | Mandibular Molars & Premolars Total patients = 40 in the age group of 18-50 years 18 males and 22 females |
1° – IANB Supplemental Group 1 - I0 with X tip Group 2 IL - 1,8 ml of 2% Lidocaine with 1 : 100000 epinephrine |
Symptomatic irreversible pulpitis Randomised Controlled clinical single blind study |
VAS | Group 1 = 100% Group 2 = 70% (No significant difference) |
| Aggarwal et al./India [29] | 2020 Act Odont Scand (English) | Mandibular Molars Total patients = 118 Group 1 - Age group 25-52 years 16 females and 28 males Group 2 - Age group 23-48 years 17 females and 27 males |
1° – IANB 2% lidocaine with 1:80,000 epinephrine Supplemental: Group 1: 2% lidocaine with 1:80,000 epinephrine. Group 2: 2% lidocaine with 1:200,000 epinephrine. |
Symptomatic irreversible pulpitis Randomised double blind study |
Heft Parker VAS | Group 1: 82% Group 2: 57% No significant difference |
IANB, inferior alveolar nerve block; IL, intraligamentary; IO, intraosseous; VAS, visaul analog scale.
2. Outcomes
Successful anesthesia was assessed in each study. Absent or mild pain reported via scores on a scale, such as the Heft Parker Visual Analog (HP VAS) [30] and Visual Analog Scales (VAS), during root canal treatment steps (access cavity preparation and instrumentation) was considered a successful anesthetic effect.
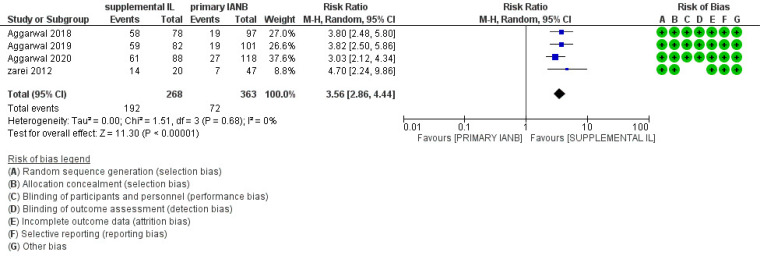
3. Risk of bias assessment
The Cochrane Collaboration ‘‘Risk of Bias’’ tool was used to analyze the quality of the studies [31]. This was performed using the RevMan 5.3 software. Various domains were assessed; final judgments were indicated as low, high, or unclear risk. The meta-analysis of the included studies was based on a comparison of primary IANB versus supplementary IL injection.
4. Interpretation of studies
Aggarwal et al. (2019) [27] carried out a randomized trial to evaluate the anesthetic effect of 4% articaine and 2% lidocaine administered as a supplemental IL technique after unsuccessful anesthesia by primary nerve block injection. Interpretation of the success or failure of anesthesia was determined by mild or absent pain during access opening. If the patient reported minimal pain during treatment (HP VAS score < 55), it was regarded as successful anesthesia. Patients with primary IANB failure received supplementary IL injections of 2% lidocaine (1:80,000 epinephrine) or 4% articaine (1:100,000 epinephrine). Success rates of 66% and 78% was observed with 4% articaine (27 out of 41 patients) and 2% lidocaine injections (32 out of 41 patients), respectively. However, no significant difference was observed (P = 0.2).
In a randomized double-blind study, Aggarwal et al. (2018) [26] investigated the anesthetic efficiency of 2% lidocaine with 1:80 000 epinephrine in two volumes, that is 0.2 mL vs. 0.6 mL, injected as a supplementary IL injection after the failure of primary IANB. As a result, 97 patients were injected with an IANB followed by the initiation of root canal treatment. Furthermore, 78 patients randomly received an IL injection using either of the two volumes after unsuccessful anesthesia. An HP VAS score ≤ 54 during the initial steps of treatment was considered as successful anesthesia. In this study, volumes of 0.2 mL and 0.6 mL of the solution was found to be successful in 64% and 84% of cases with failed primary IANB (P = 0.03), respectively.
In a single-blind randomized trial, Zarei et al. (2012) [24] compared the efficiency of supplemental anesthesia using PDL and IO injected using the X-Tip system concerning measured heart rate and pain level reported by the patient. Forty patients diagnosed with irreversible pulpitis who had reported pain after IANB using 2% lidocaine with 1:100,000 epinephrine were selected and divided randomly into two groups. One group of patients received IO injection using the X-tip system, whereas the other group received PDL injection. Pain was scored using the VAS. Patients reported a 100% success rate with X-Tip system injections and a 70% success rate with PDL injections. However, these differences were not significant (P = 0.02).
Aggarwal et al. (2020) [29] investigated the effect of supplemental IL injections administered after failed primary IANB using 2% lidocaine with two epinephrine concentrations. In total, 118 patients received primary IANB injections before endodontic treatment. Pain was assessed using the HP VAS. As a result, 88 patients reported pain during treatment and were allocated to two groups according to the concentration of epinephrine in the supplemental IL injection. The group that received 2% lidocaine and 1:80,000 epinephrine showed a success rate of 82%, while the other group that received 2% lidocaine with 1:200,000 epinephrine showed a success rate of 57%. However, the differences were not significant (P = 0.011).
5. Quality assessment
Three studies had a low risk of bias in most domains [26,27,29]. One study had unclear blinding of participants and results [24]. Evidence level grading was determined according to the National Services Scotland Guidelines [32]. Three studies had an evidence level of 1++; one study [24] had an evidence level of 1+ [26,27,29].
6. Meta-analysis
1) Forest plot calculations
RevMan 5.3 software was used for the quantitative analysis. The meta-analysis of the included studies was based on the comparison of a primary nerve block injection versus a supplementary IL injection administered after a failed IANB [24,26,27,29]. The random-effects meta-analysis is shown in the forest plot (Fig. 2). The combined risk ratios (RRs) were 3.56 (95% CI: 2.86, 4.44), favoring the supplemental injection. The statistical heterogeneity was set at 0%. The results proved that supplementary IL injection increases anesthetic efficacy in cases of failure to achieve adequate anesthesia through primary nerve block injections.
Fig. 2. Forest plot representation. CI, confidence interval; M-H, Mantel-Haenszel test; IANB, inferior alveolar nerve block; IL, intraligamentary.
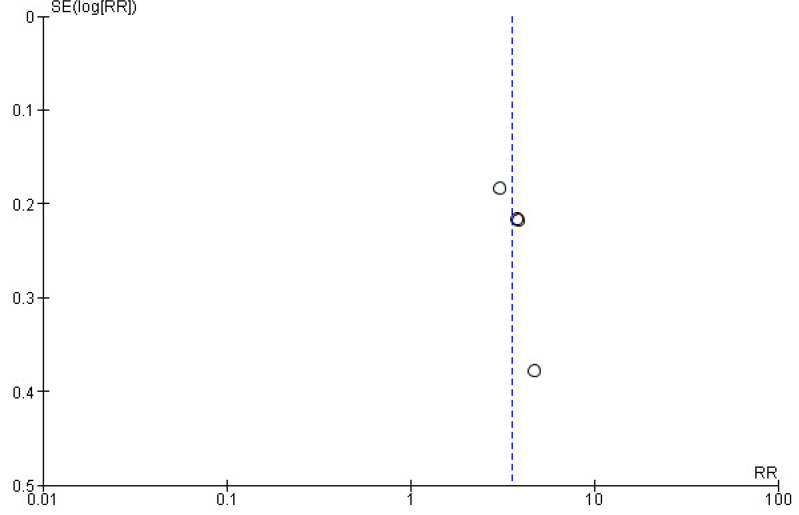
2) Funnel plots
Funnel plots were drawn to analyze the extent of bias for each publication; studies evaluating supplemental IL injections showed lower publication bias (Fig. 3).
Fig. 3. Funnel plot representation. RR, relative risk; SE, standard error.
DISCUSSION
In cases of irreversible pulpitis, IANB injections may not always be satisfactory [1,3]; both 2% lidocaine and 4% articaine solutions were associated with poor success rates [28]. Both IL and IO injections administer the anesthetic agent directly into the bone [3,9,10,14,17,18,19,20]. IO injections directly inject the solution as it perforates the buccal cortical plate [10]. On the other hand, IL injections administer the solution into the periodontal space under pressure; thus, the solution diffuses towards adjacent bony areas through natural perforations in the alveolar bone [9,10,17].
In this review, we have summarized the anesthetic efficacy of supplemental IL injections in cases of irreversible pulpitis, particularly in mandibular teeth. This is a viable and less invasive injection technique [9]. However, these techniques have adverse effects that include suboptimal anesthetic intervals and postoperative discomfort [3,22,33]. Moreover, it is a highly sensitive technique; detecting the “back-pressure” that ensures if the needle is within the PDL remains a challenge [21].
In endodontics, the IL technique has been studied as both a primary and a supplemental injection. Various clinical studies have focused on the effects of supplemental IL injections. Studies showing its anesthetic efficacy as a supplemental injection in symptomatic irreversible pulpitis showed a higher success rate of 85% [18,24,26,27,29].
A similar systematic review reported that pulpal anesthetic strategies showed the efficacy of all forms of supplemental techniques for symptomatic irreversible pulpitis in lower molars [34], including three studies for IL injection [18,24,26]. The present review reports on the efficacy of IL supplemental technique in mandibular teeth with symptomatic irreversible pulpitis, with two additional studies included in the final review [27,28].
The study by Kanaa et al. (2012) [18] was excluded from the current review because its success was evaluated via electric pulp testing and not through pain scales, as in the other four included studies. Furthermore, two other studies were excluded from the review because access preparation and pulp extirpation were not performed to assess pulpal anesthesia [35,36]. Another study by Nusstein (2005) [22] was also not included in the current review because it did not mention primary IANB failure, and the supplemental IL injection was administered to all included patients.
The limiting factor of the current review is the limited number of included studies; more reliable clinical trials are required. However, the cumulative risk of bias in every domain was low for all studies. A meta-analysis was performed to quantify the qualitative results of the review. The success rate was evaluated by the combined RR using a random risk model. According to the forest plot representation, the RRs were found to be 3.56 (95% CI: 2.86, 4.44), favoring supplemental IL injections. The statistical heterogeneity was set at 0%. These values indicated that supplemental IL injections improved anesthetic success rates. The results suggested better success rates of supplemental IL injections given after failure of the primary nerve block. The qualitative and quantitative results suggest the inclusion of supplemental IL injection after an ineffective primary IANB injection for a more optimal induction of anesthesia.
In conclusion, in this review, we focused on the important role of supplemental IL injections in clinical practice. The use of supplemental injections after a primary IANB failure is clinically relevant.
Footnotes
- Alpa Gupta: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
- Jitesh Wadhwa: Conceptualization, Data curation, Software, Supervision, Writing – review & editing.
- Vivek Aggarwal: Conceptualization, Formal analysis, Investigation, Methodology, Supervision.
- Namrata Mehta: Data curation, Formal analysis, Investigation, Methodology, Resources, Validation, Visualization, Writing – original draft, Writing – review & editing.
- Dax Abraham: Methodology, Project administration, Supervision, Writing – review & editing.
- Kritika Aneja: Data curation, Investigation, Methodology, Resources, Writing – original draft.
- Arundeep Singh: Conceptualization, Supervision, Visualization, Writing– review & editing.
DECLARATION OF INTERESTS: The authors have no conflicts of interest to declare.
References
- 1.Shahi S, Mokhtari H, Rahimi S, Yavari HR, Narimani S, Abdolrahimi M, et al. Effect of premedication with ibuprofen and dexamethasone on success rate of inferior alveolar nerve block for teeth with asymptomatic irreversible pulpitis: a randomized clinical trial. J Endod. 2013;39:160–162. doi: 10.1016/j.joen.2012.10.011. [DOI] [PubMed] [Google Scholar]
- 2.Nusstein J, Reader A, Nist R, Beck M, Meyers WJ. Anesthetic efficacy of the supplemental intraosseous injection of 2% lidocaine with 1:100,000 epinephrine in irreversible pulpitis. J Endod. 1998;24:487–491. doi: 10.1016/S0099-2399(98)80053-8. [DOI] [PubMed] [Google Scholar]
- 3.Reisman D, Reader A, Nist R, Beck M, Weaver J. Anesthetic efficacy of the supplemental intraosseous injection of 3% mepivacaine in irreversible pulpitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84:676–682. doi: 10.1016/s1079-2104(97)90372-3. [DOI] [PubMed] [Google Scholar]
- 4.Aggarwal V, Singla M, Miglani S, Kohli S. Comparative evaluation of mental incisal nerve block, inferior alveolar nerve block, and their combination on the anesthetic success rate in symptomatic mandibular premolars: a randomized double-blind clinical trial. J Endod. 2016;42:843–845. doi: 10.1016/j.joen.2016.02.015. [DOI] [PubMed] [Google Scholar]
- 5.Fowler S, Drum M, Reader A, Beck M. Anesthetic success of an inferior alveolar nerve block and supplemental articaine buccal infiltration for molars and premolars in patients with symptomatic irreversible pulpitis. J Endod. 2016;42:390–392. doi: 10.1016/j.joen.2015.12.025. [DOI] [PubMed] [Google Scholar]
- 6.Chaudhary P, Martenson ME, Baumann TK. Vanilloid receptor expression and capsaicin excitation of rat dental primary afferent neurons. J Dent Res. 2001;80:1518–1523. doi: 10.1177/00220345010800060801. [DOI] [PubMed] [Google Scholar]
- 7.Stenholm E, Bongenhielm U, Ahlquist M, Fried K. VRl- and VRL-l-like immunoreactivity in normal and injured trigeminal dental primary sensory neurons of the rat. Acta Odontol Scand. 2002;60:72–79. doi: 10.1080/000163502753509455. [DOI] [PubMed] [Google Scholar]
- 8.Hargreaves KM, Keiser K. Local anesthetic failure in endodontics: mechanisms and management. Endod Topics. 2002;1:26–39. [Google Scholar]
- 9.Meechan JG. Supplementary routes to local anaesthesia. Int Endod J. 2002;35:885–896. doi: 10.1046/j.1365-2591.2002.00592.x. [DOI] [PubMed] [Google Scholar]
- 10.Moore PA, Cuddy MA, Cooke MR, Sokolowski CJ. Periodontal ligament and intraosseous anesthetic injection techniques: alternatives to mandibular nerve blocks. J Am Dent Assoc. 2011;142(Suppl 3):13S–18S. doi: 10.14219/jada.archive.2011.0342. [DOI] [PubMed] [Google Scholar]
- 11.Lapidus D, Goldberg J, Hobbs EH, Ram S, Clark GT, Enciso R. Effect of premedication to provide analgesia as a supplement to inferior alveolar nerve block in patients with irreversible pulpitis. J Am Dent Assoc. 2016;147:427–437. doi: 10.1016/j.adaj.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 12.Aggarwal V, Jain A, Kabi D. Anesthetic efficacy of supplemental buccal and lingual infiltrations of articaine and lidocaine following an inferior alveolar nerve block in patients with irreversible pulpitis. J Endod. 2009;35:925–929. doi: 10.1016/j.joen.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 13.Aggarwal V, Singla M, Rizvi A, Miglani S. Comparative evaluation of local infiltration of articaine, articaine plus ketorolac and dexamethasone on anesthetic efficacy of inferior alveolar nerve block with lidocaine in patients with irreversible pulpitis. J Endod. 2011;37:445–449. doi: 10.1016/j.joen.2011.01.016. [DOI] [PubMed] [Google Scholar]
- 14.Parirokh M, Sadr S, Nakhaee N, Abbott PV, Askarifard S. Efficacy of supplementary buccal infiltrations and intraligamentary injections to inferior alveolar nerve blocks in mandibular first molars with asymptomatic irreversible pulpitis: a randomized controlled trial. Int Endod J. 2014;47:926–933. doi: 10.1111/iej.12236. [DOI] [PubMed] [Google Scholar]
- 15.Shapiro MR, McDonald NJ, Gardner RJ, Peters MC, Botero TM. Efficacy of articaine versus lidocaine in supplemental infiltration for mandibular first versus second molars with irreversible pulpitis: a prospective, randomized, double-blind clinical trial. J Endod. 2018;44:523–528. doi: 10.1016/j.joen.2017.10.003. [DOI] [PubMed] [Google Scholar]
- 16.Haas DA, Harper DG, Saso MA, Young ER. Comparison of articaine and prilocaine anesthesia by infiltration in maxillary and mandibular arches. Anaesth Prog. 1990;37:230–237. [PMC free article] [PubMed] [Google Scholar]
- 17.Malamed SF. The periodontal ligament (PDL) injection: an alternative to inferior alveolar nerve block. Oral Surg Oral Med Oral Pathol. 1982;53:117–121. doi: 10.1016/0030-4220(82)90273-0. [DOI] [PubMed] [Google Scholar]
- 18.Kanaa MD, Whitworth JM, Meechan JG. A prospective randomized trial of different supplementary local anesthetic techniques after failure of inferior alveolar nerve block in patients with irreversible pulpitis in mandibular teeth. J Endod. 2012;38:421–425. doi: 10.1016/j.joen.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 19.Pereira LA, Groppo FC, Bergamaschi Cde C, Meechan JG, Ramacciato JC, Motta RH, et al. Articaine (4%) with epinephrine (1:100,000 or 1:200,000) in intraosseous injections in symptomatic irreversible pulpitis of mandibular molars: anesthetic efficacy and cardiovascular effects. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116:e85–e91. doi: 10.1016/j.oooo.2011.10.045. [DOI] [PubMed] [Google Scholar]
- 20.Lin S, Wigler R, Huber R, Kaufman AY. Anaesthetic efficacy of intraligamentary injection techniques on mandibular molars diagnosed with asymptomatic irreversible pulpitis: a retrospective study. Aust Endod J. 2017;43:34–37. doi: 10.1111/aej.12169. [DOI] [PubMed] [Google Scholar]
- 21.Jing Q, Wan K, Wang XJ, Ma L. Effectiveness and safety of computer-controlled periodontal ligament injection system in endodontic access to the mandibular posterior teeth. Chin Med Sci J. 2014;29:23–27. doi: 10.1016/s1001-9294(14)60019-5. [DOI] [PubMed] [Google Scholar]
- 22.Nusstein J, Claffey E, Reader A, Beck M, Weaver J. Anesthetic effectiveness of the supplemental intraligamentary injection, administered with a computer-controlled local anesthetic delivery system, in patients with irreversible pulpitis. J Endod. 2005;31:354–358. doi: 10.1097/01.don.0000140565.88940.60. [DOI] [PubMed] [Google Scholar]
- 23.Fan S, Chen WL, Pan CB, Huang ZQ, Xian MQ, Yang ZH, et al. Anesthetic efficacy of inferior alveolar nerve block plus buccal infiltration or periodontal ligament injections with articaine in patients with irreversible pulpitis in the mandibular first molar. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:e89–e93. doi: 10.1016/j.tripleo.2009.06.012. [DOI] [PubMed] [Google Scholar]
- 24.Zarei M, Ghoddusi J, Sharifi E, Forghani M, Afkhami F, Marouzi P. Comparison of the anaesthetic efficacy of and heart rate changes after periodontal ligament or intraosseous X-tip injection in mandibular molars: a randomised controlled clinical trial. Int Endod J. 2012;45:921–926. doi: 10.1111/j.1365-2591.2012.02050.x. [DOI] [PubMed] [Google Scholar]
- 25.Shabazfar N, Daubländer M, Al-Nawas B, Kämmerer PW. Periodontal intraligament injection as alternative to inferior alveolar nerve block–meta-analysis of the literature from 1979 to 2012. Clin Oral Investig. 2014;18:351–358. doi: 10.1007/s00784-013-1113-1. [DOI] [PubMed] [Google Scholar]
- 26.Aggarwal V, Singla M, Miglani S, Kohli S, Sharma V, Bhasin SS. Does the volume of supplemental intraligamentary injections affect the anaesthetic success rate after a failed primary inferior alveolar nerve block? A randomised-double blind clinical trial. Int Endod J. 2018;51:5–11. doi: 10.1111/iej.12773. [DOI] [PubMed] [Google Scholar]
- 27.Aggarwal V, Singla M, Miglani S, Kohli S. Efficacy of Articaine versus Lidocaine administered as supplementary injection after a failed inferior alveolar nerve block: A randomised double blind study. J Endod. 2019;45:1–5. doi: 10.1016/j.joen.2018.09.012. [DOI] [PubMed] [Google Scholar]
- 28.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 29.Aggarwal V, Singla M, Saatchi M, Hasija M. Anaesthetic efficacy of 2% lidocaine with different concentrations of epinephrine (1:80,000and 1:200,000) in intraligamentary injection after a failed primary inferior alveolar nerve block:a randomized double-blind study. Acta Odontol Scand. 2020;78:275–280. doi: 10.1080/00016357.2019.1700302. [DOI] [PubMed] [Google Scholar]
- 30.Heft MW, Parker SR. An experimental basis for revising the graphic rating scale for pain. Pain. 1984;19:153–161. doi: 10.1016/0304-3959(84)90835-2. [DOI] [PubMed] [Google Scholar]
- 31.Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration; 2011. [updated March 2011]. [Accessed August 11, 2015]. Available at: www.cochrane-handbook.org . [Google Scholar]
- 32.Harbour R, Miller J. A new system for grading recommendations in evidence based guidelines. BMJ. 2001;323:334–336. doi: 10.1136/bmj.323.7308.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.White JJ, Reader A, Beck M, Meyers WJ. The periodontal ligament injection: a comparison of the efficacy in human maxillary and mandibular teeth. J Endod. 1988;14:508–514. doi: 10.1016/S0099-2399(88)80109-2. [DOI] [PubMed] [Google Scholar]
- 34.Zanjir M, Lighvan NL, Yarascavitch C, Beyene J, Shah PS, Azarpazhooh A. Efficacy and Safety of Pulpal Anesthesia strategies during endodontic treatment of permanent mandibular molars with symptomatic irreversible pulpitis: a systematic review and network meta-analysis. J Endod. 2019;45:1435–1464. doi: 10.1016/j.joen.2019.09.002. [DOI] [PubMed] [Google Scholar]
- 35.Mohajeri L, Salehi F, Mehrvarzfar P, Arfaee H, Bohluli B, Hamedy R. Anesthetic efficacy of meperidine in teeth with symptomatic irreversible pulpitis. Anesth Prog. 2015;62:14–19. doi: 10.2344/0003-3006-62.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cohen HP, Cha BY, Spångberg LSW. Endodontic anesthesia in mandibular molars: a clinical study. J Endod. 1993;19:370–373. doi: 10.1016/S0099-2399(06)81366-X. [DOI] [PubMed] [Google Scholar]